Muhammad Ali Chaudhry, M.B.A., M.B.B.S., M.D.
- Assistant Professor of Radiology and Radiological Science

https://www.hopkinsmedicine.org/profiles/results/directory/profile/1705496/muhammad-chaudhry
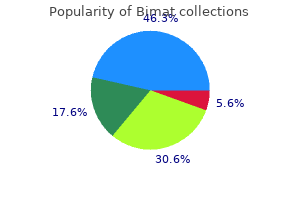
The alternative transportation strategy implemented during the 1996 Summer Olympic Games in Atlanta treatment impetigo order 3 ml bimat with mastercard, Ga symptoms zoloft withdrawal buy bimat 3 ml without a prescription, provided such an opportunity symptoms 3dpo buy cheap bimat on line. Objective: To describe traffic changes in Atlanta symptoms quitting weed purchase bimat toronto, Ga medications 1 gram bimat 3 ml with mastercard, during the 1996 Summer Olympic Games and concomitant changes in air quality and childhood asthma events symptoms zinc deficiency order bimat 3ml online. Outcome: Citywide acute care visits and hospitalizations for asthma (asthma events) and nonasthma events, concentrations of major air pollutants, meteorological variables, and traffic counts. Results: During the Olympic Games, the number of asthma acute care events decreased 41. In multivariate regression analysis, only the reduction in asthma events recorded in the Medicaid database was significant (relative risk, 0. Meteorological conditions during the Olympic Games did not differ substantially from the baseline period. Conlusions: Efforts to reduce downtown traffic congestion in Atlanta during the Olympic Games resulted in decreased traffic density, especially during the critical morning period. This was associated with a prolonged reduction in ozone pollution and significantly lower rates of childhood asthma events. These data provide support for efforts to reduce air pollution and improve health via reductions in motor vehicle traffic. References: ?Ebelt, Air quality in postunification Erfurt, East Germany: associating changes in pollutant concentrations with changes in emissions. Prevalence of respiratory and atopic disorders among children in the East and West of Germany five years after reunification. Living conditions in eastern Germany have changed rapidly since unification in 1990 and little is known about how these changes affect the prevalence of atopic diseases. This study describes methods and prevalences of a large epidemiological project investigating determinants of childhood asthma and allergies in eastern (Dresden and Leipzig) and western (Munich) Germany in 1995/1996. No difference between Munich and Dresden was observed in the prevalence of diagnosed hay fever, skin test reactivity to > or = 1 allergen, and increased levels (>0. Symptoms and visible signs of atopic eczema tended to be more prevalent in Dresden. Similar East-West differences between the three study areas were seen in the younger age group. These findings are in line with recently observed increases in the prevalence of hay fever and atopic sensitization, but not of asthma and bronchial hyperresponsiveness, among 9-11 yr old children in Leipzig. Note that there have been very few randomized controlled trials, so it is difficult to estimate the effect that these suggestions might have. Early reversal of severity signs-chest indrawing, hypoxia, and tachypnoea-improves outcome. We postulated that zinc, an acute phase reactant, would shorten duration of severe pneumonia and time in hospital. The outcomes were time to cessation of severe pneumonia (no chest indrawing, respiratory rate 50 per min or less, oxygen saturation at least 95% on room air) and discharge from hospital. Discharge was allowed when respiratory rate was 40 per minute or less for 24 consecutive hours while patients were maintained only on oral antibiotics. The mean reduction is equivalent to 1 hospital day for both severe pneumonia and time in hospital. All effects were greater when children with wheezing were omitted from the analysis. Interpretation: Adjuvant treatment with 20 mg zinc per day accelerates recovery from severe pneumonia in children, and could help reduce antimicrobial resistance by decreasing multiple antibiotic exposures, and lessen complications and deaths where second line drugs are unavailable. Investigators in Mexico conducted a study among children with asthma residing in Mexico City to determine if antioxidant supplementation could modulate the adverse effect of exposure to air pollutants on lung function of these children. There is additional evidence from studies of adults, such as the following: Among adults aged 16-50 years, apple consumption was negatively associated with asthma. Design: Diet was assessed by a detailed food frequency questionnaire and airway disease by respiratory symptoms or airway responsiveness to exercise. No other food groups or nutrients were significantly associated with either an increased or reduced risk of current asthma. Conclusion: these data suggest that consumption of oily fish may protect against asthma in childhood. Selenium and asthma?in adolescents and adults: Among adults 16-50 years old, intake of selenium was negatively associated with asthma. Controlled for age, sex, body mass index, social class, housing tenure, employment status, whether a single parent, smoking, passive smoke exposure at home, and total energy intake. Association between antioxidant vitamins and asthma outcome measures: systematic review and meta-analysis. Zinc for severe pneumonia in very young children: double-blind placebo-controlled trial. In summary, lung function levels were lower in children with inadequate dietary antioxidant vitamin intake. The opinions and conclusions expressed do not necessarily represent the official position of the World Health Organization. This publication is being distributed without warranty of any kind, either express or implied. In no event shall the World Health Organization be liable for damages, including any general, special, incidental, or consequential damages, arising out of the use of this publication the contents of this training module are based upon references available in the published literature as of its last update. Users are encouraged to search standard medical databases for updates in the science for issues of particular interest or sensitivity in their regions and areas of specific concern. If users of this training module should find it necessary to make any modifications (abridgement, addition or deletion) to the presentation, the adaptor shall be responsible for all modifications made. The World Health Organization disclaims all responsibility for adaptations made by others. Asthma still imposes an unacceptable burden on health care systems, and on society through loss of productivity in the workplace and, especially for pediatric asthma, disruption to the family. Health care providers managing asthma face different issues around the world, depending on the local context, the health system, and access to resources. The Global Strategy for Asthma Management and Prevention was extensively revised in 2014 to provide a comprehensive and integrated approach to asthma management that can be adapted for local conditions and for individual patients. Asthma is a common and potentially serious chronic disease that imposes a substantial burden on patients, their families and the community. It causes respiratory symptoms, limitation of activity, and flare-ups (attacks) that sometimes require urgent health care and may be fatal. Some variation in airflow can also occur in people without asthma, but it is greater in asthma. Factors that may trigger or worsen asthma symptoms include viral infections, domestic or occupational allergens. Asthma flare-ups (also called exacerbations or attacks) may occur, even in people taking asthma treatment. When asthma is uncontrolled, or in some high-risk patients, these episodes are more frequent and more severe, and may be fatal. A stepwise approach to treatment, customized to the individual patient, takes into account the effectiveness of available medications, their safety, and their cost to the payer or patient. A flow-chart for making the diagnosis in clinical practice is shown in Box 1, with the specific criteria for diagnosing asthma in Box 2. Depending on clinical urgency and access to resources, this should preferably be done before starting controller treatment. Confirming the diagnosis of asthma is more difficult after treatment has been started (see p7). If bronchodilator reversibility is not present when it is first tested, the next step depends on the clinical urgency and availability of other tests. Occupational asthma and work-aggravated asthma Every patient with adult-onset asthma should be asked about occupational exposures, and whether their asthma is better when they are away from work. It is important to confirm the diagnosis objectively (which often needs specialist referral) and to eliminate exposure as soon as possible. Pregnant women Ask all pregnant women and those planning pregnancy about asthma, and advise them about the importance of asthma treatment for the health of both mother and baby. The elderly Asthma may be under-diagnosed in the elderly, due to poor perception, an assumption that dyspnea is normal in old age, lack of fitness, or reduced activity. Asthma may also be over-diagnosed in the elderly through confusion with shortness of breath due to left ventricular failure or ischemic heart disease. Confirming an asthma diagnosis in patients taking controller treatment: For many patients (25?35%) with a diagnosis of asthma in primary care, the diagnosis cannot be confirmed. For example, if lung function is normal, repeat reversibility testing after withholding medications for 12 hours. If the patient has frequent symptoms, consider a trial of step-up in controller treatment and repeat lung function testing after 3 months. If the patient has few symptoms, consider stepping down controller treatment, but ensure the patient has a written asthma action plan, monitor them carefully, and repeat lung function testing. Asthma control has two domains: symptom control (previously called ?current clinical control) and risk factors for future poor outcomes. Level of asthma symptom control In the past 4 weeks, has the patient had: Well Partly Uncontrolled controlled controlled Daytime symptoms more than twice/week? Asthma severity can be assessed retrospectively from the level of treatment (p14) required to control symptoms and exacerbations. Severe asthma is asthma that requires Step 4 or 5 treatment, to maintain symptom control. How to investigate uncontrolled asthma in primary care this flow-chart shows the most common problems first, but the steps can be carried out in a different order, depending on resources and clinical context. The aim is to reduce the burden to the patient and their risk of exacerbations, airway damage, and medication side-effects. Population-level recommendations about ?preferred asthma treatments represent the best treatment for most patients in a population. Patients should preferably be seen 1?3 months after starting treatment and every 3?12 months after that, except in pregnancy when they should be reviewed every 4?6 weeks. Stepping down treatment when asthma is well-controlled Consider stepping down treatment once good asthma control has been achieved and maintained for 3 months, to find the lowest treatment that controls both symptoms and exacerbations, and minimizes side-effects. Check and improve adherence with asthma medications Around 50% of adults and children do not take controller medications as prescribed. Although allergens may contribute to asthma symptoms in sensitized patients, allergen avoidance is not recommended as a general strategy for asthma. For some patients, treatment with intranasal corticosteroids improves asthma control. Obesity: to avoid over or under-treatment, it is important to document the diagnosis of asthma in the obese. Weight reduction should be included in the treatment plan for obese patients with asthma; even 5?10% weight loss can improve asthma control. The elderly: comorbidities and their treatment should be considered and may complicate asthma management. Factors such as arthritis, eyesight, inspiratory flow, and complexity of treatment regimens should be considered when choosing medications and inhaler devices. Patients should be assisted to distinguish between symptoms of anxiety and of asthma. Food allergy and anaphylaxis: food allergy is rarely a trigger for asthma symptoms. Good asthma control is essential; patients should also have an anaphylaxis plan and be trained in appropriate avoidance strategies and use of injectable epinephrine. The management of worsening asthma and exacerbations should be considered as a continuum, from self-management by the patient with a written asthma action plan, through to management of more severe symptoms in primary care, the emergency department and in hospital. Identifying patients at risk of asthma-related death these patients should be identified, and flagged for more frequent review. Patients who deteriorate quickly should be advised to go to an acute care facility or see their doctor immediately. Arrange immediate transfer to an acute care facility if there are signs of severe exacerbation, or to intensive care if the patient is drowsy, confused, or has a silent chest. Check response of symptoms and saturation frequently, and measure lung function after 1 hour. In acute care facilities, intravenous magnesium sulfate may be considered if the patient is not responding to intensive initial treatment. Do not routinely perform chest X-ray or blood gases, or prescribe antibiotics, for asthma exacerbations. Decide about need for hospitalization based on clinical status, symptomatic and lung function, response to treatment, recent and past history of exacerbations, and ability to manage at home. Continue increased controller doses for 2?4 weeks, and reduce reliever to as-needed. Consider referral for specialist advice for patients with an asthma hospitalization, or repeated emergency department presentations. All patients must be followed up regularly by a health care provider until symptoms and lung function return to normal. Comprehensive post-discharge programs that include optimal controller management, inhaler technique, self-monitoring, written asthma action plan and regular review are cost-effective and are associated with significant improvement in asthma outcomes. Leukotriene modifiers Target one part of the inflammatory Few side-effects except (tablets). Used as an option for elevated liver function tests pranlukast, zafirlukast, controller therapy, particularly in children. Require inhalation and pharyngeal nedocromil sodium meticulous inhaler maintenance. Long-acting An add-on option at Step 4 or 5 bny soft Side-effects are uncommon anticholinergic, tiotropium mist inhaler for adults (? This report, provides an integrated approach to asthma that can be adapted for a wide range of health systems. The report has a user-friendly format with practical summary tables and flow-charts for use in clinical practice.
Evidence for efficacy and safety of some of these medications is often limited or research is conflicting symptoms upper respiratory infection buy generic bimat 3ml line. If medications are utilized treatment xeroderma pigmentosum order bimat 3ml without a prescription, they should be part of a comprehensive treatment plan that includes educational and behavioral interventions medicine jokes generic bimat 3 ml amex. Careful attention to potential adverse effects of medication should be maintained with the understanding that the risks as well as benefits of medication therapy must be considered for each individual symptoms xanax abuse purchase bimat us. Resources for Families American Academy of Child and Adolescent Psychiatry Autism Resource Center medications errors pictures discount 3ml bimat free shipping. Resources for Professionals American Academy of Child and Adolescent Psychiatry Autism Resource Center medicine jar buy cheap bimat on line. Practice parameter: screening and diagnosis of autism: Report of the quality standards subcommittee of the American Academy of Neurology and the Child Neurology Society. Evidence-based practice and autism in the schools: A guide to providing appropriate interventions to students with autism spectrum disorders. Pharmacologic treatment of repetitive behaviors in autism spectrum disorders: Evidence of publication bias. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model, Pediatrics, 125(1): 17-23. The prevalence of anxiety and mood problems among children with autism and Asperger syndrome. Clinical evaluation in autism spectrum disorders: Psychological assessment within a transdisciplinary framework. Effects of diagnosis, race, and puberty on platelet serotonin levels in autism and mental retardation. Interventions to facilitate social interaction for young children with autism: Review of available research and recommendations for educational intervention and future research, Journal of Autism and Developmental Disorders, 32(5), 351-372. Systematic review of medical treatments for children with autism spectrum disorders. Autism spectrum disorders: Pervasive developmental disorders with addendum January 2007. Evidence-based assessment of autism spectrum disorders in children and adolescents. Early intensive behavioral intervention: Outcomes for children with autism and their parents after two years. Randomized trial of intensive early intervention for children with pervasive developmental disorder. A systematic review of early intensive intervention for autism spectrum disorders, Pediatrics, 127(5), 1303-1311. Systematic observation of red flags for autism spectrum disorders in young children, Florida State University, Tallahassee, Florida. Early identification of and intervention for infants and toddlers who are at risk for autism spectrum disorder, Language, Speech, and Hearing Services in Schools, 34(3), 180-193. Warner-Metzger, PhD, University of Tennessee Health Science Center, Boling Center for Developmental Disabilities Chairperson; and Suzanne M. Contributing Factors Recent literature identifies several factors related to the development of disruptive behaviors. Although not discounted as a factor for the development of disruptive, currently there is little evidence for a genetic basis for behavior problems. Genetic contributions to childhood aggression appear to be relatively small (Jacobson, Prescott, & Kendler, 2002) and psychobiological influences are at best inconclusive (Hinshaw & Lee, 2003). Instead, a large emphasis is placed on the multifaceted and transactional causal factors for disruptive behaviors (Coie & Dodge, 1998; Hinshaw & Lee, 2003). The literature concerning underlying factors for disruptive behaviors converges on environmental factors. Most importantly, high levels of parental psychopathology, poverty, poor family functioning, dysfunctional parent-child interactions, and child abuse are thought to play a role in the severity of disruptive behaviors in children (Coie & Dodge, 1998). Associated variables with disruptive behaviors include, but are not limited to , cognitive deficits (Moffit & Lynam, 1994), difficulties in social-cognitive information processing (Crick & Dodge, 1994), and peer rejection (Coie & Dodge, 1998). The progression of conduct problems appears to remain somewhat stable from early childhood to later childhood (Broidy, et al. The behaviors were categorized by the overlay of two continuums representing the dimensions of overt-covert behavior and destructive-nondestructive behavior. The early starter pathway is characterized by conduct problems and social skills deficits originating in school-age years with increasingly severe behaviors developing through adolescence and adulthood. The early starter pathway is thought to consist of a relatively small group of children, mostly boys, who are at high risk for accelerated and chronic conduct problems and psychopathology (Moffit, 1993). On the contrary the late starter pathway represents a larger group of children and is thought to begin in adolescence rather than childhood, consist of less serious conduct problems, be influenced by a deviant peer group, and have a short duration (Moffit, 1993; Patterson et al. The tendency for late starters is to experience a surge of antisocial behavior during adolescence; however, they are supposedly at less risk for chronic offending and continued conduct problems into adulthood, as they presumably possess higher levels of social skills. Further, this same research has demonstrated that late starters do not have the childhood history of cognitive deficits, learning difficulties, preexisting family adversity, or motor skill problems such as early starters exhibit (Patterson et al. Specifically, Loeber and Hay (1997) found evidence identifying three developmental pathways for conduct problems. These included the Overt Pathway with increasing levels of aggression, the Covert Pathway with concealed problem behaviors, and the Authority Conflict Pathway with oppositional and avoidance behaviors towards authority figures. Much like the early starter model, the overt pathway is thought to better describe children who experience a progressive escalation of conduct problems over time compared to those who are experiencing transitory or temporary ones. Thus, regardless of the model used to explain the progression of conduct problems, the prognosis appears to worsen with signs of early aggressive acts that are likely to predict more severe problems over time (Moffit, 1993; Serbin, Schwartzman, Moskowitz, & Ledginham, 1991). Epidemiological Theories Despite the contributing influences to the initial appearance of disruptive behaviors, their maintenance may depend on complex cognitive processes and environmental interactions. Two such well-researched mechanisms for continued behavior problems are social-information processing (Crick & Dodge, 1994; Lemerise & Arsenio, 2000) and coercive parent-child interactions (Patterson, 1982, 2002). The social information-processing model describes how cognitive distortions and deficiencies combine with emotional processes and social contexts to result in socially incompetent behavior for children. This pattern holds true for both peer relationships and responses to authority figures (Dodge & Price, 1994). Yet, temper tantrums are common behaviors in children between the ages of 2 and 3 years. After age 3, children become more able to express their frustrations in socially acceptable ways (Hall & Hall, 2003). Typically the youth exhibits at least three of the following behaviors within the past 12 months, one or more of which occur in the past 6 months (Criterion A). The medical record should be well documented when the clinician does not adhere to standards of this nature in particular cases. These standards tend to be applicable 75 percent of the time and there are typically exceptions to their application. Therapeutic alliances with the child and his/her family must be established to ensure successful assessment and treatment of disruptive behavior disorders. The best way to engage the youth is to empathize with his/her anger and frustration while failing to sanction oppositional/aggressive behavior. Likewise, the clinician must convey empathy with the parents frustration without making them feel accused, judged, or that they have an ally. Active effort must be made to address cultural issues in the diagnosis and treatment of disruptive behavior disorders. Different ethnic subgroups have different standards of obedience and parenting and these differences are can be overlooked if the clinician and client do not share the same backgrounds. Therefore, clinicians should make every effort to be sensitive to areas of mismatch and be prepared to be educated. This sensitivity is especially critical in disruptive behavior disorders because discipline becomes a core point of discussion in every case. Assessment of disruptive behavior disorders must include information obtained directly from the child, as well as from the parents/caregivers, regarding the core symptoms; age of onset; duration of symptoms; and degree of functional impairment. In all cases, multiple settings, processes, and informants need to be considered for an exhaustive screening and/or evaluation. Clinicians should pay careful attention to significant comorbid psychiatric disorders when diagnosing and treating disruptive behavior disorders. Concurrent substance use should always be considered in youngsters with disruptive behavior disorders, but especially in teens and when interventions do not yield the expected response. Clinicians need to be aware that parents and educators tend to agree more with each other on externalizing behaviors than with the youth. Use specific questionnaires and rating scales in evaluating children and/or adolescents for disruptive behavior disorders and in tracking progress. An array of tools has been developed to measure disruptive and other aggressive behaviors of children and adolescents for diagnostic and symptom tracking purposes. Some tools offer abbreviated versions that can be completed quickly by the respondent. Nearly all tools are designed to evaluate oppositionality, hyperactivity, and impulsivity in young people of school age. Additionally, assessment of cognitive functioning, mood, suicidal potential, and substance use should occur. A urine or blood drug screen may be indicated, especially when clinical evidence suggests substance abuse that the patient denies. Evaluation of a youth to determine whether s/he meets criteria for a Disruptive Behavior Disorder diagnosis can be accomplished via thorough review of collateral information and a comprehensive clinical interview. The evaluator should interview both the youth and the parents to obtain history information about the youth. Table 1: Caregiver Interview Questions to Assess Oppositional Defiant Disorder (Angold & Costello, 1996) 1. Has your child in the past 3 months been spiteful or vindictive, or blamed others for his or her own mistakes? How often is your child touchy or easily annoyed, and how often has your child lost his/her temper, argued with adults, or defied or refused adults requests? How often has your child been angry and resentful or deliberately annoying to others? Any negative response is 94% sensitive for ruling out oppositional defiant disorder. Youth Interview Questions to Assess Conduct Disorder (Searight, Rottnek, & Abby, 2001) 1. Note: If the child is 10 to 14 years of age, cigarette smoking, sexual activity, and alcohol or drug use can serve as ?red flags for conduct problems (Searight, Rottnek, & Abby, 2001). Standardized Assessments Central to every clinical assessment utilizing psychological instruments is the process of test selection, administration, and interpretation. Although professional ethical guidelines speak directly to these issues, readers are nonetheless strongly encouraged to review the manuals of the instruments in the next paragraph to ensure that the instrument has been normed on similar populations to the youth being assessed, the instrument has been subject to peer review, administration procedures are followed, and the limitations of conclusions that have been drawn are identified. Additionally, several standardized instruments provide general information on a broad range of characteristics for children and adolescents. Parent and teacher ratings should be considered in the context of age-appropriate behaviors. Also available are teacher and self-report questionnaires for some ages, as well as a semi-structured clinical interview for children and adolescents (McConaughy & Achenbach, 2001). It is frequently used for youth who access services across the System of Care (mental health, child welfare and social services, youth & adolescent justice, education, prevention, and community-based programs). Also available for children ages 2-6 years (Conners Early Childhood; Conners, 2009). Assessing for Cognitive and Academic Deficits Evaluation of learning disorders and academic functioning is an important component in the assessment of children with Disruptive Behavior Disorders. Although the exact percentage is lacking, a significant number of children with disruptive behavior disorders have learning problems, especially in the area of verbal skills. Difficulties in reading and language may contribute to academic difficulties, especially in more advanced grades when so much depends on understanding and using the written word. Language deficits may also contribute to an inability to articulate feelings and attitudes, resulting in a child resorting to physical expression in lieu of verbal expression. Additionally, unrecognized and untreated learning disabilities and cognitive deficits create deep frustration for a child, which can lead to school avoidance/truancy. Clinicians should develop individualized treatment plans based on the specifics surrounding each case. Because of comorbidity and multiple dysfunctions, effective treatment is often multitarget, multimodal, and extensive, combining individual therapy, family therapy, pharmacotherapy, and ecological interventions (like placement and interventions designed for the school setting). Parent management training techniques are the most empirically supported programs for school-age youth. The principles underlying these approaches are: 1) reduce positive reinforcement of disruptive behavior; 2) increase reinforcement of prosocial and compliant behavior; 3) apply consequences and/or punishment for disruptive behavior, where punishment typically takes the form of time out, loss of tokens, and/or loss of privileges; and 4) make the response of parents predictable, contingent, and immediate. Pharmacotherapy may be helpful as an adjunct to treatment, for symptomatic treatment, or to treat comorbid disorders. When considering a medication trial, ensure that strong treatment alliances have been established first. Depending on the severity, persistence, or unusualness of the disruptive behavior, intensive and prolonged treatment may be necessary. These are cases in which youth have failed to demonstrate progress under the current treatment regimen. Hence, increased levels of care such as day treatment, residential, or hospitalization may be warranted, with an emphasis on the least restrictive setting for the shortest possible interval. Risks and benefits of placement in structured settings should be weighed carefully because gains typically do not continue when the youth returns to family and the community. Certain kinds of interventions will not work, for example, one-time, time-limited, short-term interventions or inoculation approaches.
The result is red when acne is severe medicine for depression generic bimat 3 ml online, but it can bumps (papules) and pus-flled pimples (pustules) medicine 7 day box purchase bimat discount. When these types of acne heal treatment urinary incontinence buy discount bimat 3ml on-line, they may leave behind discolored areas or true scars medicine 44-527 order bimat 3ml without prescription. Medications for acne try to stop the formation of new pimples by reducing or removing the oil treatment genital herpes bimat 3 ml otc, bacteria schedule 9 medications purchase discount bimat online, and other things (like dead skin Cost of the acne medications. It may take from 4 to 8 weeks ?dry or ?combination skin, for before you see any improvement and know if the medication is efective. Remember, these Potential side efects of medications do not ?cure the condition?the acne improves because the medication. Therefore, treatment must be continued in order to the ease or overall complexity of prevent the return of acne lesions. Some are applied to the skin (?topical medications) and some are taken by mouth (?oral medications). If acne is more severe and it does not respond adequately to a topical 1 medication, or if it covers large body surface areas such as the back and/ or chest, oral antibiotics and/or oral hormone therapy may be prescribed. Some patients have a good result with just one medication, Acne most commonly afects teenagers, but many will need to use a combination of treatments: two or more but it is not just a condition of adolescence. In many preadolescent children, Another treatment used for acne may include corticosteroid injections, acne may be the frst sign of puberty (sexual which are used to help relieve pain, decrease the size, and encourage development). Also, dermatologists be seen before the development of breasts, sometimes perform ?acne surgery, using a fne needle, a pointed blade, pubic and underarm hair, and frst menstruation or an instrument known as a comedone extractor to mechanically clean (period). One must always weigh the risk for inducing a scar the testicles and penis enlarge, pubic and with the potential benefts of any procedure. When this occurs, it Heat-based devices, and light and laser therapy are being studied to see is particularly important that a health care provider evaluate the condition. A physician whether there is any role for such treatments in mild to moderate acne. At should evaluate any child with acne that starts this time, there is not enough evidence to make general recommendations between the ages of 1 and 7 years of age, as about their use. A benzoyl peroxide ?wash may be recommended for use on large areas such as the chest In most preadolescents, acne is a milder and/or back. Be careful because benzoyl group have whiteheads and blackheads peroxide can bleach towels and clothing! Comedones are usually small bumps lead to excessive irritation and should be avoided during retinoid therapy. Topical However, some preadolescents do have more antibiotics commonly used in acne include clindamycin, erythromycin, severe acne. This may be a sign that a child and combination agents (such as clindamycin/benzoyl peroxide or erythromycin/benzoyl peroxide). Mild irritation and dryness are common will have more serious acne later on, so early when frst using these products. Typically, topical antibiotics should not intervention may be even more important. Are acne treatments safe for Other topical agents include salicylic acid, azelaic acid, dapsone, and sulfacetamide. To minimize this, wait 15-20 have been fully tested in adolescents and minutes after washing before applying your topical medication. When applying topical medications also have been used safely and efectively to the face, use the ?5-dot method. Then, place ?dots in each of fve locations of your face: Mid-forehead, each cheek, nose, and chin. Next, rub the medication into the entire area of skin not just on individual pimples! Be patient and use your medicine on a daily basis or as directed for six weeks before asking if your skin looks better. Use the Good skin hygiene is important to support any formulation that has been recommended and don?t switch to other forms unless instructed. If a retinoid product and a benzoyl peroxide Everyone with acne should wash the product are prescribed separately, the benzoyl peroxide should be skin twice a day: Once in the morning applied during the day and the retinoid should be applied later in the and once in the evening. If a once daily routine is easier for you, ask your doctor about any showers you take. The doctor may need to try several medications or your face (unless a medicated cleanser combinations before fnding the one that is best for that patient. These drugs can make your skin more loofah as these can irritate and infame sensitive to the sun. In fact, scrubbing may lead Don?t stop using your acne medications just because your acne got better. Remember, the acne is better because of the medication, and prevention to dryness and irritation that makes the is the key to treatment. These ingredients can be helpful in clearing oil from the skin and sulfamethoxazole; and occasionally cephalexin or azithromycin. A product containing using these products unless specifcally benzoyl peroxide should be used along with these antibiotics to help recommended by your doctor. Also, pay attention to how your sports equipment Isotretinoin, a derivative of vitamin A, is a powerful drug with several (shoulder pads, helmet strap, etc. Picking/ changes; yellowing of the skin (indicating possible liver disease); joint popping acne can also cause a serious pains, and fu-like symptoms. To reduce the risk of these kinds of problems: (1) Always take the pills with Facials and other treatments to remove, lots of water and (2) Don?t take a pill right before getting into bed?stay upright for at least one hour. Minocycline and doxycycline may be taken squeeze, or ?clean out pores are not with food to decrease stomach upset. Manipulating the skin in this way can make acne worse and can lead to severe infections and/or For further information about acne, including information on this in adolescents and young adults: scarring. It also increases the likelihood American Academy of Dermatology: that the skin will not be able to tolerate At night, you can use a mild cleanser (such as Dove, Neutrogena, Purpose, or Cetaphil). Topical Clindamycin) If you notice any of the following, stop using the medication and Clindamycin: Apply this product once or twice a day as instructed by notify your health care provider: headaches; blurred vision; dizziness; your physician. Adapalene, Tretinoin, Tazaotene) of the esophagus; discoloration of scars, gums, or teeth (often with Tretinoin: When applying this topical medication to the face (usually at minocycline); nail changes. Start by placing a small pea-sized amount Minocycline can rarely cause liver disease, joint pains, severe skin rashes, of the medication on your fnger. If you should notice yellowing of the eyes or skin, of your face: mid-forehead, each cheek, nose, and chin. Next, rub the or any of the above, notify your doctor and stop using the medication medication into the entire area of skin not just on individual pimples! Then, place ?dots in each of fve locations physician if you smoke, are pregnant (or trying to become pregnant), of your face: Mid-forehead, each cheek, nose, and chin. Next, rub the have a personal history of breast cancer, have a condition called Factor medication into the entire area of skin not just on individual pimples! Try 5 Leiden defciency, have a family history of clotting problems, regularly to avoid the delicate skin around your eyes and corners of your mouth. Don?t get it on towels, You should not be able to see any of the medicines on your face. A pill stuck in the moisturizer on top of your medicine or you may switch to using the esophagus can cause signifcant burning and irritation. Avoid ?popping a medicine ?every other day or ?every third day instead of daily. If your pill right before bed & stay upright for at least one hour after taking a pill. Discuss this problem with your physician at your the medication and notify your health care provider: headaches; blurred next visit. Taking oral not resolve with acetaminophen or ibuprofen, stop taking the medication antibiotics with food may help with symptoms of upset stomach. Each Step exam will emphasize certain parts of the outline, and no single examination will include questions on all topics in the outline. At times, there is a change in emphasis on new content development that arises from our ongoing peer-review processes. For example, there has been an emphasis on new content developed assessing competencies related to geriatric medicine, and prescription drug use and abuse. While many of the medical issues related to the health care of these special populations are not unique, certain medical illnesses or conditions are either more prevalent, have a different presentation, or are managed differently. Examinees should refer to the test specifications for each examination for more information about which parts of the outline will be emphasized in the examination for which they are preparing. Copyright 2020 by the Federation of State Medical Boards of the United States, Inc. Practice parameters for the diagnosis and management of Parameters, representing the American Academy of Allergy, Asthma & immunode? Algorithm for the diagnosis and management of asthma: a environment is a changing environment, and not all recommendations will practice parameter update. Disease management of drug hypersensitivity: a practice pa Published practice parameters of the Joint Task Force on rameter. Wallace is on the speakers bureau for speakers bureau for Merck, Novartis, Genentech, Critical Therapeutics, Schering Schering-Plough, Aventis, P? Dykewicz has consulting arrangements with AstraZeneca, Glaxo Kline and Schering-Plough and has received research support from Meda, Alcon, and SmithKline, McNeil, Medpointe/Meda, Merck, Novartis/Genentech, Schering Schering-Plough. BaroodyhasconsultingarrangementswithGlaxoSmithKline;has Plough,andTeva;hasreceivedresearchsupportfromAstraZeneca,GlaxoSmithKline, received research support from GlaxoSmithKline and Alcon; and is on the speakers Novartis/Genentech,andSchering-Plough;andisonthespeakers?bureauforAstraZe bureau for Merck and GlaxoSmithKline. Bernsteinhasresearchcontracts withGlaxo with AstraZeneca, Schering-Plough, Merck, and Medpoint and is on the speakers bu SmithKline, AstraZeneca, Schering-Plough, Novartis, and Greer; is on the speakers reau for AstraZeneca, Schering-Plough, Merck, Medpoint, and Genentech. Cox has consulting arrangements with Stallergenes, Greer, No Kline, Alcon, and Genentech. Skoner has consulting arrangements with Merck; vartis/Genentech, Planet Technology, and Schering-Plough and is on the speakers has received research support from AstraZeneca, Sano? Khan has received research Novartis, Merck, and Greer Laboratories; and is on the speakers bureau for Astra support from AstraZeneca and is on the speakers bureau for Merck and GlaxoSmith Zeneca, Sano? Stoloff has consulting arrangements with GlaxoSmithKline, AstraZeneca, Alcon, from,andisonthespeakers?bureauforGlaxoSmithKline,AstraZeneca,Sano? Oppenheimer bureau for GlaxoSmithKline and AstraZeneca; and has served as an expert witness has consulting arrangements with, has received research support from, and is on the for GlaxoSmithKline. Disease management of atopic dermatitis: an updated prac Stanford University Medical Center tice parameter. The diagnosis and management of anaphylaxis: an updated Assistant Clinical Professor of Medicine practice parameter. J Allergy Clin Immunol 2005;115(suppl): Nova Southeastern University College of Osteopathic Medicine S483-S523. J Al University of Texas Southwestern Medical Center lergy Clin Immunol 2005;116(suppl):S3-S11. Ann Allergy 2006; Director, Allergy and Immunology Fellowship Training 96(suppl):S1-S68. Appropriate management of rhinitis may be an Pittsburgh, Pa important component in effective management of coexisting or Stuart W. Evidence from meta-analysis of randomized controlled trials gic to pure nonallergic rhinitis is 3:1. Evidence from at least 1 controlled study without a combination of allergic and nonallergic rhinitis. Worldwide, randomization the prevalence of allergic rhinitis continues to increase. The graded parameter will focus on the diagnosis and treatment of allergic references and? Using the 1998 practice parameter on ?Diagnosis and Summary emphasizes the key updates since the 1998 rhinitis 8 Management of Rhinitis as the basis, the working draft of this parameter (Box). Preparation of this draft included a re and tables because these are created to provide the key information. Published clinical studies were rated by Joint Task Force formulated and graded the Summary Statements. Rhinitis is characterized by 1 or more of the following dren below age 6 years symptoms: nasal congestion, rhinorrhea (anterior and poste d Recommendation of considering second-generation anti rior), sneezing, and itching. D histamines as safe agents for use during pregnancy d Use of intranasal corticosteroids for symptoms of allergic conjunctivitis associated with rhinitis Differential diagnosis of rhinitis and associated d Consideration of using a Rhinitis Action Plan conditions d Emerging diagnostic and surgical procedures, such as 2. Symptoms of allergic rhinitis may occur only during Associated allergic conjunctivitis speci? Allergic rhinitis is often accompanied by symptoms of aller bation, may be perennial with seasonal exacerbations, or gic conjunctivitis. Episodic allergic rhinitis is a new rhinitis category that de topical ophthalmic agents is useful for speci? The severity of allergic rhinitis ranges from mild and inter antihistamines have similar effectiveness in relieving ocular mittent to seriously debilitating. Although there is no generally accepted method of grading the severity of rhinitis, the clinician may want to consider a graphic rating scale. Mixed rhinitis (combined allergic and nonallergic rhinitis) is Nonallergic rhinitis syndromes noted in approximately 44% to 87% of patients with allergic 20. Nonallergic rhinitis is characterized by periodic or perennial rhinitis and is more common than either pure allergic rhinitis symptoms of rhinitis that are not a result of IgE-dependent or nonallergic rhinitis. Allergic rhinitis affects 30 to 60 million people in the United States annually, including 10% to 30% of adults and as Vasomotor rhinitis many as 40% of children. Food allergy is a rare cause of rhinitis without to loss of workplace productivity resulting from the disease associated gastrointestinal, dermatologic, or systemic mani are substantial. The symptoms of allergic rhinitis result from a complex a large number of viruses, but secondary bacterial infection allergen-driven mucosal in?
However medicine bottle cheap 3 ml bimat with amex, cases still occur and children in childcare are at increased risk for many of these diseases because of the many hours they spend in close contact with other children medications with aspirin order bimat 3 ml without a prescription. Children who are not up to date on their vaccinations should be taken out of childcare (excluded) until they have begun the series of shots needed symptoms 0f a mini stroke order bimat 3ml on line. Each child in your care should have an Immunization certificate on file at the facility treatment 0f osteoporosis bimat 3 ml low cost. Each child shall also have a current health appraisal on file signed by a licensed healthcare provider treatment 1st degree burns order 3 ml bimat fast delivery. This health appraisal should include a description of any disability or impairment that may affect adaptation to childcare treatment gonorrhea order bimat overnight delivery. Date: Printed Name: Telephone: 8 Childcare Manual Health History & Immunization Policy for Childcare ProvidersHealth History & Immunization Policy for Childcare Providers Children, especially those in groups, are more likely to get infectious diseases than are adults. As a childcare provider, you will be exposed to infectious diseases more frequently than will someone who has less contact with children. To protect yourself and the children in your care, you need to know what immunizations you received as a child and whether you had certain childhood diseases. If you are not sure, your healthcare provider can test your blood to determine if you are immune to some of these diseases and can vaccinate you against those to which you are not immune. Childcare providers shall also have a health appraisals signed by a licensed healthcare provider on file at the facility. Providers are considered immune to rubella if they have received at least one does of rubella vaccine on or after their first birthday. A blood test indicating immunity to rubella or one dose of rubella vaccine is required. Tetanus, Diphtheria & Pertussis Childcare providers should have a record of receiving a series of 3 doses of Tetanus, Diphtheria and Pertussis containing vaccine (usually given in childhood) and a booster of tetanus given within the past 10 years. Those who have not received the Tdap vaccine (available only since 2005) should receive a single dose. Polio Childcare providers, especially those working with children who are not toilet-trained, should have a record of a primary series of 3 doses (usually given in childhood) and a supplemental fourth dose given at least 6 months after the third dose of the primary series. Providers who have had the disease (confirmed by a healthcare provider) are considered immune. Hepatitis B Childcare providers who may have contact with blood or body fluids or who work with developmentally disabled or aggressive children should be vaccinated against Hepatitis B with one series of 3 doses of vaccine. Children receiving influenza vaccination for the first time should receive 2 vaccinations during the first year. However, the risks of serious disease from not vaccinating are far greater than the risks of serious reaction to the vaccination. You may also contact the National Vaccine Injury Compensation Program at1-800-338-2382 for additional information. By immunizing on time (by age 2), you can protect your child from disease and also protect others at school or daycare. A record should be started at birth when your child receives his/her first vaccination and updated each time your child receives the next scheduled vaccination. This information will help you if you move to a new area or change healthcare providers, or when your child is enrolled in daycare or starts school. Remember to bring this record with you every time your child has a healthcare visit. Further information regarding vaccines and immunizations can be found at. Infection is the term used to describe a situation in which the germ causes disease. In childcare settings the surfaces of floors, activity and food tables, diaper changing tables, doorknobs, restrooms, toys, and fabric objects can have many germs on them if they are not properly cleaned and sanitized. Direct head to head contact, sharing hats or hairbrushes, or storing articles of clothing in close proximity can result in transmission of head lice. Close proximity to respiratory secretions can spread a variety of respiratory germs. Infection Spread by the Fecal-Oral RouteInfection Spread by the Fecal-Oral Route Children in diapers present a high risk for the spread of gastrointestinal infections through contamination of hands or surfaces with fecal matter (stool). Germs can spread by the fecal-oral route if the infected person does not wash hands after changing a diaper, using the restroom or before food preparation or when people eat food contaminated with disease-causing germs from fecal matter. Germs that spread via the fecal-oral route include campylobacter, cryptosporidium, E. Coli O157, giardia, hepatitis A, salmonella, shigella and a variety of gastrointestinal viruses. Teaching children to cover their mouths and noses with a tissue or the inside of their elbow when they cough or sneeze helps to limit the spread of these germs. It is best to use a disposable tissue to cover a cough or sneeze then wash hands before touching anything else. Hand sanitizers should be readily available for use when immediate washing with soap and water is not possible. Infection Spread through Blood, Urine, and SalivaInfection Spread through Blood, Urine, and Saliva Contact with blood and body fluids of another person usually requires more intimate exposure than typically occurs in childcare settings. Some infections are spread through contact with contaminated blood through a cut that lets germs into the body. Following standard precautions to remove blood from the environment safely prevents transmission of bloodborne germs. Infected children can possibly transmit theses infections through biting if there is blood mixed with their saliva. Saliva and urine often contain viruses long after a child has recovered from an illness. Good handwashing and standard precautions will help prevent the spread of these viruses. Thorough cleaning is one of the most important steps in reducing the number of germs and the spread of disease. Surfaces most likely contaminated are those children are routinely in contact with. These include toys that children put in their mouths, crib rails, food preparation areas, and diaper-changing areas. Routine cleaning with soap and water is the most useful method for removing germs from surfaces in the childcare setting. Good mechanical cleaning (scrubbing with soap and water) physically reduces the numbers of germs from the surface, just as handwashing reduces the numbers of germs from the hands. Removing germs in the childcare setting is especially important for soiled surfaces, which cannot be treated with chemical disinfectants, such as some upholstery fabrics. However, some items and surfaces should be disinfected after cleaning with soap and rinsing with clear water. Items that can be washed in a dishwasher or hot cycle of a washing machine do not have to be disinfected because these machines use water that is hot enough for a long enough period of time to kill most germs. Disinfection usually requires soaking or drenching the item for several minutes to give the chemical time to kill the remaining germs. Recipe for: Bleach Disinfecting Solution Weaker Bleach Disinfecting Solution (For use in bathrooms, diapering areas, etc. Therefore, bleach solution should be mixed fresh each day to make sure it is effective. Keep the bleach solution you mix each day in a cool place out of direct sunlight and out of the reach of children. The bleach and water solution or chlorine containing scouring powders or other commercial bathroom surface cleaners/disinfectants can be used in these areas. Surfaces that infants and young toddlers are likely to touch or mouth should be washed with soap and water and disinfected at least once daily and also whenever visibly soiled. After the surface has been drenched or soaked with the disinfectant for at least 10 minutes, surfaces likely to be mouthed should be thoroughly wiped with a fresh towel moistened with tap water. Washing and Disinfecting Diaper Changing AreasWashing and Disinfecting Diaper Changing Areas Diaper changing areas should. Diaper changing areas should be cleaned and disinfected after each diaper change as follows. Washing Potty Chairs and ToiletsWashing Potty Chairs and Toilets Potty chairs are difficult to keep clean and out of reach of children. Small size flushable toilets or modified toilet seats and step aids are preferable. If potty chairs are used for toilet training, you should use potty chairs only in the bathroom area and out of reach of toilets or other potty chairs. Immediately empty the contents into a toilet, being careful not to splash or touch the water in the toilet. Do not rinse the potty in a sink used for washing hands or a sink used for food preparation. You may empty solid stool into the toilet being careful not to splash or touch toilet water with your hands. Explain to parents that washing or rinsing soiled diapers and clothing increases the risk of exposure to germs that cause disease. Although receiving soiled clothes is not pleasant, remind parents that this policy protects the health of all children and providers. Each item of sleep equipment, including cribs, cots, mattresses, blankets, sheets, etc. Infants linens should be cleaned and sanitized daily, and crib mattresses should be cleaned and sanitized weekly and when soiled or wet. Linens from beds of older children should be laundered at least weekly and whenever soiled. Washing and Disinfecting ToysWashing and Disinfecting Toys Whenever possible, infants and toddlers should not share toys. Consistent use of toys that children (particularly infants and toddlers) put in their mouths should be washed and disinfected between uses by individual children. If you cannot wash a toy, it probably is not appropriate for an infant or toddler. When an infant or toddler finishes playing with a toy, you should retrieve it from the play area and put it in a bin reserved for dirty toys. Toys can be washed later, at a more convenient time; then transferred to a bin for clean toys and safely reused by other children. Toys and equipment used by older children and not put into their mouths should be cleaned at least weekly and when visibly soiled. A soap and water wash followed by clear water rinsing and air-drying should be adequate. Cleaning up Body FluidsCleaning up Body Fluids Spills of body fluids, including blood, feces, vomit, urine, nasal and eye discharges, and saliva should be cleaned up immediately. Wear disposable gloves and be careful not to get any of the fluid you are cleaning in your eyes, nose, mouth, or any open sore. Discard fluid-contaminated material in a plastic bag that has been securely sealed. Wrung as dry as possible and hung to dry completely 18 Childcare Manual HandwashingHandwashing the single most effective practice that prevents the spread of germs in the childcare setting is good handwashing. Some activities in particular expose children and providers to germs or allow the opportunity to spread them. You can stop the spread of germs by washing your hands and teaching children in your care good handwashing practices. Use of gloves alone will not prevent contamination of hands or spread of germs and should not be considered a substitute for hand washing. Pre-moistened wipes and waterless hand sanitizers should not be used as a substitute for washing hands with soap and running water. When running water is unavailable, such as during an outing, wipes or waterless hand sanitizers may be used as a temporary measure until hands can be washed under running water. A childcare provider may use a wipe to clean hands while diapering a child who cannot be left alone on a changing table that is not within reach of running water. However, hands should be washed as soon as diapering is completed and child is removed from the changing table. If forced to use a water basin as a temporary measure, clean and disinfect the basin between each use. Pre-moistened cleansing wipes do not effectively clean hands and should not take the place of handwashing. Be sure to scrub between fingers, under fingernails, and around the tops and palms of the hands. If using lotions, use liquids or tubes that can be squirted so that the hands do not have direct contact with container spout. Whichever method you choose, you should never wash or rinse diapers or clothes soiled with fecal material in the childcare setting. Because of the risk of splashing, and gross contamination of hands, sinks, and bathroom surfaces, rinsing increases the risk that you, other providers, and the children would be exposed to germs that cause infection. All soiled clothing should be bagged and sent home with the child without rinsing. Gloves are not required, but some people prefer to use gloves to prevent fecal material from getting under their nails. Using a soft nailbrush to clean under the nails during handwashing will remove soil under the nails. Get Organized Always keep the diaper changing station stocked with all necessary supplies. Do not use areas that come in close contact with children during play, such as furniture or the floor.
Additionally symptoms tonsillitis bimat 3ml sale, children born before screening may present late with clinical features treatment kidney infection generic bimat 3 ml visa, as may babies born abroad symptoms indigestion order discount bimat online. Lack of experience of clinical staff may actually lead to further delays in diagnosis in such groups of children medications to avoid during pregnancy buy bimat 3ml otc. Common features are recurrent respiratory infections and failure to thrive with steatorrhoea (but do not be fooled by the thriving child) treatment for pneumonia buy bimat master card. Finger clubbing and nasal polyps in an older child are also important medicine zofran purchase bimat with paypal, as is isolation of S. We perform the sweat test using the macroduct system, and analysis can be reliably performed on small quantities. Sweat testing can be performed once a baby is > 48 hours old although often inadequate samples are obtained in the first few weeks. As with any of these techniques, it is extremely important that they are performed by personnel who are experienced. The sweat is analysed by the Biochemistry lab and results include sweat volume and Cl levels. If there is any doubt over a result, repeat the test or discuss it with a consultant. Flucloxacillin, commonly listed in old texts as a cause of false positive sweat tests, has no effect on a sweat test result. Beware therefore of excluding the diagnosis (in highly suggestive cases) on the basis of a normal sweat test alone. Discuss the case and the possibility of nasal potential difference testing with Prof Jane Davies (see later). Many theoretical causes as listed in textbooks, most of which do not appear to cause problems in routine clinical practice. Those which may be encountered include malnutrition or skin disorders such as severe dermatitis/eczema. Transient increases in sweat electrolytes have also been reported in young patients with immunodeficiency states. The latter would detect carriers, which is something that should be postponed until the sibling is old enough to decide whether they wish to know their carrier status (usually mid teens and older). Based on current knowledge, genotype analysis should not be used to guide prognosis in an individual child, except rarely (and very cautiously) in the case of mutations usually associated with pancreatic sufficiency. Although 53 Clinical guidelines for the care of children with cystic fibrosis 2017 Limitations of mutation analysis Due to the large number of identified mutations, and the extreme rarity of many of these, it is only practical to screen for a few on a routine basis. This will usually include the commonest 50 mutations (which is standard at our genetic referral lab, Kennedy-Galton and costs? There is now a specific panel of mutations, which are common in the Asian community. Full gene sequencing can be performed if specifically requested but is expensive (in the order of? Samples need to be either given to Jackie Francis or sent to our Clinical Biochemistry Laboratory who will forward them. Mutations of varying clinical consequence There are a number of mutations in this category. Most common one leading to this scenario is R117H/7T (if R117H is reported, always make sure the 7T/5T variant is included, otherwise check with lab). Severe or persistent symptoms would be of concern, as would those accompanied by positive cultures such as P. It is likely that we may see them with decreasing frequency and/ or transition to telephone follow up during childhood. Failure to detect both mutations in the proband does not rule out the possibility of antenatal or sibling diagnosis, as linkage analysis may be possible. Our advice is that the child is not taken home until it has established feeding and had a normal bowel motion. Normal levels (are expected by day 3 in term infants and by 2 weeks of age in those born less than 28 weeks gestation, so tests should not be performed before this time. Normal > 200 mcg/g stool Mild/moderate pancreatic insufficiency 100-200 mcg/g stool Severe pancreatic insufficiency < 100 mcg/g stool these are sent by our biochemistry lab to Biochemistry Department of Sandwell and West Birmingham City Hospital. For newborn screened babies, the lab will prioritise samples to try to get the result back in 4 days, so that it will be ready for when the parents come in for their Education Visit. We rarely obtain useful readings in the presence of nasal polyps or if there has been previous nasal surgery, and it should definitely be postponed if the child has had a cold within the last 2 weeks. Our latest audit of data no longer supports use of routine bronchoscopy over surveillance swabs, which has been aided by the introduction of induced sputum cultures. We are also aware that it is quite difficult for the families to have their baby undergo this general anaesthetic procedure. We will continue to have a low threshold for starting reflux therapy when babies have symptoms. Around 30% never recover their previous spirometry, and multiple exacerbations are associated with an accelerated decline in lung function, and greater likelihood of progression to transplantation or death. Sometimes telephone advice can be given (by nurse specialist, SpR or more senior doctor only) but often the patient will need to be seen. Preferred option is in the next clinic, but they may be seen on the ward in special circumstances. Remember with the segregated clinic system the family cannot be told they can turn up any time in the afternoon of the clinic day. If the family comes from a long way away, then consider using the local hospital, but brief whoever will see them there and ask for a report back. Increased cough, and in particular a new or increased ?wet cough should always be taken seriously. Whereas it is completely fine to give repeated oral courses to cover viral colds if the child is well between colds, multiple oral courses to the chronically symptomatic, non-responding child are not useful. The published literature shows that virtually all improvement in spirometry occurs by day 13, and if there is no improvement by day 7, this is an adverse prognostic sign. We therefore need to formally reassess progress on day 6-9, and if there is no improvement in spirometry consider (a) induced sputum or bronchoscopy to determine if there is an untreated infection; 59 Clinical guidelines for the care of children with cystic fibrosis 2017 At the very least, a crude adherence check (prescription uptake and downloading data from their nebuliser) should be performed. Introduction some principles Note that if a patient is still symptomatic or has a positive culture after an appropriate course of antibiotics, admission should be discussed with a consultant. We should not give endless oral courses; the use of more than two successive courses of oral antibiotics for the same exacerbation must be discussed with the consultant; but this is a different situation from the nd child who gets completely better, and a few weeks later has a 2 oral course, from which they get better again. In general, high doses are required because of high renal clearance and also to ensure high levels of tissue and sputum penetration (see drug formulary section 11). When results of sputum culture are available, confirm that all organisms are covered by the chosen regimen. However, if the child is improving clinically on antibiotics to which the organisms exhibit in vitro resistance, do not automatically change them (but discuss with consultant). There is no evidence that in vitro sensitivity testing correlates with clinical outcomes. It is particularly important that this happens for ?out of hours calls taken by the SpR. If on no prophylaxis, you must prescribe an antibiotic, which will cover S aureus and H st influenzae. We do not tend to use oral cephalosporins although the concern with P aeruginosa relates more to their prophylactic use. Note that cefixime has no anti-staphylococcal activity, and should not be used in this context. They must be given for a minimum of 2 weeks, but carried on for at least 1 week once st the child is symptom-free. So if for example, the child is completely well after the 1 week, then they can stop the antibiotics at 2 weeks. If it takes 2 weeks to become symptom free, the antibiotics can be stopped at 3 weeks. Remember a normal child with a normal cold may have symptoms for 3 weeks, and 10 colds a year is normal in a pre-school child. Oral ciprofloxacin for 2-3 weeks if no course within previous 3 months, and previous isolation of P aeruginosa. In general, we try to reserve ciprofloxacin for exacerbations rather than simply to cover a minor cold. Co-trimoxazole is also used, but concerns about the rare complication of bone marrow suppression remain. Surveillance respiratory cultures Cough swabs/sputum must be sent every time a child is seen in clinic, the ward or at home. Also culture sputum if produced for non-tuberculous mycobacteria on annual assessment visit, in a child who is unwell but culture-negative, on bronchoalveolar lavage, and on admission for an exacerbation, and also when previously cultured. If a child is known to be chronically infected with a particular organism (3 positive samples in the last year), and the child is well and asymptomatic, a positive routine clinic swab is not necessarily treated, although often will be. For any gram-negative organism we must have full identification & extended sensitivities. Sometimes it turns out to be a Pseudomonas (not aeruginosa) and it is not enough to accept a report that says ?coliforms or ?gram-negative bacilli for example, from a local hospital. Ask the laboratory to send the strain for typing to the Public Health England Laboratory at Colindale (see appendix 20 for contact details). Start with meropenem (more gram positive and anaerobic cover than ceftazidime), and tobramycin. When to change antibiotics There is no evidence that in vitro sensitivities correlate with in vivo outcome. If the child is not responding, a change may be indicated whatever the sensitivities again, discuss with the consultant. A positive culture result will guide choice of antibiotic treatment, although the evidence that culture results predict treatment is weak. Do not change antibiotic therapy which is working just because of a culture result. The question of staphylococcal prophylaxis is based on a few studies only and evidence for benefit is weak. However it is our policy to start it in all newborn screened children, unless there is a compelling reason not to , i. It may be necessary to switch to co-amoxiclav, but we are reducing our use of co-amoxiclav as a prophylactic agent. In penicillin allergic children, if the history is dubious or uncertain we will test to ensure they have a true penicillin allergy before considering using a macrolide (with a strong history, testing is unnecessary). Oral cephalosporins should not be used for prophylaxis (or if at all possible for treatment) because of evidence implicating this class of antibiotics as causing a greater prevalence of infection with mucoid P aeruginosa. If already on flucloxacillin prophylaxis, give treatment dose for 4 weeks if S aureus is isolated and thought to be cause of the exacerbation. In a well child (clinical judgment) receiving flucloxacillin prophylaxis, we use oral co amoxiclav for 4 weeks. If there are more than 2 isolates of S aureus in a year, give prophylaxis with flucloxacillin as above (remember under 3s will be on flucloxacillin anyway). For example co-amoxiclav; fusidic acid and rifampicin (in combination), co-trimoxazole or nebulised vancomycin if this persists. In a relatively well child (clinical judgment) we use oral co-amoxiclav for 4 weeks. This may be combined with azithromycin or clarithromycin; one further course of a cephalosporin can be given if no eradication/persistent symptoms. The sole indication for cefixime is proven H influenzae isolation in pure culture, with no response to first line antibiotics. Further re-growth within 6 months clarithromycin for 14-28 days (assuming not resistant). If > 2 isolates of H influenzae in a year, consider co-amoxiclav prophylaxis, although evidence is even less secure and we are reducing our use of this drug as a prophylactic agent. Long term azithromycin may be continued for anti inflammatory / immunomodulatory effects, but it is not good for S aureus (due to resistance) and so is not used for prophylaxis, unless no other option is available. Cephalosporins are not to be used for long term prophylaxis because of worries about increased Pseudomonas isolation. Pseudomonas aeruginosa If the report indicates the organism is resistant to colistin, this may well be a Burkholderia species not Pseudomonas, and the sample must be sent to the Public Health England Laboratory at Colindale (see appendix 20 for contact details). Isolations of P aeruginosa after six months or more of clear cultures are always treated. We assume this is a new isolate so attempt re-eradication with 3 weeks oral ciprofloxacin plus 1 month nebulised tobramycin. However, do not take the statement ?Chronic Pseudomonas Infection in the letter on trust; all letters must state date of last isolation and whether mucoid/non-mucoid. If in doubt, get out the previous culture results and discuss with the Consultant. Consultant decision only, for very resistant PsA in children 12 years and above and adults. Note that ototoxicity is a proven side-effect of aminoglycosides, in particular amikacin, and families should be warned about this and offered the information sheet each time. There is evidence that once-daily dosing of aminoglycosides is less toxic and results in more effective bacterial killing than conventional three-times daily dosing. There is also evidence that the incidence of P aeruginosa resistance to aminoglycosides may decrease with once daily rather than three-times daily administration. In addition, less money is spent on 66 Clinical guidelines for the care of children with cystic fibrosis 2017 The aminoglycoside regimen is now: Tobramycin 10 mg/kg once daily over 30 minutes Amikacin 30 mg/kg once daily over 30 minutes the aminoglycoside should ideally be administered in the morning or early afternoon because there is a circadian variation in renal toxicity.
Discount bimat uk. Peter Gibson "Macrolides in Asthma and COPD".
References
- Laschinger J, Razumovsky AY, Stierer KA, et al: Cardiac surgery: Value of neuromonitoring, Heart Surg Forum 6:204, 2003.
- Hemal, A.K., Kolla, S.B., Wadhwa, P. Robotic reconstruction for recurrent supratrigonal vesicovaginal fistulas. J Urol 2008;180:981-985.
- Upreti R, Hughes KA, Livingstone DE, et al: 5-reductase type 1 modulates insulin sensitivity in men, J Clin Endocrinol Metab 99(8):E1397nE1406, 2014.
- Cassese S, de Waha A, Ndrepepa G, et al. Intra-aortic balloon counterpulsation in patients with acute myocardial infarction without cardiogenic shock. A meta-analysis of randomized trials. Am Heart J. 2012;164:58.