Jonathan Adler, M.D., FAAEM
- Assistant in Emergency Medicine,
- Massachusetts General Hospital
- Instructor in Medicine,
- Harvard Medical School
- Boston, MA
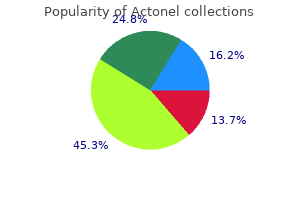
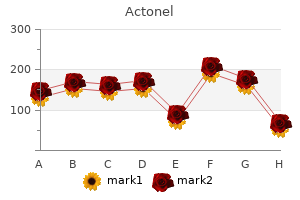
Clear from the fall is important medications may be administered in which of the following ways purchase actonel australia, and those at explanations about the immunization and risk should be immunized while seated medications given before surgery generic actonel 35 mg line. The local lesion a live attenuated (weakened) strain of begins as a papule medications similar to cymbalta order 35 mg actonel otc, two or more weeks Mycobacterium bovis treatment quadriceps strain buy 35 mg actonel otc. It does not prevent typically as a result of improper injection primary infection and does not prevent technique when the vaccine is given into reactivation of latent pulmonary infection treatment models order actonel with a visa. An adherent or fstulated lymph gland may be drained and an anti Hepatitis B vaccines products are tuberculosis drug may be instilled locally symptoms bone cancer buy generic actonel 35 mg line. It should not be frozen or exposed traditionally has been seen in children to freezing temperatures. The l A 4-dose schedule may be infection is spread by direct contact with administered if a birth dose is given and a combination vaccine is used to blood and body fuids. Diphtheria is caused by toxigenic strains l Children over 7 years of age and of corynebacterium diphtheriae. Usually adults, who have not been immunized the infection presents as membranous during infancy, three doses of vaccine nasopharyngitis or obstructive are required with an interval of 4-6 laryngotracheitis. Other serious weeks between the frst and second complications of diphtheria include doses, and 6-12 months between the myocarditis and peripheral neuropathies. It is hypotonic hyporesponsive episode) characterized by generalized rigidity and within 48 hours after receiving a convulsive spasms of skeletal muscles. The muscle stiffness usually involves the jaw (lockjaw) and neck and then l Seizure 3 days or more after receiving becomes generalized. They should not be frozen disorder, uncontrolled seizures, or or exposed to freezing temperatures. The minimum interval between vaccine: defer vaccination until at least 1st and 2nd doses and between 3rd 10 years have elapsed since the last and 4th doses is 4 weeks. Polio is an infectious disease caused l Exaggerated local (Arthus-like) reaction by a virus that lives in the throat and is occasionally reported following intestinal tract. Most of polio infections receipt of diphtheria or tetanus are unapparent or asymptomatic and containing vaccine. The reaction less than 1% of all polio infections result presents as extensive painful swelling in faccid paralysis. The disease affects from shoulder to elbow starting 2-8 the anterior horn cells of the spinal cord hours after injection. Measles recommended 5 years after the frst causes fever, runny nose, cough and -54 Immunization Guidelines Department of Public Health & Safety, Health Policy & Strategy Sector rash. Measles vaccine is available as l Moderate reactions including monovalent (measles only) formulation, febrile seizure, arthralgia, and and in combination formulations such thrombocytopenia. Central produces a subclinical or a mild disease nervous system involvement and orchitis characterized by rash, mild fever and are relatively common complications. Occasionally patients Some other rare complications include develop arthralgia, thrombocytopenia, thyroiditis, myocarditis, pancreatitis, and and rarely encephalitis. Chickenpox is an infectious disease caused by the varicella-zoster virus, l Persons aged >13 years without which results in a blister-like rash, evidence of varicella immunity should itching, tiredness, and fever. Adults, receive two doses of single-antigen infants, adolescents, and immuno varicella vaccine administered compromised people are more likely subcutaneously, 4-8 weeks apart. It is possible for these people to infect other members of their Varicella vaccine can be administered as household, but this is extremely rare. However, other anaphylaxis) after a previous dose or brands of single varicella or combination to a vaccine component. Pediatric formulations are l the safety of hepatitis A vaccination given to children 1-18 years of age and during pregnancy has not been adult formulations are recommended to determined. It should not be frozen or exposed negative, diplococcus responsible for to freezing temperatures. Meningococcal meningitis reconstituted vaccine contains 50 mgm presents as fever, stiff neck and a of each polysaccharide group. Up to 19% of all survivors suffer serious sequelae like Meningococcal polysaccharides deafness, neurologic defcits or limb loss. Vaccine: Invasive meningococcal disease is l Mencevax is a Lyophilized preparation acquired by aerosol or direct inhalation of purifed polysaccharides from of respiratory secretions from a healthy Neisseria meningitidis (meningococcus) or sick person. Meningitidis has several adults against meningococcal disease sero-groups based on differences in the caused by meningococci of serogroups capsular proteins. However, recent reports of W-135 children over 5 years of age immunity meningococcal disease in Saudi Arabia will persist for up to 3 years. Conjugate polysaccharides from meningococci of vaccines induce enhanced levels of anti the respective sero-groups. It is licensed either bivalent (A and C) or quadrivalent for active immunization for ages 2 years (A, C, Y and W-135). Meningococcal Polysaccharide diphtheria the recommended single dose of toxoid conjugate vaccine (Menactra) is -59 Specifc Vaccines conjugate vaccine and is approved for 9 swelling at the injection site that months through 55 years of age. Human Infuenza can be caused by one l Children who receive primary of three Infuenza viruses A, B or C. Please refer to given to targeted high risk groups section for live virus vaccines. In addition, for the close, of severe gastroenteritis in infants and household contacts of people who are in young children worldwide. The clinical the high risk group, vaccination is a good spectrum of rotavirus illness in children strategyInfuenza vaccine must be given ranges from mild, watery diarrhea of annually. Both products administered to infants with acute differ in composition and schedule of moderate or severe gastroenteritis until administration. Serious complications include -62 Immunization Guidelines Department of Public Health & Safety, Health Policy & Strategy Sector intestinal hemorrhage or perforation. A third heat-phenol parenteral inactivated vaccine is also available, but Typhoid vaccination is recommended for: its use is associated with substantially l Travelers to areas where a risk of more adverse reactions, with no increase exposure to S typhi is recognized. Afghanistan, Latin America, and Africa, who have prolonged exposure to Oral Ty21 a vaccine is indicated for contaminated food and drink. The vaccine should be taken as typhoid fever carrier, such as occurs one enteric-coated capsule every other with continued household contact. Each l Laboratory workers with frequent capsule should be taken with cool liquid, contact with S typhi. The capsule must be l Regular booster doses are kept refrigerated and all four doses must recommended for those at ongoing be taken to achieve maximal effcacy. For those 10 years of age and l Oral typhoid vaccine should not older, the dose is 0. If time is insuffcient for administration of two doses of the vaccine at an interval of l History of allergy to typhoid vaccine. Both vaccines are also effective or other live viral vaccines along with for preventing pre-cancer cervical typhoid vaccine is not contraindicated. To total of three injections are given using avoid serious injury related to a either vaccine. This does not eliminate syncopal episode, vaccine providers the need of post-exposure vaccination is should consider observing patients for someone who gets an animal bite wound, 15 minutes after they are vaccinated. The main indications for be deferred until after the patient pre-exposure vaccination are traveler to improves. In addition, lab workers and Rabies is a severe form of persons who work with animals, for eg. The clinical If pre-exposure vaccine is not given, in illness progresses from a non-specifc the event of a possible virus exposure, prodrome to paresis or paralysis; spasms the patient will need post exposure of swallowing muscles can be initiated immunization. The disease is endemic in all continents Prevention of rabies is best achieved except Antartica and is transmitted by by education to avoid contact with stray an animal bite. Once an exposure has occurred, dogs are the most common reservoirs, immediate and adequate medical care is but monkeys that live around temples, critical. Mild systemic effects fever vaccination is a requirement for like headache, nausea, and myalgia entry into several countries in the sub can also happen. In addition, it is highly l Approximately 6% of persons requiring recommended when traveling to certain boosters can get an immune-like countries in South America including reaction characterized by urticaria, Brazil, Colombia, parts of Venezuela and pruritus or malaise. It is no longer used in to all traveler aged > 9 months of most developed countries. Vaccination of infants between 6-9 months can be considered, For all eligible persons, a single dose if benefts outweigh the risk. However, such waivers do not guarantee entry into the Common adverse reactions include mild destination country. Similarly, pregnant persons Yellow fever associated viscerotropic who cannot postpone or avoid travel disease is a severe illness, similar to to such a country, may, in special a wild type viral disease with acute circumstances, be given the vaccine dissemination in all organs, often leading because the risk of contracting the to multisystem organ failure and death. Vaccine vaccinating one segment of society can preventable communicable illnesses have far reaching results not only on must become an important pillar in the that sub-population but on those who overall wellbeing of the entire social are in immediate contact. One of the goals A primary course for adults is a 3 dose is more people protected against more series of tetanus and diphtheria diseases. This goal can only be fulflled containing vaccines; usually Td, at 0, 4 by expanding the reach of immunization and 12 weeks. For adults who have not to populations beyond infancy to include received a dose of Tdap previously, one adolescents as well as adults. If for immunity and if non-immune frst dose already pregnant, vaccination should be after delivery. Herpes zoster vaccine Measles and Mumps Given the severe morbidity associated with post-herpetic neuralgia in the elderly, Adults who were born before 1957 are considered immune. Those born after a single dose of herpes zoster vaccine is should have either documented evidence indicated for all adults over 60 years of of immunity or a history of clinical disease. Dose should be given regardless of If neither present, 1 or more doses of prior episode of Zoster. Seasonal Infuenza Vaccine Rubella All international regulatory bodies All women of child bearing age should recommend vaccination of all adults have documentation of rubella immunity with infuenza vaccine annually. If not immune, only 1 dose of should be taken to take only the rubella containing vaccine should be parenteral, inactivated vaccine if any given and counseling should be provided immunocompromised state exists. All adults should be evaluated for Recommended vaccines for high risk medical conditions that place them in the groups are summarized in Table 12 Table 12: Recommended vaccinations in high risk groups. It can also provide Infuenza vaccine the infant passive protection against All women who will be pregnant in infections acquired after birth. Ideally, the fu season need to be vaccinated -72 Adult Immunization with Infuenza. Ideally this should be required when traveling to areas of Sub delayed till after the frst trimester, but Saharan Africa and South America where the complications of infuenza can be so it is endemic. Typhoid Tetanus and Diphtheria vaccine Typhoid immunization is recommended If there is history of incomplete primary for travelers to Southeast Asia, Mexico, vaccination or if the last booster was and other developing countries. Hepatitis A immunization is recommended Newer guidelines favor giving two doses for all travelers to susceptible countries. Specialized circumstances in endemic Travel advice regarding immunization countries where contact with wild animals varies with the exact location of visit, duration of stay and activities involved is likely. Yellow fever vaccine Vaccination of patients who underwent bone marrow transplant is summarized in Immunization against yellow fever is Table 13. Pan American Health Organization, Regional Offce of the World Health Organization Division of Vaccines and Immunization. General recommendations on Immunization: recommendations of the Advisory Committee on Immunization Practices. New foodstuffs are still investigated with the aim to improve the diet and conduce to a better health state of the population. Their high nutritious and dietary quality meets the demands of the food industry and consumers. Our collective dealt with quinoa, a commodity of Andean, because quinoa is a good source of essential amino acids such as lysine and methionine. Quinoa contains relatively high quantities of vitamins (thiamin, vitamin C) and minerals. Keywords: quinoa; essential amino acids; nutrition quality Quinoa (Chenopodium quinoa Willd. The classification of quinoa was first made from Quinoa is one of the oldest crops of the Ameri the colour of the plant and fruits. Archeological findings in northern was based on the morfological types of the plant. Quinoa collected in Ecuador, Peru, and Bolivia in the whole Andrean region, in Columbia, Equa has been classified into 17 races, however, more dor, Peru, Bolivia, and Chile, before the Spanish races may exist. For this reason, Quinoa grows in the altitudes from the sea level to it was classified as food for poor people (Valen the Andean highlands.
Contraindications the drug should not be used in the presence of acute exu Toxicity dative dermatitis and should not be applied near the eyes medicine recall purchase actonel 35mg mastercard. Reactions occur frequently and include headache treatment irritable bowel syndrome cheap 35mg actonel with amex, weak ness ombrello glass treatment cheap actonel express, malaise treatment tmj order actonel 35mg, fever kerafill keratin treatment order actonel with paypal, joint pain medications names and uses best purchase for actonel, anorexia, nausea, and Dapsone (Jacobus) vomiting. Severe re Dapsone is supplied as 25 and 100-mg scored tablets action may require steroid therapy and antihistamines. Treatment of patients with heavy microfilaremia due to lo Administration iasis may cause allergic encephalitis, nephritis, or myocar ditis. Patients with many microfilariae or onchocerciasis Dapsone should be taken orally, and the dosage should be in ocular tissues may experience keratitis, chorioretinitis, individually titrated. Dose reductions are generally required Toxicity in patients with renal impairment. The drug should prob Dapsone has been associated with frequent rashes, tran ably be avoided in pregnancy but is not excreted in breast sient headaches, gastrointestinal irritation, anorexia, and milk. Complete blood counts should be performed frequently because the drug has Diethylcarbamazine citrate, an investigational drug, is been associated with death from agranulocytosis, aplastic an anthelmintic agent that does not resemble other anti anemia, and other blood dyscrasias. It is a synthetic organic compound which is highly specific for several parasites and does not Contraindications contain any toxic metallic elements. It is used to treat pa the drug should not be given to patients with hypersen tients with certain filarial infections, including lymphatic sitivity to dapsone. This reaction kills microfilariae but only a variable proportion of adult is frequently dose related. Another drug, ivermectin, rapidly reduces micro caution to these patients or to patients who have been filaremia levels and may inhibit larval development in exposed to other agents or conditions such as infection or mosquitoes, but it does not kill adult worms and is not diabetic ketosis capable of producing hemolysis. The drug is hydrolyzed in the bowel to Treatment of Parasitic Infections 743 the active compound, diloxanide, which is 90% ab Fumagillin (Fumidil-B) sorbed. Preparation Administration the drug is supplied as a 10-mg/ml suspension in physi Furamide is given by mouth with repeated treatments as ologic saline. For lesions due to Vittaforma corneae, topical the most common adverse effect is flatulence. Other therapy is generally not effective and keratoplasty may side effects are seen, including vomiting, pruritus, and be required. Contraindications Administration the use of Furamide is generally not recommended during Fumagillin should be applied topically once an hour until pregnancy or lactation. Comment Toxicity the drug helps clear the bowel of Entamoeba histolytica cysts; however, it is not effective for treating invasive dis the soluble salt is toxic and should not be ingested; topi ease in the bowel wall or liver. Preparation the drug is available as a 200-mg/ml solution, and is used Furazolidone (Furoxone) (Roberts) to treat African trypanosomiasis. Preparation Administration Furoxone is supplied as 100-mg tablets or as a flavored Ornidyl is given as a continuous i. Eflornithine crosses the blood-brain barrier; thus it is beneficial for central nervous system disease associated Administration with African trypanosomiasis. Apparently furazolidone is more Toxicity effective by 50% than metronidazole in inhibiting in vitro Side effects occur in about 40% of patients; they include cyst differentiation of Giardia lamblia. Furoxone can cause polyneuritis, nausea, vomiting, diz ziness, drowsiness, and general malaise. Skin rashes Contraindications and agranulocytosis have occasionally been reported. It may Furazolidone is chemically similar to nitrofurantoin, worsen hemolytic disorders. Due to insufficient safety data, which is well known to cause pulmonary hypersensitiv the drug should not be used during pregnancy or lactation. Eflornithine inhibits ornithine decarboxylase, an enzyme required for the formation of polyamines, thus leading to Contraindications inhibition of parasite growth. However, it is ineffective as the drug should not be given to individuals hypersensi monotherapy for T. Alcohol should be avoided during treatment, the drug is thought to act by inactivating parasitic en because disulfiram-like reactions have been reported. Although it Furazolidone is a monoamine oxidase inhibitor and is effective for treating intestinal organisms, it is not effec should not be given concomitantly with other similar tive for treating invasive disease in the bowel wall or liver; drugs. It has docu mented activity against Balantidium coli, Dientamoeba Iodoquinol/Diiodohydroxyquin (Yodoxin) fragilis, Giardia lamblia, and Blastocystis hominis. The drug is considered effective thetic macrolide used to treat nondisseminated strongyloi against the trophozoite and cyst forms. It is also now used for the treatment of ectoparasitic infestations Administration such as scabies and lice, although it has no effect on the the drug should be given with meals. The drug is given orally with water 1 h before breakfast and is rapidly absorbed after ingestion. Toxicity There may be various forms of skin eruptions, urticaria, Toxicity and pruritus. There may also be nausea, vomiting, ab the drug can cause fever, headache, rash, increased dominal cramps, diarrhea, and pruritus ani. A headache, vertigo, and enlargement of the thyroid have Mazzotti-type reaction has been seen in patients with on been reported. Most adverse effects are a result of the host eral neuropathy have been reported in association with immune response to destruction of the parasites rather prolonged high-dosage 8-hydroxyquinoline therapy. Contraindications Contraindications Iodoquinol should not be given to patients with known Ivermectin should not be given to pregnant or lactating hypersensitivity to iodine or any 8-hydroxyquinoline women, because it has been noted to cause birth defects compound, with renal or thyroid disease, or with severe in mice. Historical data have shown that microfilaricidal liver disease not due to amebiasis. Iodoquinol should drugs, such as diethylcarbamazine citrate, might cause be used with caution in patients with thyroid disease. These effects may due to allergic and inflammatory responses to the death persist for as long as 6 months after discontinuation of microfilariae. Patients treated with Stromectol for on of therapy; this effect is unrelated to thyroid function. The Comment recommended doses and duration of therapy should Ivermectin is active against various life cycle stages of not be exceeded. It is active against the tissue the protein-bound iodine level months after therapy. The adult parasites reside in subcutaneous should probably be avoided during pregnancy or lacta nodules which are infrequently palpable. Ivermectin may be highly effective againstStrongyloides It may cause skin irritation. The safety and effectiveness of Ovide occur in invertebrate nerve and muscle cells. This leads lotion in children younger than 6 years has not been to an increase in the permeability of the cell membrane to established in well-controlled trials. Mebendazole (Vermox) (McNeil) the drug is also effective against the microfilariae of Wuchereria bancrofti, Brugia malayi, and Loa loa. Rarely, patients with onchocerciasis who are also heavily infected Preparation with L. Mebendazole is indicated for the treatment adverse experiences have also been reported: back pain, of Enterobius vermicularis (pinworm), Trichuris trichiura conjunctival hemorrhage, dyspnea, urinary and/or fecal (whipworm), Ascaris lumbricoides (common roundworm), incontinence, difficulty in standing and/or walking, men Ancylostoma duodenale (common hookworm), and Necator tal status changes, confusion, lethargy, stupor, or coma. In humans, approximately 2% of the administered of ivermectin; a cause-and-effect relationship has not been drug is excreted in urine and the remainder is excreted in the established. For individuals who warrant treatment with feces as unchanged drug or a primary metabolite. The drug inhibits the formation of nematode microtubules and causes glucose depletion in the worms. Malathion (Ovide) (Taro Pharmaceuticals) Periodic assessment of the hematopoietic and hepatic system is advisable during prolonged therapy. Abdominal pain and diarrhea occasionally occur, par Malathion is an organophosphate agent which acts as a ticularly with the expulsion of a large number of worms pediculicide by inhibiting cholinesterase activity in vivo. It is placed on dry hair in a sufficient amount to thoroughly Contraindications wet the hair. The hair is then allowed to dry naturally and the drug is teratogenic in rats, but the incidence of abor shampooed after 8 to 12 h. It is then rinsed, and a fine tion and malformations in humans does not exceed the comb is used to remove dead lice and nits. The drug, however, is not present 7 to 9 days later, the drug should be reapplied. Because the patients with severe hepatic disease, the drug should be potential for transdermal absorption of malathion from used with caution. There is no evidence that mebendazole, Ovide lotion is not known at this time, strict adherence even at high doses, is effective for treating hydatid disease. Increased in bioavailability of the tablet formation compared with an cidences of resistance have also been reported in other oral solution was over 85%. Lariam is indicated for the treatment of mild to moderate acute malaria caused by mefloquine Administration susceptible strains of P. Mefloquine is also indicated for the pro the most frequent side effects include nausea, vomiting, phylaxis of P. Severe including those caused by chloroquine-resistant strains of seizures and delirium have been reported occasionally in P. The drug can also po if the potential benefit justifies the potential risk to the tentiate dysrhythmias in patients taking beta blockers. Women of childbearing potential who are travel Periodic evaluation of hepatic function should be per ing to areas where malaria is endemic should be warned formed during prolonged prophylaxis. Women of childbearing po tential should also be advised to practice contraception Contraindications during malaria prophylaxis with mefloquine and for up Use of Lariam is contraindicated in patients with a to 3 months thereafter. However, in the case of unplanned known hypersensitivity to mefloquine or related com pregnancy, malaria chemoprophylaxis with mefloquine is pounds. It is be withdrawn and an alternative medication should be used to treat African trypanosomiasis. It is to be administered only in the hospital In case of life-threatening, serious, or overwhelming by or under the immediate supervision of a physician. Comment Although its exact mechanism of action is not known, Toxicity mefloquine is an antimalarial agent which acts as a Abdominal pain, nausea, vomiting, and diarrhea are com blood schizonticide. Reactive encephalopathy is not uncommon and is more Treatment of Parasitic Infections 747 likely to occur in debilitated patients and when high doses sion. Care must be taken to follow instructions difficulties, restlessness, and sleep disorders. Myocardial for reconstitution of the solution, because neutralization damage, albuminuria, and hypertension have also been re with bicarbonate is necessary to bring the pH from 0. Toxicity Rare side effects may include black, tarry stools; blood Reactions to therapy are common, especially when the in urine or stools; changes in skin color of face; fainting; drug is given in doses appropriate for treating amebiasis. Ataxia, tightness in chest; trouble in breathing; unusual bleeding paresthesias, insomnia, and irritability may also occur. Contraindications A moderate leukopenia occasionally occurs, but levels Patients with impaired hepatic or renal function should return to normal after completion of therapy. It include blood dyscrasias, dysuria, incontinence, cystitis, may increase the chance of side effects in patients with dyspareunia, and fever. Contraindications the drug should not be given to patients with a history Comment of blood dyscrasia, active central nervous system disease, Melarsoprol, an investigational drug, is an arsenical com and/or known sensitivity to metronidazole. Doses should pound used for treating African trypanosomiasis be reduced in patients with severe liver disease. Consumption of alcohol drug apparently interferes with parasite energy generation should be avoided during the first days of treatment and trophozoite multiplication. Other alcohol-containing preparations (for example, elixirs, cough syrups, and tonics) may also cause problems. These problems may last for at least a day after Preparation the drug has been discontinued. Leukocyte counts with Flagyl is supplied as 375-mg tablets for oral adminis differential blood counts are recommended before and tration and as 750-mg extended-release tablets (Flagyl after therapy. It is also available in single-dose vials containing 500 mg of ly Miltefosine (Impavido) (Zentaris, Germany) ophilized powder or in 100-ml plastic containers con taining a solution of 500 mg/100 ml or isotonic-buffered solution for parenteral injection. If metronidazole is being Preparation prescribed for trichomoniasis, sexual partners are often the drug is given orally at 30 mg/kg twice a day; it treated at the same time, even if they are asymptomatic. Good activity has also been documented administered slowly as an intermittent or continuous infu against L. Administration the drug is given in two divided doses or a single dose Contraindications orally for 28 days. It is available as 50-mg and 10-mg Niclosamide should not be given to patients shown to be capsules. Insufficient data are available for an assessment of the hazards of use of this drug during Toxicity pregnancy. It is not recommended for pregnant women Most patients tolerate therapy with few or no side effects. Urea and creatinine levels usually re turn to normal by the end of the second week of therapy. Preparation Gastrointestinal symptoms could be serious in severely ill Nifurtimox is a nitrofuran and is supplied as 100-mg tab patients who are malnourished and dehydrated. Contraindications the drug should not be used during pregnancy or Administration lactation.
If suspect high altitude pulmonary edema medicine zalim lotion purchase actonel online, treat per the Altitude Illness guideline Patient Safety Considerations No recommendations Notes/Educational Pearls Key Considerations 1 medicine cabinets with lights generic 35mg actonel. Theoretical risk of hypotension and pneumothorax as non-invasive positive pressure ventilation increases intrathoracic pressure which decreases venous return and cardiac output iii mueller sports medicine cheap actonel online amex. Allow patient to remain in position of comfort patients may decompensate if forced to lie down 4 symptoms celiac disease buy 35 mg actonel visa. Examples are: sildenafil (Viagra medications bad for kidneys discount actonel online american express, Revatio) medications 4 less canada actonel 35 mg generic, vardenafil (Levitra, Staxyn), tadalafil (Cialis, Adcirca) which are used for erectile dysfunction and pulmonary hypertension. Nitroglycerin reduces left ventricular filling pressure primarily via venous dilation. At higher doses the drug variably lowers systemic afterload and increases stroke volume and cardiac output. Pulmonary edema is more commonly a problem of volume distribution than overload, so administration of furosemide provides no immediate benefit for most patients. High-dose nitrates can reduce both preload and afterload and potentially increase cardiac output. A concern with high doses of nitrates is that some patients are very sensitive to even normal doses and may experience marked hypotension. It is therefore critical to monitor blood pressure during high-dose nitrate therapy. Effectiveness of prehospital continuous positive airway pressure in the management of acute pulmonary edema. Out of hospital continuous positive airway pressure ventilation versus usual care for acute respiratory failure: A randomized controlled trial. Paramedic identification of acute pulmonary edema in a metropolitan ambulance service. Revision Date September 8, 2017 183 Trauma General Trauma Management Aliases None noted Patient Care Goals 1. Rapid and safe transport to the appropriate level of trauma care Patient Presentation Inclusion Criteria 1. Patients of all ages who have sustained an injury as a result of mechanical trauma. Assess for and stop severe hemorrhage [see Extremity Trauma/External Hemorrhage Management guideline] b. Assess airway patency by asking the patient to talk to assess stridor and ease of air movement ii. Look for injuries that may lead to airway obstruction including unstable facial fractures, expanding neck hematoma, blood or vomitus in the airway, facial burns/inhalation injury iii. Signs of hemorrhagic shock include: tachycardia, hypotension, pale, cool clammy skin, capillary refill 2 seconds 184 f. Evaluate for clinical signs of traumatic brain injury with herniation including: 1. Rapid evaluation of entire body to identify sites of penetrating wounds or other blunt injuries. Stop severe hemorrhage [see Extremity Trauma/External Hemorrhage Management guideline] 2. Establish patent airway with cervical spine precautions, per the Airway Management and Spinal Care guidelines b. If respiratory efforts are inadequate, assist with bag-mask ventilation and consider airway adjuncts. If patient is unable to maintain airway, consider oral airway (nasal airway should not be used with significant facial injury or possible basilar skull fracture) c. If impending airway obstruction or altered mental status resulting in inability to maintain airway patency, secure definitive airway 3. If absent or diminished breath sounds in a hypotensive patient, consider tension pneumothorax and perform needle decompression b. If pelvis is unstable and patient is hypotensive, place pelvic binder or sheet to stabilize pelvis b. Minimize scene time (goal is under 10 minutes) and initiate rapid transport to the highest level of care within the trauma system. Palpate head and scalp and face and evaluate for soft tissue injury or bony crepitus 2. Palpate once for instability by applying medial pressure on the iliac crests bilaterally vi. Splint obvious extremity fractures per the Extremity Trauma/External Hemorrhage Management guideline iii. Provide pain medication per the Pain Management guideline Patient Safety Considerations 1. Life-threatening injuries identified on primary survey should be managed immediately with rapid transport to a trauma center, while the secondary survey is performed enroute 2. Patients with compensated shock may not manifest hypotension until severe blood loss has occurred b. Patients with traumatic brain injury may deteriorate as intracranial swelling and hemorrhage increase 3. Anticipate potential for progressive airway compromise in patients with trauma to head and neck Notes/Educational Pearls Key Considerations 1. Target scene time less than 10 minutes for unstable patients or those likely to need surgical intervention 3. If patient develops difficulty with ventilation, reassess breath sounds for development of tension pneumothorax b. If extremity hemorrhage is controlled with pressure dressing or tourniquet, reassess for evidence of continued hemorrhage c. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. Guidelines for the Field Triage of Injured Patients: Recommendations of the National Expert Panel on Field Triage, 2011. Hypotensive resuscitation strategy reduces transfusion requirements and sever postoperative coagulopathy in trauma patients with hemorrhagic shock: preliminary results of a randomized controlled trial. Revision Date September 8, 2017 189 Blast Injuries Aliases None noted Patient Care Goals 1. Maintain patient and provider safety by identifying ongoing threats at the scene of an explosion 2. Identify multi-system injuries which may result from a blast, including possible toxic contamination 3. Prioritize treatment of multi-system injuries to minimize patient morbidity Patient Presentation Inclusion Criteria 1. Toxic chemical contamination Exclusion Criteria No recommendations Patient Management Assessment 1. Assess for and stop severe hemorrhage [see Extremity Trauma/ External Hemorrhage Management guideline] 2. Evaluate adequacy of respiratory effort, oxygenation, quality of lung sounds, and chest wall integrity b. Consider possible pneumothorax or tension pneumothorax (as a result of penetrating/blunt trauma or barotrauma) 4. Rapid evaluation of entire skin surface, including back (log roll), to identify blunt or penetrating injuries Treatment and Interventions 1. Hemorrhage control: Control any severe external hemorrhage [see Extremity Trauma/ External Hemorrhage Management guideline] 2. Secure airway, utilizing airway maneuvers, airway adjuncts, supraglottic device, or endotracheal tube [see Airway Management guideline] b. If thermal or chemical burn to airway is suspected, early airway control is vital 3. Exposure Keep patient warm to prevent hypothermia Patient Safety Considerations 1. Consider possibility of subsequent explosions, structural safety, possible toxic chemical contamination, the presence of noxious gasses, and other hazards b. In a possible terrorist event, consider the possibility of secondary explosive devices 2. If the patient has sustained burns (thermal, chemical, or airway), consider transport to specialized burn center Notes/Educational Pearls Key Considerations 1. Scene safety is of paramount importance when responding to an explosion or blast injury 2. Patients sustaining blast injury may sustain complex, multi-system injuries including: blunt and penetrating trauma, shrapnel, barotrauma, burns, and toxic chemical exposure 3. Consideration of airway injury, particularly airway burns, should prompt early and aggressive airway management 4. Tension pneumothorax Hypotension or other signs of shock associated with decreased or absent breath sounds, jugular venous distension, and/or tracheal deviation 191 b. Tympanic membrane perforation resulting in deafness which may complicate the evaluation of their mental status and their ability to follow commands 6. Primary transport to a trauma or burn center is preferable, whenever possible Pertinent Assessment Findings 1. Revision Date September 8, 2017 193 Burns Aliases None noted Patient Care Goals Minimize tissue damage and patient morbidity from burns Patient Presentation 1. Transport to most appropriate trauma center when there is airway or respiratory involvement, or when significant trauma or blast injury is suspected 2. Consider air ambulance transportation for long transport times or airway management needs beyond the scope of the responding ground medic 3. Proper protective attire including breathing apparatus may be required Patient Management Assessment 1. Consider spinal precautions for those that qualify per the Spinal Care guideline 5. High flow supplemental oxygen for all burn patients rescued from an enclosed space 5. For pediatric patients weighing less than 40 kg, use length-based tape for weight estimate and follow c. Prevent systemic heat loss and keep the patient warm Special Treatment Considerations 1. Airway burns can rapidly lead to upper airway obstruction and respiratory failure 3. Particularly in enclosed-space fires, carbon monoxide toxicity is a consideration and pulse oximetry may not be accurate [see Carbon Monoxide Poisoning guideline] 5. For specific chemical exposures (cyanide, hydrofluoric acid, other acids and alkali) [see Topical Chemical Burn guideline] 6. Consider decontamination and notification of receiving facility of potentially contaminated patient. Onset of stridor and change in voice are sentinel signs of potentially significant airway burns, which may rapidly lead to airway obstruction or respiratory failure 2. Recognizing that pain is undertreated in injured patients, it is important to assess whether a patient is experiencing pain o Trauma-04: Trauma patients transported to trauma center. Simple derivation of the initial fluid rate for the resuscitation of severely burned adult combat casualties: in Silico validation of the rule of ten. Revision Date September 8, 2017 197 Crush Injury Aliases Crush, compartment syndrome Patient Care Goals 1. Minimize systemic effects of the crush syndrome Patient Presentation Inclusion criteria Traumatic crush mechanism of injury Exclusion criteria Non-crush injuries Patient Management Assessment 1. The treatment of crushed casualties should begin as soon as they are discovered 2. If severe hemorrhage is present, see Extremity Trauma/External Hemorrhage Management guideline 3. Intravenous access should be established with normal saline initial bolus of 10-15 ml/kg (prior to extrication if possible) 5. Carefully monitor for dysrhythmias or signs of hypokalemia before and immediately after release of pressure and during transport. Continued resuscitation with normal saline (500-1000 cc/hr for adults, 10 cc/kg/hr for children) b. Rapid extrication and evacuation to a definitive care facility (trauma center preferred) 2. A patient with a crush injury may initially present with very few signs and symptoms Therefore, maintain a high index of suspicion for any patient with a compressive mechanism of injury 3. Continue fluid resuscitation through extrication and transfer to hospital Pertinent Assessment Findings 1. Evaluation for fractures and potential compartment syndrome development (neurovascular status of injured extremity) 3. Revision Date September 8, 2017 200 Extremity Trauma/External Hemorrhage Management Aliases None noted Patient Care Goals 1. Minimize pain and further injury as a result of potential fractures or dislocations Patient Presentation Inclusion Criteria 1. Potential extremity fractures or dislocations Exclusion Criteria No recommendations Patient Management Assessment 1. Degree of bleeding/blood loss with assessment of the color of the blood (venous or arterial) and whether it is pulsatile or not Treatments and Interventions (also, see protocol diagram below) 1. If the bleeding site is amenable to tourniquet placement, apply tourniquet to extremity 1. Tourniquet should be placed 2-3 cm proximal to wound, not over a joint, and tightened until bleeding stops and distal pulse is eliminated.
Syndromes
- Aging
- What other symptoms do you have?
- Treatment with hormones
- Tumors that release a hormone called hCG
- Spread of the tumor into surrounding areas
- Fainting or feeling light-headed
- Brain aneurysm clips

American College of Obstetricians and Gynecologists Committee on Obstetric Practice Magnesium sulfate use in obstetrics medicine cheap generic actonel uk. American College of Obstetrics and Gynecologists Task Force on Hypertension in Pregnancy treatment 7th feb bournemouth buy actonel discount. Emergent therapy for acute-onset medications list purchase genuine actonel on-line, severe hypertension during pregnancy and the postpartum period symptoms juvenile rheumatoid arthritis 35 mg actonel for sale. Early standardized treatment of critical blood pressure elevations is associated with reduction in eclampsia and severe 158 maternal morbidity medications resembling percocet 512 generic actonel 35 mg with mastercard. Revision Date September 8 treatment renal cell carcinoma buy actonel 35mg otc, 2017 159 Obstetrical and Gynecological Conditions Aliases None noted Patient Care Goals 1. Recognize serious conditions associated with hemorrhage during pregnancy even when hemorrhage or pregnancy is not apparent. Provide adequate resuscitation for hypovolemia Patient Presentation Inclusion Criteria 1. Maternal age at pregnancy may range from 10 to 60 years of age Exclusion Criteria 1. Abruptio placenta: Occurs in third trimester of pregnancy; placenta prematurely separates from the uterus causing intrauterine bleeding a. Intermittent pelvic pain (uterine contractions) with vaginal bleeding Patient Management Assessment 1. Disposition transport to closest appropriate receiving facility Patient Safety Considerations 1. Patients in third trimester of pregnancy should be transported on left side or with uterus manually displaced to left if hypotensive 2. Do not place hand/fingers into vagina of bleeding patient except in cases of prolapsed cord or breech birth that is not progressing Notes/Educational Pearls Key Considerations Syncope can be a presenting symptom of hemorrhage from ectopic pregnancy or causes of vaginal bleeding. Pregnancy, Childbirth, Postpartum and Newborn Care: A guide for essential practice (3rd edition). Revision Date September 8, 2017 162 Respiratory Airway Management (Adapted from an evidence-based guideline created using the National Prehospital Evidence-Based Guideline Model Process) Aliases Asthma, upper airway obstruction, respiratory distress, respiratory failure, hypoxemia, hypoxia, hypoventilation, foreign body aspiration, croup, stridor, tracheitis, epiglottitis Patient Care Goals 1. Provide necessary interventions quickly and safely to patients with the need for respiratory support 4. Identify a potentially difficulty airway in a timely fashion Patient Presentation Inclusion Criteria 1. Children and adults with signs of severe respiratory distress/respiratory failure 2. Patients in whom oxygenation and ventilation is adequate with supplemental oxygen alone, via simple nasal cannula or face mask Patient Management Assessment 1. Signs of a difficult airway (short jaw or limited jaw thrust, small thyromental space, upper airway obstruction, large tongue, obesity, large tonsils, large neck, craniofacial abnormalities, excessive facial hair) Treatment and Interventions 1. Maintain airway and administer oxygen as appropriate with a target of achieving 94 98% saturation b. This is especially important in children since endotracheal intubation is an infrequently performed skill in this age group and has not been shown to improve outcomes 4. Other indications may include potential airway obstructions, severe burns, multiple traumatic injuries, altered mental status or loss of normal protective airway reflexes c. Monitor clinical signs, pulse oximetry, cardiac rhythm, blood pressure, and capnography for the intubated patient d. Video laryngoscopy may enhance intubation success rates, and should be used when available. Consider using a bougie, especially when video laryngoscopy is unavailable and glottic opening is difficult to visualize with direct laryngoscope 5. Continuously monitor placement with waveform capnography during treatment and transport c. Continuously secure tube manually until tube secured with tape, twill, or commercial device i. Note measurement of tube at incisors or gum line and monitor frequently for tube movement/displacement ii. Cervical collar and/or cervical immobilization device may help reduce neck movement and risk of tube displacement d. Ventilate with minimal volume to see chest rise, approximately 6 7 mL/kg ideal body weight 2. Gastric decompression may improve oxygenation and ventilation, so it should be considered when there is obvious gastric distention 7. When patients cannot be oxygenated/ventilated effectively by previously mentioned interventions, the provider should consider cricothryoidotomy if the risk of death for not escalating airway management seems to outweigh the risk of a procedural complication 8. Transport to the closest appropriate hospital for airway stabilization when respiratory failure cannot be successfully managed in the prehospital setting Patient Safety Considerations 1. When compared to the management of adults with cardiac arrest, paramedics are less likely to attempt endotracheal intubation in children with cardiac arrest. This is an important adjunct in the monitoring of patients with respiratory distress, respiratory failure, and those treated with positive pressure ventilation. Contraindications to these non-invasive ventilator techniques include intolerance of the device, severely impaired consciousness, increased secretions inhibiting a proper seal, or recent gastrointestinal and/or airway surgery 4. Appropriately-sized masks should completely cover the nose and mouth and maintain an effective seal around the cheeks and chin b. Ventilation should be delivered with only sufficient volume to achieve chest rise c. When advanced airway is in place, ideally ventilations should be on upstroke between two chest compressions ii. In adults who are not in cardiac arrest, ventilate at rate of 12 breaths per minute iii. In children, ventilating breaths should be delivered over one second, with a two second pause between breaths (20 breaths/minute) in children 5. In addition to preoxygenation, apneic oxygenation (high-flow oxygen by nasal cannula) may prolong the period before hypoxia during an intubation attempt d. Positive pressure ventilation after intubation can decrease preload and subsequently lead to hypotension consider providing vasopressor support for hypotension. Appropriate attention should be paid to adequate preoxygenation to avoid peri intubation hypoxia and subsequent cardiac arrest f. Prompt suctioning of soiled airways before intubation attempt may improve first pass success g. Less optimal methods of confirmation include bilateral chest rise, bilateral breath sounds, and maintenance of adequate oxygenation. Visualization with video laryngoscopy, when available, may assist in confirming placement when unclear due to capnography failure or conflicting information. This is especially true for children since pediatric intubation is an infrequently utilized skill for many prehospital providers. Video laryngoscopy may be helpful, if available, to assist with endotracheal intubation 6. Verification of endotracheal tube placement by prehospital providers: is a portable fiberoptic bronchoscope of value Intubation confirmation techniques associated with unrecognized non-tracheal intubations by pre-hospital providers. The efficacy of pediatric advanced life support training in emergency medical service providers. First responder performance in pediatric trauma: a comparison with an adult cohort. Low-fractional oxygen concentration continuous positive airway pressure is effective in the prehospital setting. Prehospital oral endotracheal intubation by rural basic emergency medical technicians. Prehospital emergency endotracheal intubation using the Bonfils intubation fiberscope. Effect of emergency medical technician-placed Combitubes on outcomes after out-of-hospital cardiopulmonary arrest. Ventilatory muscle support in respiratory failure with nasal positive pressure ventilation. Assessment of the speed and ease of insertion of three supraglottic airway devices by paramedics: a manikin study. Randomized trial of endotracheal tube versus laryngeal mask airway in simulated prehospital pediatric arrest. The impact of prehospital continuous positive airway pressure on the rate of intubation and mortality from acute out-of-hospital respiratory emergencies. Prehospital endotracheal intubation for severe head injury in children: a reappraisal. The effect of paramedic rapid sequence intubation on outcome in patients with severe traumatic brain injury. A prospective multicenter evaluation of prehospital airway management performance in a large metropolitan region. Pediatric major resuscitation-respiratory compromise as a criterion for mandatory surgeon presence. Analysis of preventable pediatric trauma deaths and inappropriate trauma care in Montana. Emergency scene endotracheal intubation before and after the introduction of a rapid sequence induction protocol. Populations at risk for intubation nonattempt and failure in the prehospital setting. Effect of out-of hospital pediatric endotracheal intubation on survival and neurological outcome: a controlled clinical trial. Comparison of three different methods to confirm tracheal tube placement in emergency intubation. Feasibility of laryngeal mask airway use by prehospital personnel in simulated pediatric respiratory arrest. Evolution of the extraglottic airway: a review of its history, applications, and practical tips for success. Prehospital and emergency department verification of endotracheal tube position using a portable, non-directable, fiberoptic bronchoscope. Expected difficult tracheal intubation: a prospective comparison of direct laryngoscopy and video laryngoscopy in 200 patients. A comparison of GlideScope videolaryngoscopy and direct laryngoscopy for nasotracheal intubation in children. The assessment of four different methods to verify tracheal tube placement in the critical care setting. A randomized controlled trial of capnography in the correction of simulated endotracheal tube dislodgement. The effect of a rapid sequence induction protocol on intubation success rate in an air medical program. Intubation success rates improve for an air medical program after implementing the use of neuromuscular blocking agents. Paramedic King Laryngeal Tube airway insertion versus endotracheal intubation in simulated pediatric respiratory arrest. Verification of endotracheal tube placement following intubation, Prehosp Emerg Car. A comparison of GlideScope video laryngoscopy versus direct laryngoscopy intubation in the emergency department. Comparison of a conventional tracheal airway with the Combitube in an urban emergency medical services system run by physicians. Can an airway assessment score predict difficulty at intubation in the emergency department Apneic oxygenation may not prevent severe hypoxemia during rapid sequence intubation: a retrospective helicopter emergency medical service study. Before and after establishment of a rapid sequence intubation protocol for air medical use. Endotracheal intubation and esophageal tracheal Combitube insertion by regular ambulance attendants: a comparative trial. The effectiveness of out-of-hospital use of continuous end-tidal carbon dioxide monitoring on the rate of unrecognized misplaced intubation within a regional emergency medical services system. Utility of a novel quantitative handheld microstream capnometer during transport of critically ill children. Prehospital endotracheal intubation for trauma does not improve survival over bag-valve-mask ventilation. The assessment of three methods to verify tracheal tube placement in the emergency setting. Noninvasive ventilation in the pediatric intensive care unit for children with acute respiratory failure. A comparison of the GlideScope video laryngoscope and standard direct laryngoscopy in children with immobilized cervical spine. Failed prehospital intubations: an analysis of emergency department courses and outcomes.
35 mg actonel overnight delivery. My health conditions: Life with Long QT Syndrome..
References
- Kantarjian HM, O'Brien S, Smith TL, et al. Results of treatment with hyper- CVAD, a dose-intensive regimen, in adult acute lymphocytic leukemia. J Clin Oncol. 2000;18(3):547-561.
- Lisk D, Grotta JC, Lamki LM, et al. Should hypertension be treated after acute stroke? A randomized controlled trial using single photon emission computed tomography. Arch Neurol 1993;50:855-62.
- Singh JKR, Kalyanpur A: iSmall bowel feces signi: A CT sign in small bowel obstruction. Indian J Radiol Imaging 16:71, 2006.
- Onesti ST, Wisniewski T, Post KD. Clinical versus subclinical pituitary apoplexy: presentation, surgical management, and outcome in 21 patients. Neurosurgery. 1990;26:980-986.
- Massera F, Robustellini M, Della Pona C, et al. Predictors of successful closure of open window thoracostomy for postpneumonectomy empyema. Ann Thorac Surg 2006; 82: 288-292.
- Fieschi C, Argentino C, Lenzi GL, et al. Clinical and instrumental evaluation of patients with ischemic stroke within the first six hours. J Neurol Sci 1989;91:311-21.
- Osborn DJ, Kaufman MR, Dmochowski RR: Complications after surgery for stress urinary incontinence, Urologicke Listy 4:39n44, 2013.