Michael W. Weaver MD
- Assistant Professor of Neurosurgery, Temple University Hospital and School of
- Medicine, Philadelphia, Pennsylvania
Plasma deriva tives are prepared by pooling plasma from many donors and subjecting the plasma to a fractionation process that separates the desired proteins diabetes insipidus urine lytes safe 25 mg cozaar, including immune globulin and clotting factors metabolic disease genetics buy cozaar 50 mg with visa. From an infectious disease standpoint juvenile diabetes diet purchase cheap cozaar online, plasma derivatives differ from blood compo nents in several ways diabetic diet in hindi cozaar 25mg cheap. For economic and therapeutic reasons diabetes classes buy cozaar without prescription, plasma from thousands of donors is pooled diabetes signs mayo order cozaar 25mg overnight delivery, and therefore, recipients of plasma derivatives have vastly greater donor exposure than do blood component recipients. However, plasma derivatives are able to withstand vigorous viral inactivation processes that would destroy Red Blood Cells and Platelets. Development and evaluation of various novel strategies for inactivation of infectious agents are ongoing for cellular components. Since January 2007, most donations also have been tested for anti bodies to Trypanosoma cruzi, the etiologic agent of Chagas disease, on an investigational basis. Transfusion-Transmitted Agents: Known Threats and Potential Pathogens Any infectious agent that has an infectious blood phase potentially can be transmitted by blood transfusion. Although blood donations are screened for these viruses, there is a very small residual risk of infec tion resulting almost exclusively from donations collected during the ?window period of infection?the period soon after infection during which a blood donor is infectious but screening results are negative. Blood donations generally are not screened for parvovirus B19, because previous infection with this virus is common in adults. The risk of transmission of parvovirus B19 from Whole Blood donations is unknown but thought to be rare. A small proportion of people with post transfusion hepatitis as well as community-acquired hepatitis will have negative test results for all known hepatitis agents. No test has been licensed to screen donors for any of these viruses, and no data suggest that such tests would be benefcial. The predominant modes of transmission are male-to-male sexual contact in the United States and close, nonsexual contact in Africa and Mediterranean Europe. Blood collection agencies primarily use an algorithm starting with minipools of donation samples. Donations constituting a reac tive minipool are retested individually and, if results are positive, the reactive units are removed from the blood supply. A case of transfusion-transmitted dengue hemorrhagic fever was recognized during a recent outbreak of dengue fever in Puerto Rico (and other transfusion-transmitted dengue cases in East Asia). Small outbreaks of dengue fever in Florida, Texas, and Hawaii resulted in no recognized transfusion transmissions. Currently, healthy blood donors recently returning to the continental United States from areas with endemic or epidemic dengue are not deferred, and no licensed tests to screen donors for dengue infection are available, although some blood establish ments have implemented investigational donor screening and deferral programs; similar programs are under consideration nationally. Bacterial contamina tion can occur during collection, processing, and transfusion of blood components. Platelets are stored at room temperature, which can facilitate growth of con tami nating bacteria. The predominant bacterium that contaminates Platelets is Staphylococcus epidermidis. Bacillus species; more virulent organisms, such as Staphylococcus aureus; and various gram-negative bacteria, including Salmonella and Serratia species, also have been reported. Transfusion reactions attributable to contaminated Platelets potentially are underrecognized, because episodes of bacteremia with skin organisms are common in patients requiring Platelets, and the link to the transfusion may not be suspected. As a result, most apheresis platelets are screened using liquid culture meth ods, whereas pooled platelets generally are screened using nonculture-based, less-sensitive methods. The American Red Cross has estimated that current culture methods may detect only 50% of bacterial contamination. Hospitals should ensure that protocols are in place to communicate results of bacterial contamination, both for quarantine of components from individual donors and for prompt treatment of any transfused recipients. Post-transfusion notifcation of appropriate personnel is required if cultures identify bacteria after prod uct release or transfusion. If bacterial contamination of a component is suspected, the transfusion should be stopped immediately, the unit should be saved for further testing, and blood cultures should be obtained from the recipient. Bacterial isolates from cultures of the recipient and unit should be saved for further investigation. Red Blood Cell units are much less likely than are Platelets to contain bacteria at the time of transfusion, because refrigeration kills or inhibits growth of many bacte ria. However, certain bacteria, most notably gram-negative organisms such as Yersinia enterocolitica, may contaminate Red Blood Cells, because they survive cold storage. Cases of septic shock and death attributable to transfusion-transmitted Y enterocolitica and other gram-negative organisms have been documented. Reported rates of transfusion-associated bacterial sepsis have varied widely depend ing on study methodology and microbial detection methods used. A prospective, volun tary multisite study (the Assessment of the Frequency of Blood Component Bacterial Contamination Associated with Transfusion Reaction [BaCon] Study) estimated the rate of transfusion-transmitted sepsis to be 1 in 100 000 units for single-donor and pooled Platelets and 1 in 5 million units for Red Blood Cells. Increasing travel to and immigration from areas with endemic infection have led to a need for increased vigilance in the United States. The incidence of transfusion-associated malaria has decreased over the last 30 years in the United States. Most cases are attributed to infected donors who have immigrated to the United States rather than people born in the United States who traveled to areas with endemic infec tion. Prevention of transfusion-transmitted malaria relies on interviewing donors for risk factors related to residence in or travel to areas with endemic infection or previous treatment for malaria. Donation should be delayed until 3 years after either completing treatment of malaria or living in a country where malaria is found and 12 months after returning from a trip to an area where malaria is found. The immigration of millions of people from areas with endemic T cruzi infection (parts of Central America, South America, and Mexico) and increased international travel have raised concern about the potential for transfusion-transmitted Chagas disease. To date, fewer than 10 cases of transfusion-transmitted Chagas disease have been reported in North America. However, studies of blood donors likely to have been born in or to have trav eled to areas with endemic infection have found antibodies to T cruzi in as many as 0. Although recognized transfusion transmissions of T cruzi in the United States have been rare, in some areas of the United States, the prevalence of Chagas disease estimated by detection of antibodies appears to have increased in recent years. In the absence of treatment, seropositive people can remain potential sources of infection by blood trans fusion for decades after immigration from a region of the world with endemic disease. Screening for Chagas disease by donor history is not adequately sensitive or specifc to identify infected donors. In the frst 16 months of screen ing, more than 14 million donations were tested, yielding a seroprevalence of 1:27 500; the highest rates were in Florida (1:3800) and California (1:8300). However, more recent discussions have suggested that donors only be screened a limited number of times, depending on their risk of continued exposure. Babesiosis is the most commonly reported transfusion-associated tickborne infection in the United States. However, at least 4 cases have been associated with receipt of whole blood-derived Platelets, which often contain a small number of red blood cells. Although most infections are asymptomatic, Babesia infection can cause severe, life-threatening disease, particularly in the elderly and people without spleens. Severe infection can result in hemolytic anemia, thrombocytopenia, and renal failure. Surveys using indirect immunofuorescent antibody assays in areas of Connecticut and New York with highly endemic infection have revealed seropositivity rates for B microti of approxi mately 1% and 4%, respectively. Although people with acute illness or fever are not suitable to donate blood, people infected with Babesia species commonly are asymptomatic or experience only mild and nonspecifc symptoms. In addition, Babesia species can cause asymptomatic infection for months and even years in untreated, otherwise healthy people. Questioning donors about recent tick bites has been shown to be ineffective, in part because donors who are sero positive for antibody to tickborne agents are no more likely than seronegative donors to recall tick bites. The asymptomatic incubation periods in the clini cally ill recipients lasted from 6. Improving Blood Safety A number of strategies have been proposed or implemented to further decrease the risk of transmission of infectious agents through blood and blood products. Methods used for this include wet and dry heat and treatment with a solvent/detergent. Solvent/detergent-treated pooled Plasma for transfusion no longer is marketed in the United States, but methods of treating single donor Plasma are under study. Because of the fragility of Red Blood Cells and Platelets, pathogen inactivation is more diffcult. However, several methods have been developed, such as addition of pso ralens followed by exposure to ultraviolet A, which binds nucleic acids and blocks replica tion of bacteria and viruses. Leukoreduction, in which flters are used to remove donor white blood cells, is performed increasingly in the United States. Benefts of this process include decreasing febrile transfusion reactions related to white blood cells and their products and decreasing the immune modulation associated with transfusion. Established alternatives include recombinant clotting factors for patients with hemophilia and factors such as erythropoietin used to stimulate red blood cell production. These adverse safety outcomes and shortened time to tumor progression have been observed in certain patients with cancer who have chemotherapy-related anemia, such as people with advanced head and neck cancer receiving radiation therapy and metastatic breast cancer. Blood may be donated by the patient several weeks before a surgical procedure (preoperative autologous donation) or, alternatively, donated immediately before surgery and replaced with a volume expander (acute normovolemic hemodilution). Autologous blood is not completely risk free, because bacterial contamination may occur. During surgery, blood lost by the patient may be collected, processed, and reinfused into the patient. The National Healthcare Safety Network is a secure Internet-based surveillance system that collects data from voluntary participating health care facilities in the United States. A similar system has been established in several centers in the United States that treat patients with thalassemia who depend on frequent blood transfusions. For regulatory purposes, serious adverse reactions and product problems should be reported to the manufacturer (or, alternatively, to the sup plier for transmission to the manufacturer). The proliferation of these products also has increased the opportuni ties for transmission of infectious pathogens, including bacteria, viruses, and parasites. The Joint 1 Commission adopted some of these standards, which will apply to accredited organiza tions that store or use tissue. Solid organs are overseen by the Health Resources and Services Administration through the Organ Procurement and Transplant Network, which also compiles donor-derived disease reports. All suspected disease-transmission cases, notifable diseases, and clusters should be reported to public health agencies. Human Milk Breastfeeding provides numerous health benefts to infants, including protection against morbidity and mortality from infectious diseases of bacterial, viral, and parasitic ori gin. In addition to providing an ideal source of infant nutrition, human milk contains immune-modulating factors, including secretory antibodies, glycoconjugates, anti infammatory components, and other factors. Breastfed infants have high concentra tions of protective bifdobacteria and lactobacilli in their gastrointestinal tracts, which diminish the risk of colonization and infection with pathogenic organisms. Protection by human milk is established most clearly for pathogens causing gastrointestinal tract infec tion. In addition, human milk seems to provide protection against otitis media, invasive Haemophilus infuenzae type b infection, and other causes of upper and lower respiratory tract infections. Evidence also indicates that human milk may modulate development of the immune system of infants. No evidence exists to validate concern about the potential presence of live viruses from vaccines in maternal milk if the mother is immunized during lactation. Lactating women may be immunized as recommended for adults and adolescents to protect against many infectious diseases ( If previously unimmunized or if traveling to an area with endemic infection, a lactating mother may be given inactivated poliovirus vaccine. Attenuated rubella can be detected in human milk and transmitted to breastfed infants with seroconversion; infections usually are asymptomatic or mild. Women who previ ously have not received tetanus toxoid, reduced diphtheria toxoid, and acellular pertus sis (Tdap) should receive a dose of Tdap vaccine during pregnancy, preferably during the third or late-second trimester (after 20 weeks gestation). If not administered during pregnancy, Tdap should be administered immediately postpartum. Breastfeeding women should receive a seasonal infuenza immunization for the current season when available, if not received while pregnant. Either inactivated or live-attenuated infuenza immunizations may be administered during the postpartum period. Transmission of yellow fever vaccine virus via breastfeeding has resulted in meningoencephalitis in the nursing infant. Yellow fever vaccine is contraindicated in the breastfeeding mother in nonemergency situations. The immunogenicity of some recom mended vaccines is enhanced by breastfeeding, but data are lacking as to whether the effcacy of these vaccines is enhanced. Although high concentrations of antipoliovirus antibody in human milk of some mothers theoretically could interfere with the immuno genicity of oral poliovirus vaccine, this is not a concern with inactivated poliovirus vac cine. The effectiveness of rotavirus vaccine in breastfed infants is comparable to that in nonbreastfed infants. Mastitis and breast abscesses have been associated with the presence of bacterial pathogens in human milk. Breast abscesses have the potential to rupture into the ductal system, releasing large numbers of organisms, such as Staphylococcus aureus, into milk. Temporary discontinuation of breastfeeding on the affected breast for 24 to 48 hours after surgical drainage and appropriate antimicrobial therapy may be necessary. In general, infectious mastitis resolves with continued lactation during appropriate antimicrobial therapy and does not pose a signifcant risk for the healthy term infant. Even when breastfeeding is interrupted on the affected breast, breastfeeding may continue on the unaffected breast. Women with tuberculosis who have been treated appropriately for 2 or more weeks and who are not considered contagious may breastfeed. Women with tuberculosis disease suspected of being contagious should refrain from breastfeeding and other close contact with the infant because of potential spread through respiratory tract droplet or airborne transmission (see Tuberculosis, p 736).
K feed the baby by cup managing diabetes in hemodialysis patients order discount cozaar line, if possible with her own breast milk diabetes type 1 paleo diet buy cozaar 50mg with visa, until he or she is willing to take the 7 diabetes in dogs exercise generic cozaar 50 mg without prescription. Symptoms:The baby refuses to breastfeed diabetic diet weekly menu purchase cheap cozaar, and may cry diabetes symptoms heart rate buy cozaar 50mg lowest price, arch his or her back diabetes symptoms glucose generic 50 mg cozaar, and turn away when put to the 7. Twins who are low birth weight need to be managed Causes: There may be a physical problem such as: accordingly (see Session 6. K illness, an infection, or a sore mouth, for example For larger twins, management should be as for single thrush (see Session 7. Early effective suckling can ensure an ade K sedation, if the mother received analgesics during quate milk supply for both infants. Mothers may need help to fnd the best way to hold the baby may have diffculty or frustration with two babies to suckle, either at the same time, or one at breastfeeding because of: a time. They may like to give each baby its own breast, K sucking on a bottle or pacifer; or to vary the side. Holding one or both babies in the underarm position for feeding, and support for the K diffculty attaching to the breast; babies with pillows or folded clothes is often helpful. If the mother has had spinal or epidural anaesthesia, Management: If a cause is identifed, it should be treat the baby should be delivered onto her chest, and she ed or removed, if possible. She can be helped If she has had a general anaesthetic, she should start to improve her breastfeeding technique, and how to skin-to-skin contact and initiate breastfeeding as avoid the use of bottles and pacifers. She can also be soon as she is able to respond, usually about 4 hours helped to: after delivery. A baby who is full term and in good condition can wait for the frst feed until the mother K keep her baby close, with plenty of skin-to-skin responds. Babies who are at risk of hypoglycaemia contact, and no other carers for a time; may need an alternative feed until they can start K offer her breast whenever the baby shows signs of breastfeeding (see Session 6. Hospital staff K sleep with her baby, so that she can breastfeed at and family members can all help her in this way. Dif work; fculties in the past have often been because mothers K express her milk while she is at work to keep up did not receive enough help to establish breastfeeding the supply. She can refrigerate the milk if this is in the post-operative period, and because babies were possible, or keep it for up to 8 hours at room tem given other feeds meanwhile. If this is not possible, If a baby is too ill or too small to fed from the breast she may have to discard it. She needs to understand soon after delivery, the mother should be helped that the milk is not lost her breasts will make to express her milk to establish the supply, starting more. If a mother does not express when at work, within 6 hours of delivery or as soon as possible, in her milk production will decrease. If facilities are avail the commonest reason for a mother being separated able, she can store her milk by freezing it (see Session from her baby for part of the day is because she is 4. Help the baby to start breastfeeding as soon as he employed outside the home, for example when mater or she is able and can be with the mother again. She Symptoms related to feeding should be encouraged to breastfeed the baby as much K the infant may want to breastfeed more often than as possible when she is at home, and to consider before. The infant may suckle for only a short time and not take enough expressing her milk for the baby milk. A trained health worker should teach her how to express and store her breast milk (see Session 4. Breast milk is the and to feed her infant using supplementary suckling ideal food during illness, especially for infants less to stimulate breast-milk production (see Session 6. With appropriate skilled support, many mothers can resume exclusive breastfeeding within 1?2 weeks. Babies under 6 months of age If a baby is in hospital, the mother should be allowed Infants and young children over 6 months of age to stay with him or her, and to have unrestricted A young child may prefer breastfeeding to comple access so that she can respond to and feed the baby mentary foods while he or she is ill, and breastfeed as needed. Milk production may increase, so that the mother notices increased fullness of her If a baby has a blocked nose breasts. She should be encouraged to stay with her child in hospital and to breastfeed on demand. She can give complementary foods, which may need to be given shorter more frequent breastfeeds, allowing the baby more often, in smaller quantities and of a softer con time to pause and breathe through the mouth until sistency than when the child is well. Jaundice can make a baby sleepy so that he or she suck If a baby is not able to breastfeed adequately, but can take oral les less. Early initiation of breastfeeding and frequent or enteral feeds breastfeeding reduce the severity of early jaundice. She should express as often as the baby would feed, that Prolonged jaundice starts after the seventh day of life is 8 times in 24 hours, to keep up her milk supply. She should be encouraged is sometimes called ?breast-milk jaundice which is to let the baby suckle whenever he or she wants to . If the jaundice is due to a more serious condition there are usually other signs, If a baby is not able to take any oral or enteral feeds such as pale stools, dark urine, or enlarged liver and spleen. The mother should be encouraged to continue expressing to keep up her milk supply. Her expressed Management milk can be stored safely and given to the baby as early jaundice soon as he or she starts enteral feeds. She may be able Water and glucose water do not help, and may make to freeze unused milk for later use. Taking more breast has milk-banking facilities, the milk may be used for milk helps jaundice to clear more quickly, so the another child. She can also express her milk If breast-milk production decreases during an illness after feeds and give some extra by cup or tube. If she is feeding her baby on expressed breast milk, she should A decrease in production is especially likely if a moth give 20% extra. If jaundice is severe, phototherapy er has breastfeeding diffculties or if she has given (light treatment) may be needed. The mother needs help to increase her milk supply the baby should be referred for clinical assessment, again. These babies the lip is affected, the breast covers the cleft, and the may feed slowly, and it may be necessary for the baby may be able to suckle effectively. Sometimes a mother to express her milk and give some feeds by baby with a cleft palate can suckle quite well, if there cup or tube. The mother will need extra support and is enough palate for the tongue to press the nipple counselling to bond with her baby, to feel that she is against. This can make attachment diffcult, which may dancer hand position cause sore nipples. Muscular weakness: babies with Down syndrome or cerebral palsy have diffculty attaching to the breast and suckling because of the weakness. Congenital heart or kidney problems: a baby fails to grow, but there is no apparent diffculty with breast feeding or breast-milk supply. Heart, kidney or other abnormalities Management Consider these possibilities in a baby who fails to Cleft lip and/or palate grow despite good breastfeeding practices. Examine the baby should be referred for surgery, which usually the baby carefully, and refer for further assessment. It is important for the baby to grow and to be well References nourished before undergoing surgery. Evidence for the Ten Steps to successful the mother can be helped to hold the baby in an breastfeeding. Breastfeeding: physiology into be able to lead a normal life if he or she has surgery. Pacifer use, early weaning, and baby will need referring for cutting of the frenulum. Randomized control trial of division of tongue-tie in infants with feeding problems. However, child feeding, it is important to remember her own a woman with a poor diet may not have laid down health, and care for her as well as the baby. She needs to eat an extra address include any illness she may have, her nutri meal with a variety of foods each day to cover her tional status and food intake, maternal medication, needs and protect those stores that she has. It is generally helpful to advise the woman to eat a greater amount and variety of foods, such as meat, 8. It is impor important to consider what effect it might have on tant to determine if there are taboos about foods, and breastfeeding. Pregnant and her to breastfeed, for example if she has a disability, lactating women can eat any foods normally included or is mentally ill. If a mother is very ill and unable in the local diet these will not harm the breastfeed to breastfeed, options for feeding her infant or child ing baby. Very thin women and adolescents require until she can resume will need to be considered. If a mother has hepatitis (A, B, or C) breastfeeding If extra food is not available, this should not prevent can continue normally as the risk of transmission by a mother from breastfeeding. Only when a woman about different feeding options and support for her is seriously malnourished does the quantity of breast choice (see Session 6. Where household resources are scarce, breast milk is likely to be the most complete and safest 8. A need supplements of fortifed products both for their diet that is poor in quantity or quality may affect her own health and that of their breastfeeding infants. Others need to are some medicines that can cause side-effects in the come from an increased intake. Antibiotics: ampicillin, amoxicillin, cloxacillin and other penicillins, erythromycin, Antituberculosis drugs, anti-leprosy drugs (see dapsone above) Antimalarials (except mefoquine, fansidar) Anthelminthics, antifungals Bronchodilators. Birth-to-pregnancy intervals of against pregnancy, even if they are breastfeeding. Birth-to-pregnancy intervals of (see Box 18): around 18 months or less are associated with a signif the mother must be amenorrhoeic that is, she must cantly higher risk of neonatal and infant mortality, low not be menstruating. If she menstruates, it is a sign birth weight, small size for gestational age and preterm that her fertility has returned, and she can become birth. The baby must breastfeed exclusively,1 and feed fre quently during both day and night. If Box 18 there is a gap of 6 hours or more between breastfeeds, ovulation may occur. After 6 no other method use another method if: months, a woman is more likely to be fertile, even needed if: if she has not started to menstruate. Even K Baby exclusively K other foods and fuids after 6 months, if she has not menstruated and the breastfed have been introduced baby is still breastfeeding frequently, she is partially protected. If she wishes to avoid Hormonal methods can have an effect on lactation, and pregnancy she should start another method imme reduce breast-milk production. It is better to work and cannot breastfeed her baby while she is to avoid them altogether if possible. If she is not exclusively breastfeed other method is available, then it is better for both ing, she should start another method of family plan mother and child if she uses the combined pill than ning no later than 6 weeks after delivery, at her fnal if she risks an early pregnancy. Management of Pregnancy and Childbirth: preg K Intra Uterine Devices are very suitable. Geneva, World K Condoms, diaphragms and spermicides are suitable, Health Organization, 2006. Geneva, World Health Organization Task Force on Methods for Health Organization, 2003. World Policy, health system and community actions the Global Strategy for Infant and Young Child Feeding K Ensure that the health and other relevant sectors (1) is the overarching framework for action by gov protect, promote and support exclusive breastfeed ernments and all concerned parties to ensure that the ing for 6 months and continued breastfeeding up health and other sectors are able to protect, promote to 2 years of age or beyond, while providing women and support appropriate infant and young child feed access to the support they require in the family, ing practices. It identifes four operational tar families and other caregivers; gets (2): K Consider what new legislation or other suitable K Appoint a national breastfeeding co-ordinator measures may be required, as part of a comprehen with appropriate authority, and establish a multi sive policy on infant and young child feeding, to sectoral national breastfeeding committee com give effect to the principles and aim of the Code. K cash benefts during leave of at least two thirds of previous or insured earnings; the Code addresses the quality and availability of the products, and information concerning their use. It K access to medical care, including prenatal, child provides recommendations concerning the market birth and postnatal care, as well as hospitalization ing of industrially-prepared complementary foods, when necessary; encouraging the use of locally-available foods. Thus K health protection: the right of pregnant and nurs the Code does not seek to ban products, but to control ing women not to perform work prejudicial to their promotion that may infuence families to use them health or that of their child; when they are not needed. K breastfeeding: minimum one daily break, with pay; Health workers have important responsibilities to K employment protection and non-discrimination. For exam ple, health care facilities should not be used for the Few countries have ratifed this Convention, although purpose of promoting or displaying infant formula or many countries have adopted some provisions other products within the scope of the Code. Health professionals have an should be done only by trained health workers and important role to advocate for good legislation on only to mothers or family members who need to use maternity protection, and hospitals and other health formula, or who have made an informed decision to facilities should offer maternity leave and breastfeed do so. Health workers should explain clearly the dan ing support for their own personnel. These include: Health workers have a critical role in protecting, promoting and supporting infant and young child K to encourage and protect breastfeeding; feeding. The advice given by health workers has been K not to accept fnancial or material inducements to identifed as one of the key determinants infuencing promote these products; mothers feeding practices. Health workers therefore should have the necessary knowledge and skills to K not to give samples of infant formula to pregnant counsel caregivers and help them overcome feeding women, mothers of infants and young children, or diffculties when they occur. Activities to egy for infant and young child feeding interventions create a breastfeeding culture and ensure that moth through which many children can be reached and ers, other caregivers and the wider community have coverage improved. K appropriate complementary feeding from 6 months with continued breastfeeding up to 24 months or 9. Other people in the family and com during and after illness; munity infuence them. To improve practices, a com munication strategy must address the beliefs of these K adequate nutrition of women; other people, so that there is a change in family and K control of vitamin A defciency; community norms.
Implicit in his alliance with cultural studies is the belief that humanities research on scientific and medical disciplines can gestational diabetes definition diagnosis cheap cozaar 50mg online, by exposing problematic scientific and medical practices diabetes test boots generic 50 mg cozaar amex, also work to change them diabetes obesity and metabolism generic 50mg cozaar with mastercard. Also diabetes type 1 and 2 buy cozaar 50mg overnight delivery, the point of situating texts within their historical and political context is to use rhetorical analysis to better understand the particular cultural milieu such texts are a part of: ?Rather than gesturing toward larger cultural entanglements as a way to situate and elucidate texts control diabetes urdu cheap 50mg cozaar with amex, a rhetorical-cultural study examines specific texts as a way to situate shifting cultural entanglements blood glucose 397 order generic cozaar on line. The trajectory of a shifting intertext, rather than specific texts, becomes the primary object of study (25). What that means for the chapters that follow is that context plays a key role in understanding rhetorical analysis; each analysis of texts from a particular discourse community begins by charting the shifting intertext, or the historical specificity, necessary to understand how the texts under consideration fit into?and shed light on?a broader picture. This perspective seems especially important in negotiating the textual and material terrain of American obstetrics, a specialty that traffics heavily between the designs of nature and the imposition of culture. To borrow an image from Haraway, I am not so much interested in pinpointing that boundary as I am in analyzing the traffic for challenges to the established order it might engender (Primate Visions). My project here is to use the embodied and medicalized processes of childbirth as a lens through which we might more clearly see such traffic at work in a particular historical moment. To put it simply, I will attempt to map out the trajectory of narratives working to produce knowledge about childbirth in the first decade of the twenty-first century in the United States. Once I have drawn the basic contours of that map, I will focus in on smaller, more detailed regions, fleshing out the narratives particular to various discourse 18 communities and the contexts in which they have been used. In each chapter, I will be more specific about the methods I use for each of those discourse communities, especially how and why I chose certain texts. By unearthing the narratives circulating not just about birth, but also about the authority of professional medicine, the power of medical technology, and the role of scientific research in shaping medical practice and individuals relationships to health care, I intend to reframe discussions of birth through a more interdisciplinary lens. Moreover, I hope to use my analysis of childbirth discourses as a model to demonstrate that how science and medicine are articulated can have a weighty effect on material lives and to show that critiquing the way that articulation works can begin to trouble its persuasiveness. Though much of the work in feminist science studies and rhetorical studies of science 6 and medicine has focused on reproductive politics and technologies, few rhetoricians have turned their attention to the bodily process of childbirth and its scientific, medical, and cultural 7 trappings. I hope my project will fill that gap and bring this medically and technologically mediated event into larger conversations about the ways our cultural construction of biomedicine shapes our experiences of material reality. Social science literature, particularly sociology, anthropology, and history, has attended to the cultural meanings inscribed on the birthing body, especially since the 1970s. Much of this work focuses on the professionalization of obstetrics and the increased use of technological intervention in the birthing process. Wertz were among the first to produce a sustained historical critique of this kind, and their 1977 study, Lying-In: A History of Childbirth in America remains one of the most comprehensive narratives of how the shift from home to hospital came to be the norm. Their narrative works to revise what they call the ?success story of modern medicine to reveal a more complex web of power, economics, and a confluence of social forces that has resulted in a system where birth ?routinely requires the arts of medicine to overcome the processes of nature, often to the detriment of women (emphasis in original, xvi). Anthropologist Emily 8 For an overview of work they call the ?anthropology of birth, see Robbie Davis-Floyd and Carolyn F. Robbie Davis-Floyd, who has been writing about reproduction and medicine for nearly two decades, theorized what she called ?technocratic birth as an elaborate set of rituals, a ?rite of passage designed to communicate core cultural values to birthing women, especially that technology is superior and should be used to overcome the processes of nature, that their bodies are fundamentally flawed, and that physiological reproduction is inherently dangerous. Historian Judith Walzer Leavitt offered a revisionary history of the often-told story of medical men wresting control of birth from women by showing how women have always influenced the models of birth that rise to power. More recent work in the social sciences includes an ethnographic account of traditional African American midwifery in Virginia (G. Fraser), a history of anesthesia (Wolf), cultural analyses of specific obstetric practices like amniocentesis (Rapp) and fetal ultrasound (Taylor), and returns to earlier conceptions of power, knowledge, and medicine (Simonds, Rothman, and Norman; Davis-Floyd and Sargent). In the field of literary studies, scholarship particular to representations of childbirth is relatively sparse. Mothering has received a great deal of attention from feminist literary scholars, as has reproductive politics; far less attention has been paid to the maternal body. The unarticulated space of maternity exists largely because the maternal body occupies such a liminal space, 21 according to Kristeva: pregnancy is the ?threshold between culture and nature, unable to be subsumed by either the signified or the biological essence (182). The inability of existing discourses to speak to this condition are not inconsequential ?silence weighs heavily none the less on the corporeal and psychological suffering of childbirth and especially the self-sacrifice involved in becoming anonymous in order to pass on the social norm (183). As part of that project, she makes the case that dualism?especially the body/mind split?will never serve the interests of women, that we should be able to find ways to ?think through the body, without remaining trapped in patriarchal demands on it (284). In her attempt to make sense of her own bodily experience of maternity, she describes hospitalized childbirth as a metaphor for the oppression of women in general: ?No more devastating image could be invented for the bondage of woman: sheeted supine, drugged, her wrists strapped down and her legs in stirrups, at the very moment when she is bringing life into the world (171). Since Kristeva and Rich first articulated the need for more thinking about how to include the embodied experience of childbirth in feminist theorizing about maternity, relatively few scholars in literary studies have attended to that project. Part of the reason for that, according to some scholars, is that literature has often reproduced the cultural silences surrounding the birthing body of particular historical periods. Identifying the cultural forces and textual patterns that have 22 contributed to the persistence of such attitudes is one way some scholars have worked to reclaim the maternal body. Krista Ratcliffe, for instance, writes that the first step in liberating the maternal body from its marginalized position in discourse is to draw attention to the narrative silences surrounding birth, to dig into the ways that literary and cultural texts have evaded maternal experience. In literature, argues Ratcliffe, this silencing happens most often when male writers have ?remov[ed] birth from the physical realm and render[ed] it metaphorical (49) and when they have objectified birthing women and erased their perspective from the account (51). Patricia Yaeger also finds attending to the literary silences of birth an important component of establishing what she calls a ?poetics of birth. Another component of such a poetics would locate the spaces that unearth a ?reproductive unconscious, that point to reproductive anxiety or ?cultural contestation or struggle (267-68). Another way, and the one feminists interested in maternity have turned to most often, is to look to representations of birth by women writers. The edited collection, this Giving Birth, takes as its purpose this very recovery. This project will build on this small but rich body of scholarship on childbirth and extend the focus of analysis across disciplines and beyond the birthing room. As my review 24 shows, much of the scholarship specifically devoted to childbirth emerges out of a fairly static disciplinary boundary: the social sciences have produced research that has been primarily concerned with the material conditions of birth, while literary studies has been mostly concerned with the symbolic representation of childbirth; there has been little cross-over 9 between the two arenas. My project has been informed and enriched by much of this work, as it has taught us a great deal about the conditions and the representation of childbirth and medicine. Where I see my project intervening in this discussion is in connecting representation with its potential effects on material bodies, discourse with the knowledge it produces, and science and medicine with the narratives that give them meaning. A foundational premise for my study is that more purposeful interdisciplinarity can contribute to a fuller, richer understanding of childbirth and what it can mean for our engagement with medicine, science, and physiological human reproduction and can begin to unsettle the boundary between the ?real and the representational in order to bring them to bear on one another. Before I begin that project, of tracing the trajectory of childbirth and medicine through contemporary culture, I will briefly sketch the historical movements necessary to understand how we have arrived at the particular context of birth practices in the twenty-first century. Mazzoni and Adams also both use scientific and cultural discourses to illuminate their literary analyses in productive ways. However, this work is rarely taken up by scholars in other disciplines; though the individual texts themselves include some interdisciplinarity, the conversation, as I see it, has remained fairly enclosed within each disciplinary home. My hope is that by locating the conversation about childbirth squarely within medicine and science studies, rather than as a separate (and marginal) issue, those disciplinary boundaries will start to give way. Midwives attended 8% of all births, including certified nurse midwives attendance at hospital births, and traditional and nurse-midwives attendance at home and at freestanding birth centers (Martin et al. The vast majority of women also experience high rates of medical intervention, and many give birth by major abdominal surgery. Though the rates of preterm birth and low birthweight babies have slightly decreased in the last few years (Martin et al. The maternal and infant mortality rates, though relatively low compared to the rest of the world, are still higher than those in most industrialized countries (Wagner). Especially troubling is the racial disparity in birth outcome: African American women are four times more likely to die from childbirth-related causes than are white women in the United States and their babies are 26 twice as likely to die before their first birthdays (Hoyert 8-9). They also experience cesarean section at higher rates than any other racial or ethnic group and have much higher rates of preterm birth and low and very low birthweight babies (Martin et al. In general, birth is highly medically managed by the profession of obstetrics, but due to some of the concerning statistics listed above, a growing birth advocacy movement indicates increasing discontent with the current state of maternity care. Nonprofit organizations dedicated to reforming maternity care and hospital birth abound: the Center for Childbirth Choices, Childbirth Connection, the International Cesarean Awareness Network, as well as a grassroots campaign to legalize certified midwives in all fifty states. Additionally, blogs and social media devoted to childbirth reform have proliferated in the last few years, a phenomenon I will discuss in more detail in Chapter Five. The traditional story told in light of medical and scientific progress indicates that once upon a time, childbirth was a very dangerous event for women and babies, then doctors took over and began delivering babies in hospitals, and birth ceased to be a 10 risky affair. The logic implied by this narrative is that childbirth was dangerous because it lacked medical management, and obstetrical control and the hospital environment were the things that vastly improved birth outcomes. A more careful look at the big picture of history, however, has told a slightly different story. It was, without a doubt, far more dangerous than it is today; however, most historians and sociologists of medicine agree that the danger of mortality, for women and children, was caused by a range of factors, including very high fertility rates and a lack of safe, reliable contraception; the inability to diagnose or treat infection, especially with antibiotics; little knowledge about the physiological mechanisms and potential complications of birth; and poorer health in general, especially a lack of disease control for common causes of death like tuberculosis (Leavitt; Starr; Wertz and Wertz). Both groups of women experienced many physical complications as the result of years of continuous childbearing, including vaginal fistulas, incontinence, and prolapsed uteri, all of which contributed to even more painful and complicated deliveries (Leavitt 29-30). Though it is impossible to determine exactly how many pregnancies women endured or how many deaths resulted, the cultural attitudes towards the event of birth indicate that it was shrouded in the possibility of death, for mother or child. Leavitt writes that ?childbed deaths were so familiar to Americans, from the eighteenth century to the twentieth century, that fearful anticipation characterized the common and realistic attitude towards pregnancy (27). It is no wonder, then, that many women welcomed the possibility of scientific medicine and professional expertise to alleviate some of that anxiety. Until the nineteenth century, many of these women would have had little to no formal education and no access to formal midwifery training; their training in attending births would have been experiential (Rooks 20-21). Most of the midwives practicing in nineteenth-century America who did have formal training were European immigrants and had been educated in urban midwifery schools in Italy, Germany, or France. For the most part, American midwifery was a community-based vocation, steeped in tradition and passed on from one generation to the next as younger women observed their elders attending births. Gradually, over the course of the nineteenth century, medical men began to enter the birthing room in greater numbers; midwives and female attendants still retained control, but they sometimes called male doctors to assist if there was a complication (Wertz and th Wertz 43). The development and use of forceps in 18 -century England was instrumental in providing access to birth for medically trained men: they had a tool they could use that midwives did not have. Partly as a result of male doctors increased use of forceps at birth, which proved they could do something to help, and partly as a result of an increased value in formal education, the all-female domain of birth gradually shifted. Towards the end of the nineteenth century, middle and upper-class families more frequently chose male physicians to attend their births, and midwives were left to care primarily for women in lower social classes, especially in rural areas (Rooks; Leavitt). Historians are quick to point out, however, that formal education did not necessarily make for a skilled birth attendant. Many male doctors who had had training in the ?new midwifery had never seen a birth before they began practicing. Also, Victorian notions of 29 propriety prevented male physicians from looking at what they were doing; they often examined women with their hands under a sheet, while diverting their gaze away from the woman (Wertz and Wertz). Especially since they relied on forceps to demonstrate their expertise (and the reason women should pay extra fees for their attendance), these conditions created a problem: ?Physicians who had been trained to use forceps only on manikins and who were required by custom to perform the operation without the benefit of sight ran considerable risk of creating new problems for women whose obstructed labors they tried to ameliorate (Leavitt 46). In fact, until obstetric science improved so that doctors had a better grasp of the physiological event they were dealing with and until physicians learned from bacteriologists that washing their hands between exams could prevent infection, almost any intervention by the physician created the potential for harm. If a birth could not proceed without help, the physician provided a life-saving service not available elsewhere. If, however, as was statistically more probable, labor was proceeding normally and physicians intervened anyway, their actions introduced dangers not otherwise present. In the last decades of the nineteenth century and early into the twentieth, physicians knew that infection was a problem, but there was widespread disagreement about the cause of it. They focused on maintaining cleanliness, but what this meant and how to achieve it remained a mystery (Leavitt 156-59). Even so, the promise of cleanliness?and therefore, safety?is what drew many women into the new hospitals of the early twentieth century in the 1920s and 30s. The promise of safer birth did not immediately come to fruition; in fact, despite some hospitals elaborate prophylactic routines designed to eradicate puerperal fever, including giving the patient an enema, shave, bath, and 30 regular doses of quinine, maternal mortality due to infection did not start to significantly decline until the 1930s and 40s (Wertz and Wertz). The hospital provided an environment where asepsis alone was not enough: because doctors believed the quicker they got the birth over with, the more likely they would avoid harm, they intervened regularly and often caused wounds that served as breeding grounds for bacterial infection. The combination of frequent operative deliveries, the possibility of doctors spreading germs from patient to patient during internal exams, and careless antiseptic routines created an environment where infection was far more likely to occur than at home. A better understanding of how to create a sterile environment and the availability of antibiotics to treat infection eventually brought the infection rate in hospitals down, but by that time, many midwives had ceased practicing and most women were attracted to the hospital for what they believed would be a safe, modern, and painless birth (Leavitt; Wertz and Wertz). DeLee is the obstetrician credited with developing what is now called the active management of labor, and his method was explicitly based on a belief that labor and delivery was inherently a ?pathologic process (qtd. In the first issue of the American Journal of Obstetrics and Gynecology, DeLee wrote, ?So frequent are these bad effects [of damage during labor] that I have often wondered whether Nature did not deliberately intend women should be used up in the process of reproduction, in a manner analogous to that of salmon, which dies after spawning? His procedure involved routine use of the forceps, aided by an episiotomy (a cut 31 made to the perineum with surgical scissors to widen the vaginal opening). Wertz and Wertz describe his regimen this way: the procedure he commended involved sedating the woman and allowing her cervix to dilate, making a cut of several inches through the skin and muscles of the perineum. While DeLee advocated for doctors to proactively intervene in every step of labor, upper and middle-class women clamored for the hospital to offer them more than safety: they demanded the elimination of pain and suffering. When first-wave feminists, suffragettes, and other women of privilege heard of something called ?Twilight Sleep, a German technique that promised painless birth, they demanded American doctors make it available to them. Doctors were at first resistant, as those that had attempted to replicate the process had deemed it ?unreliable and unsafe (Wertz and Wertz 150). By the 1930s, however, the highly publicized experiences of women who had been overseas to try it out and the organized effort by women to get their doctors to provide it was enough to convince the medical profession (Wolf 46-47). Twilight Sleep involved injecting women with morphine at the onset of labor, and then giving them doses of an amnesiac drug called scopolamine. The forces that drew women out of their homes and into the hospital were many and complex, but they were eventually successful. By 1945, around 70% of women delivered in hospitals, and by the 1950s, that number had increased to over 90% (Wertz and Wertz 134-35). Women no longer determined who was present at birth, and many of them did not remember the experience at all. I do not want to romanticize the pre-hospital era; certainly, there was nothing ideal about the dangers women faced as a regular part of their biological life. However, like Leavitt and other historians, I also think it is a mistake to see the move from home to hospital as one of unquestionable progress. The story is far more complicated than that, and it is important to account for what was lost in the transition, in addition to what was gained. Traditional midwifery was obliterated in many places, women lost knowledge about the birth process that once was a regular part of community life, and they also gave up much of the control they once had to determine the setting, attendant, and procedures they desired for their births.
Ask your partner to massage you you to be more relaxed in labour diabetes signs in toddler buy cozaar in united states online, (although you may? Read books like this one gestational diabetes signs symptoms purchase cozaar toronto, talk to your ?Gas and air (Entonox) midwife or doctor and attend antenatal classes if they are this is a mixture of oxygen and available in your area diabetes mellitus type 2 hindi buy cozaar 50mg otc. Try kneeling diabetes mellitus type 2 in urdu cozaar 25mg with mastercard, walking around Water can help you to relax How it works or rocking back and forwards blood sugar drop discount 50mg cozaar fast delivery. The water will be chance to practise using the mask kept at a temperature that is or mouthpiece if you attend an comfortable for you but antenatal class blood sugar magik zip buy generic cozaar 25 mg. It is probably most effective You are given an intramuscular during the early stages, when many injection. You might prefer How it works anaesthetic and opioid) are then to ask for half a dose initially, to Electrodes are taped onto your back administered through this tube. For most heart will need to be continuously women, an epidural gives complete monitored by a machine. Side effects sit up in a curled position, an w ill h lp There are no known side effects anaesthetist will clean your back. If your waters have broken, you a feeling of tingling or pins and effective pain relief. However, if will probably be told to go in to needles down one leg after having you would like to use any of these be checked. You will be taken to the in the room where you are labour ward or your room, where giving birth. Choose one that is loose and Water births preferably made of cotton, because you will feel hot during labour and Some hospitals have birthing will not want something tight. Speak having a home birth, then this to your midwife about the examination will take place at advantages and disadvantages home. Some women heart, and like to spend much of their labour in the bath as a way of easing the pain. You can also snack, although many women don?t feel very hungry and some feel nauseated. Pushing When the head is visible, the When your cervix is fully dilated, midwife will ask you to stop you can start to push when you feel pushing, and to pant or puff you need to during contractions: a couple of quick short breaths, blowing out through your mouth. Find a position that you prefer and which will make labour easier this stage is hard work, but your for you. You can have your baby lifted straight onto you before the cord is cut by your midwife or birthing partner. The third stage of prevent the heavy bleeding which Your baby may be born covered some women experience. Skin-to-skin contact really helps the baby is born, which will speed Babies start sucking immediately, bonding, so it is a good idea to up the delivery of the placenta. If you prefer, you can s ask the midwife to wipe your baby and wrap him or her in a blanket before your cuddle. Some babies need additional help to establish breathing and may be taken to the resuscitor in the room to be given oxygen. Most women will go About 1 baby in every 13 will into labour within a week either be born before the 37th week side of this date. Your baby will like breaking of the waters or a ?show this involves having a vaginal being close to you just after birth. If your baby doesn?t have an injection, oral baby is showing signs of distress, doses of vitamin K are available. If you need stitches or other doctors may be able to use drugs to treatments, it should be possible stop your contractions temporarily. You will probably be given injections Your midwife will help with this as of steroids that will help to mature much as they can. If Many multiple birth babies are born you have not, you should be offered prematurely. Sometimes a hormone drip head and, with a contraction is needed to speed up the labour. A ventouse ventouse are used to help the baby is not used if your baby is less out of the vagina. Both ventouse and forceps are safe and are used only when necessary for you and your baby. A local anaesthetic will usually be given to numb the birth canal if you have not already had an epidural or spinal anaesthetic. If your obstetrician has any concerns, you may be moved to a theatre so that a caesarean section can be carried out if needed. This will depend on how spinal anaesthesia, which minimises your pregnancy progresses, the risk and means that you are awake position of your babies and whether for the delivery of your baby (see the babies share a placenta. A general anaesthetic is sometimes used particularly Whenever a caesarean is suggested, if the baby needs to be delivered your doctor will explain why it very quickly. Do not hesitate to If you have an epidural or spinal Caesarean section ask questions. Planned (elective) caesareans A caesarean is ?elective if it is planned in advance. Your obstetrician and midwife will talk to you about the best and safest way for your breech baby to be born. For example, Triplets or more are almost there may be a midwife, an always delivered by elective obstetrician and two paediatricians caesarean section. External cephalic version the process of labour is the same You will usually be offered the Help and support but the babies will be closely option of an external cephalic monitored. If the baby is close to being born, it may be safer for you to have a vaginal breech birth. There is no way of knowing what your labour is going to be like or how each of you will cope, but there are many ways in which a partner can help. Breastfeeding gives your baby the best possible start in life as it has lots of bene? After that, giving your baby breastmilk alongside solid food Your baby: You: will help them continue to grow and develop. The World Health Ear infections Breast cancer Organization recommends Asthma Weak bones breastfeeding for two years later in life Eczema or longer. Breastfeeding protects your cancer baby from infections and Obesity Women who diseases. To keep yourself as Colostrum is sometimes baby will be getting to know each comfortable as possible, feed called ?liquid gold. Finding one amount of milk you produce will that is comfortable for both of settle. Your baby will be happier if you will help your baby feed as you keep them near you and feed well as possible. At night, your baby baby lying on your tummy, they the nose level with your nipple. This will make it easier to hold your baby so their neck, shoulders and back are supported and they can reach your breast easily. Some parents worry the head tipped back so that the tongue that breastfeeding will make it harder for their partner to bond can reach as much breast as possible. Tips for breastfeeding By the time a newborn baby starts crying, they will normally have. Try not to give your baby any nappies should then start to body make the right amount of other food or drink before the become more frequent, with milk and stop your breasts getting age of about six months. These hungrier, feed more stools should be at least Day 2?3 often, rather than the size of a? The Equality Bill (0300 100 0212) can explain the will make it clear that it is unlawful than one baby options and talk them through to force breastfeeding mothers Twins, triplets or more can be with you. The practicalities will depend on how old your baby 107 Expressing milk 3 Using your thumb and the rest of Expressing milk if your your? Different pumps suit different women, so ask 4 Release the pressure then repeat, for information to compare them. It is more effective to express milk With practice, and a little time, by hand than to use a pump in the milk will? The following suggestions should help: 1 Before you start, wash your hands thoroughly then gently massage your breast. Milk that has been frozen is still of your milk at the end of a feed In this case, your midwife might good for your baby and better than and gently rubbing it into your suggest that you give your baby formula milk. If your baby is unsettled at the Tender breasts, blocked breast and doesn?t seem satis? It is very important to carry to prevent the soreness, but it on breastfeeding as this will help is important to get support you get better more quickly. Aim to stroke the lumpy area with your will still need some cream for eat healthily as a family. If necessary, helps with both of these or health visitor or contact the they can prescribe antibiotics that National Breastfeeding Helpline. These may affect your baby as when you were pregnant) in the same way they affect you. The general advice for all adults which might be is to avoid eating more than one high in caffeine. However, we do know your partner and especially bad for breastfeeding, you can choose that alcohol passes through to the your baby. One of the best things to do so as part of a healthy baby in very small amounts in your you can do for your own and your balanced diet, unless you are breastmilk. You can get help from a peer online from the Association supporter, your midwife or health All these voluntary organisations of Breastfeeding Mothers visitor. The following voluntary There may be specialist drop-ins in organisations can also provide your area where you can go if you information and advice: have a speci? Once opened, the cleaning and sterilising the following new advice is based the carton should be stored in the instructions on page 116. If you are using a and even though tins and packets cold water steriliser, shake off any of milk powder are sealed, they excess solution from the bottle and Sterilising the teat or rinse the bottle with can contain bacteria such as Cronobacter sakazakii (formerly All the equipment used for feeding cooled boiled water from the kettle known as Enterobacter sakazakii) your baby must be sterilised. If the feed is not prepared safely, the preparation area clean, you will Don?t put them on the work surface. Formula must therefore be made up with water the following cleaning and hot enough to kill the bacteria at sterilising instructions apply whether least 70? If you are Rinse all equipment in cold, clean using formula, mix the formula and running water before sterilising. Throw every 24 hours, and leave away unused formula within two feeding equipment in the hours. Make sure the openings of the bottles and teats are facing For information about using bottled down in the steriliser. Shake the bottle until It is important to use only the scoop the powder dissolves. Don?t add sugar formula milk can increase the or cereals to the feed in the bottle. To cool it, hold Get everything you need ready When feeding, make sure you keep the bottle, with the cap covering before you start feeding. It will continue to heat up for alone to feed with a propped-up formula feeding, talk to your a time after you take it out of the bottle, as they may choke. See microwave, even though the outside the list of useful organisations of the bottle may feel cold. They come in different be hot when you use it, otherwise shapes and with different hole any bacteria in the milk powder sizes, and you may have to try At the end of the feed, sit and might not be destroyed. If you need to use bottled water, remember that any bottled water that is labelled ?natural mineral water might contain too much sodium for babies. If you are giving bottled water to babies under six months, you should boil and cool it just like tap water. Babies who within four hours, take it out of are allergic to cows milk may also 9 If you think your baby might be the cool bag and store it at the be allergic to soya. Always get When this is not possible, feeds their advice before using soya-based should never be stored for longer than 24 hours. Some babies bring up more milk Breastfed babies do not need any If your baby brings up a lot of milk, than others during or just after a water. They may feel a little left out, especially if they have to leave you and the baby in hospital and return to an empty home. For a lot of mothers, the excitement and the pleasure of the new baby far outweigh any problems. A midwife will be available in your community to help you look after yourself and your baby. These the thought of passing urine can If you have had stitches, bathe the are both because feeding causes the be a bit frightening at? While unless you want to get pregnant breastfeeding you may notice that (see page 135 for your different the discharge is redder or heavier. If you are breastfeeding, you may not have another period until you stop feeding, or even for some weeks or months after that. Let the midwife know whenever you see anyone lot bigger than you were before if you feel very uncomfortable. If you prefer that your baby doesn?t have an injection, oral doses of vitamin K are available. Within 72 hours of hearing loss early means that practitioner to make sure birth, another more detailed babies and parents can get everything is all right. It will probably be a Newborn blood Cord care year or more before the bones close spot screening (belly button) over. Keep rare but potentially serious More information the navel clean and dry until this illnesses.
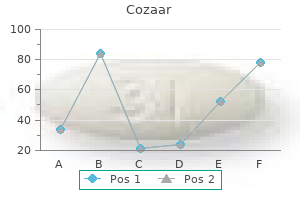
Antibiotics: to guard against pneumonia which is liable to develop after prolonged resuscitation zonulin type 1 diabetes cheap 25 mg cozaar with amex. Drugs : the most well documented are: Drug Effect I Antibiotics Streptomycin Nerve deafness diabetes signs of diabetes order cozaar 25mg line. Diagnosis and Differential Diagnosis: Cephalhaematoma Caput Succedaneum Develops hours or days after birth diabetes medicine himalaya buy generic cozaar. Sudden compression and decompression of the head as in breech and precipitate labour diabetes symptoms excessive sweating cozaar 25mg with mastercard. Prematurity due to physiological hypoprothrombinaemia diabetes urine order cozaar 50mg, fragile blood vessels and liability to trauma diabetes treatment centers of america buy cozaar 25 mg fast delivery. Subdural : results from damage to the superficial veins where the vein of Galen and inferior sagittal sinus combine to form the straight sinus. Subarachnoid: the vein of Galen is damaged due to tear in the dura at the junction of the falx cerebri and tentorium cerebelli. In (1) and (2) it is usually due to birth trauma, in (3) and (4) the foetus is usually a premature exposed to hypoxia. Forceps delivery: carried out by an experienced obstetrician respecting the instructions for its use. Lumbar puncture: is diagnostic and therapeutic to relieve the intracranial tension if the anterior fontanelle is bulging. The pain is due to increased intrauterine pressure 10-12 1 with each contraction to 25 mmHg or more and due to cervical dilatation. The highest degree of pain felt during the transitional period between the first and second stage. Breathing and relaxation exercises: increases the oxygen supply to the contracting myometium so ischaemia is reduced and pain is minimised. Complications: it may cause neonatal hypothermia, hypotonia and respiratory depression. It should not be given 2 hours before delivery to avoid foetal respiratory depression. It has more potent analgesic effect but more depression to the foetal respiratory centre so it should not be given 4 hours before delivery. The antidote of narcotic analgesics is Naloxone 5 g/ kg body weight into the umbilical vein. It abolishes the perineal reflex leading to prolonged second stage and hence increased incidence of instrumental delivery. El-Mowafi It is the safest and simplest technique but time should be allowed to establish analgesia. Complications of General Anaesthesia: (I) Foetal : Depression of the respiratory centre and asphyxia. During induction: occlude the oesophagus by cricoid pressure and guard the trachea by cuffed endotracheal tube. During recovery: remove the tube in lateral position with the head lower down and only when the patient is conscious. Hypotension: because block of the sympathetic nerve supply to the lower part of the body leads to peripheral vasodilatation. Accidental dural puncture: There is a 50% possibility of a low pressure headache which lasts for few days from leakage of cerebrospinal fluid into the epidural space. These cause initiation and increase in frequency, strength and duration of uterine contractions. Before delivery of the foetus as it will cause foetal asphyxia and rupture uterus. Direct obstetric deaths: resulting from obstetric complications of pregnancy, labour or puerperium and from interventions, omissions and/or incorrect treatment. Indirect obstetric deaths: resulting from previously existing disease or a disease that developed during pregnancy, labour or puerperium. Accidental deaths: not related to pregnancy, labour or puerperium itself but happened during it. Maternal age: the golden age for fertility and childbearing is between 18 and 35 years, the risk is more both to the mother and foetus with more deviation below or above this range. Proper intranatal monitoring by clinical observation, cardiotocography and partogram. Indications: (I) Maternal: (1) Hypertensive disorders with pregnancy: i Severe pre-eclampsia. El-Mowafi Modified Bishop Score: this score is predicting for the succession of induction of labour. The total score is in the range of 0-13, a score of 9 or more is favourable for successful induction. In most of the cases with favourable bishope score labour is commenced within 24 hours. No side effects, complications or contraindications as regard the mother or the foetus. Spontaneous uterine contractions start without medication or surgical interference. The procedure can be repeated for unlimited times and caesarean section must not be the alternative if it fails. These can be administered via many routes (see ecbolics) but the commonest are: (A) In living foetus: q Prostaglandin E vaginal tablet 3 mg (Prostin) is applied deep in the 2 posterior fornix. A drip of normal saline is connected to it to pass extra-amniotic in a rate of 1 ml / minute. Hindwater (high) amniotomy: the Drew-Smythe catheter is introduced between the membranes and uterine wall to a point above the presenting part. Method of administration : the initial rate of administration is 6 m units/ minute, increased by 6 m units/ minute every 15 minutes up to a maximum of 36 m units/minute or until 3 contractions/ 10 minutes are achieved. Ultrasound is sound waves above this audible range and for diagnostic purposes it ranges between 2. The transducer of the ultrasound machine contains piezoelectric crystals previously were made of quartz but now these are synthetic crystals. These crystals have the property of changing the electric to sound waves and vice versa. The electric current supplied to the machine generates ultrasound waves from these crystals to be reflected from tissue interfaces at various depths and by different echoes according to the nature of the medium i. The reflected sound waves is re-transformed again into electric waves presented as dotes or lines on the ultrasound screen. The ultrasound waves can pass through fluid and solid media but not effectively through gases,so a gel should be applied between the transducer and skin. In abdominal ultrasonography, the full bladder is essential for effective transmission of the waves and delineation of the pelvic organs in gynaecological and first trimester obstetric diagnosis. El-Mowafi Modes: (I) A (Amplitude) mode: It is a unidimensional system used to measure the depth of structures not used in obstetrics. Real-time: 40 images or more are obtained per second so that the movement of the structures is shown. This can be achieved by 3 different techniques: i Linear : giving a rectangular image (more convenient for obstetric examination). Multiple pregnancy: may be detected in the early weeks but diagnosed reliably by 16 weeks. Different types of abortion including blighted ovum, threatened, inevitable, incomplete, complete and missed abortions. Hazards of Ultrasound: Up till now, there is no data about any deleterious effects on the foetus or the mother. Localisation of placental site (the old methods of head displacement from the symphysis pubis or placentography). All these indications are now covered by ultrasound and radiodiagnosis is nearly out of modern obstetrics due to its hazards. Death of the embryo or teratogenicity particularly if used in the first trimester. Obstetric Diagnosis the diagnosis in medicine depends upon the triad of history, examination and investigations. Certain occupations are carrying the risk of teratogenicity as radiation technicians. Some diseases are common or endemic in certain areas as rheumatic heart in dark humid areas. In each pregnancy ask about: i duration of pregnancy, ii any complication during it, iii mode of termination, iv the offspring (male or female, alive or dead), v the puerperium or postabortive period, vi the time of last delivery or abortion. Fundal level : is detected by the ulnar border of the left hand starting from the xiphisternum downwards after centralising the uterus. The consistency of the uterus is detected which may be: i Cystic : in polyhydramnios. So G3 P1 +1 means 3 pregnancies, one delivery and one abortion 4 Duration of present pregnancy : in weeks. Full diagnosis may be like; 4th gravida, 2nd para + 1, pregnant 38 weeks, cephalic, L. Bleeding at expected time of menstruation may occur in the first trimester but not after that due to obliteration of the decidual space. This gives a high false results due to interfering factors as maternal obesity, ascitis, polyhydramnios, multiple pregnancy. Types: (A) Long curved obstetric forceps: It consists of 2 blades each of them is 15 inches (37. El-Mowafi There are 2 common types of axis traction piece: i Neville Simpson Barnes: is the commoner one composed of a single bar attached to the handle just behind the lock. Minimal pelvic curve which is again nullified by a slight bend between the blade proper and the shank so it is nearly a straight forceps allowing rotation and extraction of the head by a single application. Knobs on the handle: on the side of the minimal pelvic curve and should be directed toward the foetal occiput during application. Rotation: in deep transverse arrest, persistent occipito posterior and mento posterior. Indications of Forceps Delivery: (I) Prolonged 2nd stage: file:///D|/Webs On David/gfmer/Books/El Mowafi/forceps. El-Mowafi It is prolongation for more than 1 hour in primigravidae or 30 minutes in multiparae. Sagital suture is in anteroposterior diameter, right or left occipito-anterior or posterior. The leading point of the skull is at station +2 or more and divided into: i-Rotation? El-Mowafi Mid forceps the head is engaged, but the leading point is above station +2. Cephalic application: the forceps is applied on the sides of the foetal head in the mento-vertical diameter so injury of the foetal face, eyes and facial nerve is avoided. Pelvic application: the forceps is applied along the maternal pelvic wall irrespective to the position of the head. Cephalo-pelvic application : It is the ideal application and possible when the occiput is directly anterior or posterior or in direct mento-anterior position. How to know Right and Left Blades: Putting in consideration that the mother is in the lithotomy position, the blade will be applied with the pelvic curve directed anteriorly and the cephalic curve directed medially. If the blade will be applied to the left maternal side it is a left blade and vice versa. Technique of Forceps Delivery: (A) In occipito anterior position: q the left blade is applied first. It is held by its handle between the thumb and fingers of the left hand almost parallel with the right inguinal ligament and passed along the left side of the maternal pelvis between the guiding palm of the right hand and foetal head. El-Mowafi q As the blade passes into the birth canal the handle is carried backwards and towards the midline. The operator cannot place more than a finger tip between the fenestration of the blade and the foetal head. The posterior fontanelle is not more than one finger breadth above the plane of the shanks. Traction should be: gentle by the force of the arm only, intermittent with uterine contractions only, in correct direction i. The wandering method: the anterior blade is guided into the lateral side of the pelvis with the cephalic curve facing the foetal head. The direct method: when the head is low down in the pelvis, the anterior blade is slid between the head and symphysis pubis with the cephalic curve facing the foetal head. The old (classical) method: the anterior blade is applied with the cephalic curve towards the symphysis pubis then it is rotated 180o to fit with the head. This method is not recommended as the lower uterine segment and bladder may be injured. Complications of Forceps Delivery: (A) Maternal complications: file:///D|/Webs On David/gfmer/Books/El Mowafi/forceps. Reassessment: the forceps is removed and the patient is re-examined to detect the cause and correct it if possible. Caesarean section: is indicated in uncorrectable causes as cephalo-pelvic disproportion, and contracted outlet. A rubber tube attaching the cup to a glass bottle with a screw in between to release the negative pressure. A manometer fitted in the mouth of the glass bottle to declare the negative pressure. Another rubber tube connecting the bottle to a suction piece which may be manual or electronic creating a negative pressure 2 that should not exceed 0.
Discount cozaar 50mg on-line. Type 1 Diabetes Walk 2014.
References
- Anderson RM, Bloomer WE, Kay JH. Suspension of Aortic Cusps for Correction of Aortic Insufficiency Annals of Surgery. 1961.
- Andersen M, Dahlstrand C, Hoye K: Double-blind trial of the efficacy and tolerability of doxazosin in the gastrointestinal therapeutic system, doxazosin standard, and placebo in patients with benign prostatic hyperplasia, Eur Urol 38(4):400n409, 2000.
- Blaivas M, Adhikari S. An unseen danger: frequency of posterior vessel wall penetration by needles during attempts to place internal jugular vein central catheters using ultrasound guidance. An unseen danger: frequency of posterior vessel wall penetration by needles during attempts to place internal jugular vein central catheters using ultrasound guidance. Crit Care Med. 2009;37(8):2345-2349.
- Turba UC, Uflacker R, Hannegan C, et al: Anatomic relationship of the internal jugular vein and the common carotid artery applied to percutaneous transjugular procedures. Cardiovasc Intervent Radiol 28:303-306, 2005.
- Kim SP, Frank I, Cheville JC, et al: The impact of squamous and glandular differentiation on survival after radical cystectomy for urothelial carcinoma, J Urol 188:405n409, 2012.
- Gray, R. B. & Gottlieb, N. L. (1976). Rheumatic disorders associated with diabetes mellitus: Literature review. Seminars in Arthritis & Rheumatism, 6, 19n34.