Cynthia Moreau, PharmD, BCACP
- Assistant Professor
- College of Pharmacy
- Nova Southeastern University
- Fort Lauderdale, Florida
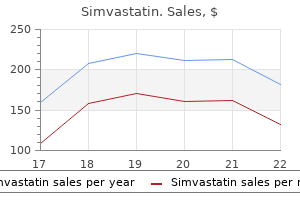
There are no data regarding the most appropriate method of identification of patients who may safely be retreated with Herceptin after experiencing a severe infusion reaction cholesterol content in eggs during the laying period buy 20 mg simvastatin otc. Prior to resumption of Herceptin infusion cholesterol vap test simvastatin 20 mg otc, the majority of patients who experienced a severe infusion reaction were pre-medicated with antihistamines and/or corticosteroids cholesterol test on empty stomach buy simvastatin 40 mg on line. While some patients tolerated Herceptin infusions ldl cholesterol level definition order 5 mg simvastatin visa, others had recurrent severe infusion reactions despite pre-medications cholesterol average male cheap 40mg simvastatin fast delivery. In post-marketing reports cholesterol sphingomyelin ratio cheap simvastatin 10mg line, use of Herceptin during pregnancy resulted in cases of oligohydramnios and oligohydramnios sequence manifesting as pulmonary hypoplasia, skeletal abnormalities, and neonatal death. Verify the pregnancy status of females of reproductive potential prior to the initiation of Herceptin. Advise pregnant women and females of reproductive potential that exposure to Herceptin during pregnancy or within 7 months prior to conception can result in fetal harm. Advise females of reproductive potential to use effective contraception during treatment and for 7 months following the last dose of Herceptin [see Use in Specific Populations (8. Pulmonary toxicity includes dyspnea, interstitial pneumonitis, pulmonary infiltrates, pleural effusions, non-cardiogenic pulmonary edema, pulmonary insufficiency and hypoxia, acute respiratory distress syndrome, and pulmonary fibrosis. Such events can occur as sequelae of infusion reactions [see Warnings and Precautions (5. Patients with symptomatic intrinsic lung disease or with extensive tumor involvement of the lungs, resulting in dyspnea at rest, appear to have more severe toxicity. The incidence of septic death was similar among patients who received Herceptin and those who did not [see Adverse Reactions (6. The most common adverse reactions which resulted in discontinuation of treatment on the Herceptin containing arm in the absence of disease progression were infection, diarrhea, and febrile neutropenia. Adjuvant Breast Cancer Studies the data below reflect exposure to one-year Herceptin therapy across three randomized, open-label studies, Studies 1, 2, and 3, with (n = 3678) or without (n = 3363) trastuzumab in the adjuvant treatment of breast cancer. The data summarized in Table 3 below, from Study 3, reflect exposure to Herceptin in 1678 patients; the median treatment duration was 51 weeks and median number of infusions was 18. Among the 3386 patients enrolled in the observation and one-year Herceptin arms of Study 3 at a median duration of follow-up of 12. In Study 3, a comparison of 3-weekly Herceptin treatment for two years versus one year was also performed. The rate of asymptomatic cardiac dysfunction was increased in the 2-year Herceptin treatment arm (8. More patients experienced at least one adverse reaction of Grade 3 or higher in the 2-year Herceptin treatment arm (20. The safety data from Studies 1 and 2 were obtained from 3655 patients, of whom 2000 received Herceptin; the median treatment duration was 51 weeks. Metastatic Breast Cancer Studies the data below reflect exposure to Herceptin in one randomized, open-label study, Study 5, of chemotherapy with (n = 235) or without (n = 234) trastuzumab in patients with metastatic breast cancer, and one single-arm study (Study 6; n = 222) in patients with metastatic breast cancer. Among the 464 patients treated in Study 5, the median age was 52 years (range: 25? Eighty-nine percent were White, 5% Black, 1% Asian, and 5% other racial/ethnic groups. All patients received 4 mg/kg initial dose of Herceptin followed by 2 mg/kg weekly. Among the 352 patients treated in single agent studies (213 patients from Study 6), the median age was 50 years (range 28? Most of the patients received 4 mg/kg initial dose of Herceptin followed by 2 mg/kg weekly. In the Herceptin plus chemotherapy arm, the initial dose of Herceptin 8 mg/kg was administered on Day 1 (prior to 13 chemotherapy) followed by 6 mg/kg every 21 days until disease progression. Cisplatin was 2 administered at 80 mg/m on Day 1 and the fluoropyrimidine was administered as either 2 2 capecitabine 1000 mg/m orally twice a day on Days 1?14 or 5-fluorouracil 800 mg/m /day as a continuous intravenous infusion Days 1 through 5. Median duration of Herceptin treatment was 21 weeks; median number of Herceptin infusions administered was eight. Following initiation of Herceptin therapy, the incidence of new-onset dose-limiting myocardial dysfunction was higher among patients receiving Herceptin and paclitaxel as compared to those receiving paclitaxel alone in Studies 1 and 2, and in patients receiving one-year Herceptin monotherapy compared to observation in Study 3 (see Table 6, Figures 1 and 2). This analysis also showed evidence of reversibility of left ventricular dysfunction, with 64. In the metastatic breast cancer trials, the probability of cardiac dysfunction was highest in patients who received Herceptin concurrently with anthracyclines. Infusion Reactions During the first infusion with Herceptin, the symptoms most commonly reported were chills and fever, occurring in approximately 40% of patients in clinical trials. Symptoms were treated with acetaminophen, diphenhydramine, and meperidine (with or without reduction in the rate of Herceptin infusion); permanent discontinuation of Herceptin for infusion reactions was required in < 1% of patients. Other signs and/or symptoms may include nausea, vomiting, pain (in some cases at tumor sites), rigors, headache, dizziness, dyspnea, hypotension, elevated blood pressure, rash, and asthenia. In the post-marketing setting, severe infusion reactions, including hypersensitivity, anaphylaxis, and angioedema have been reported. Anemia In randomized controlled clinical trials, the overall incidence of anemia (30% vs. The most common site of infections in the adjuvant setting involved the upper respiratory tract, skin, and urinary tract. Fatal respiratory failure occurred in 3 patients receiving Herceptin, one as a component of multi-organ system failure, as compared to 1 patient receiving chemotherapy alone. In Study 3, there were 4 cases of interstitial pneumonitis in the one-year Herceptin treatment arm compared to none in the observation arm at a median follow-up duration of 12. Metastatic Breast Cancer Among women receiving Herceptin for treatment of metastatic breast cancer, the incidence of pulmonary toxicity was also increased. Pulmonary adverse events have been reported in the post-marketing experience as part of the symptom complex of infusion reactions. Pulmonary events include bronchospasm, hypoxia, dyspnea, pulmonary infiltrates, pleural effusions, non-cardiogenic pulmonary edema, and acute respiratory distress syndrome. Thrombosis/Embolism In 4 randomized, controlled clinical trials, the incidence of thrombotic adverse events was higher in patients receiving Herceptin and chemotherapy compared to chemotherapy alone in three studies (2. Of patients receiving Herceptin as a single agent for the treatment of metastatic breast cancer, 25% experienced diarrhea. An increased incidence of diarrhea was observed in patients receiving Herceptin in combination with chemotherapy for treatment of metastatic breast cancer. Renal Toxicity In Study 7 (metastatic gastric cancer) on the Herceptin-containing arm as compared to the chemotherapy alone arm the incidence of renal impairment was 18% compared to 14. Treatment discontinuation for renal insufficiency/failure was 2% on the Herceptin-containing arm and 0. In the post-marketing setting, rare cases of nephrotic syndrome with pathologic evidence of glomerulopathy have been reported. The time to onset ranged from 4 months to approximately 18 months from initiation of Herceptin therapy. Pathologic findings included membranous 20 glomerulonephritis, focal glomerulosclerosis, and fibrillary glomerulonephritis. The incidence of antibody formation is highly dependent on the sensitivity and the specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to Herceptin with the incidence of antibodies to other products may be misleading. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Providers should consider additional monitoring and/or treatment as clinically indicated. If possible, physicians should avoid anthracycline-based therapy for up to 7 months after stopping Herceptin. If Herceptin is administered during pregnancy, or if a patient becomes pregnant while receiving Herceptin or within 7 months following the last dose of Herceptin, health care providers and patients should immediately report Herceptin exposure to Genentech at 1-888-835-2555. Risk Summary Herceptin can cause fetal harm when administered to a pregnant woman. In post-marketing reports, use of Herceptin during pregnancy resulted in cases of oligohydramnios and of oligohydramnios sequence, manifesting as pulmonary hypoplasia, skeletal abnormalities, and neonatal death [see Data]. There are clinical 21 considerations if Herceptin is used in a pregnant woman or if a patient becomes pregnant within 7 months following the last dose of Herceptin [see Clinical Considerations]. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. Clinical Considerations Fetal/Neonatal Adverse Reactions Monitor women who received Herceptin during pregnancy or within 7 months prior to conception for oligohydramnios. If oligohydramnios occurs, perform fetal testing that is appropriate for gestational age and consistent with community standards of care. Data Human Data In post-marketing reports, use of Herceptin during pregnancy resulted in cases of oligohydramnios and of oligohydramnios sequence, manifesting in the fetus as pulmonary hypoplasia, skeletal abnormalities, and neonatal death. These case reports described oligohydramnios in pregnant women who received Herceptin either alone or in combination with chemotherapy. In one case, Herceptin therapy resumed after amniotic index improved and oligohydramnios recurred. Animal Data In studies where trastuzumab was administered to pregnant Cynomolgus monkeys during the period of organogenesis at doses up to 25 mg/kg given twice weekly (up to 25 times the recommended weekly human dose of 2 mg/kg), trastuzumab crossed the placental barrier during the early (Gestation Days 20 to 50) and late (Gestation Days 120 to 150) phases of gestation. The resulting concentrations of trastuzumab in fetal serum and amniotic fluid were approximately 33% and 25%, respectively, of those present in the maternal serum but were not associated with adverse developmental effects. Published data suggest human IgG is present in human milk but does not enter the neonatal and infant circulation in substantial amounts. Trastuzumab was present in the milk of lactating Cynomolgus monkeys but not associated with neonatal toxicity [see Data]. This consideration should also take into account the trastuzumab wash out period of 7 months [see Clinical Pharmacology (12. Data In lactating Cynomolgus monkeys, trastuzumab was present in breast milk at about 0. Infant monkeys with detectable serum levels of trastuzumab did not exhibit any adverse effects on growth or development from birth to 1 month of age. Contraception Females Herceptin can cause embryo-fetal harm when administered during pregnancy. Advise females of reproductive potential to use effective contraception during treatment with Herceptin and for 7 months following the last dose of Herceptin [see Use in Specific Populations (8. The risk of cardiac dysfunction was increased in geriatric patients as compared to younger patients in both those receiving treatment for metastatic disease in Studies 5 and 6, or adjuvant therapy in Studies 1 and 2. Limitations in data collection and differences in study design of the 4 studies of Herceptin in adjuvant treatment of breast cancer preclude a determination of whether the toxicity profile of Herceptin in older patients is different from younger patients. In Study 7 (metastatic gastric cancer), of the 294 patients treated with Herceptin, 108 (37%) were 65 years of age or older, while 13 (4. Herceptin (trastuzumab) for injection is a sterile, white to pale yellow, preservative-free lyophilized powder with a cake-like appearance, for intravenous administration. Total trastuzumab clearance increases with decreasing concentrations due to parallel linear and non-linear elimination pathways. Although the average trastuzumab exposure was higher following the first cycle in breast cancer patients receiving the three-weekly schedule compared to the weekly schedule of Herceptin, the average steady-state exposure was essentially the same at both dosages. The pharmacokinetics of trastuzumab in patients with severe renal impairment, end-stage renal disease with or without hemodialysis, or hepatic impairment is unknown. Drug Interaction Studies There have been no formal drug interaction studies performed with Herceptin in humans. Clinically significant interactions between Herceptin and concomitant medications used in clinical trials have not been observed. Paclitaxel and doxorubicin: Concentrations of paclitaxel and doxorubicin and their major metabolites. Docetaxel and carboplatin: When Herceptin was administered in combination with docetaxel or carboplatin, neither the plasma concentrations of docetaxel or carboplatin nor the plasma concentrations of trastuzumab were altered. Cisplatin and capecitabine: In a drug interaction substudy conducted in patients in Study 7, the pharmacokinetics of cisplatin, capecitabine and their metabolites were not altered when administered in combination with Herceptin. No evidence of mutagenic activity was observed when trastuzumab was tested in the standard Ames bacterial and human peripheral blood lymphocyte mutagenicity assays at concentrations of up to 5000 mcg/mL. In an in vivo micronucleus assay, no evidence of chromosomal damage to mouse bone marrow cells was observed following bolus intravenous doses of up to 118 mg/kg of trastuzumab. Patients with a history of active cardiac disease based on symptoms, abnormal electrocardiographic, radiologic, or left ventricular ejection fraction findings or uncontrolled hypertension (diastolic > 100 mm Hg or systolic > 200 mm Hg) were not eligible. Paclitaxel was administered either weekly (80 mg/m) or every 3 weeks (175 mg/m) for a total of 12 weeks in Study 1; paclitaxel was administered only by the weekly schedule in Study 2. Herceptin was administered at 4 mg/kg on the day of initiation of paclitaxel and then at a dose of 2 mg/kg weekly for a total of 52 weeks. Radiation therapy, if administered, was initiated after the completion of chemotherapy. The data from both arms in Study 1 and two of the three study arms in Study 2 were pooled for efficacy analyses. Similar demographic and baseline characteristics were reported for the efficacy evaluable population, after 8. Patients were randomized (1:1:1) upon completion of definitive surgery, and at least four cycles of chemotherapy to receive no additional treatment, or one year of Herceptin treatment or two years of Herceptin treatment. Herceptin was administered with an initial dose of 8 mg/kg followed by subsequent doses of 6 mg/kg once every three weeks. A protocol specified interim efficacy analysis comparing one-year Herceptin treatment to observation was performed at a median follow-up duration of 12. Among the 3386 patients randomized to the observation (n = 1693) and Herceptin one-year (n = 1693) treatment arms, the median age was 49 years (range 21? Prior to randomization, 94% of patients had received anthracycline-based chemotherapy regimens. Radiation therapy, if administered, was initiated after completion of chemotherapy.
Portal hypertension leads to profound systemic and splanchnic vasodilatation and intravascular volume depletion cholesterol levels history purchase simvastatin 40 mg fast delivery. This increases renal vasoconstriction via both the renin?angiotensin?aldosterone pathway and sympathetic nervous system activation cholesterol test dublin purchase simvastatin us. The diagnosis is based on the absence of primary kidney disease cholesterol levels for 60 year old woman purchase 20mg simvastatin visa, proteinuria cholesterol check up fasting purchase simvastatin canada, or systemic hypovolemia causing renal hypoperfusion cholesterol levels in child simvastatin 20mg for sale. There is normal urinary sediment test of cholesterol discount simvastatin uk, low urinary sodium (<10 mEq/L), uremia, and oligu ria. Despite low platelet counts, platelet adhesion and aggregation might be normal, because of increased endothelial production of von Willebrand factor. Thrombin then triggers the formation of a strong clot made of fibrinogen and platelets that can withstand fibri nolysis. Thromboelastography/thromboelastometry can determine the quality of clot forma tion (generation of thrombin), clot strength (the effect of fibrinogen and platelets), and fibrinolysis. Other common causes include portal hypertension and varices, endothelial dysfunction, renal failure, and disseminated intravascular coagulation. Basic intraoperative monitoring includes central venous and intraarterial pressure monitoring. Echocardiography is a powerful tool to assess major hemodynamic changes and guide inotropic therapy. It also can detect major complications early such as intracardiac thromboembolism or air embolism. Anesthesia for Liver Transplantation 503 response laboratory service with rapid turnaround times and blood bank services are essential. The operation is divided into 3 phases: preanhepatic, anhepatic, and the neohepatic phases. Compression or occlu sion of major blood vessels can cause further hemodynamic compromise. This phase ends in the clamping of the inferior vena cava, portal vein and hepatic artery, and removal of the liver. The presence of portal varices and other new vessels in patients with longstanding cirrhosis can ameliorate this effect. Care must be taken not to overcompensate with significant volume expansion, because this volume will return to the circulation upon unclamping. The resulting hypervolemia can lead to venous congestion and poor function of the new liver. With partial return of blood from the inferior vena cava to the heart, hemo dynamics are usually more stable than with a full clamp. Venovenous bypass: Venous blood from the inferior vena cava and femoral vein is returned into the internal jugular vein using extracorporeal venovenous cannulas and a centrifugal pump. As the vena cava is unclamped, adequate return of venous blood volume to the heart is restored. The portal vein is then opened, causing the cold, acidotic, hyperkalemic blood from below the clamp and from the liver graft itself to circulate directly into the right heart. This can cause a significant decrease in blood pressure, bradycardia, other arrhythmias, and occa sionally cardiac arrest. Severe hypotension upon unclamping is called reperfusion syndrome and can be ameliorated by administration of calcium chloride, bicarbonate, epinephrine, and vasopressin. Warm ischemia is very damaging to the graft, and thus limiting warm ischemia time is critical to graft function. The neohepatic phase consists of the hepatic artery and bile duct anastomoses, often with a concomitant cholecystectomy. During this time, the anesthesiologist is looking for signs that the new liver is beginning to function?improvement in acidosis and clearing of lactic acid, and improved hemostasis and production of bile. Hemosta sis requires excellent surgical skills, temperature control and the early diagnosis and treatment of fibrinolysis. Failure to do so leads to breakdown of existing clots and the development of diffuse bleeding. Maintenance of a low central venous pressure may reduce venous bleeding during hepatectomy. Treatment of abnormal laboratory values such as low platelet counts, low fibrin ogen, and high prothrombin times is only required if there is clinical bleeding. These laboratory values frequently normalize as the new graft functions and platelets return to the circulation from the spleen. In case of bleeding, patients are treated with factor replacement, blood, and platelets. Approaches to resuscitation and treatment of high blood loss differ by institution. Renal dysfunction, with poor urine output and rising creatinine, may occur during transplantation, especially after a full caval clamp, long anhepatic time, or prolonged hypotension. Patients with volume overload, hyperkalemia, or hyponatremia may benefit from continuous venovenous hemodialysis that can be instituted in the oper ating room or upon arrival to the intensive care unit. They must meet usual standard Anesthesia for Liver Transplantation 505 extubation criteria. In some institutions, extubated patients with good liver function can bypass the intensive care unit and are sent to the postoperative recovery unit and then to a regular surgical floor or step-down unit. Occasionally, the abdominal distension owing to an especially large organ or tissue swelling might prevent primary closure of the surgical wound. Abdominal closure can be delayed for several days af ter transplantation to prevent abdominal compartment syndrome. Function of the new graft must be moni tored closely, looking especially for signs of infection, bleeding, and acute rejection. Some patients with bleeding or graft dysfunction may require emergent return to the operating room. Patients may have a difficult postoperative course with significant multiorgan dysfunction, and these patients require expert intensive care. Does intraoperative hepatic artery flow pre dict arterial complications after liver transplantation? Evaluation and management of hepatic en cephalopathy: current status and future directions. Hepatic encephalopathy in chronic liver dis ease: 2014 Practice Guideline by the American Association for the Study Of Liver Diseases and the European Association for the Study of the Liver. Complications and use of intracranial pressure monitoring in patients with acute liver failure and severe encephalopa thy. Clinical management of acute liver fail ure: results of an international multi-center survey. Diastolic cardiac dysfunction is a predictor of dismal prognosis in patients with liver cirrhosis. Diastolic dysfunction in liver cirrhosis: prognostic predictor in liver transplantation? Effectively screening for coronary artery disease in patients undergoing orthotopic liver transplant evaluation. The prevalence of coronary artery dis ease in liver transplant candidates over age 50. Factors associated with major adverse cardiovascular events after liver transplantation among a national sample. Liver transplantation outcome in patients with angiographically proven coronary artery disease: a multi-institutional study. Intraoperative management of liver transplantation in patients with hypertrophic cardiomyopathy: a review. The perioperative management of patients undergoing combined heart-liver transplantation. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Dis eases and the American Society of Transplantation. Hepatopulmonary syndrome and liver transplantation: a recent review of the literature. Improved survival after liver transplantation in patients with hepatopulmonary syndrome. Retrospective analysis of the re sults of liver transplantation for adults with severe hepatopulmonary syndrome. Severe pulmonary hypertension and amelioration of hepatopulmonary syndrome after liver transplantation. Association between primary pulmonary-hypertension and portal-hypertension analysis of its pathophysiology and clinical, laboratory and hemodynamic manifestations. Survival in portopulmonary hypertension: Mayo Clinic experience categorized by treatment subgroups. International liver transplant society prac tice guidelines: diagnosis and management of hepatopulmonary syndrome and portopulmonary hypertension. Rebalanced hemostasis in patients with liver disease: evi dence and clinical consequences. Hemostasis in liver transplantation: pathophys iology, monitoring, and treatment. Intraoperative hypercoagulability during liver transplantation as demonstrated by thromboelastography. The coagulopathy of chronic liver disease: is there a causal relationship with bleeding? Transesophageal echocardiography during orthotopic liver transplantation: maximizing information without the distraction. Anesthesia for liver transplantation in United States academic centers: intraoperative practice. Postreperfusion syndrome during liver transplantation for cirrhosis: outcome and predictors. Effects of continuous octreotide infusion on intraoperative transfusion requirements during orthotopic liver transplantation. Contemporary care has been shaped by the PublishedOnline availability of more sensitive diagnostic techniques and the earlier use of therapeutic interventions, which have the January 23, 2018 potential to improve patients duration and quality of life. It is intended to MetroHealth Medical Center, the 2010 care considerations for Duchenne muscular serve as a pocket guide to overall disease management. These core therapies can decrease respiratory and Department of Pediatrics the near future. Spirometry Sleep studies with capnography might be necessary Correspondence to: should be initiated when the patient is 5?6 years of age. We also recommend public health entities such as the Immunization Action initiation of antibiotic therapy during acute respiratory For more on theImmunization Coalition,23 and Parent Project Muscular Dystrophy. Indications for nocturnally (expressed both as an absolute value and as a percentage assisted ventilation include signs or symptoms of hypo predicted on the basis of arm span or ulnar length), ventilation or sleep-disordered breathing, irrespective of maximum inspiratory and expiratory pressures, peak the level of pulmonary function; relevant symptoms cough fow, and blood oxygen saturation by pulse include fatigue, dyspnoea, morning or continuous head oximetry (SpO2) should be measured at least every aches, frequent nocturnal awakenings or difcult 6 months in all non-ambulatory individuals. However, some individuals remain asymp should be measured every 6 months or any time SpO is tomatic despite the presence of hypoventilation. Non-ambulatory respiratory management of patients undergoing surgery, individuals with symptoms of sleep-disordered breathing including indications for preoperative training in the should have sleep studies as often as annually, if use of assisted cough devices and non-invasive possible. When SpO2 is less than 95% on Therefore, supplemental oxygen therapy should not be room air, the frequency of assisted coughing should be used alone. The failing symptoms of hypoventilation such as dyspnoea, fatigue, myocardium is also at risk of life-threatening rhythm and difculty concentrating, despite their use of assisted abnormalities. Thus, referred to a cardiac specialist until late in the disease, patients often self-extend their use of assisted ventilation contributing to poor clinical outcomes. The cardiac management has been challenging because the indications for daytime-assisted ventilation are listed in New York Heart Association classifcation of heart fgure 1. The signs and symptoms of heart nasal ventilation with a bi-level pressure device overnight. Some centres use time on the ventilator (eg, 16 cardiologist should have clinical expertise in diagnosing h/day or more) as an indication for tracheostomy. A National Heart, Lung, and Blood Lung, and Blood Institutesee most clinical situations. Until the age of 10 years, individuals should available in case the primary ventilator malfunctions. With the of a night nurse can greatly decrease the risk of onset of heart failure symptoms or when abnormalities potentially catastrophic medical events, such as mucus are frst seen on cardiac imaging?eg, myocardial plugging of the trachea. After discussing potential benefts and Progressive myocardial fbrosis leads to ventricular risks with the family, the cardiologist could initiate dysfunction. Given the absence of Clinical manifestations of heart failure?fatigue, weight dystrophin-specifc targeted cardiac therapies, traditional loss, vomiting, abdominal pain, sleep disturbance, and treatment strategies for heart failure should be used. The cardiologist should double-blind placebo-controlled trial in patients maximise medical therapy for heart failure. Surveillance Bone health and osteoporosis management should include periodic Holter monitoring. The optimum frequency of monitoring has not combined with progressive myopathy, both of which are been established and should be directed by the key risk factors for reduced bone strength. The beneft of Vertebral fractures are frequently asymptomatic when implantable cardioverter defbrillators as primary identifed in children with glucocorticoid-treated ill prevention for ventricular tachycardia or ventricular nesses through a monitoring programme that includes a fbrillation is unknown. These devices can be used for lateral spine radiograph,69?73 so the true prevalence is secondary prevention in patients who have had probably higher than existing reports suggest. At untreated, vertebral fractures can lead to chronic back present, placement for primary arrhythmia prevention is pain and spine deformity, while leg fractures can cause on the basis of established adult heart failure guidelines. A left ventricular assist device could be used as a difcult; however, disease outcomes were favourable in destination therapy?ie, in individuals for whom a heart the defazacort-treated children, with associated transplant is not considered appropriate.
Generic 40mg simvastatin overnight delivery. Statin Side Effects: What Cholesterol Meds Are Doing to Your Brain - Audio Article.
Specialist commentator comments One specialist commentator noted that for out-of-hospital cardiac arrests caused by myocardial infarction cholesterol chinese food purchase simvastatin with paypal, using the AutoPulse could allow lifesaving interventions such as primary angioplasty (percutaneous coronary intervention) to be performed while compressions are maintained cholesterol on keto buy simvastatin 40mg free shipping. The instructions for use of the AutoPulse device say that it should only be used in adults over 18 years of age cholesterol test bupa purchase simvastatin canada. They suggested that some people who experienced traumatic cardiac arrest may beneft from automated chest compressions cholesterol risk factor buy 5mg simvastatin fast delivery, for example people who have a hypoxic aetiology such as hanging cholesterol test guildford buy simvastatin cheap, asphyxia and drowning cholesterol test results 4.5 order cheap simvastatin. A specialist commentator mentioned that there are currently 2 high-quality randomised controlled trials evaluating the use of the AutoPulse (Hallstrom et al. Risk factors for cardiac arrest include age (incidence increases with advancing age) and sex (men are at higher risk of experiencing sudden cardiac arrest). Another event (February 2013) concerning a nickel-metal hydride battery occurred because the battery did not have daily operational checks or battery swaps, and the battery was not fully charged. The third event (August 2012) is ongoing and only limited information is available, but it relates to an unexpected stop in AutoPulse compressions. Clinical eClinical evidencevidence A literature search identifed 2 randomised controlled trials (Wik et al. Five non-controlled observational studies (summarised in table 14), 2 case report studies and 1 conference abstract are also presented in this briefng. Inclusion and exclusion were determined after patient enrolment to avoid treatment delay. Of those randomised, 522 met post-enrolment exclusion criteria and for 12 people there was no survival to hospital discharge data available. No statistically signifcant differences in people with injuries were found between the 2 groups, although some injuries were more prevalent in 1 group than the other. Subgroup analysis was conducted based on the primary comparison population (cardiac arrests of cardiac aetiology at the time of emergency medical service arrival) and the non-primary population (cardiac arrests after emergency medical services arrival, non-cardiac aetiology, or advanced life support >90 seconds before study). The trial protocol allowed each emergency medical service site to choose from 3 options for resuscitation intervention. One site (site C) changed its resuscitation intervention from option 1 to option 2 half way through the study. Logistic regression found site C to be statistically signifcantly associated with worsening of survival to hospital discharge. Following the frst planned interim monitoring, the study enrolment was terminated for safety in every site. The re-analysis found that survival to hospital discharge decreased signifcantly after the protocol change at site C (19. Four-hour survival at site C decreased over time during the study period but increased at the other sites favourable to the AutoPulse (p=0. The authors concluded that the difference in survival appears to have been limited to 1 site after its protocol change. Paradis and colleagues responded, arguing that their analysis was merely hypothesis-generating. They also stated that although they did not dismiss the results from the original trial, they considered that it lacked homogeneity between the trial sites. Also, because the protocol allowed sites to change the execution during the trial, the potential harm from using the device seemed to be associated with site C following a change in the protocol at that site. A subgroup analysis of people in asystole or agonal rhythms also showed similar results (37% compared with 22%, p=0. The study population comprised adults who had non-traumatic cardiac arrest and were admitted to the emergency department, or whose cardiac arrest happened in the emergency department. Neurological (functional) status was assessed using the Glasgow-Pittsburgh outcome categories. The cause of death for the people of this study was not restricted to cardiac arrest of known cause. Causes of death included natural (67%), accidental (24%, primarily deaths due to drug toxicity), suicide (5%), homicide (3%) and undetermined (1%). No statistically signifcant differences were seen between the groups in fractures of the anterolateral, lateral, or posterolateral regions of the ribcage. Non-contrNon-controlled studiesolled studies Table 14 summarises 5 non-controlled studies that were identifed for this briefng. Despite similar return of spontaneous circulation results, the authors explained that 39. The authors stated that no comparisons were made because this was not the aim of the study. Although the AutoPulse is meant for use in adults aged 18 years or over with non-traumatic cardiac arrest, in this study the AutoPulse was used for people aged 15 years. Also, for 20 people, the cardiac arrest was caused by trauma, including chest (n=1), abdominal (n=2) or thoracic injuries (n=5). The new guidelines gave chest compressions a higher priority and stated that ventricular fbrillation should be treated with only 1 direct current shock, followed by chest compressions and ventilation without checking the rhythm or the pulse. Although a statistically signifcantly higher proportion of people obtained spontaneous circulation at admission, the 30-day survival was not signifcantly different between the 2 groups of people. Logistic regression analysis suggested that using the AutoPulse was associated with worse 30-day survival. However, the authors acknowledged that the use of the AutoPulse was not fully implemented in their unit: it was only used in 77 of 419 cardiac arrests (18%) after implementation of the guidelines. All people in this study were terminally ill from heart disease and had additional co-morbidities. Comparative and non-comparative studies suggest that use of the AutoPulse is not associated with worse outcomes. No statistically signifcant differences for survival were observed in 4 different studies (Jennings et al. One study observed superiority of the AutoPulse in terms of survival to admission and discharge (Ong et al. People were allocated to the design 2 comparison arms in a 1:1 ratio using randomised permuted blocks of 24 stratifed by study site. In some cases, inclusion and exclusion criteria were determined after the person was enrolled to avoid treatment delay. The analyses excluded people who were methods retrospectively found to meet exclusion criteria and people without survival to hospital discharge data. Variables associated with survival to hospital discharge were selected as covariates, including the age category of the person, witnessed arrest, initial cardiac rhythm, and enrolment site. One sided p-values for testing non-inferiority of each intervention arm were calculated. Of 4753 randomised people (2359 to the AutoPulse and 2394 to the manual group), 522 met post enrolment exclusion criteria. Follow-up duration was 4 hours for the primary outcome and up to discharge for the secondary outcomes. People whose cardiac arrest was treated by emergency medical service and subsequently determined not to meet the inclusion criteria were excluded from the analysis. Logistic regression using generalised linear mixed models was applied to compare the outcome of individual episodes between the 2 comparison groups. The model was adjusted for covariates previously demonstrated to predict survival as well as cluster (based on an emergency service station or group of stations). Subgroup analysis was conducted for a priori primary population and non-primary population respectively. People eligible: randomised people, excluding those who met the exclusion criteria (n=1071, including 554 in the AutoPulse group and 517 in the manual group). Primary comparison population: of those eligible, people who were in cardiac arrest at the time of emergency medical service arrival and whose cardiac arrest was considered to be of cardiac origin (n=767, including 394 in the AutoPulse group and 373 in the manual group). Non-primary population: of those eligible, people with cardiac arrest after emergency medical services arrival, non-cardiac aetiology, or advanced life support > 90 seconds before study (n=304, including 160 in the AutoPulse and 144 the manual group). Results There was no signifcant difference in survival to 4 hours between the AutoPulse group and the manual resuscitation group, either based on the randomised population (28. Score of 1: conscious and alert with normal function or only slight disability; 2, conscious and alert with moderate disability; 3, conscious with severe disability; 4, comatose or persistent vegetative state; and 5, brain dead or death from other causes. An overall performance category score of 1 indicates good overall performance; 2, moderate overall disability; 3, severe overall disability; 4, coma/vegetative state; and 5, brain death: certifed brain dead or dead by traditional criteria. Study Case-control study using prospectively collected case data matched to an design Australian emergency service data registry. Setting Three regional sites in mixed urban or rural settings of Ambulance Victoria, Australia; out-of hospital cardiac arrest cases using the AutoPulse from 1 October 2006 to 30 April 2010. Deriving and adjusting for propensity score was attempted to reduce selection bias introduced via non-random assignment of treatment groups. All controls were selected from regional settings similar to those of the AutoPulse trial sites (n=220). Results were similar using only bystander witnessed out-of-hospital cardiac arrest cases with presumed cardiac aetiology. Further research is warranted with prospective nature, randomisation and larger number of cases to investigate potential sub-group benefts of the AutoPulse including survival to hospital discharge. Cases were matched using exact matches for all values with the following prospectively defned criteria: age (?3 years), gender, presenting cardiac rhythm, number of shocks delivered, and number of doses of medication administered. Matching was performed by an investigator blinded to the treatment group and patient outcome. Differences between treatment groups in the primary outcome were determined with the Chi-square test. Inclusion/ Not specifed, but stated that the study population comprised adults with exclusion non-traumatic cardiac arrest occurring out of hospital or in the emergency criteria department over the study period. Primary Survival to hospital discharge, defned as the patient surviving the primary event outcomes and to discharge from the hospital. For each end point, logistic regression was used to compare the 2 comparison groups, adjusting for covariates that on univariate analysis were signifcantly different between treatment groups at p<0. Survival to hospital discharge showed no statistically signifcant difference in the AutoPulse phase than manual phase (3. Conclusions the authors concluded that a resuscitation strategy using the AutoPulse in an emergency department environment was associated with improved neurologically intact survival on discharge in adults with prolonged, non-traumatic cardiac arrest. Univariate comparisons using t tests, Chi-square tests, or Fisher tests were conducted to identify differences in distribution of covariates between phases. Outcome Frequency of rib fractures, sternum fractures, skin abrasions, visceral measures injuries. Population 46 adult people with out-of-hospital, non-traumatic cardiac arrest and a mean age of 66. Population 16 adult people (mean age 68?6 years) with in-hospital sudden cardiac arrest. Case reportsCase reports Two publications with 3 relevant case reports were identifed. A Mobile Emergency Care Unit then arrived, the AutoPulse was ftted to the patient and endotracheal intubation was performed. The patient was discharged from the hospital on day 11 after cardiac arrest with no signs of neurological defcits. The patient was discharged 12 days after the accident with no signs of neurological defcit. Autopsy revealed that the patient had a ruptured liver and spleen with 1 litre of abdominal blood. Other injuries included bilateral dorsal rib fractures, a fractured manubrium of the sternum and lateral cutaneous lacerations. AbstrAbstract fract from conferom conference prence proceedingsoceedings One study published as an abstract was identifed to be potentially relevant (Jalali et al. Effectiveness of the interventions was measured by return of spontaneous circulation, 6-hour survival, blood pressure and blood gas. Recent and ongoing studiesRecent and ongoing studies Two ongoing or in-development trials on the AutoPulse for cardiac arrest were identifed in the preparation of this briefng (Clinicaltrials. Estimated enrolment is 24 patients Costs and resource consequences No published evidence on resource consequences was identifed. In addition to the initial cost of the AutoPulse and essential components, there are ongoing costs associated with its use (such as LifeBands, replacement of batteries). Space in the ambulances must be allocated to the AutoPulse platform and essential items. Staff would need training to ensure that they can deploy the device in the minimum amount of time. However, it should be noted that the AutoPulse is normally an addition to the treatment pathway. Better neurological outcomes may lead to a decrease in subsequent treatment costs and a reduction in the duration of hospital stay following the cardiac arrest episode. Therefore, only those who met the inclusion criteria following treatment were included in the analysis. Due to the nature of the AutoPulse device it would be impossible to blind the patient, rescuer and outcome assessor to the intervention being delivered. However, allocation could have been concealed for data analysis to prevent a potential source of bias. The AutoPulse device was implemented at various stages of resuscitation; a protocol specifying device implementation at a set point of care might have produced different results. The training and experience of personnel using the device would potentially also impact on the effectiveness of the intervention. It was also impossible to standardise hospital-based post-resuscitation care at the study sites and centres.
Ascending located on the right side of the abdomen; effluent is high volume with a liquid-mush consistency ii cholesterol test meter simvastatin 5mg otc. Transverse located upper abdomen cholesterol test exercise cheap simvastatin 40 mg without a prescription, either in the middle or toward the right side of the body; effluent is a paste-like cholesterol testing cvs 40mg simvastatin amex, soft substance iii cholesterol in shrimp good or bad discount 20 mg simvastatin otc. Continent Ileostomy (Kock Pouch) located right lower abdomen just above pubic hair line; effluent is liquid ii cholesterol levels high risk discount 10 mg simvastatin mastercard. Ureterostomy two stomas; one on the right side of the abdomen and one on the left side of the abdomen 2 cholesterol test hdl ldl ratio simvastatin 5mg with mastercard. The type or construction of the stoma: end stoma, loop stoma, or a double-barrel stoma. A loop stoma is a stoma where both the upstream (proximal) and downstream (distal) openings of the bowel are brought out through the same place in the abdominal wall. The proximal opening of the stoma drains stool from the intestine, while the distal opening of the stoma (the mucous fistula) drains mucus. Double-barrel stoma two distinct stomas; one discharges stool, the second mucus. The bowel is severed and both ends are brought out onto the abdomen and two distinct stomas are made. One stoma is usually called the proximal stoma, while the other is called the distal stoma. The proximal opening of the stoma drains stool from the intestine, while the distal opening of the stoma (the mucous fistula) drains mucus. Short, hard plastic tube or flexible plastic catheter that is placed under the loop of the stoma i. Butterfly shaped bridge folds in half along a hinge and forms a convenient curved shape. Plastic Rod with Rubber Tubing: the rubber tubing is connected to both ends of the rod to prevent the rod from slipping out. The stoma should be over the middle of the rod and not pushed to one end of the rod. If the stoma rubs up against the end of the rod the stoma can sustain damage in the form of ischemia causing the tissue to die and slough off. Fine bore catheters inserted in urostomy surgery to prevent stenosis of the anastomosis between the ureter and the bowel. The ureteral stents originate in the renal pelvis, extend down the ureters, and exit 3 through the stoma. Brown melanosis coli a discoloration from excessive laxative use; lack of blood supply to the stoma 7. Edematous normal finding post-op; gradually decreases over 6-8 weeks after surgery 4. Moist the stoma is a mucous membrane and should always be moist with its own natural lubrication 6. Superficial bleeding that does not stop spontaneously, excessive bleeding, or prolonged bleeding may be indicative of a stoma complication. Bleeding as a stoma complication can result from inadequate hemostasis during stoma construction, portal hypertension, trauma, underlying disease, and because of some medications, such as prolonged use of analgesic anti 4 inflammatory drugs, blood thinners, and chemotherapy. Luminal bleeding (bleeding that comes from the lumen of the stoma) is often associated with underlying disease. It is normal to be able to see movement of the stoma; stomas expand and contract in a "wave-like motion" due to peristalsis. The height or protrusion of the stoma is important not only for proper drainage but also to conceal the stoma. The protrusion varies in length and can slightly retract or extend throughout the life of the stoma. The stoma height should be measured at the mucocutaneous junction where it attaches to the skin to top of stoma. Greater risk for injury from trauma, laceration or being folded or bent over into 7 the pouching system iv. Colostomy size varies as the width of the colon varies and therefore, stoma size will vary. Ureterostomy is a small stoma as it is created from the ureter which has small 8 diameter, compared to the ileal conduit which is created from the wider ileum. Irregular or oval stomas are measured using the clock method with for length and width. Accurate measurements of the stoma are important to track the progress of the ostomy but also to determine the correct size of the skin barrier and pouching 8 system. Measurements should be done frequently during the first six to eight weeks of the post-operative period. Line the center of the transparent ruler over the center of the stoma and measure according to ruler instructions. For appliance sizing measurement irregular stomas should be traced and a copy of the tracing should be recorded for appliance fitting. Be sure to line it up so that the tail of pouch will be in the appropriate direction. Most of the manufacturers will provide them free of charge, and most cut-to-fit products will contain one per box. The card comes with numerous pre-cut holes, measured in millimeters and/or inches. Select the hole in the card that fits closest around the base of the stoma without touching it. Postop Ileostomy Initial output: usually 12 24 hours postop dark green, 7 viscous, odorless ; as the patient eats the output will thicken. Consistency of output Thick, Viscous, Liquid, Pasty, Oily, Formed, Soft, Thin, Tarry, Bloody 3. Objectively recording flatus frequency (using a diary kept by the patient) is a first step in 10 evaluation if perceived excessive. Definition: the skin/stoma junction where the mucosa of the stoma is approximated to 8 the skin surrounding the stoma. This area should be treated as a wound until the junction of the skin and the mucosa are healed and sutures are removed. The mucocutaneous junction should be free of tension, infection, and skin breakdown. If a separation is noted between stoma and surrounding skin, document measurements 8 (width and depth) and location of the separation. Peristomal plane surface area that extends out from the base of the stoma in area of 8 approximately 4x4 inches (102mm x 102mm) 1. Assess peristomal plane at a minimum and extend assessment outward as needed based upon findings. The skin around the stoma should be intact, without erosion, rashes or lacerations. Redness may be caused by infection, irritation from drainage, urine/feces, dermatitis/trauma from tape or dressing b. Redness from infection may be seen as diffuse and indistinct, or as intense with demarcated borders, red streaking. In dark skin, the skin may appear purple or a gray hue or deepening of the ethnic skin color iv. Scars connective tissue reflective of dermal damage; new scars are pink and thick, over time become white and atrophic 3. Induration process of the skin becoming hard?; hardened mass with defined edges; detected by palpation (feeling) C. Throbbing, aching, squeezing, constant, intermittent, spasmodic, tender, crushing? Location of pain one site, several sites, does it move or radiate to another site, generalized or specific area b. Utilize pain severity scale, be consistent with the scale with each assessment, assess for severity at present, worst, and least levels. Developed as a comprehensive tool to use for documentation and grading of the peristomal skin. The scoring system allows the health care provider to compare and contrast the condition of the peristomal skin from one assessment to the next and make adjustments to care as necessary. The tool includes two simple approaches for obtaining information on the condition of the peristomal skin: a. Provides operational definitions for the consistent interpretation of peristomal skin lesions iii. A content validated measurement instrument to classify lesion type and location iv. An objective classification system to document the incidence of peristomal skin lesions v. Assessment and management of stomal complications: a framework for clinical decision making. Contact Information: Wound Care Education Institute Fax: 877-649-6021 Phone: 855-391-1556 Email: Info@wcei. Figure 1a A normal Figure 1b Multiple heart is shown on the echocardiographic left compared to a views of a normal heart with dilated heart on the left and cardiomyopathy on a heart with dilated the right. This condition is the most common form of cardiomyopathy and accounts for approximately 55?60% of all childhood cardiomyopathies. According to the pediatric cardiomyopathy registry database, this form of myopathy is detected in roughly one per 200,000 children with roughly one new case per 160,000 children reported each year in the United States. It is more commonly diagnosed in younger children with the average age at diagnosis being 2 years. When only subtle symptoms exist, infants and young children are sometimes diagnosed with a viral upper respiratory tract infection or recurrent pneumonia without realizing that a heart problem is the basis for these symptoms. Older children and adolescents are less likely to be diagnosed with viral syndromes and more likely to present with decreased exercise capacity or easy fatigability. In older children, congestive heart failure can manifest as diffculty breathing and/or coughing, pale color, decreased urine output and swelling, excessive sweating, and fatigue with minimal activities. Until the diagnosis is made in many children, chronic coughing and wheezing, particularly during activities, can be misinterpreted as asthma. Symptoms of rhythm problems include palpitations (feeling of funny or fast heart beats), syncope (fainting), seizures (convulsions), or even sudden cardiac arrest (heart stops beating effectively requiring resuscitation). These symptoms can occur at any age and with any stage of cardiomyopathy, even if other more severe symptoms of congestive heart failure have not yet appeared. With this test, your physician will be using ultrasound beams to evaluate the heart looking for dilated chambers and decreased pump function. Along with the echocardiogram, there are other tests that will likely be done to confrm the diagnosis or provide clues as to the cause. A chest X-ray will show the heart size and can be used as a reference to follow increases in heart size that may occur over time. To more completely evaluate for the presence or absence of these abnormal heart rhythms, which may effect treatment, your doctor may also order a Holter monitor which records heart beats over a 24?48 hour period. A treadmill test can also be useful in some children (beyond age 5?7 years) who can cooperate with this study. In many cases, no cause is discovered, and the cardiomyopathy may be referred to as idiopathic (cause unknown). Many heart failure specialists believe this idiopathic form of the cardiomyopathy is genetic. While genetic screening has not yet become a standard procedure, some physicians may send blood to molecular testing labs located in a few centers around the country so that limited genetic testing can be performed looking for possible mutations currently known to cause dilated cardiomyopathy. If your physicians believe the cause is genetic (especially common in older children and adolescents), evaluation, usually with echo, of other family members is recommended to rule out presence of this disease in other close relatives (parents, siblings). A cardiac biopsy, which involves removing tiny pieces of heart muscle for inspection under the microscope, may be performed to help distinguish between infectious and genetic causes. The information provided during the catheterization may also be helpful if transplantation is being considered as one of the treatment options for your child. The choice of a specifc therapy depends on the clinical condition of the child, the risk of dangerous events and the ability of the child to tolerate the therapy. The most common types of medications used to treat heart failure include diuretics, inotropic agents, afterload reducing agents and beta-blockers. Diuretics, sometimes called water pills, reduce excess fuid in the lungs or other organs by increasing urine production. The loss of excess fuid reduces the workload of the heart, reduces swelling and helps children breathe more easily. Common side effects of diuretics include dehydration and abnormalities in the blood chemistries (particularly potassium loss). Inotropic medications and are most commonly used intravenously to support children who have severe heart failure and are not stable enough to be home. Side effects include low heart rate, and, with high blood levels, vomiting and abnormal heart rhythm. Side effects include increased heart rate, arrhythmias and for some, constriction of the arteries. Afterload Reducing Agents reduce the work of the heart by relaxing the arteries and allowing the blood to fow more easily to the body. Side effects include low blood pressure, low white blood cell count, high potassium levels and kidney or liver abnormalities. Beta-blockers slow the heartbeat and reduce the work needed for contraction of the heart muscle.
References
- Midulla PS, Dapunt OE, Sadeghi AM, et al. Aortic dissection involving a double aortic arch with a right descending aorta. Ann Thorac Surg. 1994;58:874-5.
- Levitan RM, Ochroch EA, Stuart S, et al: Use of the intubating laryngeal mask airway by medical and nonmedical personnel. Am J Emerg Med 18:12, 2000.
- Kock M, Blomberg S, Emanuelsson H, et al: Thoracic epidural anesthesia improves global and regional left ventricular function during stress-induced myocardial ischemia in patients with coronary artery disease, Anesth Analg 71:625, 1990.
- Wesnes SL, Hunskaar S, Bo K, et al: Urinary incontinence and weight change during pregnancy and postpartum: a cohort study, Am J Epidemiol 172:1034n1044, 2010.