Jodi A. Antonelli, MD
- Assistant Professor Department of Urology
- University of Texas Southwestern Medical Center Dallas, Texas
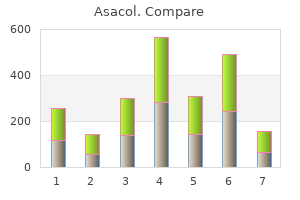
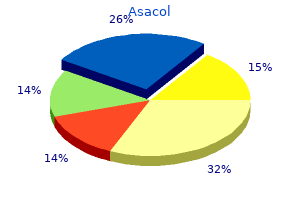
Sixty percent of all pediatric cases Neuroblastoma is an embryonal neoplasm of the are caused by Neisseria meningitidis treatment norovirus 800mg asacol fast delivery. Streptococcus sympathetic nervous system and can be located anywhere pneumoniae is the second most common microorganism there is nervous tissue medicine 1700s generic asacol 800 mg free shipping. More than 90% of children with neurob group B beta-hemolytic streptococci are the most com lastoma have increased catecholamines in their urine symptoms 7 days pregnant discount asacol 400 mg. Retinoblastoma is a rare congenital eye neoplasm the hallmark of viral meningitis consists of a mono that has both hereditary and nonhereditary forms symptoms for pink eye purchase asacol 800 mg. Ninety percent of neural tube defects are among the top ten causes of death in children treatment 1st degree burns discount asacol 400mg free shipping. Anencephaly is the result of premature closure of chronic medicine evolution buy asacol 800mg with mastercard, progressive vascular stenosis of the circle of the sutures of the skull. Environmental influences play an important role in result of cranial radiation therapy. Encephalocele is the result of herniation of the brain and meninges through a defect of the lower vertebrae. Describe the types of brain tumors in children and characterize their presentation. The cause of most childhood bacterial meningitis is Study pages 419 and 421-423; refer to Figures 16-7 Neisseria meningitidis. The prognosis for an individual with Brain tumors are the most common solid tumors in meningomyelocele depends on the level and extent childhood and the second most common neoplasms in of the defect. Infratentorial tumors often cause increased intracranial pressure because of a mass block 10. Signs include early morning and resolve naturally because the neurons and the vomiting with neither nausea nor headache, lethargy, neuronal pathways are constantly maturing. Supratentorial tumors frequently cause localized neurologic symptoms, such as truncal ataxia, 11. Aspirin administration during a viral illness has symptoms of headache, lethargy, and stiff neck after several days of treatment for otitis been associated with media may be showing findings consistent with syndrome, which is considered to be a(n). Early morning vomiting without associated with premature closure of the sutures of the skull. Focal neurologic findings such as ataxia may be associated with a(n) fossa brain tumor. He has a very deep, dime-sized sacral dimple and highly fissured skin over his lower sacral spine. What would you expect the radiographs to reveal, and what would be the next step/s Organs that respond to a particular hormone are called: and describe the regulation of hormone a. Classify the types of hormones, their receptors, and proposed mechanisms of action. The renin-angiotensin-aldosterone system begins to function when renin is secreted by the: 15. Describe hormone receptors as recognizing and signaling mechanisms for hormonal action. Water soluble hormones, which include the protein hormones and epinephrine or norepinephrine, cannot cross the cell membrane and interact or bind with receptors located in or on the cell membrane. Once inside the cytosol, some hormones bind to receptor molecules in the cytoplasm and then diffuse into the nucleus. Hormones without cytoplasmic receptors diffuse directly into the nucleus and bind with an acceptor molecule. Once activated by hormones, the first messengers, the receptor likely binds to specific sites on the chro matin of the target cell. After studying this chapter, the learner will be able to Study pages 449-450 and Table 18. Identify the mechanisms causing hormonal occur, they are usually related to abnormal antidiuretic hor alterations. This state leads to serum cell receptors decreases, their receptor/hormone affinity hyponatremia and hyposmolality. This action ders develop if there is inadequate synthesis of second increases their permeability to water through the action of messengers, acquired defects in postreceptor signaling, aquaporin, which is a water channel protein. Hyponatremia altered synthesis of intracellular proteins of enzymes, or suppresses renin and aldosterone secretion, thus decreasing nuclear co-regulator dysfunction. Chapter 18 Alterations of Hormonal Regulation Thirst, impaired taste, anorexia, dyspnea on exertion, of infarction increases during pregnancy. The primary fatigue, and dulled consciousness occur when the serum pathologic mechanism in postpartum pituitary infarction, sodium level falls from 140 to 130 mEq/L. Vomiting and or Sheehan syndrome, is vasospasm of the artery supply abdominal cramps occur with a drop in sodium level ing the anterior pituitary. With a serum sodium level occurs, which expands the pituitary within the fixed con below 113 mEq/L, confusion, lethargy, muscle twitching, fines of the sella turcica. Symptoms usually resolve with blood supply to the pituitary and promotes hypofunction. If all hormones are absent, a condition termed hyponatremia by administration of hypertonic saline, and panhypopituitarism develops. These diabetes insipidus: a neurogenic or central form, a nephro deficiencies do not generally develop in adults. This diabetes is generally related to dis In cases of hypopituitarism, the underlying disorder orders and drugs that damage the renal tubules or inhibit the should be corrected as quickly as possible. The psychogenic form cortisol replacement therapy may need to be initiated and is caused by an extremely large volume of fluid intake. Sex steroid replacement may be required, the clinical manifestations of diabetes insipidus are depending on the needs and desires of the individual. These signs and symptoms Pituitary adenomas that cause hyperpituitarism are include polyuria, nocturia, continuous thirst, polydipsia, usually benign, slow-growing tumors. Visual changes produced by pressure on the optic Individuals who have excessive urine output and low chiasma include visual field impairments. Acromegaly as either hypofunctions or hyperfunctions of the occurs in adults after epiphyseal closure has occurred and gland. If untreated, acromegaly is associated with a decreased life expectancy because of a Anterior pituitary hypofunction may develop from greater occurrence of hypertension, congestive heart failure, infarction of the gland, removal or destruction of the gland, diabetes mellitus, and colon or lung cancer. Hyperfunction of the anterior pitui involves periosteal vertebral growth and enlargement of tary generally involves an adenoma composed of secretory the facial bones and the bones of the hands and feet. An adenoma may cause hypersecretion of associated growth results in protrusion of the lower jaw and the hormone it produces and hyposecretion of another hor forehead. Because somatomedins stimulate cartilaginous mone because of the compressive effects of the tumor. The pituitary gland may be susceptible growth, nerves may be entrapped and damaged, which may to necrosis because its blood supply through the portal be manifested by weakness, muscular atrophy, foot drop, and system is already partially deoxygenated. In men, as headache, seizure activity, and visual disturbances may hyperprolactinemia causes hypogonadism and erectile develop. Dopaminergic agonists are the treatment of impaired carbohydrate tolerance and increased metabolic choice for prolactinomas. Describe the disorders of hyperthyroidism; note In children and adolescents whose epiphyseal plates the progressive states of severity. Specific secretion while minimizing damage to appropriately secret diseases of primary hyperthyroidism include Graves ing portions of the pituitary. Surgery and radiation therapy disease, toxic multinodular goiter, and solitary toxic are used, depending on the extent of tumor growth. Skeletal growth the antibody binds to the plasma membrane and initiates is stunted and the child will be dwarfed with short thyroid hyperplasia of the gland (goiter), vascularity, and limbs if not treated. Ophthalmopathy is charac Mental retardation in cretins is a function of the sever terized by edema of the orbital contents, exophthalmos, ity of hypothyroidism and the delay before initiation and extraocular muscle weakness that sometimes leads to of thyroxine treatment. Treatment consists of a combination of radioac high birth weight, hypothermia, delay in passing meco tive iodine, surgery, or antithyroid drugs. Thyrotoxic crisis (thyroid storm) is a rare but a There is a high probability of normal growth and intel dangerous worsening of the thyrotoxic state; death can lectual function if treatment is started immediately after occur within 48 hours without appropriate treatment. This condition occurs most often in individuals who Thyroid carcinoma is the most common endocrine have undiagnosed or partially treated severe hyperthy malignancy but is still relatively rare. The most consist roidism and who are subjected to excessive stress from ent causal risk factor for the development of thyroid other causes. The systemic symptoms of thyrotoxic crisis cancer is exposure to ionizing radiation. Changes in voice include hyperthermia, tachycardia, high-output heart and swallowing and difficulty in breathing are related to failure, agitation or delirium, and nausea, vomiting, or impingement of tumor growth on the esophagus or tra diarrhea contributing to fluid depletion. Primary causes include congenital defects cemia and decreased serum phosphate levels. The individual develops a low meta Chronic hypercalcemia may be associated with kidney bolic rate with this disorder. It is characterized by swelling of the hand, Long-term management of hypercalcemia uses drugs face, feet, and periorbital tissues. Definitive Myxedema coma is a medical emergency associated treatment requires the surgical removal of the hyperplas with severe hypothyroidism. Hypocalcemia lowers the threshold for the diagnosis of diabetes is based on several obser nerve and muscle excitation. Muscle spasms, hyperreflexia, vations: (1) more than one elevated fasting plasma clonic-tonic seizures, laryngeal spasms, and, in severe cases, glucose value; (2) elevated plasma glucose values in death from asphyxiation are seen with hypocalcemia. In individuals with poorly controlled diabetes, cataracts, bone deformities, and basal ganglia calcifica increases in the quantities of glycosylated hemoglobins tions do not respond to the correction of hypocalcemia, are seen. Once a hemoglobin molecule is glycosylated, but the other symptoms of hypocalcemia are reversible. Other signs and symptoms are weight loss, fatigue, prolonged wound healing, visual changes, neuropathies, 7. Describe the similarities and differences between and formation of atherosclerosis. Study pages 458, 459 and 461-464; refer to Figures Oral medication may be needed for optimal management 18-11 and 18-12, and Tables 18-3 through 18-6. Insulin is required in type 1 diabetes the four major categories of diabetes mellitus are and also may be required in the treatment of some indi absolute insulin deficiency (type 1 diabetes mellitus), viduals with type 2 diabetes. Exercise is an important insulin resistance with an insulin secretory deficit (type aspect of treatment for the individual with type 2 diabe 2 diabetes mellitus), other types of diabetes mellitus, and tes. Identify the acute complications of diabetes 70-110 mg/dL when there has been no caloric intake mellitus; describe the features of each. Diabetic conditions exist whenever: Study page 465; refer to Figure 18-13 and Table 18-7. Describe the etiology, pathogenesis, and Hyperaldosteronism is characterized by excessive manifestations of hyperfunction and aldosterone secretion by the adrenal glands. Cushing disease refers specifically to pituitary Conn disease, or primary hyperaldosteronism, dependent hypercortisolism. Cushing-like syndrome also presents a clinical picture of hypertension, hypoka may develop as a result of the exogenous administration lemia, renal potassium wasting, and neuromuscular of cortisone. The most common cause of primary neoplasms account for many cases of hypercorticoad aldosteronism is the benign, single adrenal adenoma, renalism. Cushing syndrome (chronic hypercortisolism) followed by multiple tumors and idiopathic hyperplasia refers to excessive levels of circulating cortisol caused of the adrenals. Hypertension and hypokalemia are the essential mani Most of the clinical signs and symptoms of Cushing are festations of hyperaldosteronism. The most common feature is ally results from increased intravascular volume and the accumulation of adipose tissue in the trunk, facial, altered serum sodium concentrations. Loss of the protein matrix in Treatment of hypertension and hypokalemia consists bone leads to osteoporosis and accompanying pathologic of correction of any underlying causal abnormalities. If fractures, vertebral compression fractures, bone and back an aldosterone-secreting adenoma is present, it must be pain, kyphosis, and reduced height.
Fever strips and pacifier thermometers are A young child with a fever will often appear not recommended because they do not give ill medicine zoloft buy generic asacol 800mg line. If your child is over six months old medicine daughter lyrics buy asacol 400 mg online, call Health Links-Info Sante (Winnipeg What is the best way to 788-8200 medicine 1900s spruce cough balsam fir cheap asacol 400 mg on line, toll-free 1-888-315-9257) asthma medications 7 letters cheap 400 mg asacol fast delivery, your public health nurse or your doctor take a temperature This will help straighten the ear canal medicine ethics discount asacol 800mg amex, and make a clear path inside the ear to the ear How do you take a drum symptoms 5 days post embryo transfer order asacol american express. If your child is older, the child can sit on your lap, with one arm behind your back. A quiet activity such as breastfeeding, or singing or telling a story to your child may help keep the child still. When your child has a fever, medication is not always needed to reduce the temperature. In fact, the best reason for giving your child Medication: medication is not to reduce fever but to Acetaminophen is the best drug for relieve the associated aches and pains. Shivering down in one-and-a-half to two hours produces more body heat, causing after taking acetaminophen. Keep rises again and then the medication your child in light clothing: diapers or may have to be repeated. This allows not to exceed the recommended doses the extra heat to escape from your in 24 hours. Protect the delicate inner workings of your ears with practical advice from the experts. Your middle ears are dead air spaces, connected to the outer world only by the Eustachian tubes running to the back of your throat. If you fail to increase the pressure in your middle ears to match the pressure in your outer and inner ears, the result is painful middle-ear barotrauma, the most common pressure-related ear injury. Each has a kind of one-way valve at its lower end called the "Eustachian cushion, " which prevents contaminants in your nose from migrating up to your middle ears. Opening the tubes, to allow higher-pressure air from your throat to enter your middle ears, normally requires a conscious act. In fact, you equalize your ears many times a day without realizing it, by swallowing. Oxygen is constantly absorbed by the tissues of your middle ear, lowering the air pressure in those spaces. When you swallow, your soft palate muscles pull your Eustachian tubes open, allowing air to rush from your throat to your middle ears and equalize the pressure. Why You Must Equalize If you dive without equalizing your ears, you can experience painful and damaging middle-ear barotrauma. Mucus begins to fill your Eustachian tubes, making it difficult to equalize your ears if you try. Small blood vessels in your eardrums may expand or break, causing bruising which will last up to three weeks. Your Eustachian tubes are now locked shut by pressure, making equalization impossible. If you are lucky, blood and mucus is sucked from surrounding tissues and begins to fill your middle ear. Pain subsides, replaced by a feeling of fullness in your ears which will remain for a week or more until the fluid is reabsorbed by your body. The sudden sensation of cold against your balance mechanism, your vestibular canals, may cause vertigo, especially if only one eardrum breaks. Suddenly, the world is spinning around you, though the sensation will probably stop when your body warms up the water in your middle ear. Or, if you try to equalize by blowing hard and long against pinched nostrils, you may rupture the "round window" membrane between your middle and inner ears. How To Equalize All methods for equalizing your ears are simply ways to open the lower ends of your Eustachian tubes, so air can enter. This is the method most divers learn: Pinch your nostrils (or close them against your mask skirt) and blow through your nose. The resulting overpressure in your throat usually forces air up your Eustachian tubes. And blowing against a blocked clearing methods utilize the muscles of the nose raises your internal fluid pressure, throat to open the tubes. Unfortunately, including the fluid pressure in your inner ear, the Valsalva maneuver that most divers which may rupture your "round windows. Swallowing pulls open your Eustachian tubes while the movement of your tongue, with your nose closed, compresses air against them. A combination of Valsalva and Toynbee: while closing your nostrils, blow and swallow at the same time. However, if a diver does not close the back of your throat as if straining to equalize early or often enough, the lift a weight. Tense the the middle ears, which do not equalize, so muscles of the soft palate and the throat barotrauma results. Even worse, blowing while pushing the jaw forward and down as if too hard during a Valsalva maneuver can starting to yawn. These muscles pull the rupture the round and oval windows of the Eustachian tubes open. Practice Makes Perfect Divers who experience difficulty equalizing may find it helpful to master several techniques. Many are difficult until practiced repeatedly, but this is one scuba skill you can practice anywhere. For example, a descent of six feet from the surface will compress your middle ear space by 20 percent and produce pain. Several hours before your dive, begin gently equalizing your ears every few minutes. The lesson here is to pre-pressurize only if it seems to help you, and to pressurize gently. Air tends to rise up your Eustachian tubes, and fluid-like mucus tends to drain downward. Pulling yourself down an anchor or mooring line helps control your descent rate more accurately. Without a line, your descent rate will probably accelerate much more than you realize. A line also helps you stop your descent quickly if you feel pressure, before barotrauma has a chance to occur. Equalize often, trying to maintain a slight positive pressure in your middle ears. Your Eustachian tubes are probably locked shut by pressure differential, and the only result will be barotrauma. Both tobacco smoke and alcohol irritate your mucus membranes, promoting more mucus that can block your Eustachian tubes. Water up your nose can irritate your mucus membranes, which then produce more of the stuff that clogs. Other Ear Problems Middle-Ear Barotrauma on Ascent, or Reverse Squeeze What happens: Pressure must be released from your middle ear as you ascend, or the expanding air will bulge and even break your eardrums. Normally, expanding air escapes down your Eustachian tubes, but if the tubes are blocked with mucus at depth (usually the result of poor equalizing on descent, diving with a cold or relying on decongestants that wear off at depth), barotrauma can result. Some divers also feel vertigo from the unusual pressure on their balance mechanism. What to do: Sometimes one of the equalizing techniques used on descent will clear your ears on ascent. Ascend as slowly as your air supply allows, remembering that the last 30 feet will be most difficult. What you feel: o Deafness: Hearing loss can be complete, instant and permanent, but divers usually lose just the higher frequencies. What to do: Abort the dive and go as soon as possible to an ear, nose and throat specialist with experience treating divers. Inner-ear injuries are tricky and require prompt, correct treatment from a specialist. Your eardrum bulges outward, and increasing pressure in the surrounding tissues fills the canal with blood and fluid. What to do: Keep your outer ear clear, which can be difficult for divers with exospores (see pg. These are hard, bony growths in the ear canal that can trap dirt and wax and even grow so big they completely block the ear canal. It will reduce the flow of water to your ears, and what does reach them will be warmer. Some divers do, but they are taking a serious risk of permanent loss of hearing or, even worse, balance control. Vertigo, the sense that the world is spinning around you, is a common symptom of middle-ear or inner-ear injury. If vertigo happens under water, you may not be able to tell which way is up and panic. Damage the vestibular canals on the other side too, and you could be unable to drive a car, much less dive. In both cases, your brain interprets unequal stimulation of your vestibular systems as movement. This type of vertigo disappears with the unequal stimulation, fortunately, and leaves no after-effects. Direct observation of the structures of the fundus through an effective ophthalmoscope may show disease of the eye itself or may reveal abnormalities indicative of disease elsewhere in the body. Among the most important of these are vascular changes due to diabetes or hypertension and swelling of the optic nerve head due to papilledema or optic neuritis. In this sense, the eye serves as a window through which many valuable clinical evaluations may be made. When a preliminary diagnosis of an imminently dangerous eye condition, such as acute glaucoma or retinal detachment, is made by the examiner, prompt referral to an ophthalmologist may prevent irreversible damage. Or, when distressing but less urgent conditions, such as visual impairment due to cataract or vitreous floaters are recognized, the patient can be reassured and referred. A Macula J Cornea B Vitreous Humor K Ciliary Body Welch Allyn ophthalmoscopes, with their bright, white halogen C Sclera L Zonule (Suspensory Ligament) illumination coupled with their patented optical systems, allow D Choroid M Conjuctiva the examiner to clearly see these important structures of the eye E Retina N Lens to aid in making the correct diagnosis. F Ora Serrata O Hyaloid Canal G Canal of Schlemm P Central Retinal Vein Little has been written giving the practitioner detailed instructions H Anterior Chamber Q Optic Nerve I Iris R Central Retinal Artery on the use of the ophthalmoscope. The following pages in this section contain information on ophthalmoscopes, how to conduct an ophthalmic exam, and what to look for while examining the eye. The optics system converges optical system, allowing the axis of illumination to be coincidental the light to a point at the cornea, which allows the practitioner easy with the axis of vision into the retina, thereby eliminating annoying Front Rubber surface brow rest entry into small pupils. The illumination pathway then diverges to shadows and facilitating examination through virtually any size pupil mirror the retina, illuminating a very wide area of the fundus. The fundus and interior anatomy of the eye are system enables the operator to view the illuminated area on virtually viewed with precision and clarity. Crossed Lens linear selection the same axis, thus creating the widest field of view attainable in polarizing disc undilated ophthalmoscopy. The this helps compensate for patient or examiner refractive error, the Aperture Dynamic Focusing Wheel adjusts the focus in a continuous, smooth position of the ophthalmoscope and the changes in viewing require selection dial action for more precise control and optimum view. This helps com ments necessitated by focusing on different points within the eye. Dynamic On/Off switch pensate for patient or examiner refractive error, the position of the PanOptic Soft Grip Focusing Wheel and rheostat ophthalmoscope and the changes in viewing requirements necessitated Some coaxial models offer an additional crossed linear polarizing control by focusing on different points within the eye. When used in conjunction with available apertures, the coaxial the patient side eyecup helps the practitioner establish and maintain the ophthalmoscope yields 15 possible apertures. It also serves as the pivoting point for leverage in panning around the the illuminated lens dial enables the practitioner to check the lens being retina.
Order 800 mg asacol with visa. Chronic Nausea | My Experience and Solution: ALifeLearned.
It is physically medicine 5 rights order asacol now, emotionally medications you can take while pregnant for cold generic 400mg asacol visa, and intellectually demanding medicine expiration purchase asacol 800 mg mastercard, and requires longitudinally-concentrated effort on the part of the resident symptoms type 1 diabetes purchase asacol 800mg otc. As residents gain experience and demonstrate growth in their ability to care for patients medicine dispenser discount asacol 800mg mastercard, they assume roles that permit them to exercise those skills with greater independence adhd medications 6 year old generic asacol 400 mg online. Definition of Discipline Neurological surgery is a discipline of medicine and the specialty of surgery that provides operative and nonoperative management. The required length of a neurological surgery residency is 72 months in a curriculum under the control of the neurological surgery program director. Programs can be approved for up to 84 months of neurological surgery training, 72 months of which are for clinical and didactic education and 12 months of research or advanced training. The resident must complete all years of education for which the program is accredited. Programs that extend the residency beyond 72 months must present a clear educational rationale consonant with the program requirements and the objectives of the residency. The program director must obtain the approval of the sponsoring institution and the Review Committee prior to implementation and at each subsequent accreditation review of the program. Before entry into the program, each resident must be notified in writing of the required length of the program. This period may not be changed for a particular resident during his or her program unless there is a significant break in his or her education, or the resident needs remedial education. Residents must have a minimum of three months of structured education in general patient care to include rotations in surgery, critical care, trauma, and other related rotations as determined by the program director. The program must provide 42 months of clinical neurological surgery at the sponsoring institution or one of its approved participating sites. A minimum of 21 months of neurological surgery education must occur at the sponsoring institution. The remaining time not devoted to clinical neurology and neurological surgery should be spent in the study of the basic sciences, neuroradiology, neuropathology, or other appropriate subject matter related to the neurosciences. These topics should be agreed upon by individual residents and the program director. The program director should consult the American Board of Neurological Surgery for certification requirements concerning any training conducted outside the approved sites of the program. The program must provide residents with experience in direct and progressively responsible patient management experience as they advance through training. Residents must spend a 12-month period of time as chief resident on the neurological surgery clinical service in the sponsoring institution or its approved participating sites. Sponsoring Institution One sponsoring institution must assume ultimate responsibility for the Neurological Surgery 3 193 program, as described in the Institutional Requirements, and this responsibility extends to resident assignments at all participating sites. The sponsoring institution and the program must ensure that the program director has sufficient protected time and financial support for his or her educational and administrative responsibilities to the program. The sponsoring institution for a neurological surgery program must be in a single geographic location. The institution must demonstrate commitment to the program in terms of financial and academic support, including timely appointment of a permanent department or division chairperson of neurological surgery. An integrated site must function as a single neurological surgery service with the sponsoring institution. The program director must demonstrate to the Review Committee that the clinical service operates as a single unit in the assignment of residents and their faculty supervisors, the formulation of call schedules, and the convening of teaching conferences and related educational activities. A participating site functions as a separate neurological surgical service with a local training director under the direction of the program director and should be sufficiently close to the sponsoring institution to ensure Neurological Surgery 4 194 peer interaction and regular attendance at joint conferences and other activities. There must be a single program director with authority and accountability for the operation of the program. The program director should continue in his or her position for a length of time adequate to maintain continuity of leadership and program stability. This record must include all procedures in which the neurological surgery resident was either resident surgeon or assistant and must be signed by both the resident and the program director as a statement of its accuracy. Conferences must be coordinated among training program sites to allow attendance by a majority of staff and residents. The physician faculty must have current certification in the specialty Neurological Surgery 8 198 by the American Board of Neurological Surgery, or possess qualifications acceptable to the Review Committee. This individual must be responsible for the education of the residents and also will supervise the educational activities of other neurological surgeons relating to resident education at that site. The physician faculty must possess current medical licensure and appropriate medical staff appointment. The faculty must establish and maintain an environment of inquiry and scholarship with an active research component. Outpatient Facilities Residents must have available appropriate outpatient facilities, clinic, and office space for training purposes in the regular preoperative evaluation and postoperative follow-up for cases for which the resident has responsibility. Recognizing the nature of the specialty of neurological surgery, it is unlikely that a program can mount an adequate educational experience for neurological surgery residents without approved training programs in related fields. Clinically oriented training programs in the sponsoring institution of the neurological surgery program should include accredited training programs in neurology, general surgery, internal medicine, pediatrics, and radiology. There should be clinical resources for the education of neurological surgery residents in anesthesiology, critical care, emergency medicine, endocrinology, ophthalmology, orthopedics, otolaryngology, pathology, and psychiatry. There shall be sufficient patients admitted each year to ensure that the resident participates in the care of patients suffering from the full spectrum of neurosurgical diseases. A program must demonstrate to the satisfaction of the Review Committee that it has both the volume of patients under neurological care and the breadth and depth of academic support to ensure that it may provide excellent neurological surgery training to residents. The volume of patients must be substantiated in part by a compilation of annual institutional operative data and resident operative data (including that from residents rotating on the service from other programs) provided in a fashion prescribed by the Review Committee. Within the total clinical facilities available to the training program, there should be a minimum of 500 major neurological surgery procedures per year per finishing resident. However, meeting this minimum number does not ensure accreditation of a training program. The presence within a given training program of this neurological surgery workload and the distribution of the surgical experience are equally important. For instance, the cases should be appropriately distributed among cranial, extracranial, spinal, and peripheral nerve surgical procedures and should represent a well-balanced spectrum of neurological surgery in both adults and children. This spectrum should include craniotomies for trauma, neoplasms, aneurysms, and vascular malformations; extracranial carotid artery surgery; transsphenoidal and stereotaxic surgery (including radiosurgery); pain management; and spinal procedures of a sufficient number and variety using modern techniques. During duty hours residents must be provided with adequate sleeping, lounge, and food facilities. Support services must be such that the resident does not spend an inordinate amount of time in noneducational activities that can be discharged properly by other personnel. Medical Information Access Residents must have ready access to specialty-specific and other appropriate reference material in print or electronic format. The Review Committee will review the selection process of residents and seek evidence that the program evaluates the progression of the residents during training. Where there is demonstrated excellence in providing educational experience for the residents, as determined by the Review Committee, a program may be authorized to enroll more than one resident per year. The ability to do so does not depend on any multiplication of the minimum requirements as established by the Program Requirements for Graduate Medical Education in Neurological Surgery. The number of residents at each year of training in a given program shall not exceed the number approved by the most recent accreditation review of that program. A new resident may be appointed to fill a vacancy provided that there is no adverse impact on the existing resident staff. The program must provide the Review Committee with an explanation for the excess complement and its plan for resolution to normal complement. A program director must provide timely verification of residency education and summative performance evaluations for residents who leave the program prior to completion. Programs must notify the Review Committee when they sponsor or participate in any clinical fellowship taking place within sites participating in the program. This notification must occur before the commencement of such training and at each subsequent review of the program. If fellows so appointed will, in the judgment of the Review Committee, detract from the education of the regularly appointed residents, the accreditation status of the program may be adversely affected. Competency-based goals and objectives for each assignment at each educational level, which the program must distribute to residents and faculty annually, in either written or electronic form. Under appropriate supervision, this experience should include obtaining a complete history, conducting an examination, ordering (if necessary) and interpreting diagnostic studies, and arriving independently at a diagnosis and plan of management. Consonant with their skills and level of experience, residents should be actively involved in preoperative decision making and subsequent operative procedures under the supervision of the attending physician who has ultimate responsibility for the patient. Residents should similarly be actively involved in postsurgical care and follow-up evaluation of their patients to develop skills in assessing postoperative recovery, recognizing and treating complications, communicating with referring physicians, and developing the physician patient relationship. Preoperative interview and examination of patients already scheduled for a surgical procedure will not satisfy these requirements. This continuity of care must take precedence-without regard to the time of day, day of the week, number of hours already worked, or on-call schedules. At the same time, patients have a right to expect a healthy, alert, responsible, and responsive physician dedicated to delivering effective and appropriate care. Summative Evaluation the program director must provide a summative evaluation for each resident upon completion of the program. The program must document formal, systematic evaluation of the curriculum at least annually. If deficiencies are found, the program should prepare a written plan of action to document initiatives to improve performance in the areas listed in section V. The action plan should be reviewed and approved by the teaching faculty and documented in meeting minutes. Programs and sponsoring institutions must educate residents and faculty members concerning the professional responsibilities of physicians to appear for duty appropriately rested and fit to provide the services required by their patients. The program must be committed to and responsible for promoting patient safety and resident well-being in a supportive educational environment. The program director and institution must ensure a culture of professionalism that supports patient safety and personal responsibility. The sponsoring institution must provide adequate sleep facilities and/or safe transportation options for residents who may be too fatigued to safely return home. The program must demonstrate that the appropriate level of supervision is in place for all residents who care for patients. In some circumstances, supervision may include post-hoc review of resident-delivered care with feedback as to the appropriateness of that care. Neurological surgery residents practice across a diversity of care settings with varying degrees of primary patient responsibility. These situations vary from first call cross-coverage on the floors to possible interaction with a primary intensivist, pediatric, or hospitalist service. Peri-operative inpatient care must be further balanced with resident participation in the operating room. This must include the opportunity to work as a member of effective interprofessional teams that are appropriate to the delivery of care in the specialty. Maximum Hours of Work per Week Duty hours must be limited to 80 hours per week, averaged over a four-week period, inclusive of all in-house call activities and all moonlighting. While it is desirable that residents in their final years of education have eight hours free of duty between scheduled duty periods, there may be circumstances [when these residents must stay on duty to care for their patients or return to the hospital with fewer than eight hours free of duty. The frequency of at-home call is not subject to the every-third night limitation, but must satisfy the requirement for one-day in-seven free of duty, when averaged over four weeks. Innovative Projects Requests for innovative projects that may deviate from the institutional, common and/or specialty specific program requirements must be approved in advance by the Review Committee. Once a Review Committee approves a project, the sponsoring institution and program are jointly responsible for the quality of education offered to residents for the duration of such a project. These strategies will help you un derstand both your role in patient safety and how to make patient safety a core component of your medical residency program. Email: More information about patient safety can be ob tained at the Corporate Patient Safety Gateway intranet site: patientsafety. Make Safe Choices to Prevent Harm 16 Patient/Family Involvement8 Corporate and Facility Patient Safety Reducing and Preventing Adverse Drug Events To De Make Safe Choices to Prevent Harm. New Study Estimates Eight Medication Safety 26 Million American Families Experienced a Serious Near Misses, Events and/or Occurrences 28 Medical or Drug Error: April 15, 2002:
The aprosodias: functional-anatomic organization of the affective com ponents of language in the right hemisphere medicine 369 generic 800 mg asacol amex. Cross References Retinopathy; Scotoma Are exia Are exia is an absence or a loss of tendon re exes moroccanoil oil treatment purchase asacol 400mg otc. This may be physiological symptoms anxiety buy asacol pills in toronto, in that some individuals never demonstrate tendon re exes; or pathological medications that cause hair loss 400mg asacol amex, re ect ing an anatomical interruption or physiological dysfunction at any point along the monosynaptic re ex pathway which is the neuroanatomical substrate of pha sic stretch re exes symptoms whooping cough discount asacol 400 mg on line. Sudden tendon stretch medicine research buy online asacol, as produced by a sharp blow from a tendon hammer, activates muscle spindle Ia afferents which pass to the ventral horn of the spinal cord, there activating motor neurones, the efferent limb of the re ex, so completing the monosynaptic arc. Are exia is most often encountered in disorders of lower motor neurones, speci cally radiculopathies, plexopathies, and neuropathies (axonal and demyeli nating). It fails to react to light (re ex iridoplegia), but does constrict to accommodation (when the eyes converge). Since the light re ex is lost, testing for the accommodation reaction may be performed with the pupil directly illuminated: this can make it easier to see the response to accommodation, which is often dif cult to observe when the pupil is small or in individuals with a dark iris. Although pupil involvement is usually bilateral, it is often asymmetric, causing anisocoria. The Argyll Robertson pupil was originally described in the context of neu rosyphilis, especially tabes dorsalis. A lesion in the tectum of the (rostral) midbrain proximal to the oculomotor nuclei has been suggested. Four cases of spinal myosis [sic]: with remarks on the action of light on the pupil. It is said that in organic weakness the hand will hit the face, whereas patients with functional weakness avoid this consequence. The term was invented in the nineteenth century (Hamilton) as an alternative to aphasia, since in many cases of the latter there is more than a loss of speech, including impaired pantomime (apraxia) and in symbolizing the relationships of things. Hughlings Jackson approved of the term but feared it was too late to displace the word aphasia. Cross References Aphasia, Apraxia Asomatognosia Asomatognosia is a lack of regard for a part, or parts, of the body, most typically failure to acknowledge the existence of a hemiplegic left arm. Asomatognosia may be verbal (denial of limb ownership) or non-verbal (failure to dress or wash limb). All patients with asomatognosia have hemispatial neglect (usually left), hence this would seem to be a precondition for the development of aso matognosia; indeed, for some authorities asomatognosia is synonymous with personal neglect. Attribution of the neglected limb to another person is known as somatoparaphrenia. The neuroanatomical correlate of asomatognosia is damage to the right supramarginal gyrus and posterior corona radiata, most commonly due to a cerebrovascular event. The predilection of asomatognosia for the left side of the body may simply be a re ection of the aphasic problems associated with left sided lesions that might be expected to produce asomatognosia for the right side. Asomatognosia is related to anosognosia (unawareness or denial of ill ness) but the two are dissociable on clinical and experimental grounds. The term has no standardized de nition and hence may mean different things to different observers; it has also been used to describe a disorder characterized by inability to stand or walk despite nor mal leg strength when lying or sitting, believed to be psychogenic (although gait apraxia may have similar features). A transient inability to sit or stand despite normal limb strength may be seen after an acute thalamic lesion (thalamic astasia). Cross Reference Gait apraxia Astereognosis Astereognosis is the failure to recognize a familiar object, such as a key or a coin, palpated in the hand with the eyes closed, despite intact primary sensory modal ities. Description of qualities such as the size, shape, and texture of the object may be possible. There may be associated impairments of two-point discrim ination and graphaesthesia (cortical sensory syndrome). Astereognosis was said to be invariably present in the original description of the thalamic syndrome by Dejerine and Roussy. Some authorities recommend the terms stereoanaesthesia or stereohypaes thesia as more appropriate descriptors of this phenomenon, to emphasize that this may be a disorder of perception rather than a true agnosia (for a similar debate in the visual domain, see Dysmorphopsia). Cross References Agnosia; Dysmorphopsia; Graphaesthesia; Two-point discrimination Asterixis Asterixis is a sudden, brief, arrhythmic lapse of sustained posture due to involun tary interruption in muscle contraction. It is most easily demonstrated by observ ing the dorsi exed hands with arms outstretched. These features distinguish asterixis from tremor and myoclonus; the phenomenon has previously been described as negative myoclonus or neg ative tremor. Unilateral asterixis has been described in the context of stroke, contralateral to lesions of the midbrain (involving corticospinal bres, medial lemniscus), tha lamus (ventroposterolateral nucleus), primary motor cortex, and parietal lobe; and ipsilateral to lesions of the pons or medulla. Asynergia Asynergia or dyssynergia is lack or impairment of synergy of sequential muscular contraction in the performance of complex movements, such that they seem to become broken up into their constituent parts, so-called decomposition of move ment. Dyssynergy of speech may also occur, a phenomenon sometimes termed scan ning speech or scanning dysarthria. This is typically seen in cerebellar syndromes, most often those affecting the cerebellar hemispheres, and may coexist with other signs of cerebellar disease such as ataxia, dysmetria, and dysdiadochokinesia. Cross References Ataxia; Cerebellar syndromes; Dysarthria; Dysdiadochokinesia; Dysmetria; Scanning speech Ataxia Ataxia or dystaxia refers to a lack of coordination of voluntary motor acts, impairing their smooth performance. Ataxia is used most frequently to refer to a cerebellar problem, but sensory ataxia, optic ataxia, and frontal ataxia are also described, so it is probably best to qualify ataxia rather than to use the word in isolation. An International Cooperative Ataxia Rating Scale has been developed to assess the ef cacy of treatments for cerebellar ataxia. These bres run in the corticopontocerebellar tract, synapsing in the pons before passing through the middle cerebellar peduncle to the contralateral cerebellar hemisphere. Triple ataxia, the rare concurrence of cerebellar, sensory, and optic types of ataxia, may be associated with an alien limb phenomenon (sensory type). International Cooperative Ataxia Rating Scale for pharmacological assessment of the cerebellar syndrome. This syndrome is caused by lacunar (small deep) infarcts in the contralateral basis pons at the junction of the upper third and lower two-thirds. It may also be seen with infarcts in the contralateral thalamocapsular region, posterior limb of the internal capsule (anterior choroidal artery syndrome), red nucleus, and the paracentral region (anterior cerebral artery territory). Sensory loss is an indica tor of capsular involvement; pain in the absence of other sensory features is an indicator of thalamic involvement. Athetosis often coexists with the more owing, dance-like movements of chorea, in which case the movement dis order may be described as choreoathetosis. Athetoid-like move ments of the outstretched hands may also been seen in the presence of sensory ataxia (impaired proprioception) and are known as pseudoathetosis or pseudo choreoathetosis. Cross References Chorea, Choreoathetosis; Pseudoathetosis; Pseudochoreoathetosis Athymhormia Athym(h)ormia, also known as the robot syndrome, is a name given to a form of abulia or akinetic mutism in which there is loss of self-autoactivation. Clinically there is a marked discrepancy between heteroactivation, behaviour under the in uence of exogenous stimulation, which is normal or almost normal, and autoactivation. Left alone, patients are akinetic and mute, a state also known as loss of psychic self-activation or pure psychic akinesia. It is associated with bilat eral deep lesions of the frontal white matter or of the basal ganglia, especially the globus pallidus. Athymhormia is thus environment-dependent, patients nor malizing initiation and cognition when stimulated, an important differentiation from apathy and akinetic mutism. The term is often applied to wasted muscles, usually in the context of lower motor neurone pathology (in which case it may be synonymous with amyotrophy), but also with disuse. Atrophy develops more quickly after lower, as opposed to upper, motor neurone lesions. It may also be applied to other tissues, such as subcutaneous tissue (as in hemifacial atrophy). Atrophy may sometimes be remote from the affected part of the neuraxis, hence a false-localizing sign, for example, wasting of intrinsic hand muscles with foramen magnum lesions. Cross Reference Dementia Attention Attention is a distributed cognitive function, important for the operation of many other cognitive domains; the terms concentration, vigilance, and per sistence may be used synonymously with attention. It is generally accepted that attention is effortful, selective, and closely linked to intention. Impairment of attentional mechanisms may lead to distractability (with a resulting complaint of poor memory, perhaps better termed aprosexia), disori entation in time and place, perceptual problems, and behavioural problems. The neuroanatomical substrates of attention encompass the ascending retic ular activating system of the brainstem, the thalamus, and the prefrontal (mul timodal association) cerebral cortex (especially on the right). In the presence of severe attentional disorder (as in delirium) it is dif cult to make any meaningful assessment of other cognitive domains. Cross References Aprosexia; Delirium; Dementia; Disinhibition; Dysexecutive syndrome; Frontal lobe syndromes; Pseudodementia Auditory Agnosia Auditory agnosia refers to an inability to appreciate the meaning of sounds despite normal perception of pure tones as assessed by audiological examination. This agnosia may be for either verbal material (pure word deafness) or non verbal material, either sounds (bells, whistles, animal noises) or music (amusia, of receptive or sensory type). This may be equivalent to noise induced visual phosphenes or sound-induced photisms. Augmentation also refers to the paradoxical worsening of the symptoms of restless legs syndrome with dopaminergic treatment, manifesting with earlier onset of symptoms in the evening or afternoon, shorter periods of rest to provoke symptoms, greater intensity of symptoms when they occur, spread of symptoms to other body parts such as the arms, and decreased duration of bene t from medication. Auras are exclusively subjective, and may be entirely sensory, such as the forti ca tion spectra (teichopsia) of migraine, or more complex, labelled psychosensory or experiential, as in certain seizures. Although initially classi ed (by Gilles de la Tourette) with tic syndromes, there are clear clinical and pathophysiological differences. Cross Reference Tic Automatic Writing Behaviour Automatic writing behaviour is a form of increased writing activity. It has been suggested that it should refer speci cally to a permanently present or elicitable, compulsive, iterative and not necessarily complete, written reproduction of visu ally or orally perceived messages (cf. This is characterized as a particular, sometimes isolated, form of utilization behaviour in which the inhibitory functions of the frontal lobes are suppressed. Increased writing activity in neurological conditions: a review and clinical study. Cross References Hypergraphia; Utilization behaviour Automatism Automatisms are complex motor movements occurring in complex motor seizures, which resemble natural movements but occur in an inappropriate set ting. These may occur during a state of impaired consciousness during or shortly after an epileptic seizure. Automatisms occur in about one-third of patients with complex partial seizures, most commonly those of temporal or frontal lobe origin. Although 52 Autoscopy A there are qualitative differences between the automatisms seen in seizures arising from these sites, they are not of suf cient speci city to be of reliable diagnostic value; bizarre automatisms are more likely to be frontal. Cross References Absence; Aura; Pelvic thrusting; Poriomania; Seizure Autophony the perception of the reverberation of ones own voice, which occurs with external or middle, but not inner, ear disease.
References
- Kee K, Naughton MT. Heart failure and the lung. Circ J 2010; 74: 2507-2516.
- Hannila SS, Filbin MT. The role of cyclic AMP signaling in promoting axonal regeneration after spinal cord injury. Exp Neurol. 2008;209:321-332.
- Haberle J, Gorg B, Rutsch F, et al. Congenital glutamine deficiency with glutamine synthetase mutations. N Engl J Med 2005;3:353.
- Graham TP. Ventricular performance in adults after operation for congenital heart disease. Am J Cardiol 1991;68:403.