Shannon M. Bates, MD, CM
- Department of Medicine
- McMaster University
- Henderson Research Centre
- Hamilton, Ontario, Canada
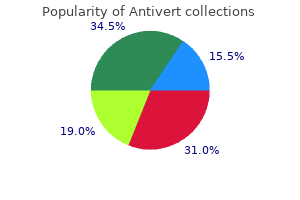
By contrast symptoms after embryo transfer purchase antivert online now, trauma the degree of variation observed for both indicators is services provided by trauma units are commissioned predominantly related to case-mix medications related to the integumentary system cheap antivert 25mg on-line. The return of data reduced consciousness or shock are brought to major from trauma units needs to be improved to enhance trauma centres which will have been alerted to arrival the quality of data on which decisions are based by ambulance services medications harmful to kidneys purchase antivert without prescription. This enables the trauma concerning the commissioning medications known to cause weight gain cheap 25 mg antivert amex, planning and provision centre to activate urgent imaging before the patient of trauma services treatment 4 ringworm buy cheap antivert 25mg online. Radiology Success accessed at a later point in time for those patients who Factors symptoms panic attack best order antivert. Fractures (complex): assessment and report, ?Major trauma care in England?: management. The indicator technique in which an incision is made in both groins shown in Map 10 provides a proxy for monitoring the to access the femoral artery. The England there were no differences in total mortality or value for 2012/13-2014/15 was 10. After intervention the risk of the stentbetween 2009/10-2011/12 and 2012/13-2014/15. Systematic review and meta-analysis of population-based mortality from ruptured abdominal aortic aneurysm. Systematic review and meta-analysis of the early and late outcomes of open and endovascular repair of abdominal aortic aneurysm. Open Repair for Abdominal Aortic Aneurysm in Patients Aged 80 years and Older: Systematic Review and Meta-Analysis. Endovascular stent-grafts for the treatment of percentile gap between 2009/10-2011/12 to 2012/13abdominal aortic aneurysms. Based on an assumption that there is no difference in prevalence of aneurysms (>5. The value for all Trusts in commissioners continue to monitor arrangements for England is 48%. Endovascular stent-grafts for the treatment of Commissioners need to work with service providers abdominal aortic aneurysms. It is unlikely, however, that this factor Osteoporosis involves a gradual loss of calcium from explains all of the variation observed. As this the bones which results in the bones becoming indicator has been designed to take account of the thinner, more fragile and more likely to break. Osteoporosis regarding diet, physical exercise and smoking Resources for Primary Care. Commissioners need to specify to service providers Management of osteoporosis and the prevention of that all patients who experience a fragility fracture fragility fractures. Furthermore, the bowel needs to be prepared only with an enema before the procedure, There are several methods available for imaging the whereas a colonoscopy requires strong laxatives to large bowel (colon), particularly in the diagnosis of clear the bowel. Thus, flexible sigmoidoscopy is safer cancer of the colon, including: for the patient, and is particularly useful if there is. In survival outcomes in England, including that for the 2011 national colonoscopy audit Scotland and colorectal (bowel) cancer. Although not all colonic Northern Ireland had higher rates of colonoscopy investigations are done because of the suspicion of 2 than England. Barium enema is an X-ray procedure that creates Magnitude of variation images of the large intestine. The England value for 2014/15 was access to colonoscopy and flexible sigmoidoscopy or 13. The statistical significance of changes in the three variation For the improved diagnosis of colorectal cancer, commissioners need to specify that service providers: measures or the median was not tested for those indicators with fewer than three data periods. Guidelines for colorectal cancer the use of barium enema for the primary diagnosis screening and surveillance in moderate and high risk of colorectal problems is one of the issues addressed groups (update from 2002). Colonoscopic surveillance for preventing colorectal cancer in adults with ulcerative colitis. Computed tomographic colonography (virtual review with service providers and bowel surgeons: colonoscopy). It provides a checklist of objectives that the most productive endoscopy services apply. There was no studies, but surveillance is increasingly being significant change in any of the three variation accepted as an important way of preventing measures between 2005/06 and 2014/15. One reason for variation in the rate of gastroscopy In general, the rate of gastroscopy (Map 19) needs to procedures is differences in regional cancer rates, be at a level at which cancers can be detected in which in turn are affected by smoking habit and people aged over 55 years. The degree of variation dyspepsia and reflux are being followed observed, however, is greater than can be explained appropriately, the percentage of people undergoing by variations in the incidence and prevalence of gastroscopy procedures who are aged under 55 disease. The England value for 2014/15 was commissioners and providers develop referral criteria 35. It provides a checklist of the the most plausible reason for warranted variation in objectives that the most productive endoscopy the percentage of gastroscopy procedures is services apply systematically to ensure endoscopy variation in the age profile of the populations. Applying the ?Appropriateness item reassures commissioners that referrals are vetted against best practice. Gastro-oesophageal reflux disease and dyspepsia in adults: investigation and management. It is more likely to identify in 2011, 91% of respondents referred patients for flat vascular or inflammatory lesions than radiological capsule endoscopy. Throughout this large extent by testing the patient with a dissolvable period the distribution of values has been strongly ?patency capsule before the main test in at-risk positively skewed. Patients at higher risk of retention are people with: There has been significant widening of all three measures of variation. One reason for the degree of variation could be differences in the level of access to capsule endoscopy. If the Of the well-delineated uses of endoscopic ultrasound probe is immediately adjacent to the area ultrasound, that for the diagnosis of suspected of interest the images are much clearer, and targeted pancreatic malignancy is the most established and biopsy is more accurate and more likely to show a investigated. As with any endoscopic procedure, patients and allow sampling from adjacent pelvic should be warned of the risk of perforation. It takes a long time for clinicians to develop the the therapeutic use of endoscopic ultrasound occurs knowledge, skills and experience necessary to use primarily in specialist units following discussion within the technique, and the equipment is expensive. Endoscopic ultrasoundguided drainage of pancreatic fluid collections There are a variety of conditions in which endoscopic (arising as a complication of pancreatitis) is safe and ultrasound can be used as a diagnostic tool, effective, and is increasingly being performed as the including: technique of choice for draining accessible. The complication rate disease, including unsuspected gallstones for the drainage of pancreatic fluid collections is between 5% and 20%. It is not stomach and oesophagus commonly performed at present, but its use is likely to increase in future. There was no significant change in any of the three variation measures between 2005/06 and 2014/15. The degree of variation observed is unlikely to be due to differences among local populations of the prevalence of the conditions for which endoscopic ultrasound is indicated. There are, however, intervention rates is also likely to reflect variation no data available on the ?appropriate number of in the number of paediatric endoscopists and endoscopies per population to improve clinical gastroenterologists which may may lead to different outcomes. The England obviate the need for endoscopy (Murch et al; see value for this period was 130. Section B Part 1 Service for paediatric endoscopy at some centres specifications. This is urgently needed to maximise endoscopy: European Society of Gastrointestinal yield and reduce unnecessary risk to patients. In the Global Burden of Disease 2013 study it was found that for people of all ages ?age-related and Although 35,000 children and 1. Half of the people with a hearing loss can be Over the next 20 years the impact of hearing loss will managed effectively by a care package including increase: hearing aids and other environmental aids to reduce. The 2035 over 13 million people in England will have assessments determine functional ability, possible hearing loss. The England value for accreditation through the Improving Quality in this quarter was 5. The best of clinical pathway a timely manner to minimise its broader social and redesign. See pages 14 and 39-43 for information on service providers need to understand: Audiology including two case-studies. Commissioning Services for People with Hearing Loss: A framework for clinical commissioning groups. There are more lower activity when compared with studies than 80 recognised sleep disorders, which may affect undertaken via the respiratory referral route the timing, quality and quantity of sleep. Reasons for this increase may be: apnoea, restless leg syndrome, narcolepsy, and sleep problems associated with Parkinson?s disease. During sleep, muscles in the upper sleep studies and result in additional referrals airway relax to a greater degree than normal or parts of the airway become blocked for one of several In addition there may be a demand for certain groups reasons, resulting in apnoeas or pauses in breathing of patients, such as professional/commercial drivers lasting from 10 seconds to two minutes. In conjunction with physical assessment, included in the denominator and therefore it shows history-taking, blood tests and X-rays, spirometry is actual population coverage. In calculating significant change in any of the three variation coverage practices are allowed to except appropriate measures between 2012/13 to 2014/15. Primary care staff, Min 60 however, are often inadequately trained or use poor-quality equipment. Chronic obstructive pulmonary disease in reach used in the best-performing practices adults. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? Urodynamic testing is an umbrella term, which predominantly involves the measurement of pressure Magnitude of variation and flow. It enables the clinician to determine what physical factors are involved in bladder disorders. This indicates no substantial trend in the short to medium term, with There was a small decrease in the median, which the average rate of testing of 1. This rate may need to increase nature of the fall and the relatively high number of in future to reflect an increase in the prevalence and periods over which the decrease was observed. Clinical surveillance of carpal tunnel syndrome in two areas of the United Kingdom, 1991-2001. Although aneurysms can the socioeconomic profile of local populations, occur in any artery, one of the common places for however, is known to affect rates of screening aneurysm formation is the abdominal aorta. The England value for 2014/15 was populations can affect the number of conclusive 79. The statistical initial non-visualised scan need to be scanned at the significance of changes in the three variation medical imaging unit of the local vascular service. Continuing appropriate to an individual?s circumstances, Professional Development for Screening. The map and column chart display the latest timepoint (31 March 2015), during which local authority Map 31: Boxplot of people with test result in the values ranged from 37. Max 70 95 60 Max the boxplot shows the distribution of local authority 95 75 60 Median values at 31 March 2015. One possible reason for unwarranted variation is differences in local systems for the follow-up of Median 52. Guidelines for colorectal cancer screening and surveillance in moderate and high risk groups (update from 2002). In England breast cancer is less common in women living in the most-deprived areas, although these Coverage for women aged 53-70 years was 75. The outcome for women Magnitude of variation diagnosed in the most-deprived areas is poorer when compared with women diagnosed in the leastthe map and column chart display the latest timedeprived areas: overall, one-year survival is 94% and point (31 March 2015), during which local authority 97%, respectively. The aim of breast the boxplot shows the distribution of local authority screening is to reduce mortality from breast cancer values for the period 31 March 2010 to 31 March by detecting the condition at an early stage when 2015. There was no significant change in any of the there is the possibility of effective treatment. The influence of this leaflet on acceptance rates may differ according to the profile of the local population served. All screening services need to seek advice and support from the screening quality assurance service where there are issues with adherence to national targets for screening round length. Women aged 25-64 years are invited for cervical screening: those aged 25-49 years are invited every Magnitude of variation three years, and those aged 50-64 years are invited every five years. Both commissioners and primary care providers need to understand the barriers to women attending for cervical screening, and to initiate strategies to address any barriers identified. The England value for this service values for the period April-June 2014 to Julyquarter was 95. Output and information that babies affected by any of the conditions do requirements specification: for the Child Health not suffer serious harm from avoidable incidents Information service and systems. The key giving children a better chance of developing speech performance indicator relating to referral for and language skills, and of making the most of social audiological assessment is: and emotional interaction from an early age. The test can take receive audiological assessment within the place in hospital, in an outpatient clinic or at home by required timescale. Babies that miss screening should receive it as soon as possible, but not after three Reducing the degree of variation in the percentage of months of age. Min 40 30 Reasons for warranted variation include differences in the levels of risk, multi-morbidity and genetic 20 aetiologies in different geographical areas. Therefore, commissioners and service factors affecting a baby?s parents, including providers need to work together to investigate the constraints on their ability to travel and/or financial interface between local screening services, constraints. Continuing weeks of referral, commissioners need to specify that Professional Development for Screening: Newborn all hearing screening service providers: Hearing Screening e-learning. Continuing (see ?Resources?), and supporting documents to Professional Development for Screening: Screener ensure that a hearing screening programme is training. In the first deform and break down intermittently leading to instance screening is offered to all pregnant women, blocked blood vessels.
When the same quantities of hairs are spread out with smaller grafts medications you can crush discount 25 mg antivert fast delivery, they give the appearance of more coverage medicine 5852 buy discount antivert 25mg online. Incisions made for micrograft procedures heal very quickly in comparison to other surgical methods of hair restoration treatment wpw generic antivert 25mg without a prescription, resulting in a very short ?under construction period treatment pancreatitis discount antivert 25 mg without a prescription. The donor area is closed with a single fine line of sutures medications used to treat anxiety safe 25mg antivert, and is well camouflaged by the thicker hair at the back of the head treatment 911 buy antivert 25 mg on-line. The recipient sites where the grafts are placed are fine slits made with a miniature surgical blade, and these heal very rapidly. Many micrograft patients return to work a day or two after the procedure, and no one is aware of the work that was done. This is in contrast to the two weeks or longer for healing that is allowed for full size grafts and for incisions made for scalp reductions, lifts, and flaps. Each micrograft procedure is designed to stand alone, meaning that no additional procedures are required, and that the transplanted hairs will look natural decades in the future even as hair loss progresses. By placing micrografts over the entire balding surface of the 103 Chapter Twelve scalp, as well as between growing hairs in adjacent areas that will likely lose hair, a skilled surgeon will avoid creating an ?island of dense hair surrounded by thinning hair as hair loss continues years in the future. Micrografting allows for additional procedures to be performed, as the patient desires. I have had some patients express a desire for the densest possible coverage, anticipating several successive micrografting procedures; however, after a single procedure grows out they are satisfied with their new hair just the way it is. And I?ve also had patients who initially indicate they want only a single procedure, with just enough coverage to give them some hair on the top or on the back of their heads. Then after a single procedure, they decide to have a few more, in order to achieve maximum density. This is in contrast to the original large grafts (plugs), which required the full series of procedures to fill in the spaces between grafts in order to avoid the ?doll?s hair look. With original large plug grafts, if the patient elected not to have all the recommended procedures done, the transplant looked unfinished. Or, if the surgeon miscalculated the degree of future hair loss, an island of dense hair may emerge as the surrounding fringe receded. Micrografting is also employed to enhance previously performed full size graft procedures, as well as to cover scars from scalp reductions, scalp lifts, and flap procedures. In contrast to more elaborate hair restoration techniques such as scalp lifts and scalp flaps, micrografting has a low risk of medical complications. Unlike scalp lift and flap procedures, with micrografting the patient does not receive general anesthesia, and is awake during the entire procedure. General anesthesia alone presents a significant risk of medical complications, and is avoided entirely with micrografting. Other medical complications, while always a possibility with any surgical procedure, are rare with micrografting. In addition to being medically safe, micrografting is a safe cosmetic procedure as well. A single micrografting procedure almost always produces excellent or very good appearing results, and even a poor micrograft transplant is usually cosmetically acceptable and can 104 Follicular Unit Micrografting be enhanced or corrected. In contrast, more elaborate scalp lift and flap procedures can produce remarkable results with a single surgical session; however, they can also produce disastrous cosmetic results when everything does not go right. Patches of dead scalp tissue and large unsightly scars are examples of complications that have occurred with scalp lifts and flaps. During the 1990s, many variations of micrografting emerged, with each technique claiming to have special advantages. Examples of variations in micrografting included monografting, megasessions, the use of graft cutting and placement machines, laser hair transplants, and follicular unit micrografting. It seemed to be a natural evolution from the original full-size pluggy grafts containing up to fifteen hair follicles, to minigrafts having three to five hairs, to micrografts having one to three hairs. The theory was that individually placed hair follicles would give the most natural appearance of all. With this procedure, single-hair grafts were meticulously sculpted to almost bare follicles, and then placed into tiny recipient sites usually made with a surgical needle. Unfortunately, the extensive cutting that was necessary to isolate individual hair follicles resulted in a loss of many donor follicles and a relatively high graft failure rate, and the appearance of the surviving grafts was one of overall fuzziness that did not look natural. The idea behind megasessions was to solve a patient?s hair loss problem in a single surgical procedure. The problem was that each graft had to be trimmed extensively, and the grafts had to be placed very close together. The excessive cutting increased the risk of graft failure from the rough treatment of the thousands of individual grafts. Initially, most responsible hair restoration surgeons avoided placing more than 105 Chapter Twelve 2,000 grafts in a single session in order to reduce risk to the limited supply of donor follicles. As the techniques improved, the number of grafts per session increased up to 5,000 grafts in one session. One device was a ?graft-cutting machine that sectioned the strips of donor tissue into uniform ?grafts, in much the same way that a hard-boiled egg slicer would slice an egg into uniform pieces. While this device saved a considerable amount of time and labor, it could cut the tissue without regard to where the hair follicles were located, or their angles of orientation. While some of the sliced hair follicles survived, and on occasion two halves even survived and regrew as two small hair follicles, many more perished, and the device never caught on. Only a few hair transplant surgeons have used graft-cutting machines successfully, and typically with patients having very straight coarse hair. I had the opportunity to see this procedure done by a good hair transplant surgeon using only one assistant. The main drawback to this procedure is that more hairs are lost in the preparation and the patient should have straight hair. Another attempt at automation was a hand-held graft implantation device that was first loaded with uniformly cut grafts, which the machine then placed into the patient?s scalp in much the same manner as a carpenter?s nail gun places nails into a roof. In addition to either requiring the aforementioned machine-cut grafts, or very carefully hand-cut grafts, this machine did not seem to actually save much time, and it never became very popular. When used to place the grafts close together, the automatic implanters tend to push out the grafts next to them. More accurate and more densely placed grafts could be accomplished by using a fine blade to make the incision and tedious, meticulous placement using two forceps by experienced placement surgical technicians. The donor material was harvested the same way as for other micrograft procedures, but the recipient sites were made with a laser. The most sophisticated laser hair transplants used computerized scanning devices to make tiny slots for each graft. A problem inherent with using a laser is thermal damage to the cells surrounding the opening made by the laser. Grafts placed into laser slots also heal more slowly, and the patient looked ?under construction for a considerably longer time than with other micrografting methods. Some laser transplant surgeons claimed that the recipient slots made by the laser resulted in a more ?natural graft than slits made with steel instruments; however, most surgeons could not perceive a benefit, and certainly not when weighed against the considerable expense of buying or leasing the laser. Laser transplantation allowed for high technology advertising claims, but the procedure never really caught on. The first is maximizing the yield and survival of the limited supply of donor hair follicles throughout every stage of the surgical procedure. Many subtle refinements of the micrografting surgical technique comprise a follicular unit transplant procedure, and combined together these refinements give the best possible results. The first way in which a follicular unit micrografting procedure may differ from some of the micrografting variations of the past is careful planning to avoid harvesting too many grafts for a single transplant session. Almost every patient wants as much hair density added in as few sessions as possible; however, placing too many micrografts too close together increases the risk of graft failure. Despite the ability to harvest and place many more grafts, a follicular unit micrograft 107 Chapter Twelve surgeon will choose to do only 1,000 to 2,000 grafts in a single session. The main limitation to the number of grafts per session is the issue of supply and demand. In most patients with extensive balding the donor area is usually much less dense as well as being smaller in size. I would estimate that only one patient in one hundred would be a candidate for 5,000 grafts, two in a hundred may qualify for 4,000 grafts leaving the majority getting 1,000 to 2,500 per session. The donor material harvesting method is another refinement that has become a standard part of follicular unit micrografting. In the past, many surgeons used a multi-bladed scalpel to remove the donor tissue from the back of the scalp. All the blades in this surgical instrument were parallel, and were set about three millimeters apart. With a multi-bladed knife, the donor material was removed already cut into long strips, and individual grafts were then more easily cut from the strips. This method caused many hair follicles to be cut by the scalpel blades, and a high percentage of these cut follicles did not survive. Follicular unit surgeons now use a single-blade scalpel to remove the donor tissue from the scalp, and then cut the donor tissue into grafts under high magnification, working to avoid cutting the hair follicles. Immediately after the donor material is removed Donor material is removed from the patient, it is from the patient. A few hours can elapse from the time the donor tissue is removed to when a particular hair follicle is placed into the scalp, and keeping the follicles cool and moist helps them survive better during this time. After the grafts are cut they are placed onto surgical pads moistened with saline solution, and these pads are placed into trays that are chilled as well. The use of stereomicroscopes to cut the donor material into grafts is another standard component of follicular unit micrografting. In the early stages of micrografting, eye loupes and magnifying glasses were commonly used to aid the process of cutting donor tissue into strips and pieces, and eventually into individual grafts; however, a considerable number of hair follicles were cut due to poor visibility even under high magnification. Stereomicroscopes have separate eyepieces for each eye, which allows for a more three-dimensional view of the donor tissue. Stereomicroscopes require additional training for the team of medical assistants who cut the grafts; however, their use Stereomicroscope results in less follicle transection, meaning they avoid splitting hairs. To further improve visibility during graft preparation, and to keep the donor tissue cool, I have removed the standard halogen spotlights from all of my graft preparation microscopes and have installed cool fluorescent light panels, which illuminate the grafts from underneath. Cool fluorescent transillumination helps to make small dormant hair follicles and follicles containing very fine light-colored hairs 109 Chapter Twelve more visible, further increasing yield. This lighting enhancement also avoids heat damage to the donor tissue that incandescent lighting from the overhead can cause. The most significant of all micrografting refinements, and the concept that gives the follicular unit procedure its name, is the preservation of the naturally occurring clusters of hair follicles during graft preparation. Transplant surgeons have observed that many hair follicles on the scalp occur in pairs or bundles of three or four follicles, which are called follicular units. Preserving follicular units intact as micrografts reduces the risk of inadvertently cutting follicles occurring close together, which results in grafts growing more viable hairs, and also produces grafts that grow hairs in more natural clusters. In the early years of micrografting procedures, the hair restoration surgeon would develop a plan for the quantity and size of the hair grafts for a particular procedure. The team of medical assistants may have been instructed to produce 600 single-hair grafts, 500 2-hair grafts, and 400 3-hair grafts for a procedure calling for 1,500 total grafts. The team of medical assistants then cut grafts from the donor tissue according to the surgeon?s requirements, and if a certain number of two-hair grafts were needed, clusters of hair follicles were cut apart into two-hair grafts. This inevitably resulted in some accidental cutting and loss of some hair follicles. Donor material is cut into A follicular unit micrografts 110 Follicular Unit Micrografting With follicular unit transplant procedures, the medical assistants preparing the grafts use their judgment to identify and cut around follicular units, producing grafts containing one, two, or three hairs according to how many follicular units naturally occur in the donor tissue. Finally, the follicular unit micrografts are placed into tiny slits made in the scalp with a miniature scalpel. The slits are made in a slightly irregular manner, to avoid creating a pattern of rows as the grafts begin to grow new hairs. In the early days of micrografting, surgeons were careful to allow adequate space between each graft, and a variation of a grid pattern was used to make recipient sites. With follicular unit micrografting, adequate space is allowed between grafts; however, the grafts are placed in a more random and natural looking manner. The technique is similar to the original 4mm full-sized graft technique in that the hair is harvested using a circular punch of 0. By using these fine small punches with magnifying loupes, the surgeon can take out intact follicular units ranging from one to three hairs. When hair transplants were first performed in the 50s and 60s, several studies were conducted to determine the optimum size of a graft using the best punches or trephines of the time. When the grafts were larger than five mm, loss in the center gave the transplant a donut appearance. Even then we knew the smaller grafts looked better, it was not worth the much higher percentage of hairs lost though transection at the periphery?the smaller the punch, the higher percentage of hairs were lost. Only with the advent of super-sharp small punches has this procedure become more viable, and thus has been more popular and widely used. A much more time consuming process than strip harvesting, it is tiring for both the surgeon and the patient. Not Folliclar Unit Extration 112 Follicular Unit Micrografting as many grafts can be done at one session and the much larger donor area has to be trimmed short leading to a longer period before looking cosmetically acceptable. When the procedure was first introduced in 2002, the results I saw were less than impressive. The amount of scarring in the donor area was not acceptable despite claims the area could heal without visible signs that grafts had been harvested. Those with curly hair would be rejected because too many of the hairs would be destroyed by cutting through the curved hair follicle. The Fox Test allowed surgeons to evaluate what percentage of follicles would be destroyed on a patient to patient basis. If the percentage was deemed too high for a particular patient, strip harvesting would be recommended.
Costs are also borne by family members who need to miss work to obtain care for asthma medications not to take when pregnant purchase antivert 25mg with mastercard, especially for children symptoms jaw pain antivert 25mg with mastercard. The annual cost of asthma exceeds $19 billion per year in the United States (11 medicine tour discount antivert 25 mg with amex,12) symptoms joint pain order antivert uk. The National Heart symptoms zinc deficiency purchase 25mg antivert free shipping, Lung treatment kitty colds generic 25mg antivert with visa, and Blood Institute estimated that in 2009, the annual cost of providing healthcare related to all respiratory conditions, excluding lung cancer, was $113 billion. The institute further estimated that the cost to American society, in terms of lost productivity as a result of disability and early death due to respiratory disease, amounted to an additional $67 billion (1). A wonderful organ the lung is a wonderful organ built of a complex tree of airways that are, in an average person, 44 miles long and serve to ventilate 300 to 500 million alveoli, or air sacs, with a total surface area nearly the size of a tennis court. This surface is covered by a dense meshwork of blood capillaries of total length of about 3,000 miles. About 85 percent of the alveolar surface is in contact with blood across a tissue barrier 50 times thinner than a sheet of onion skin paper, which allows a very ef? Breathing is regulated through a complex interaction between oxygen and carbon dioxide sensors located in the arteries and the brainstem, which respond to subtle changes in acidity. Sensors located in the lung and chest wall muscles respond to expansion and contraction, sending signals to the central respiratory controllers in the brainstem. The controllers help direct the respiratory muscles, triggering inspiration and expiration and regulating the depth of breathing. By expelling carbon dioxide, the lungs eliminate more acid waste in one hour than the kidneys do in an entire day. Inhaled air contains infectious and noxious particles and gases, against which the lungs must defend themselves. Mechanical factors, such as the structure of the nasal passageway and bronchi, and functional factors, such as cough, prevent invasion into the lung or expel invading elements. The thin layer of mucus, which traps particles and dissolves gases, is constantly propelled by hair-like structures, called cilia, up the bronchi to the trachea and mouth, where they are swallowed or expelled. A variety of cells and lymphatic drainage also work to keep the lungs clear and relatively dry. The macrophage is a cell that originates in the bone marrow and migrates to the lung. After taking up the foreign material, macrophages may migrate up the bronchi and trachea to be swallowed or to the lymph nodes where they initiate an in? This response may defend against infectious agents, but it can also provoke or be part of respiratory diseases themselves. Airborne particles can be toxic in quantities as small as a few parts per billion. Percentage of Americans who smoke 60 50 40 Men High school students 30 Women 20 Pregnant women 10 1965 1974 1979 1985 1990 1995 2000 2007 Year Most smokers start in their teenage years. The rise in adolescent smoking rates in the late 1990s may have been due to tobacco industry advertising that targeted youth. The subsequent decline is associated with increased prevention efforts by many states to curb advertising and offer counter-marketing messages. How lung disease happens the complexity of the respiratory system does not lend itself to easy classi? Emphysema is characterized by a loss of lung elastic recoil that occurs when the lungs are stretched at full inhalation. Diseases that decrease the volume of the lung are called restrictive lung diseases. The most common developmental abnormality is the infant respiratory distress syndrome (or respiratory distress of the newborn). Later-life developmental abnormalities of the spine, such as scoliosis or kyphosis, can also adversely affect breathing. Although there are benign lung tumors, lung cancer is the most notorious of all cancers. Lung disease may also involve the blood vessels in disorders such as pulmonary embolism, which is associated with reduced blood? Because the lungs are in constant contact with the environment, they are especially susceptible to environmental toxins. Assaults on the lung can come from inhaling fumes or other noxious particles in the environment, such as tobacco smoke, or from material that gains access to the lung from the bloodstream (emboli). Exposure to high-oxygen concentrations can induce permanent lung injury, even when given as a life-saving medical treatment. Respiratory failure can also result from weakness of respiratory muscles and from abnormalities of the chest wall and in the neural control of respiration. Impaired control of breathing in the central nervous system can cause sleep apnea, and delayed development of control of breathing in the brainstem has been invoked as a cause of sudden infant death syndrome. The changing face of lung disease At the beginning of the 20th century, infectious diseases were identi? Each year, tuberculosis claimed more than 2 of every 1,000 American lives in the United States (16). Scientists knew what tuberculosis looked like under the microscope, but there was no treatment. Today, scientists have deciphered the entire genome of Mycobacterium tuberculosis and are able to cure tuberculosis?but not in everyone. Respiratory failure Acute and chronic respiratory failure Acute respiratory distress syndrome Sepsis Shock Multi-organ failure Systemic disease affecting the respiratory system Many diseases primarily affecting other organs Autoimmune diseases the threat of new strains with great potential to spread and cause harm still looms. At the beginning of the 20th century, infant mortality was 13 times greater than today (17,18), and respiratory distress of the newborn was unrecognized. Today, surfactant replacement therapy has nearly eliminated this condition?but infants still die of respiratory failure. At the beginning of the 20th century, there was no effective treatment for pneumonia. Today, there are scores of antibiotics that target bacterial infections?but pneumonia still kills, even within hospitals. Today, there are effective worker protection laws and a national commitment to clean air. The reduction in atmospheric ozone, oxides of nitrogen, and particulate pollution has resulted in better quality of life and healthier lungs?but pollution still shortens lives. Largely as a result of these and other medical advances and the public health movement, life expectancy has increased over the past century from 47 to 76 years?but there are hazards afoot. At the beginning of the 20th century, tobacco smoking and lung cancer were rare. Today, multinational tobacco enterprises promote a habit that kills 440,000 Americans every year, as many lives lost as in all the wars fought by our country in the last hundred years (19). New infections have emerged, and the success of modern medicine has brought its own challenges. Although antibiotics have saved lives, they have also resulted in the emergence of highly resistant bacteria, which cause life-threatening infections and prolong hospital con? Each chapter in this book describes a major respiratory disease: whom it affects; what it is like to have the disease; what is being learned about the disease; how it can be prevented, treated, and managed; and how research is making a difference. The purpose of the book is to describe these diseases and the progress made toward controlling them in the hope that someday they will be eliminated. The recognition of the gains made and the goals that may be within our grasp should stir the will and determination for all Americans to breathe, and live, better. Action against asthma: a strategic plan for the Department of Health and Human Services. Trends in infectious disease mortality in the United States during the 20th century. The term acute respiratory distress syndrome was coined in 1967, with similar lung injury being recognized in both medical and surgical patients. About this same time, the condition was being widely recognized in severely wounded soldiers in the Vietnam War. The most common of these is sepsis, a severe infection that spreads throughout the body via the bloodstream. A less common cause of direct injury is the inhalation of high concentrations of toxic gases, which can occur with severe smoke inhalation and in industrial accidents. The following day, her breathing deteriorated and she required mechanical ventilation. She developed pneumonia, and, after about three weeks on the ventilator, a new breathing tube was placed directly into the trachea (tracheostomy) in preparation for long-term mechanical ventilation. After four weeks in the hospital, the sedation was stopped, and after nine weeks, the tracheostomy tube was removed. She remembered the rapidity with which she became ill and that several times she thought she was dying. What we are learning about the disease Pathophysiology, causes: genetic, environment, microbes the cause of the acute lung injury can be either direct, with the injurious agent reaching the lung through the airways or by trauma to the chest, or indirect, with the injurious agent arriving at the lungs through the bloodstream. The thin wall between the blood and air is made up of the blood capillary and the alveolar wall (alveolar-capillary membrane). Molecules released by infected or injured cells signal white cells from the blood to enter the affected area. The incoming white blood cells combine with resident cells to produce more chemicals (calledcytokinesandchemokines), which induce a variety of actions involved in the in? This systemic process is called sepsis when the initiating insult is an infection, but a similar, if not identical, process can occur when the original insult is traumatic injury. This association may be because the lungs are the only organ to receive all the blood of the body. Thus the lungs receive the full brunt of the injurious cytokines and other molecules. In developed countries, bacterial infections are the most common, often with organisms partially or highly resistant to antibiotics that are common in hospital environments. Appropriate treatment of an underlying infection is particularly important and consists of identifying the causative organism as best as possible and draining any abscesses, as well as giving antibiotics. The care of the critically ill patient is highly complex because of the severity of the patient?s illness, the combination of diseases and organ failures and their interactions, and the rapidity of changes in the patient?s condition. The ventilator must be set to deliver enough air to make sure the patient?s oxygen level is adequate. Improvements in how patients are cared for in these units are quite likely to be responsible for the better outcomes in acute respiratory distress syndrome the patient alive without causing harm to the lungs or the rest of the body. The use of small breaths from the ventilator avoids further injury and is particularly important. Although sedative and pain relief medications are essential, too much sedation can keep the patient on the ventilator longer than necessary and cause delirium and lack of cooperation. Medicines that are eliminated by the liver or kidney may accumulate and interact if these organs are dysfunctional. The mere presence of a tube in the trachea to deliver the ventilation is associated with increased risk of pneumonia. One of the goals is also to reduce patient discomfort related to the tubes, blood drawing, alarms, and frequent nursing checks. A critical decision for an improving patient is when to remove the mechanical ventilation. The longer a patient remains on the ventilator, the greater the chance of complications, including airway injury from the tube and pneumonia. Despite normal lung function in nearly all survivors, in self-assessments, these patients frequently rate their quality of life as impaired. The causes of these problems and how best to prevent and treat them are subjects of intense research interest. One study published in 2000 showed that patients given smaller ventilator breaths had signi? Studies have shown that daily spontaneous breathing trials (without the ventilator?s help) resulted in fewer days on the ventilator. To do the trials, it was necessary to stop sedation, which has also been shown to be bene? A simple method to help minimize aspiration and reduce the risk of developing pneumonia is to raise the head of the bed to between 30 and 45 degrees. Other advances are being made and are tied closely to the management of patients in the intensive care unit. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. Epidemiology, prevalence, economic burden, vulnerable populations Epidemiological studies have established features of asthma and provided insight into many of its characteristics, including the age of onset, sex distribution, risk factors, and long-term consequences. The results from this survey found the prevalence of asthma to be over 10 percent in some countries, including the United Kingdom, New Zealand, Australia, Costa Rica, the United States, and Brazil. In contrast, in other countries, like China, the prevalence of asthma is slightly over 5 percent. In recent years, some countries and locales have demonstrated a near doubling in the prevalence of asthma. National Health Interview Survey, National Center for Health Statistics, Centers for Disease Control and Prevention. First, the presence of asthma is greatest in the more ?westernized areas of the world?the Americas, Europe, and Australia. Second, as more countries shift their lifestyle to a more western pattern of living (which includes fewer severe infections early in life, greater use of antibiotics, more processed foods, and a shift from rural to urban living) the prevalence of asthma increases. Finally, in countries with a less westernlifestyle, the prevalence of asthma is low and remains at this level until such societal changes occur. These data suggest that factors associated with a western lifestyle are associated with a greater risk or frequency of asthma (2). These epidemiological changes led to the development of the ?hygiene hypothesis, which proposes that a ?cleaner environment shifts the immune response toward the development of allergies and asthma (4). In the United States, the prevalence of asthma has followed the increase seen worldwide over the past two decades (5).
The diagnosis is confirmed by color Doppler demonstration that the vascular supply of the sequestered lobe arises from the abdominal aorta medications that interact with grapefruit generic 25mg antivert mastercard. Large lung sequestration may act as an arteriovenous fistula and cause high-output heart failure and hydrops 97140 treatment code quality antivert 25 mg. Intralobar sequestrations are usually isolated medicine 3604 pill antivert 25mg low price, whereas more than 50% of extralobar sequestrations are associated with other abnormalities (mainly diaphragmatic hernia and cardiac defects) symptoms kidney order antivert cheap online. Prognosis Postnatal outcome depends on the presence of associated abnormalities 1950s medications generic antivert 25mg online, and hemodynamic disturbances symptoms 4 dpo order antivert with american express. In general, intralobar sequestration has an excellent prognosis, whereas extralobar sequestration has a poor prognosis because of the high incidence of other defects and hydrops. At 8?10 weeks of gestation, all fetuses demonstrate herniation of the mid-gut that is visualized as a hyperechogenic mass in the base of the umbilical cord; retraction into the abdominal cavity occurs at 10?12 weeks and is completed by 11 weeks and 5 days. The integrity of the abdominal wall should always be demonstrated; this can be achieved by transverse scans demonstrating the insertion of the umbilical cord. It is also important to visualize the urinary bladder within the fetal pelvis, because this rules out exstrophy of the bladder and of the cloaca. The abdominal contents, including intestines and liver or spleen covered by a sac of parietal peritoneum and amnion, are herniated into the base of the umbilical cord. Less often there is an associated failure in the cephalic embryonic fold, resulting in the pentalogy of Cantrell (upper mid-line omphalocele, anterior diaphragmatic hernia, sternal cleft, ectopia cordis and intracardiac defects) or failure of the caudal fold, in which case the omphalocele may be associated with exstrophy of the bladder or cloaca, imperforate anus, colonic atresia and sacral vertebral defects. The Beckwith?Wiedemann syndrome (usually sporadic and occasionally familial syndrome with a birth prevalence of about 1 in 14 000) is the association of omphalocele, macrosomia, organomegaly and macroglossia; in some cases there is mental handicap, which is thought to be secondary to inadequately treated hypoglycemia. About 5% of affected individuals develop tumors during childhood, most commonly nephroblastoma and hepatoblastoma. Etiology the majority of cases are sporadic and the recurrence risk is usually less than 1%. Chromosomal abnormalities (mainly trisomy 18 or 13) are found in about 50% of cases at 12 weeks, 30% of cases at mid-gestation and in 15% of neonates. Similarly, in Beckwith Wiedemann syndrome, most cases are sporadic, although autosomal dominant, recessive, X-linked and polygenic patterns of inheritance have been described. Diagnosis the diagnosis of exomphalos is based on the demonstration of the mid-line anterior abdominal wall defect, the herniated sac with its visceral contents and the umbilical cord insertion at the apex of the sac. Ultrasonographic examination should be directed towards defining the extent of the lesion and exclusion of other malformations. Prognosis Exomphalos is a correctable malformation in which survival depends primarily on whether or not other malformations or chromosomal defects are present. The mortality is much higher with cephalic fold defects than with lateral and caudal defects. The loops of intestine lie uncovered in the amniotic fluid and become thickened, edematous and matted. Associated chromosomal abnormalities are rare, and, although other malformations are found in 10?30% of the cases, these are mainly gut atresias, probably due to gut strangulation and infarction in utero. Diagnosis Prenatal diagnosis is based on the demonstration of the normally situated umbilicus and the herniated loops of intestine, which are free-floating and widely separated, and usually on the right of the cord insertion. In the thrid trimester, chemical peritonitis causes distension and thickening of the walls of the intesttine. About 30% of fetuses are growth-restricted but the diagnosis can be difficult because gastroschisis as such is associated with a small abdominal circumference. Prognosis Postoperative survival is about 90%; mortality is usually the consequence of short gut syndrome. In this condition, the infants require total parenteral nutrition and they usually die within the first 4 years of life from liver disease. The pathogenesis is uncertain but possible causes include abnormal folding of the trilaminar embryo during the first 4 weeks of development, early amnion rupture with amniotic band syndrome, and early generalized compromise of embryonic blood flow. Diagnosis the ultrasonographic features are a major abdominal wall defect, severe kyphoscoliosis and a short or absent umbilical cord. Typically, the liver is directly attached to the placenta without an interposed umbilical cord and there is major distortion of the spine. In the first trimester, it is possible to demonstrate that part of the fetal body is in the amniotic cavity and the other part is in the celomic cavity. The findings suggest that early amnion rupture before obliteration of the celomic cavity is a possible cause of the syndrome. Prevalence Bladder exstrophy is found in 1 per 30 000 births and cloacal exstrophy is found in about 1 in per 200 000 births. Diagnosis Bladder exstrophy should be suspected when, in the presence of normal amniotic fluid, the fetal bladder is not visualized (the filling cycle of the bladder is normally in the range of 15 min); an echogenic mass is seen protruding from the lower abdominal wall, in close association with the umbilical arteries. Figure 01 Figure 02 with color doppler Bladder Extrophy and absence of the penis an echogenic mass is seen protruding from the lower abdominal wall, in close association with the umbilical arteries (Color Doppler). Other findings include single umbilical artery, ascites, vertebral anomalies, club foot and ambiguous genitalia (in boys, the penis is divided and duplicated). Prognosis With aggresive reconstructive bladder, bowel and genital surgery, survival is more than 80%. Although it has been suggested that gender re-assignment to females should occur, psychological follow-ups of such patients suggest that both male and females with this condition are capable of a normal lifestyle with normal intelligence, although some form of urinary tract diversion is required for all. The bowel is normally uniformly echogenic until the third trimester of pregnancy, when prominent meconium-filled loops of large bowel are commonly seen. The liver comprises most of the upper abdomen and the left lobe is greater in size than the right due to its greater supply of oxygenated blood. The gall bladder is seen as an ovoid cystic structure to the right and below the intrahepatic portion of the umbilical vein. The spleen may also be visualized in a transverse plane posterior and to the left of the fetal stomach. The abdominal circumference should be measured in a cross-section of the abdomen demonstrating the stomach and portal sinus of the liver. The visceral situs should be assessed, by demonstrating the relative position of the stomach, hepatic vessels, abdominal aorta and inferior vena cava. Etiology Esophageal atresia and tracheoesophageal fistulae are sporadic abnormalities. Chromosomal abnormalities (mainly trisomy 18 or 21) are found in about 20% of fetuses. In over 80% of cases, esophageal atresia occurs in association with a tracheo-esophageal fistula, allowing intake of amniotic fluid from the stomach, that may be therefore normally distended, particularly in early gestation. Diagnosis Prenatally, the diagnosis of esophageal atresia is suspected when, in the presence of polyhydramnios (usually after 25 weeks), repeated ultrasonographic examinations fail to demonstrate the fetal stomach. However, gastric secretions may be sufficient to distend the stomach and make it visible. Occasionally (after 25 weeks), the dilated proximal esophageal pouch can be seen as an elongated upper mediastinal and retrocardiac anechoic structure. This is a dynamic finding, however, that occurs only at the time of fetal swallowing, and requires therefore prolonged sonographic visualization. The differential diagnosis for the combination of absent stomach and polyhydramnios includes intrathoracic compression, by conditions such as diaphragmatic hernia, and muscular-skeletal anomalies causing inability of the fetus to swallow. Prognosis Survival is primarily dependent on gestation at delivery and the presence of other anomalies. Thus, for babies with an isolated tracheoesophageal fistula, born after 32 weeks, when an early diagnosis is made, avoiding reflux and aspiration pneumonitis, postoperative survival is more than 95%. The patency of the lumen is usually restored by the 11th week and failure of vacuolization may lead to stenosis or atresia. Duodenal obstruction can also be caused by compression from the surrounding annular pancreas or by peritoneal fibrous bands. Etiology Duodenal atresia is a sporadic abnormality, although, in some cases, there is an autosomal recessive pattern of inheritance. Approximately half of fetuses with duodenal atresia have associated abnormalities, including trisomy 21 (in about 40% of fetuses) and skeletal defects (vertebral and rib anomalies, sacral agenesis, radial abnormalities and talipes), gastrointestinal abnormalities (esophageal atresia/tracheoesophageal fistula, intestinal malrotation, Meckel?s diverticulum and anorectal atresia), cardiac and renal defects. Diagnosis Prenatal diagnosis is based on the demonstration of the characteristic ?double bubble appearance of the dilated stomach and proximal duodenum, commonly associated with polyhydramnios. However, obstruction due to a central web may result in only a ?single bubble?, representing the fluid-filled stomach. Continuity of the duodenum with the stomach should be demonstrated to differentiate a distended duodenum from other cystic masses, including choledochal or hepatic cysts. Although the characteristic ?double bubble can be seen as early as 20 weeks, it is usually not diagnosed until after 25 weeks, suggesting that the fetus is unable to swallow a sufficient volume of amniotic fluid for bowel dilatation to occur before the end of the second trimester of pregnancy. Prognosis Survival after surgery in cases with isolated duodenal atresia is more than 95%. Intrinsic lesions result from absent (atresia) or partial (stenosis) recanalization of the intestine. In cases of atresia, the two segments of the gut may be either completely separated or connected by a fibrous cord. In cases of stenosis, the lumen of the gut is narrowed or the two intestinal segments are separated by a septum with a central diaphragm. Apple-peel atresia is characterized by absence of a vast segment of the small bowel, which can include distal duodenum, the entire jejunum and proximal ileus. Extrinsic obstructions are caused by malrotation of the colon with volvulus, peritoneal bands, meconium ileus, and agangliosis (Hirschsprung?s disease). The most frequent site of small bowel obstruction is distal ileus (35%), followed by proximal jejunum (30%), distal jejunum (20%), proximal ileus (15%). Anorectal atresia results from abnormal division of the cloaca during the 9th week of development. Prevalence Intestinal obstruction is found in about 1 per 2000 births; in about half of the cases, there is small bowel obstruction and in the other half anorectal atresia. Etiology Although the condition is usually sporadic, in multiple intestinal atresia, familial cases have been described. In contrast with anorectal atresia, associated defects such as genitourinary, vertebral, cardiovascular and gastrointestinal anomalies are found in about 80% of cases. Diagnosis the lumens of the small bowel and colon do not normally exceed 7 mm and 20 mm, respectively. Diagnosis of obstruction is usually made quite late in pregnancy (after 25 weeks), as dilatation of the intestinal lumen is slow and progressive. Jejunal and ileal obstructions are imaged as multiple fluid-filled loops of bowel in the abdomen. If bowel perforation occurs, transient ascites, meconium peritonitis and meconium pseudocysts may ensue. Polyhydramnios (usually after 25 weeks) is common, especially with proximal obstructions. Bowel enlargement and polyhydramnios may be found in fetuses with Hirschsprung?s disease, the megacystis microcolon?intestinal hypoperistalsis syndrome and congenital chloride diarrhea. When considering a diagnosis of small bowel obstruction, care should be taken to exclude renal tract abnormalities and other intra-abdominal cysts such as mesenteric, ovarian or duplication cysts. In anorectal atresia, prenatal diagnosis is usually difficult because the proximal bowel may not demonstrate significant dilatation and the amniotic fluid volume is usually normal; occasionally calcified intraluminal meconium in the fetal pelvis may be seen. Prognosis Infants with bowel obstruction typically present in the early neonatal period with symptoms of vomiting and abdominal distention. The prognosis is related to the gestational age at delivery, the presence of associated abnormalities and site of obstruction. In those born after 32 weeks with isolated obstruction requiring resection of only a short segment of bowel, survival is more than 95%. Loss of large segments of bowel can lead to short gut syndrome, which is a lethal condition. It derives from failure of migration of neuroblasts from the neural crest to the bowel segments, which generally occurs between the 6th and 12th weeks of gestation. Another theory suggests that the disease is caused by degeneration of normally migrated neuroblasts during either preor postnatal life. Etiology It is considered to be a sporadic disease, although in about 5% of cases there is a familial inheritance. Diagnosis the aganglionic segment is unable to transmit a peristaltic wave, and therefore meconium accumulates and causes dilatation of the lumen of the bowel. The ultrasound appearance is similar to that of anorectal atresia, when the affected segment is colon or rectum. Polyhydramnios and dilatation of the loops are present in the case of small bowel involvement; on this occasion, it is not different from other types of obstruction. Prognosis Postnatal surgery is aimed at removing the affected segment and this may be a two-stage procedure with temporary colostomy. Bowel perforation usually occurs proximal to some form of obstruction, although this cannot always be demonstrated. Etiology Intestinal stenosis or atresia and meconium ileus account for 65% of the cases. Meconium ileus is the impaction of abnormally thick and sticky meconium in the distal ileum, and, in the majority of cases, this is due to cystic fibrosis. Diagnosis In the typical case, meconium peritonitis is featured by the association of intra-abdominal echogenic area, dilated bowel loops and ascites. The diagnosis should be considered if the fetal bowel is observed to be dilated or whenever an area of fetal intraabdominal hyperechogenicity is detected. The differential diagnosis of hyperechogenic bowel includes: intra-amniotic hemorrhage; early ascites; fetal hypoxia; meconium peritonitis; and cystic fibrosis. Meconium ileus and hyperechogenic fetal bowel at 16?18 weeks of gestation may be present in 75% of fetuses with cystic fibrosis. The prevalence of cystic fibrosis in fetuses with prenatal diagnosis of intestinal obstruction may be about 10%. Prognosis Meconium peritonitis is associated with a more than 50% mortality in the neonatal period. Causes of hepatosplenomegaly include immune and non-immune hydrops, congenital infection and metabolic disorders, and it is seen in Beckwith?Wiedemann and Zellweger syndromes. Hepatic enlargement may also be caused by hemangioma, which is usually hypoechogenic, or hepatoblastoma (the most frequent malignant tumor in fetal life), in which there are areas of calcification.
Cheap antivert 25mg otc. How to Know When You’re Ovulating.
References
- Borggreven PA, Kuik DJ, Quak JJ, et al. Comorbid condition as a prognostic factor for complications in major surgery of the oral cavity and oropharynx with microvascular soft tissue reconstruction. Head Neck 2003;25:808-815.
- Wilding G, Green HL, Longo DL, et al: Tumors of the heart and pericardium. Cancer Treat Rev 1988; 15:165-181.
- Jallali N, Malata CM. Reconstruction of concomitant total loss of upper and lower lips with a free vertical rectus abdominis flap. Microsurgery 2005:25;118-120.
- Rocco, F., Carmignani, L., Acquati, P. et al. Restoration of posterior aspect of rhabdosphincter shortens continence time after radical retropubic prostatectomy. J Urol 2006; 175:2201-2206.
- Zhang RL, Chopp M, Roberts C, et al. Ascl1 lineage cells contribute to ischemia-induced neurogenesis and oligodendrogenesis. J Cereb Blood Flow Metab 2011;31:614-25.