Mohan S. Gundeti, MB, MS, DNBE, MCh (Urol), FEBU, FICS, FRCS (Urol), FEAPU
- Assistant Professor of Urology in Surgery and Pediatrics,
- The University of Chicago and Pritzker School of Medicine
- Director, Pediatric Urology, and Chief Pediatric Urologist,
- Comer Children? Hospital, the University of Chicago
- Medical Center, Chicago, Illinois
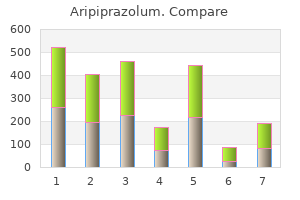
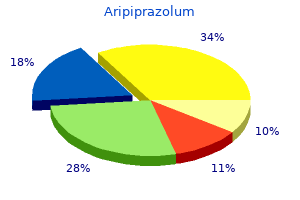
This means that in subsequent erythrocyte transfusions anxiety girl meme purchase aripiprazolum 20mg without prescription, the cross match must be performed using the serum/plasma both from the mother and the child depression symptoms for 13 year olds order aripiprazolum 20mg without a prescription. Antibodies against low frequency antigens occur primarily in patients who already have IgG antibodies in their circulation depression books buy generic aripiprazolum 10mg on-line. A cross match in the indirect anti-globulin test is not strictly necessary for patients with clinically irrelevant alloantibodies anxiety techniques buy discount aripiprazolum 20mg online. For patients with clinically significant alloantibodies anxiety vs panic attack purchase aripiprazolum pills in toronto, it is essential that the compatibility of an erythrocyte unit be checked by means of a cross match in the indirect anti-globulin test between the erythrocytes from the donor Level 4 and the serum/plasma of the patient mood disorder questionnaire history safe aripiprazolum 10 mg. C Lee 2007, Engelfriet 2000 For patients who have undergone transplantation of a vascularised organ, it is essential to check the compatibility of an erythrocyte unit by means of a cross match in the indirect anti-globulin test between the erythrocytes Level 4 from the donor and the serum/plasma from the patient in the subsequent period of three months. A blood transfusion with a unit of erythrocytes that is positive for the antigen against which the antibodies are targeted can cause a (delayed) haemolytic transfusion reaction. Patients with clinically significant erythrocyte alloantibodies should therefore only receive erythrocytes that are negative for the relevant blood group antigens, see 3. Therefore, if there are irregular erythrocyte antibodies, the antibodies must be identified. In order to identify an alloantibody with certainty, the study must meet the following requirements: the antibody identification is primarily performed using the technique with which the antibodies were demonstrated. If an anti-D antibody is present, the presence of anti-C and anti-E antibodies may be ruled out heterozygously. An anti-E may also be ruled out heterozygously in the presence of an anti-c, and an anti-C may be ruled out heterozygously in the presence of an anti-e. Identification studies can be extremely complicated in patients with clinically relevant autoantibodies. The chance of the presence of alloantibodies or alloantibody formation is 76 Blood Transfusion Guideline, 2011 relatively large (in excess of 30%) in patients with autoantibodies(Ahrens 2007, Engelfriet 2000). Therefore, it is important for this group that the presence of alloantibodies be ruled out (as far as possible), for example using adsorption techniques (Leger 1999, Engelfriet 2000). If this study is not possible due to time constraints, it is preferable to transfuse the patient with donor erythrocytes that are compatible with the Rhesus phenotype, the K antigen and the antigens of the Kidd system. Matches for Duffy and Ss antigens are also preferably indicated (in order of importance), also see other considerations. As antibodies against erythrocytes can decrease in concentration over time and can then no longer be demonstrated, it is important to accurately record the data concerning clinically significant erythrocyte antibodies (Schonewille 2000, Sazama 1990). C Leger 1999, Engelfriet 2000, Ahrens 2007 Level 3 Antibodies against erythrocytes can decrease in concentration over time Blood Transfusion Guideline, 2011 77 77 and therefore no longer be detectable. C Schonewille 2000, Sazama 1990 Other considerations the antigens of the Rhesus, Kell, Kidd and Ss systems can usually be detected serologically with monoclonal reagents in patients with warm autoantibodies, provided the person has not received a transfusion in the past three months. In the case of complex antibody identification, for example due to a combination of several antibodies, or antibodies targeted against high frequency antigens, the use of various panels of test erythrocytes is essential. In order to identify an alloantibody with certainty, the study must meet the following requirements: * the antibody identification should primarily be performed using the technique with which the antibodies were demonstrated. This 2 a b a b includes: antibodies against the C, c, D, E, e, K, Fy, Fy, Jk, Jk, M, S and s antigens must be ruled out using homozygous test erythrocytes, and antibodies against the K antigen can be ruled out using heterozygous test erythrocytes. If an anti-RhD antibody is present, the presence of any anti-C and anti-E antibodies may be ruled out using heterozygous test erythrocytes. In the presence of an anti-c, the presence of an anti-E may be ruled out using heterozygous test erythrocytes and if an anti-e is present, the presence of an anti-C antibody may be ruled out in the same manner. If this exclusion study cannot be performed (completely), erythrocytes that are compatible for Kidd, Duffy, S and s can also be considered as a preventative measure. The validity of the result of the antibody identification study is a maximum of 72 hours after collection of the sample during the first three months after transfusion or pregnancy. The presence of clinically relevant irregular erythrocyte antibodies should be 78 Blood Transfusion Guideline, 2011 recorded accurately. In these types of situations the working group deems it desirable to consult a specialised laboratory. Some weak antibodies targeted against antigens in the Kidd system, for example, can only be demonstrated because they bind complement (Klein 2005). Level 3 C Klein 2005, Nance 1987 the method and technique used to demonstrate the presence of erythrocyte antibodies must be sufficiently sensitive to demonstrate Kidd Level 3 antibodies. There must be a procedure in place in the hospital to record the result of irregular erythrocyte antibodies determined by third parties as such with source reporting. Level 3 C McClelland 1994, Sazama 1990 Six to twenty percent of the errors were made during the selection of blood components from the stock and during the transfer of these components Level 3 from the blood transfusion laboratory to the ward. C Williamson 1999, Linden 1992 Other considerations When blood components that have been declared compatible are released to the ward, there is a transfer of the responsibility from the blood transfusion laboratory to the ward. The procedure up to and including the administration of blood components should be recorded and registered within legal parameters using a sound administrative system. Examples of such a checking procedure for the release of blood components from the blood transfusion laboratory to the ward are described in table 3. Exceptions are made for wards that have a validated and monitored blood storage refrigerator. In accordance with European legislation, this registration is stored for a minimum of 30 years. The procedure for the transfer of blood components from the blood transfusion laboratory to the ward should be recorded in writing. This procedure should describe checks that are performed to prevent possible administrative mix-ups. If possible, the blood transfusion laboratory releases one unit of blood component per patient, per time to a ward. The blood transfusion laboratory must supply an (electronic) accompanying form to the ward with each blood component. In accordance with European legislation, this administration should be stored for 30 years. An RhD positive recipient can receive both RhD positive and RhD negative donor blood transfusions. Consequently, a blood group O RhD negative erythrocyte concentrate is compatible for all recipients. However, practical experience from Sanquin Blood Supply shows that a much higher percentage of blood group O RhD negative units is used, 13. The use of O RhD negative units is therefore higher than expected based on statistical calculations. As a result, this places an additional burden on the donor population with this specific blood group (11. The chance of the presence of anti-RhD antibodies is smaller in male RhD negative patients than in female RhD negative patients, who can become immunised through pregnancy. The clinical importance of the development of anti-RhD antibodies is less important in RhD negative men than in RhD negative women < 45 years of age. In RhD negative women of childbearing age, the presence of anti-D antibodies can cause complications for the foetus during pregnancy and can also have consequences for the neonate. For the selection of RhD identical units, it is recommended that negative units be selected for women younger than 45 years if the RhD blood group has not been determined with certainty. For men with a negative antibody screening, the selection of RhD identical units can be considered for a one-off RhD determination. In emergencies, women over the age of 45 years and men with unknown RhD blood group can also receive RhD positive units (Gonzalez 2008). It is essential that the hospitals take the necessary logistical measures to reduce the unnecessary use of blood group O RhD negative erythrocytes. For men with a negative antibody screening, the selection of RhD identical units can be considered after a one-off RhD determination. In emergencies, women over the age of 45 years and men with unknown RhD blood group can also receive RhD positive units. For patients known to have clinically relevant allo-erythrocyte antibodies, only blood from which the relevant antigen is missing will be selected. This is performed, among other reasons, to rule out any incompatibility due to antibodies targeted against specific (private) antigens that are not routinely present on test erythrocytes. If the transfusion cannot wait for the result of the antibody identification or the selection of typed units, the treating doctor and blood transfusion specialist must weigh the risk of transfusion reactions. After anti-RhD, Caucasian patients most readily form antibodies against K, E and c. It is therefore recommended that rhesus phenotype and K compatible erythrocytes be administered as a preventative measure to recipients with clinically relevant alloantibodies, in order to prevent further antibody formation. Rhesus phenotype and K matching in a b immunised patients reduces additional antibody formation by 71%, addition of Fy, Jk and S reduces antibody formation by 93% (Schonewille 2006). For patients known to have clinically relevant allo-erythrocyte antibodies, only blood from which the relevant antigen is missing should be selected. For patients with clinically irrelevant alloantibodies against erythrocytes, a negative cross match performed in the indirect agglutination test is sufficient if this result is negative. For patients with known erythrocyte antibodies, the treating doctor must weigh the risk of transfusion reactions due to non-selected units against the risk of delaying the blood transfusion until compatible units have been found. In order to rule out antibodies against specific (private) antigens, a complete cross match (including indirect anti-globulin phase) should always be performed during the compatibility study. It is recommended that rhesus phenotype and K compatible erythrocytes be administered to recipients with clinically relevant alloantibodies, in order to prevent further antibody formation. In addition to RhD antibodies, other irregular antibodies can also be responsible for this. In the Caucasian population, 91% is negative for the K-antigen and 9% is positive. The large majority of the Dutch donor population is typed for the rhesus phenotype (C, c, D, E and e) and the K-type (K negative or K positive). A Health Council Committee on Pregnancy Immunisation concluded in its report in 2009 that it is recommended to give erythrocytes that are compatible with regard to the antigens c, E and K during blood transfusion to girls and women up to the age of 45 years (Health Council 2009). It was left up to the professionals to determine how this recommendation is implemented. Level 3 B Koelewijn 2009 C Castel 1996, Van Dijk 1991, Contreras 1991 In the Caucasian population, 91% is negative for the K-antigen and 9% is positive. If the typing of the K antigen for the patient is known, then K compatible blood can also be transfused. The study by Ness et al has shown this to 10% in children and up to 50% in adults with sickle cell anaemia (Ness 1994). Olujohungbe et al state a figure of 76% allo88 Blood Transfusion Guideline, 2011 immunisation in patients with sickle cell anaemia in the United Kingdom (Olujohungbe 2001), primarily caused by racial differences between donor and recipient (Vishinski 1990). What probably played a role in these studies is the fact that a group of primarily Negroid patients was transfused with blood from white donors, who have different frequencies of blood groups. Spanos described a similar phenomenon in patients with thalassaemia (Spanos 1990). There are no control studies that examine the effect of matching to prevent alloantibody formation. Three observational studies support the matching for the complete rhesus phenotype and blood group K (Wayne 1995, Pearlman 1994, Russel 1984). The degree of immunisation in these patients decreases as a result of selection of rhesus phenotype compatible and K negative blood.
Allow bleach to contact surfaces for at least 1 minute and then follow with a water rinse land depression definition purchase on line aripiprazolum. Submerge the manifold in household bleach diluted 1:1 with water depression definition et synonyme cheap aripiprazolum 15 mg otc, ensuring that the handles and pipette tip nozzles are covered by the bleach solution mood disorder nos dsm 5 code buy cheapest aripiprazolum and aripiprazolum. Rinse the manifold thoroughly with water and then dry completely with paper towels anxiety 6 months after quitting smoking order 10 mg aripiprazolum with amex. Reconnect the manifold and run the pump for 3 minutes to complete the drying process depression test cost discount aripiprazolum 20mg fast delivery. Follow the bleach step with a water rinse and then dry completely with paper towels depression wiki purchase genuine aripiprazolum line. Racks Submerge the racks in household bleach diluted 1:1 with water, ensuring that they are covered by the bleach solution. The introduction of contaminating materials may occur if sufficient care is not taken during the assay protocol. As in any reagent system, excess powder on some gloves may cause contamination of opened tubes. A test result may be invalid due to a parameter outside the normal expected ranges. If desired, a dual negative control furnished by the user can be added to monitor assay background. Test results may be affected by improper specimen collection, improper specimen storage, technical error, or specimen mix-up. Urine specimens were evaluated for interference by blood, commonly used vitamins, minerals, and over-the-counter pain relievers. The effects of tampon use, douching, and specimen collection variables have not been assessed for their impact on the detection of C. The presence of mucus in endocervical samples does not interfere with the detection of C. Failure to follow the instructions given in this insert may result in erroneous results. This method has been tested using endocervical and male urethral swab specimens and female and male urine specimens only. Urine sampling is not designed to replace cervical exams and endocervical samples for diagnosis of female urogenital infections. Patients may have cervicitis, urethritis, urinary tract infections, or vaginal infections due to other causes or concurrent infections with other agents. Because the transport system used for this assay does not permit microscopic assessment of specimen adequacy, training of clinicians in proper specimen collection techniques is necessary. Test results may be affected by improper specimen collection, technical error, or specimen mix-up. Therefore, a correlation cannot be drawn between the magnitude of a positive assay signal and the number of organisms in a specimen. Positive results in low prevalence populations should be interpreted carefully with the understanding that the likelihood of a false positive may be higher than a true positive. Additional volumetric verifications and assay specific studies will be performed prior to , or as part of, the installation and acceptance process in laboratories above 2700 ft altitude. These calculations are based on a hypothetical prevalence and the overall sensitivity and specificity calculated from the patient infected status. As many as three urethral swabs and a urine specimen were collected from male subjects and four endocervical swabs and a urine specimen were collected from female subjects. The designation of a subject being infected, not infected, or inconclusive was based on the combined results of the comparator assay swab and urine results. A negative culture and a single positive result by the amplified comparator assay resulted in an inconclusive status. Specimens with missing comparator assay results, single positive results, or insufficient numbers of specimens were originally classified as inconclusive during the clinical trial. As part of a subsequent data analysis, these inconclusive specimens were reclassified as non-infected. Performance of the assay with specimens from pregnant females was assessed in the clinical trial. Specificity for swab and urine specimens was 100% (26/26) and 100% (26/26), respectively. Each site was provided with three identical panels of 13 samples containing 0 to 500 fg of C. Analytical Sensitivity Chlamydia trachomatis analytical sensitivity (limits of detection) was determined by directly comparing dilutions of C. The analytical sensitivity claim for the assay is 50 cells/assay (362 cells/swab, 250 cells/mL urine). These isolates included 86 organisms that may be isolated from the urogenital tract and 68 additional organisms that represent a phylogenetic cross-section of organisms. B 27 Interfering Substances Table 16 lists the commonly encountered substances found in swab and/or urine specimens that were tested in the assay. All were tested for potential assay interference in the absence and presence of C. Table 16: Interfering Substances Testing Swab Urine 10% Blood 30% Blood Contraceptive jelly Urine analytes: Spermicide Protein Moisturizer Glucose Hemorrhoidal anesthetic Ketones Body oil Bilirubin Powder Nitrate Anti-fungal cream Urobilinogen Vaginal lubricants pH 4 (acidic) Feminine spray pH 9 (alkaline) 6 6 Leukocytes (1 x 10 cells/mL) Leukocytes (1 x 10 cells/mL) Cellular debris Vitamins Minerals Acetaminophen Aspirin Ibuprofen No interference was observed with any of the tested substances. Swab and Urine Specimen Stability Studies Data to support the recommended shipping and storage conditions for swab samples were generated with pooled negative endocervical swab samples. Data to support the recommended shipping and storage conditions for urine samples were generated with 10 female and 10 male negative urine samples. Clinical Specimen Agreement Study the clinical specimen agreement study evaluated agreement between the two systems using swab and urine specimens from 485 male and 576 female subjects. Positive and negative percent agreements are shown in Tables 19 and 20 where results are stratified by symptom status and gender for each specimen type. Positive agreements for the total number of swab and urine specimens tested ranged from 91. Negative agreements for the total number of swab and urine specimens ranged from 99. Positive and negative agreements calculated by gender and symptom status were based on small sample sizes and are not intended to represent assay performance. Performance estimates would be expected to be similar given the agreement findings across different genders and specimen types. Performance estimates would be expected to be similar given the agreement findings across different genders. Analytical Specificity Equivalence Study For a nucleic acid amplification assay, analytical specificity with respect to individual organisms is largely determined by the chemistry of the assay. Twenty-four (24) culture isolates were selected from the panel of organisms in Table 15, including 3 organisms that are most closely related to C. All samples containing target nucleic acid were positive when tested at a level of 10% blood in swab specimens and 30% blood in urine specimens. A total of 25 negative samples were reported as invalid and were excluded from the calculation. A separate analysis was conducted on a subset of the study population comprised of the negative samples that immediately followed a high-target positive. Respiratory tract colonization and a distinctive pneumonia syndrome in infants infected with Chlamydia trachomatis. Detection of Chlamydia trachomatis and Neisseria gonorrhoeae by Ligase chain reaction-based assays with clinical specimens from various sites: implications for diagnostic testing and screening. Urinary inhibitors of polymerase chain reaction and Ligase chain reaction and testing of multiple specimens may contribute to lower assay sensitivities for diagnosing Chlamydia trachomatis infected women. Direct detection of Chlamydia trachomatis in urine specimens from symptomatic and asymptomatic men by using a rapid polymerase chain reaction assay. Any other brand name that may appear in this package insert belongs to its respective owner. This product and its use are covered under one or more of the following patents: U. This guideline includes the level of recommendation and quality of evidence indicators for the treatment recommendations. Preventive Services Task Force and the Canadian Task Force on Preventive Health Care and have been modified and simplified for use as outlined below (re-printed with permission from the Canadian Guidelines on Sexually Transmitted Infections). Levels of recommendation and quality of evidence were adapted from the Canadian Guidelines for Sexually Transmitted Infections; if Alberta guidelines differ from the Canadian Guidelines for Sexually Transmitted Infections levels of recommendation and quality of evidence are based on a comprehensive literature review. At least clinical trial without randomization, from cohort concludes that benefits substantially outweigh fair evidence that the treatment is ineffective or case-control analytic studies (preferably harms. Contacts (all chlamydia cases) Prophylactic treatment is not *Available data suggests that azithromycin is All contacts in the last 60 days, regardless of recommended unless follow-up cannot be safe and effective in pregnant women. Therefore, not everyone with positive history of prior treatment or stable serology. Primary, Secondary, Early Latent gestation, a detailed fetal ultrasound should be performed and she should be managed Contacts (all syphilis cases) Preferred together with a materno-fetal specialist. Minimum Herxheimer reaction which may cause fetal trace back periods are as follows: primary Alternate (Only for penicillin allergic distress or premature labor; therefore all syphilis: 3 months, secondary syphilis: 6 patients) patients > 20 weeks gestation should months, early latent: 1 year. There is no satisfactory female cases and regular partners of all alternative to penicillin in pregnancy. Primary, Secondary, Early Latent Strongly consider penicillin desensitization Long-acting benzathine penicillin G 2. Screening should be performed in the first trimester and again at the time of delivery. A risk of preterm rupture of membranes and single oral dose also has a cure rate of * the effect of oral metronidazole on the nursing stillbirth. Vulvovaginal Candidiasis Non-Pregnant/Non-Lactating Women Pregnant/Breastfeeding Women Treatment of sexual partners is not Preferred Preferred routinely recommended unless male Topical Agents Topical azole for 7 days (A-1) partner has candida balanitis. In males, use Intravaginal, over-the-counter azole ovules and a topical azole cream twice a day for 7 creams. Fort McMurray, Alberta T9H 5E5 Information for the general public can be obtained through Health Link at 811. Children under 12 do not have the legal capacity to consent to any form of sexual activity. The percentage of women and heterosexual men with chlamydia remained stable between 2016-2018 (15 percent and 18 percent respectively) after a steady increase in the two previous years. Resistance to azithromycin has continued to increase: from 2 percent in 2012 to 11 percent in 2018. The number of diagnoses among women and heterosexual men remained very low in 2018, with diagnoses among 0. Bij huisartspraktijken nam het aantal soa-consulten toe, voornamelijk onder personen ouder dan 25 jaar. Infecties werden het vaakst gevonden bij mensen die waren gewaarschuwd voor een soa, gevolgd door mensen met hiv. Het percentage vrouwen en heteroseksuele mannen met chlamydia bleef in de afgelopen 3 jaar stabiel (respectievelijk 15 procent en 18 procent), na een aanhoudende stijging in de voorgaande jaren. Het aantal geschatte diagnoses door huisartsen was in 2017 stabiel ten opzichte van 2016. De resistentie tegen azitromycine steeg in de afgelopen jaren van 2 procent in 2012 tot 11 procent in 2018. Het percentage vrouwen en heteroseksuele mannen met de infectie bleef in 2018 zeer laag, respectievelijk 0,1 en 0,2 procent. Dit percentage daalde na een jarenlange stijging licht, van 2,9 procent in 2016 naar 2,6 procent in 2017 en 2,4 procent in 2018. This is an increase from the 281,300 episodes in 2016 and 267,400 episodes recorded in 2015. Sexually transmitted infections in the Netherlands in 2018 21 Most chlamydia infections were diagnosed in people aged under 25 (63% of registered diagnoses). The number of estimated chlamydia episodes reported in general practice (39,800) increased compared to the previous years. Reporting rates of chlamydia episodes per 1,000 population mainly increased among people aged under 25 (from 3. In general practice, the number of estimated gonorrhoea-episodes increased among men/women from 5,400/2,500 in 2015 to 6,100/2,850 in 2016 and 6,200/3,400 in 2017, mainly recorded in people aged 25 and older. Of these, 527 were diagnosed in 2018 (615 in 2017), though this number can still increase due to reporting delay. In 2017, an estimated 42,000 cases of of genital warts (37,500 in 2016), and 25,800 cases of of genital herpes (22,500 in 2016) were diagnosed. The number of reported acute hepatitis B cases in the notification data decreased compared to the previous year (101 in 2018 versus 115 in 2017). The number of reported acute hepatitis C cases has fluctuated around 60 cases from 2011 onwards (62 in 2018). The main reported transmission route for acute hepatitis C was sexual contact between men (61%). It is also important to keep track of the general population, who test mainly through other care providers or self-testing. Further efforts, such as promotion of condom use, repeat testing, and more effective (timely and complete) partner notification are needed to ensure that people in high-risk groups are effectively targeted. Testing and treatment strategies need to be optimised to maximize the effect of control efforts and to reach those most in need of care. Sexually transmitted infections in the Netherlands in 2018 23 24 Sexually transmitted infections in the Netherlands in 2018 Samenvatting In 2018 hebben er in totaal 152. Om een trendbreuk the voorkomen is het aantal consulten en de vindpercentages voor chlamydia, gonorroe, infectieuze syfilis en hiv per geslacht en seksuele voorkeur berekend met geregistreerde consulten en geaggregeerde data van niet-geregistreerde consulten.
Buy aripiprazolum 15mg overnight delivery. What Causes Light Sensitivity In Your Eyes?.
R Rubber sheets (Mackintosh) are to be cleaned with detergent and water depression supplements order 20mg aripiprazolum free shipping, dried depression symptoms anxiety order aripiprazolum 15 mg line, powdered and replaced depression jury duty generic aripiprazolum 10 mg otc. Infections can be caused by contamination of supplies/equipment with bloodborne viruses and pathogenic bacteria depression online chat safe 20mg aripiprazolum. Cleaning and disinfection of equipment and proper handling of reusable and disposable supplies is critical to the safety of patients in this high-risk area mood disorder odd effective 20mg aripiprazolum. There should be written protocols for cleaning and disinfecting surfaces and equipment in the dialysis unit bipolar depression elderly generic 15 mg aripiprazolum fast delivery. Instructions should includethe steps for careful mechanical cleaning before disinfection. Visitor restrictions apply to all visitors, including staff members and their families. Visitors should clean their hands with hand rub before entering and when leaving the room. An alcohol hand rub should be available at the entrance of the facility/ unit/ ward, along with a poster displaying instructions for using the hand rub. Before entering the room, visitors must enquire at the nursing station for instructions and for gown and mask, if indicated. The patient and the relatives must be educated about the cause, spread and prevention of infection, if any. One attendant should be allowed to stay in the ward with the patient who should be taught to practice hand hygiene before and after touching the patient. There should be a policy on the use of mobile phones and visitors should be taught to decontaminate the phone with a hand rub. Brothers and family members and sisters of paediatric friends who have patients on droplet immunity to your precautions are illness. Take all necessary steps to ensure that biomedical waste is handled without any adverse effect to human health and the environment and in accordance with these rules; b. Make a provision within the premises for a safe, ventilated and secured location for storage of segregated biomedical waste in coloured bags or containers in the manner as specified in Schedule I, to ensure that there shall be no secondary handling, pilferage of recyclables or inadvertent scattering or spillage by animals and the biomedical waste from such place or premises shall be directly transported in the manner as prescribed in these rules to the common biomedical waste treatment facility or for the appropriate treatment and disposal, as the case may be, in the manner as prescribed in Schedule I (Annex 8. Dispose of solid waste other than biomedical waste in accordance with the provisions of respective waste management rules made under the relevant laws and amended from time to time (Solid Waste Rules, 2016 as amended); f. Provide training to all its health-care workers and others, involved in handling of biomedical waste at the time of induction and thereafter at least once every year and the details of training programmes conducted, number of personnel trained and number of personnel not undergone any training shall be provided in the Annual Report; h. Immunize all its health-care workers and others, involved in handling of biomedical waste for protection against diseases including hepatitis B and tetanus that are likely to be transmitted by handling of biomedical waste, in the manner as prescribed in the National Immunization Policy or the guidelines of the Ministry of Health and Family Welfare issued from time to time; i. Ensure segregation of liquid chemical waste at source and ensure pre-treatment or neutralization before mixing with other effiuent generated from health-care facilities; k. Ensure treatment and disposal of liquid waste in accordance with the Water (Prevention and Control of Pollution) Act, 1974 (6 of 1974); l. Ensure occupational safety of all its health-care workers and others involved in handling of biomedical waste by providing appropriate and adequate personal protective equipment; m. Conduct health check up at the time of induction and at least once in a year for all its healthcare workers and others involved in handling of biomedical waste and maintain the records for the same; n. Maintain and update on day-to-day basis the biomedical waste management register and Annexes 213 display the monthly record on its website according to the biomedical waste generated in terms of category and colour coding as specified in Schedule I; o. Report major accidents including accidents caused by fire hazards, blasts during handling of biomedical waste and the remedial action taken and the records relevant thereto, (including nil report) in Form I to the prescribed authority and also along with the annual report; p. All the healthcare facilities (any number of beds) shall make available the annual report on its website within a period of two years from the date of publication of Biomedical Waste Management (Amendment) Rules, 2018, published 16 March 2018); q. Inform the prescribed authority immediately in case the operator of a facility does not collect the biomedical waste within the intended time or as per the agreed time; r. Establish a system to review and monitor the activities related to biomedical waste management, either through an existing committee or by forming a new committee and the committee shall meet once in every six months and the record of the minutes of the meetings of this committee shall be submitted along with the annual report to the prescribed authority and the healthcare establishments having less than 30 beds shall designate a qualified person to review and monitor the activities relating to biomedical waste management within that establishment and submit the annual report; s. All other discarded medicines shall be either sent back to manufacturer or disposed by incineration. Annexes 215 Category Type of waste Type of bag or Treatment and disposable container to be options used (e) Chemical waste: Yellow-coloured Disposed of by incineration or Chemicals used in production containers or plasma of biological and used or non-chlorinated pyrolysis or encapsulation in discarded disinfectants. In the absence of above facilities, shredding or mutilation or combination of sterilization and shredding. Treated waste tubes and sets, catheters, urine to be sent to registered or bags, syringes (without needles authorized recyclers or for and fixed needle syringes) and energy recovery or plastics vacutainers with their needles to diesel or fuel oil or for cut) and gloves. White Waste sharps, including metals: Puncture proof, Autoclaving or dry heat sharps bin Needles, syringes with Leak proof, sterilization followed by (translucent) fixed needles, needles from tamper proof shredding or mutilation or needle tip cutter or burner, containers encapsulation in metal scalpels, blades, or any other container or cement concrete; contaminated sharp object combination of shredding that may cause puncture and cum autoclaving; and sent for cuts. This includes both used, final disposal to iron foundries discarded and contaminated (having consent to operate metal sharps. Blue sharps (a) Glassware: Puncture-proof Disinfection (by soaking the bin Broken or discarded and and leakwashed glass waste after contaminated glass including proof boxes or cleaning with detergent medicine vials and ampoules containers with and sodium hypochlorite except those contaminated with blue-coloured treatment) or through cytotoxic wastes. The deep burial facility shall be located as per the provisions and guidelines issued by Central Pollution Control Board from time to time. There will be no chemical pretreatment before incineration, except for microbiological, laboratory and highly infectious waste. Incineration ash (ash from incineration of any biomedical waste) shall be disposed through hazardous waste treatment, storage and disposal facility, if toxic or hazardous constituents are present beyond the prescribed limits as given in the Hazardous Waste (Management, Handling and Transboundary Movement) Rules, 2008 or as revised from time to time. Dead fetus below the viability period (as per the Medical Termination of Pregnancy Act 1971, amended from time to time) can be considered as human anatomical waste. Such waste should be handed over to the operator of common biomedical waste treatment and disposal facility in yellow bag with a copy of the official Medical Termination of Pregnancy certificate from the Obstetrician or the Medical Superintendent of hospital or healthcare establishment. Cytotoxic drug vials shall not be handed over to unauthorized person under any circumstances. These shall be sent back to the manufactures for necessary disposal at a single point. Residual or discarded chemical wastes, used or discarded disinfectants and chemical sludge can be disposed at hazardous waste treatment, storage and disposal facility. In such case, the waste should be sent to hazardous waste treatment, storage and disposal facility through operator of common biomedical waste treatment and disposal facility only. However, in case there is no common biomedical facility within 75 km distance, the same may be installed by occupier after taking authorization from the State Pollution Control Board. Syringes should be either mutilated or needles should be cut and or stored in tamper-proof, leak-proof and puncture-proof containers for sharps storage. Wherever the occupier is not linked to a disposal facility it shall be the responsibility of the occupier to sterilize and dispose in the manner prescribed. Biomedical waste generated in households during healthcare activities shall be segregated as per these rules and handed over in separate bags or containers to municipal waste collectors. Duties of the operator of a common biomedical waste treatment and disposal facility It shall be the duty of every operator to: a. Take all necessary steps to ensure that the biomedical waste collected from the occupier is transported, handled, stored, treated and disposed of, without any adverse effect to the human health and the environment, in accordance with these rules and guidelines issued by the Central Government or, as the case may be, the Central Pollution Control Board from time to time; b. Ensure timely collection of biomedical waste from the occupier as prescribed under these rules; c. Establish bar coding and global positioning system for handling of biomedical waste in accordance with the guidelines issued by the Central Pollution Control Board by 27 March 2019; d. Inform the prescribed authority immediately regarding the occupiers which are not handing over the segregated biomedical waste in accordance with these rules;. Provide training for all its workers involved in handling of biomedical waste at the time of induction and at least once a year thereafter; f. Assist the occupier in training conducted by them for biomedical waste management; g. Undertake appropriate medical examination at the time of induction and at least once in a year and immunise all its workers involved in handling of biomedical waste for protection against diseases, including hepatitis B and tetanus, that are likely to be transmitted while handling biomedical waste and maintain the records for the same; h. Report major accidents including accidents caused by fire hazards, blasts during handling of biomedical waste and the remedial action taken and the records relevant thereto, (including nil report) in Form I (refer to rules) to the prescribed authority and also along with the annual report; j. Maintain a log book for each of its treatment equipment according to weight of batch; categories of waste treated; time, date and duration of treatment cycle and total hours of operation; k. Allow occupier, who are giving waste for treatment to the operator, to see whether the treatment is carried out as per the rules; l. Supply non-chlorinated plastic coloured bags to the occupier on chargeable basis, if required; n. Common biomedical waste treatment facility shall ensure collection of biomedical waste on holidays also; o. Maintain all record for operation of incineration, hydro or autoclaving for a period of five years; and p. Upgrade existing incinerators to achieve the standards for retention time in secondary chamber and dioxin and furans within two years from the date of this notification. Standards for incineration All incinerators shall meet the following operating and emission standards. Parameter Standards Limiting Sampling duration in minutes, concentration unless stated in mg/Nm3 unless stated 1. The existing incinerators shall comply with the above within a period of two years from the date of the notification. The existing incinerators shall comply with the standards for dioxins and furans of 0. All upcoming common biomedical waste treatment facilities having incineration facility or captive incinerator shall comply with standards for dioxins and furans. The existing secondary combustion chambers of the incinerator and the pollution control devices shall be suitably retrofitted, if necessary, to achieve the emission limits. Wastes to be incinerated shall not be chemically treated with any chlorinated disinfectants. Ash from incineration of biomedical waste shall be disposed of at common hazardous waste treatment and disposal facility. However, it may be disposed of in municipal landfill, if the toxic metals in incineration ash are within the regulatory quantities as defined under the Hazardous Waste (Management and Handling and Transboundary Movement) Rules, 2008 as amended from time to time. Only low sulphur fuel such as light diesel oil or low sulphur heavy stock or diesel, compressed natural gas, liquefied natural gas or liquefied petroleum gas shall be used as fuel in the incinerator. The occupier or operator of a common biomedical waste treatment facility shall monitor the stack gaseous emissions (under optimum capacity of the incinerator) once in three months through a laboratory approved under the Environment (Protection) Act, 1986 and record of such analysis results shall be maintained and submitted to the prescribed authority. The occupier or operator of the common biomedical waste treatment facility shall instal continuous emission monitoring system for the parameters as stipulated by State Pollution Control Board or Pollution Control Committees in authorization and transmit the data real time to the servers at State Pollution Control Board or Pollution Control Committees and Central Pollution Control Board. Incinerators (combustion chambers) shall be operated with such temperature, retention time and turbulence, as to achieve Total Organic Carbon content in the slag and bottom ashes less than 3% or their loss on ignition shall be less than 5% of the dry weight. Operating and emission standards for disposal by plasma pyrolysis or gasification A. Operating standards All the operators of the plasma pyrolysis or gasification shall meet the following operating and emission standards: 1. Suitably designed air pollution control devices shall be installed or retrofitted with the plasma pyrolysis or gasification to achieve the above emission limits, if necessary. Wastes to be treated using plasma pyrolysis or gasification shall not be chemically treated with any chlorinated disinfectants and chlorinated plastics shall not be treated in the system. Standards for autoclaving of biomedical waste the autoclave should be dedicated for the purposes of disinfecting and treating biomedical waste. When operating a vacuum autoclave, medical waste shall be subjected to a minimum of three pre-vacuum pulse to purge the autoclave of all air. Medical waste shall not be considered as properly treated unless the time, temperature and pressure indicators indicate that the required time, temperature and pressure were reached during the autoclave process. If for any reasons, time temperature or pressure indicator indicates that the required temperature, pressure or residence time was not reached, the entire load of medical waste must be autoclaved again until the proper temperature, pressure and residence time were achieved. Recording of operational parameters: Each autoclave shall have graphic or computer recording devices which will automatically and continuously monitor and record dates, time of day, load identification number and operating parameters throughout the entire length of the autoclave cycle. Validation test for autoclave: the validation test shall use four biological indicator strips, one shall be used as a control and left at room temperature, and three shall be placed in 222 National Guidelines for Infection Prevention and Control in Healthcare Facilities the approximate centre of three containers with the waste. Personal protective equipment (gloves, face mask and coveralls) shall be used when opening containers for the purpose of placing the biological indicators. At least one of the containers with a biological indicator should be placed in the most difficult location for steam to penetrate, generally the bottom centre of the waste pile. The occupier or operator shall conduct this test three consecutive times to define the minimum operating conditions. The temperature, pressure and residence time at which all biological indicator vials or strips for three consecutive tests show complete inactivation of the spores shall define the minimum operating conditions for the autoclave. After determining the minimum temperature, pressure and residence time, the occupier or operator of a common biomedical waste treatment facility shall conduct this test once in three months and records in this regard shall be maintained. Routine test: A chemical indicator strip or tape that changes colour when a certain temperature is reached can be used to verify that a specific temperature has been achieved. It may be necessary to use more than one strip over the waste package at different locations to ensure that the inner content of the package has been adequately autoclaved. The occupier or operator of a common biomedical waste treatment facility shall conduct this test during autoclaving of each batch and records in this regard shall be maintained. Spore testing: the autoclave should completely and consistently kill the approved biological indicator at the maximum design capacity of each autoclave unit. Biological indicator for autoclave shall be Bacillus stearothermophilus spores using vials or spore strips; with at least 1fi106 spores.
Helping navigate the course of the illness anxiety 12 step groups generic 15 mg aripiprazolum free shipping, and thinking through decisions can help those facing such rare illnesses feel much less isolated anxiety kava aripiprazolum 20 mg discount. Parents describe having a greater appreciation for the things they do with their children anxiety buzzfeed discount 10 mg aripiprazolum free shipping, learning how to experience each day to its fullest anxiety 78749 buy generic aripiprazolum 20 mg line. This process can be fnancially depression symptoms eyes purchase aripiprazolum 20 mg visa, emotionally mood disorder group curriculum order aripiprazolum with american express, and physically draining and in some cases, all-consuming. Families can beneft from talking with others who have been in this situation to help mitigate the intense emotions that can occur during this time. If parents create an environment that allows for questions, discussions, and an expression of feelings, children will feel free to ask their parents about their illness and treatment options and become active participants in the disease management. Children often know much more about what is happening than adults might believe. In addition to what they have been told, they pick up information from ambient conversation, have independent interactions with professionals, and surmise things from the emotional climate around them. They will ask questions when they want to know, and will often shy away from questions to which they do not want the answers. Children are good regulators of their own knowledge base, providing cues to the adults around them at all junctures. Children need to be able to confde in their parents and others when they feel limited physically or socially by Fanconi anemia. At each stage of development, children need age-appropriate explanations of their diagnosis and treatment. Information offered regularly to children will enhance their ability to understand their disease and establish trusting relationships. As they get older and medical problems emerge, groundwork set in earlier years will encourage patients to rely on health care providers. Others may have no known problems but, because of illness-related absence, may need extra assistance. School-age children develop increasingly strong relationships with their peers as they begin to differentiate themselves from their families. Each child and family must fnd a balance in social and family relationships, which allows for a blend of independence and dependence, nurturing and differentiation. They may, therefore, come to understand and deal with issues with which adults may not feel comfortable. Thus, they may seem more mature than their chronological ages and often are more sophisticated than their peers in matters of illness and death. They may also appreciate life, and the meaning of life, more than the adults they encounter. For adolescents, challenging the rules is age-appropriate and functional at times for emotional growth. It allows them to assert themselves as individuals and to begin to learn to take responsibility for their actions. Young adults report stopping their medications, sun bathing, drinking alcohol, smoking, etc. Compliance with medication regimens may be of concern and should be given particular attention at this stage, as should the risk-taking behaviors associated with greater chances of malignancy. As children get older, they need to be involved in assenting, consenting, and participating in actual decisions about their medical care. As their children become more active decision-makers, parents may feel some Chapter 16: Psychosocial Issues 299 relief that they are now making decisions with, rather than for, their children. Yet as children approach young adulthood, parents have expressed anxiety about how their children will learn to make complicated, sophisticated decisions for themselves. For some young adults, the decisions will continue to be made in partnership with their parents. This time of growth for the person with Fanconi anemia also becomes a time of growth for parents. Children of all ages need to be allowed to continue to grow, regardless of the status of their medical conditions. Achievements, great or small, cultivate growth and satisfaction for both children and parents. Children need to be prepared to be successful and motivated in life, and not exclusively focused on Fanconi anemia. Siblings Siblings present their own unique concerns, some visible and some invisible. They may feel guilty that the disorder happened to their sibling and not to them or may feel that they are less important because they are not getting as much attention. Siblings care about and 300 Fanconi Anemia: Guidelines for Diagnosis and Management worry about each other a great deal. For many, their universe is defned by their role as either an older or younger brother or sister. Siblings of children with life-threatening or fatal illnesses often have as much of an emotional response to the illness as the affected children. Open communication, the opportunity for expression, and the ability to process the experience help siblings to fnd their place in the world. Siblings need their own time with parents, medical knowledge appropriate to their age, and to truly be and feel that they are an integral part of the family. These relationships have a very powerful presence that may not always be visible in a family. It is important that affected and nonaffected siblings have the opportunity to talk with each other and with their parents. These can be among the strongest relationships in life and need to be cultivated and nurtured during this journey. Young adults who face the most severe manifestations of the illness may, of necessity, Chapter 16: Psychosocial Issues 301 remain more physically and emotionally dependent on family members. On the other hand, their family connections may reach deeper levels than those of their healthy peers. It is important to help such individuals gain their independence while helping them understand that they can still rely on their families for support and assistance. Family members need to work together to understand the best decision-making practices in their families. Fanconi anemia affects the whole family, not just when a child is initially diagnosed, but throughout the course of the illness. Some of the magnitude of the diagnosis is not apparent to the child until he or she reaches adolescence and young adult years. Relationships, 302 Fanconi Anemia: Guidelines for Diagnosis and Management peer pressure, experimentation with drugs and alcohol, and sexual relationships all pose emotional and physical challenges. The issues of whom to tell, when to tell, and what to tell seem to be related to whom to trust and an ongoing evaluation of who needs to know what and why. These issues can frame early stages of relationships with roommates and romantic partners. As relationships fourish, there is a natural inclination to think towards the future. All of this may infuence how they make choices of friends, relationships, careers, marriage, and parenthood. Partners also need an outlet for information, expression, and help at times when their partner is not doing well or has to make major life decisions. Negotiating their roles as partners and with parents who have nurtured their children for decades can be quite challenging. Increasing numbers of children are becoming young adults and adults with Fanconi anemia. In the same way that the needs of the children and then teens became a priority as treatment evolved, now the needs of these adults, physically and emotionally, become the priority. The medical course of Fanconi anemia is evolving, allowing for the emotional and physical sequelae to be better understood. Emotional connections for this group can be found in young adults 304 Fanconi Anemia: Guidelines for Diagnosis and Management and adults with other rare illnesses who have survived to adulthood. The Death of a Child If a patient nears death, the patient and the family need emotional support, clear thinking, concrete assistance, and tremendous understanding. By this point, the family has lived through many struggles with the illness and therefore may continue fghting longer than others might expect. Fighting, trying the next thing, and looking towards experimental options are the armor that families use to cope. Providing information and opportunities for discussion, helping families make decisions, supporting their choices, comforting, remembering, and remaining available are signifcantly helpful to families at this stage. Rarely do bereaved parents feel that their loss is understood and therefore their ability to accept support, except from people in similar situations, may be limited. Chapter 16: Psychosocial Issues 305 Relationships with families should not end abruptly during the bereavement period, because it is a most diffcult phase for them. Assisting families to understand many of the more intense feelings (anger, regret, loneliness, depression) as part of the natural process at this time is helpful. The complication of having a genetic illness, an illness that a family will have to deal with for generations to come, adds to the complexity of coping after a child dies. Enable patients, as they mature, to become responsible and proactive with regard to their medical care (recommended by a focus group of parents). The increasing prevalence of complicated mourning: the onslaught is just the beginning. Or grieving can begin later, when baffing physical symptoms fnally lead to the diagnosis of Fanconi anemia. The grief one experiences often proceeds in predictable stages, as one struggles to cope with this devastating reality. Since this illness often progresses slowly and patients sometimes live for years or decades after diagnosis, the family suffers from chronic grief. With every acute crisis of this illness, loved ones experience again the most painful phases of the grieving process. Experts who study stages of grieving often refer to four phases, which usually proceed in order, but can co-exist in the same time frame. It is also possible to survive one phase only to fnd oneself experiencing feelings or behaviors characteristic of an earlier phase. This phase can last from hours to months and is often intermingled with the second stage of grief. Emotions commonly experienced are crippling sadness, anger, guilt, anxiety, despair, terror, and feeling out of control. When parents have unknowingly passed lethal genes on to their children, feelings of guilt can be quite intense, however irrational. Disorganization the third phase of the grieving process is often referred to as a period of disorganization. The emotions of the second phase continue, but the waves of sadness, anger, anxiety, and other disabling emotions are less intense. Most parents feel that part of their role is to protect their children from dangerous, unhappy experiences. They often feel quite helpless when confronted with the knowledge that they are unable to protect precious children from a life-threatening condition.
References
- David DS, Tegtmeier BR, OíDonnell MR, et al. Visceral varicellazoster after bone marrow transplantation: report of a case series and review of the literature. Am J Gastroenterol. 1998;93:810-813.
- Judge KW, Pawitan Y, Caldwell J, et al: Congestive heart failure symptoms in patients with preserved left ventricular systolic function: Analysis of the CASS registry, J Am Coll Cardiol 18(2):377-382, 1991.
- Lin JT, Wei-Shu W, Yen CC, et al. Stage IV thymic carcinoma: a study of 20 patients. Am J Med Sci 2005;330(4):172-175.
- May P, Stein EJ, Ryter RJ, et al. Cushing syndrome from percutaneous absorption of triamcinolone cream. Arch Intern Med 1976;136:612-3.