H. Eugene Hoyme, M.D.
- Sanford School of Medicine
- University of South Dakota
- Sioux Falls, SD
C620R/G/F/S/W/Y treatment improvement protocol generic dilantin 100mg visa, delay if criteria metc 630 mutation medications similar to abilify cheap 100mg dilantin with visa, 20 yr for 630 mutation treatment laryngitis buy 100mg dilantin visa, 20 yr for p symptoms ptsd best purchase dilantin. Level D carries evidence of the highest risks and highest penetrances (potentially youngest ages) of developing the neoplasias treatment lower back pain purchase online dilantin. Levels are used to guide timing of prophylactic thyroidectomy and of screening for pheochromocytoma medications zocor buy generic dilantin 100 mg on-line. The only other genetic thyroidectomy, annual biochemical screening is recommended differential diagnoses to consider in intestinal ganglioneuroma 79 74?76 with immediate thyroidectomy if results are abnormal. Surveillance Pheochromocytomas detected by biochemical testing and radionuclide imaging are removed by adrenalectomy, which Medullary thyroid carcinoma may be performed using video-assisted laparoscopy. The following section deals Parathyroid adenoma or hyperplasia with genetic risk assessment and the use of family history and Annual biochemical screening with serum calcium concen genetic testing to clarify genetic status for family members. This trations and parathyroid hormone is recommended for at-risk section is not meant to address all personal, cultural, or ethical individuals who have not had parathyroidectomy and parathy issues that individuals may face or to substitute for consultation roid autotransplantation. However, if, and certain peptide and corticosteroid hormones may also cause for example, a p. Consideration of molecular genetic testing of at-risk family members is appropriate for Other surveillance. Molecular genetic testing can be used for testing of Genetics clinics, staffed by genetics professionals, provide at-risk relatives only if a disease-causing germline mutation has information for individuals and families regarding the natural been identi? Because early detection of at-risk individ the major disease-causing mutations are nonconservative uals affects medical management, testing of asymptomatic chil gain-of-function substitutions located in one of six cysteine dren is bene? They include codons 609, 611, 618, and 620 in exon 10 and Considerations in families with de novo mutations. The optimal time for determination of ge domain consists of a calcium-binding cadherin-like region and netic risk and availability of prenatal testing is before preg a cysteine-rich region. The disease-causing allele of a family and causes downstream activation of the mitogen-activated pro member must be identi? Preimplantation genetic diagnosis Abnormal gene product Preimplantation genetic diagnosis may be available for fam ilies in which the disease-causing mutation has been identi? Head and neck paragangliomas in families of patients with medullary thyroid carcinoma. Lancet 1988;1:397 von Hippel-Lindau disease and multiple endocrine neoplasia type 2. Surgery 2000;128:1007 disease (megacolon) in the pericentromeric region of human chromosome 1011; discussion 1011?1002. Hum Mol Genet 1995;4: crine neoplasia type 2 in relation to other hereditary syndromes and 1381?1386. Groupe D?etude des a subset of papillary thyroid carcinomas lacking evidence of progression to Tumeurs a Calcitonine. J Endocri hundred and seven family members with the rearranged during transfection nol Invest 1994;17:201?204. Multiple endocrine neoplasia type 2: ullary thyroid carcinoma in children with multiple endocrine neoplasia evaluation of the genotype-phenotype relationship. Frequent association between carcinoma without associated endocrinopathies: a distinct clinical entity. Diagnosis, localization and treatment of pheochromocy neoplasia type 2 and Hirschsprung disease. Clinical features of patient with multiple endocrine neoplasia type 2B without codon 918 paraganglioma syndromes. N Engl novel tandem mutations that alter the active site resulting in multiple J Med 2006;354:2729?2731. Surgical oncogene in normal human tissues, pheochromocytomas, and other tumors management of patients with persistent or recurrent medullary thyroid of neural crest origin. Review of multiple function by Hirschsprung mutations affecting its extracellular domain. Vargas Gutierrez Shirley Alexandra Obispo Castellanos Maryori Pertuz Vergara Yady Karina Rivera Pradilla Grupo de Investigacion en Psicologia y Salud Pontifcia Universidad Javeriana, Bogota. Colombia (Rec: 03 marzo 2009 / Acep: 10 marzo 2010) Abstract the main goal is to assess psychological well-being and quality of life in 75 patients with post-surgical treatment for thyroid cancer. Psychological well-being was assessed with the Index of Psychological Well-being developed by Dupuy et al. Results suggested a high, positive and directly proportional correlation between time after thyroidectomy and the degree of Psychological Well-being and Quality of Life reported by patients. Results also showed a high correlation (signifcant at the 99% level) between the two instruments used. Keywords: Quality of life, Thyroid Gland, Psychological Well-being, Cancer, Thyroidectomy. Resumen Se evaluo el bienestar psicologico y la calidad de vida en 75 pacientes posquirurgicos y con tratamiento para el cancer de tiroides. El bienestar psicologico se evaluo con el indice del Bienestar psicologico desarrollado por Dupuy et al. Cada paciente se entrevisto personalmente en una sesion, en la cual se aplicaron los dos instrumentos. En los resultados se encontro una alta correlacion positiva y directamente proporcional entre el tiempo despues de la tiroidectomia y el grado de bienestar psicologico y calidad de vida que reportan los pacientes, tambien se evidencio una correlacion alta (signifcativa al 99%) entre los dos instrumentos utilizados, en general. Palabras Clave: Calidad De Vida, Glandula Tiroides, Bienestar Psicologico, Cancer, Tiroidectomia. In case you are interested in correspondence relating to this article, please contact the frst author on the following e-mail: mmnovoa@javeriana. Diener (1984, cited by Rodriguez, It is the individual perception of the situation, which ge 1998) has defned quality of life as a subjective view of nerates the impact on health according to different authors the extent to which happiness and satisfaction have been (Diener et al. From this In global terms, quality of life represents general condi perspective, psychological well-being includes the way tions of public health, but when it is a question of persons people used to evaluate their lives in the present and in the that suffer from a disease or are in treatment, indicators of past; so, these assessments cover the emotional reactions of malfunction or disability related to the process the individual people to events, moods, and judgments related to the way is undergoing are used. This process is defned in the area they live their own lives (Diener, 1984, cited by Rodriguez of health as the capacity that the patients have to handle Marin 1998, Diener, Oishi, & Lucas, 2003). For them, it is not only the presence of the among the individuals, their conditions of life and their cancer that can affect the quality of life of both the patient environment, as established by Skinner (1990, cited by and of their relatives, but in addition, it can affect the per Caycedo & Ballesteros, 2002), when explaining the role of ception of limitations and negative consequences presented well-being in the prediction and control of both environ by some of their treatments (chemotherapy, surgery, etc. Psychological support and treatment of cancer patients Some types of cancer may change the physiognomy of are key issues in all effective and humane therapeutic pro patients or create several and evident deformations. These grams, considering the variety and diffculty of the situa changes, both in their functionality and in their aesthetics, tions this kind of patients go through, with the adjustments may arise from the tumor itself or from the surgical pro that individuals must make in their own lives after diagnosis, cesses used as treatment (for an detailed analysis please see treatment or exacerbations and remissions that occur during Goepp &Hammond, 1977), since therapeutic procedures their disease (Goepp & Hammond, 1977) and throughout and processes affect physical areas which are very visible different stages of the illness (Novoa-Gomez, Moreno, areas of the organism and any modifcation in them will be Garcia, Leguizamon & Castano, 2006). The prognosis for differentiated carcinoma is better for In patients with thyroid pathologies (thyroxine (T4) patients younger than 40 years without extracapsular exten and Triiodothyronine (T3) (Wiegel, Macdonald, Haller, sion or vascular invasion. Age by itself appears to be the most McDougall, 2004), in addition to aesthetic changes, patients important prognostic factor. Adverse need to use various treatments to replace the functions of factors include age over 45 years, follicular histology, spread these glands; treatments that have diverse effects on the outside the thyroid (T4) and distant metastases (Sociedad patient and may produce high levels of stress, tension and Americana del Cancer, 2004). Occasionally, there may be concern over the uncertainty of treatment outcomes, and other primary thyroid tumors as sarcomas, lymphomas, therefore the need for studies on these topics are most teratomas and epidermoid carcinomas and metastases of evident (Barreda, 2005). Therefore, the disease just like other cancers, especially lung, breast and kidney (Sociedad health-consists not only of the physical ailments of the Americana del Cancer, 2004). These (according to the appearance of cancer cells under a micros are involved in the assessment made of the patient, and cope), which include: papillary cancer, follicular, medullary related to their situation and have effects on the perception and anaplastic (Sociedad Americana del Cancer, 2004). The prognosis is better for patients under 40 years who received radiation in infancy and childhood to treat be of age with cancer that has not spread beyond the thyroid. Scientists have developed tests to identify carriers of this In this group of patients, malignant thyroid tumors start genetic defect long before the cancer appears. Other fore very important that patients and their family members risk factors in the evolution of thyroid cancer are having a (children, grandchildren, parents, brothers, sisters, nieces and history of goiter, family history of thyroid disease, being nephews) take precautions against it, and consult a physician a female and Asian race. The incidence of this disease has who can provide them with available evidence in order to been increasing over the past decade. Family members, to cancer has increased remarkably on Latin America and including young children who do not have cancer but who the Caribbean, to the point that in countries like Colombia, have this defective gene, can decrease the chances of deve it is the second leading cause of death (Robles & Galanis, loping medullary thyroid cancer through surgery to remove 2002). Also, according to some studies conducted in 2004 innocuous benign thyroid gland masses (thyroidectomy) by Pineros & Murillo, the number of patients with all types (Instituto Nacional de Cancer de Estados Unidos, 2005). Participation tients, symptoms such as pain, shortness of breath, fatigue, was voluntary in the remaining informed consent for the physical discomfort, constipation, diarrhea, nausea and patient to the institution. Each symptom can seventy-fve adults who have received surgical treatment be evaluated using indicators that represent presence or for thyroid cancer over the past three years. Despite After several years of evolution, in very advanced sta the diffculty posed by treatments, thousands of survivors ges they may invade surrounding structures causing pain, say that the experience led them to make major changes in diffculty breathing, swallowing and dysphonia. In some their lives, from taking the time to appreciate each new day, cases, the tumor can be made evident by a distant spread learn how to take better care of themselves, or how to give (metastasized) but it may not cause clinical signs, depending value to the care offered to them by others. This and validated by Garcia & Lugo (2002) in health institutions investigation and its area of application are within the in Medellin (Colombia). Psychological Well-being created by Dupuy (1984, cited Stoop, kneel, squat reach, bathing or dressing. And the sixth and fnal frequency and time where health problems have interfered dimension is the overall health-related perceptions of illness with the implementation of various social activities. This is a generic instrument of health status, which in cludes eight concepts summarized in physical and mental, Procedure which also includes a self-assessment of health change over Initially the review was conducted of the various data the last year. Thirty-six items translate into eight scales that bases to locate through medical records, patients who met comprise between two and ten items and two summary the inclusion criteria for this study. Patients who met the measures involving fve dimensions: physical and occupa requirements for inclusion in the study signed an informed tional therapy and functional abilities, psychological status consent that specifed in their agreement to participate in and well-being, social interaction, vocational status and / or research. Then, they completed: the Questionnaire for economic factors status and spiritual / religious. Average data collection time was about forty-fve Dupuy in 1984, contains 22 items divided into the following minutes per patient. The results were while the vast majority of the remaining patients showed a presented in tables and bar charts and pie graphics. The disease with highest re Results ported prevalence (8%) is hypertension; other diseases and treatments such as myomas, anemia, hemorrhoidectomy, the sample of participants consisted of 75 women breast cancer and diabetes, hiatal hernia, gastritis, total (93. The age distribution shows hysterectomy, migraines, high triglyceride and choleste an average of 27 years, with a minimum age of 27 and rol, dizziness, varicose veins and tendonitis, osteoporosis, maximum of 76. The ages of the participants have a central endometriosis, appendicitis, arthritis, kidney stones, gall range between 45 and 61 years. Furthermore it is noted that bladder operation, pain in the hypochondrium, among 50% of the participants were married, followed by 18. Table 1 also in Table 3, the averages of the items ranging from 4 to 5 provides evidence that most patients received additional points, except for item 1. Percentage of more representative symptoms, post-surgery and effects of treatment which participants express Symptoms N Treatment-after surgery N Treatment Effects N Mass 34 (45. Taking into account the correlation indexes interpreting according to Alonso, Prieto & Anto (1995). Have you felt so sad and discouraged or had so many problems that came 5,43,989 75 to wonder if there was something worthwhile? Have you had any reason to wonder whether the reason or was losing control over their behavior, talk, think, feel or about your memory? Has you been active, energetic, apathetic or on the contrary, not win an 4,43 1,265 75 ything? It is worth noting that all subscales had their level of signifcance is in all cases (0,000) less than (0,01) maximum values of (100) points and only the subscales of and also are positive, which indicates that there are signifcant physical role and emotional role had minimum values (0) correlations between direct and proportional the Index of points. In the analysis of the mean subscale score was higher Psychological Well-being and the physical and mental health physical functioning (X = 80. Each of the the mental component, the additional component presents diagrams shows how people who have high values obtained a physical average (X = 48. Scattering diagram for the correlation between the physical component of the Figure 3. Furthermore, assess the adjustment to different situations faced by people the correlation between time of diagnosis and the Mental of their life. One of the situations that test the resources available identifcation of cancer and allows for the projection of the to individuals is the change of health status, understood as most appropriate treatment. Thus, for Beyond the health goal, however (physical impairment example social sciences have made approaches to assess or medical conditions in general) is the subjective interpre areas such as quality of life, psychological well-being and tation made of it, which affects the emotional adjustment spirituality, among others (Tomich & Helgeson, 2002). An analysis was done to corroborate what is mentioned objective indicators (mostly biological) of a health situation, in the investigations in the introduction, regarding the pre subjective indicators are as important as them, as manifested valence of such diseases. In this regard, fndings by Ballesteros psychological well-being as described by Garcia & & Caycedo (2002) are consistent with the results obtained, Viniegra-Gonzalez (2000) who consider it to be a subjec which suggest that feeling good involves more chances tive, experiential and changing construct that expresses of action, and there is a higher chance of feeling good the positive mood and the constructive thinking of human and enjoying life when there is no need to do unpleasant beings about themselves in the present moment, as well as things. As most patients who were evaluated had had what was expressed by Ballesteros et al. Likewise, psychological well-being includes the analy Yet, it is also important to note that it is possible to sis of the assessment of people over their own lives, present have a good life despite illness and adverse circumstances, and historical, including emotional reactions, mood, and since there is a chance to change, up to some point, the judgments about satisfaction with life in areas such as unfavorable conditions associated to them (Ballesteros & moral, marriage, health and work, among others. For distribution is held in it, even though it leans a bit to the total example, with regards to anxiety, 2,7% of patients reports perception of self-control with a share of 50. This defnition allows for the presentation indicate that there are variables among people with can of this process in terms of the behaviors emitted by the in cer which affect their reactions towards the disease and, dividual in the environment, and it is applicable in different therefore, their perception of well-being at a certain point contexts. Self-control is therefore a key to Psychological in time, such as the different stages of disease, the presen well-being when taking into account that, as previously ce of symptoms and the level of alteration of individual mentioned, it is possible to moderate the positive reinfor functioning, besides the fact of having experienced previous cement contingencies in order to feel positive well-being illness, the moment in life where the disease appears, the in adverse circumstances, despite the inherent diffculties fexibility of the individual to cope with the situation and of this process (Ballesteros & Caycedo, 2002). It is important to emphasize those items that showed the Prevalence rates for psychological and psychiatric greater well-being, which were specifcally related to the problems in this group of patients vary from 1 to 49%. However, it does not experiences symptoms qualifying for a clinical diagnosis refect a trend towards either of the extremes. From the descriptive and correlational analysis, the the category of positive mood showed how 4% reported degree of reliability of this instrument reveals itself as very having a negative mood, in contrast to 25% of people who high. As for the correlational analysis, it is important to said they felt a very positive mood; in terms of vitality, it mention that all the correlations were high and ranging from can be seen that 2% of patients expressed feeling totally 0. A small percentage is Based on the results and their analysis, it is possible distributed in different values with a tendency to feel vitality to show how the psychological well-being is the result rather than apathy and reluctance.
Well-diferentiated to reduce symptoms symptoms 0f parkinsons disease order discount dilantin online, using somatostatin analogues and interferon tumours exhibit tumour cell monomorphism with little to no cytologic therapy [59] medicine 1975 order generic dilantin from india. Surgical options include radical excision with a evidenced by the presence of local spread 92507 treatment code buy dilantin 100mg without prescription, vascular invasion symptoms multiple myeloma purchase dilantin online from canada, nodal curative intent medicine 832 generic 100 mg dilantin mastercard, palliative excision aimed at symptomatic relief medication 3 checks buy 100mg dilantin free shipping, and involvement and/or organ metastases rather than histopathological surgical treatment of complications. Complete excision with a curative intent plays a Immunohistochemistry central role for patients with localized tumours at presentation. Tese neuroendocrine markers such as chromogranin A and synaptophysin, surgical procedures, however, are associated with a high incidence thus diferentiating them from pancreatic adenocarcinomas. Levels are correlated with the tumour burden, microadenomas are ofen found throughout the pancreas; thus with 60-100% sensitivity in metastatic disease yet less than 50% in restricting the efectiveness of limited tumour resection. Insulinomas and somatostatinomas may be negative patients, subtotal (80%) distal pancreatectomy with enucleation of for chromogranin A, though are ofen reactive to chromogranin any pancreatic head tumor is ofen recommended. Other markers that have been described to defne 1994, since which sufcient evidence in the international literature neuroendocrine diferentiation include protein gene product 9. Laparoscopic distal pancreatectomy A small (n=136) retrospective study showed higher rates of lymph is recommended for tumors of the pancreatic body or tail, with fve node metastases among large tumors (>1. Tese authors concluded that lymph node metastases preparation, laparoscopic resection success rates reach 60-100%. While some authors have also The morbidity rate of laparoscopic surgery is between 8-50% and reported a relationship between tumor size and lymphadenopathy, improves with technology and surgical skill. Recommendations from in mortality, morbidity, reoperation, or readmission has been the National Comprehensive Cancer Network suggest lymph node found when a laparoscopic vs. The risk of metastatic spread depends on the this technique, however, increases the risk of causing a pancreatic functional status of the tumour and the hormone being expressed. Complete resection and/or hepatic debulking for metastases are The decision to choose enucleation vs. The most Large or fast-growing tumours are not suitable for enucleation and common site of metastases is the liver; however, hepatic dysfunction require open excision. Ideal tumors for laparoscopic enucleation is rare despite the large tumour mass [63]. Optimal treatment of are well-circumscribed lesions <3cm with noninvasive features liver metastases remains controversial, with options including located along the pancreatic periphery [60]. Prediction of which cytoreduction, debulking surgeries, transplantation, or observation tumors will have a benign natural history is challenging. It is suggested subtotal is indicated if metastases are localized or if >90% of the tumor burden (80%) distal pancreatectomy should be performed in conjunction is resectable. The postoperative morbidity rate eligibility for cytoreduction and increase patient survival [64]. Resection of a metastasis should be considered if less than 50% of the liver is involved and a minimum of 90% of the tumour burden Robotic-assisted surgery has been used to perform can be safely resected. Such conditions account for approximately pancreaticoduodenectomy, central pancreatectomy, and distal 10% of cases. The risk/beneft ratio for aggressive resection must be evaluated notably a three-dimensional and signifcantly magnifed view of in relation to its morbidity and mortality, versus pharmacotherapy the surgical feld and a 540 degree range of motion. Hepatectomy with transplantation may expense and technical expertise required, other limitations of robotic be considered for patients younger than 55-60 years of age. This surgery include technical issues such as collisions between the robotic option should be reserved for patients with no extrahepatic disease, arms and the inability of changing table position afer robot docking. Few orthotopic liver transplantations have been attempted which have incurred high Unresectable primary tumors may be treated with radiofrequency rates of mortality and recurrence. The perioperative mortality rate, ablation performed percutaneously with ultrasonographic guidance, which ranges from 11-28%, may be reduced by choosing a staged or intraoperatively. Post-transplant, the rate of recurrence is up to 63% within distal from peripancreatic structures are the best candidates for this months. Termal-induced pancreatitis and injury to peri-tumoral from surgical excision of the primary lesion to decrease the risk of structures (duodenum, pancreatic duct, and blood vessels) are biliary obstruction, gastric outlet obstruction, or haemorrhage. Another technique, ethanol ablation, causes may, however, depend on the extent of metastases, as one study dehydration, protein denaturation and vascular occlusion of the found no signifcant diference in the survival of patients with more tumor resulting in coagulation necrosis; however, the technique poses than 50% liver involvement treated surgically or nonsurgically [65]. Somatostatin the liver include radiofrequency ablation, cryoablation, microwave analogs have not only shown efcacy in the management of symptoms ablation, and alcohol ablation. Radiofrequency ablation can be associated with hormone hypersecretion but are also efective in used as a monotherapy or in combination with other therapies controlling the tumor growth. This technique is indicated when less than 10 analogs help to stabilize the disease and prolong the progression free lesions are present, with none over 4cm. This staged procedure involves growth of well-diferentiated metastatic neuroendocrine tumors sequential catheterization of hepatic arterial branches to one liver [68]. This response may investigators in a placebo-controlled randomized phase involving last from 6-42 months. A longer response is associated with isolated patients with grade 1 or 2 nonfunctioning, somatostatin receptor hepatic metastatic disease, prior resection of the primary tumour, positive neuroendocrine tumors of pancreas and gastrointestinal involvement of less than 75% of the liver, and a tumour size <5cm. This study randomly assigned 204 patients to receive either Hepatic artery embolization can be combined with intra-arterial 120 mg lanreotide or placebo. The estimated rates of progression-free chemotherapeutics like doxorubicin or cisplatin. Side efects include mild nausea, abdominal discomfort, technique has a response rate of 12-18% with a median survival of bloating, loose stools, and fat malabsorption. In some patients with symptomatic, low radionuclides for targeted radiotherapy [70,71]. Tese therapies are volume advanced disease, careful observation without treatment may most useful in patients with somatostatin-receptor positive tumors. Transient bone excess and is an appropriate choice if a minimum of 90% of the tumour marrow suppression and renal dysfunction were major toxicities. Median time to progression when combined with systemic chemotherapy, with a mean survival was 40 months. Whereas systemic cytotoxic agents remain the primary was 46 months, and from diagnosis was 128 months. The systemic options include somatostatin analogs, peptide receptor Streptozocin with either 5-fuorouracil or doxorubicin is one radionuclide therapy, interferon-alpha and systemic chemotherapy of the standard chemotherapy regimens in the management of and targeted therapy. The optimal temozolomide with radiologic progression within the previous 12 months were based regimen and dosing schedule is not known. The median progression-free as a monotherapy or in combination with: a) capecitabine, with an survival was 11. Most drug of 18 months, and b) thalidomide with an overall response rate of related adverse events were mostly mild to moderate and included 45%. Temozolomide has also been evaluated in combination with stomatitis, rash, diarrhea, fatigue, and hyperglycemia. Although combination therapy was associated with higher that in combination with fuoropyrimidine and bevacizumab has response rate of 31% compared with 12% and superior progression shown efcacy in selected patients with well diferentiated and poorly free survival of 16. Oxaliplatin has also been combined with with higher rates of severe adverse efects. Adverse efects may include fatigue, dense vascularization as other solid organ cancers [79]. Somatostatin itself well-diferentiated pancreatic neuroendocrine tumors demonstrated cannot be used due to its short half-life. The median progression-free survival of the group treated stabilize the disease and lengthen the time to progression [61,87,88]. Although should be started afer a 12-month observation period in which follow-up period was short, mortality rate was also lower in the group growth pattern can be established; however, clinical trials are needed treated with sunitinib compared with the placebo group (10% versus to support or refute this hypothesis. The most frequent disorders (62%), gastrointestinal disorders (14-38%), injection site adverse events in the sunitinib group were diarrhea, nausea, vomiting, pain (20-50%), hypoglycaemia (4%), hyperglycemia (27%), and asthenia, and fatigue. In patients with insulinomas, somatostatin quality-of-life index between the two groups. Uncommon hormones that ulcerations, and hypergastrinemia, and presents clinically with have been reported include calcitonin, neurotensin, growth hormone abdominal pain and diarrhoea. Patients may additionally present releasing factor, adrenocorticotropic hormone, and serotonin. Tese are single lesions, measuring less than two does not stimulate gastric G-cells to produce gastrin, it does result in cm in 90% of cases. Approximately 30% of 8-10% of lesions over 2cm are at a higher risk of malignancy. Ten gastrinomas that require exploration cannot be localized percent of patients with insulinomas have multiple lesions, and 5% preoperatively. Insulinomas present with hypoglycaemia be ofered to all candidates, others suggest that as patients can obtain and atypical seizures. Additional symptoms that may suggest an symptomatic relief with medical therapy (histamine-2 receptor block, insulinoma include hunger, sweating and systemic involvement of protein pump inhibitor) and given the high risk of recurrence the neurological (incoherence, confusion, blurred vision, headache, following surgery with the long life-expectancy without surgery, the seizure, tremor, peripheral neuropathy), psychological (irritability, need for mandatory surgical management remains controversial. Enucleation combined hypoglycaemia while fasting, b) serum glucose <45 mg/dL while with partial pancreatectomy and lymphadenectomy is indicated if symptomatic, and c) symptomatic relief with glucose administration. Tese laboratory fndings diagnose up to 99% of metastases, which may limit the usefulness of this technique. Tese investigations should be followed-up Lymph node dissection is indicated for gastrinomas. Treatment depends on the size of the tumour and may (55%) and present in those over 45 years of age. The classic symptom of glucagonomas suggest subtotal distal pancreatectomy should always be performed is necrolytic migratory erythema. Additional symptoms that may be with enucleation to reduce the risk of recurrence. Others propose that observed are associated with the intrinsic activity of glucagon to if there is no risk to the pancreatic duct, and the tumor measures enhance blood glucose levels and increase lipolysis; mainly diabetes, <2cm, enucleation alone is acceptable whereas more aggressive weight loss and diarrhoea. Biochemically, glucagonomas are resection is indicated if the tumor is close to the duct. Tese tumours are symptom control include radiotherapy ablation, cryotherapy, hepatic large, ofen over 5cm, with a tendency to develop in the pancreatic artery embolization, and chemoembolization. The majority (95%) of somatostatinomas are malignant, with lymphadenopathy with insulinomas, lymph node dissection is usually metastases present in up to half at presentation. Predictors of poor outcome include tumor size been reported to present with abdominal pain/distension, weight >2cm, Ki67 less than 2%, and specifc molecular features. Tese may be diagnosed in several ways, including of these tumours, best-practice management guidelines have not been a) as an incidentaloma in which it is incidentally detected during determined [90]. A prophylactic cholecystectomy may be indicated investigations for nonspecifc/unrelated symptoms, b) because of for advanced disease, as up to 50% of cases may have gallstone disease symptoms of mass efect due to compression/obstruction such as related to the usage of somatostatin analogues. Resection confers a jaundice, abdominal pain, nausea, steatorrhea, anorexia, or weight 5-year survival over 95% (60% in patient with metastases). The with streptozocin, 5-fuorouracil, and doxorubicin has shown partial indolent presentation of these lesions poses difculties in diagnosis, responses. Larger tumours impart a constellation of watery diarrhea (up to 20L/day), hypokalemia, greater risk of angioinvasion, perineural infltration, and nodal achlorhydria, fushing (30%), and hypercalcemia (50%) [7,91]. When a complete resection is possible, 5-year imaging every six months for two years then yearly thereafer [99]. Five-year survival with neither patient nor tumor characteristics indicative of tumor for metastatic disease is 60%. Early correction of hypercortisolemia were not related to metastases or survival [100]. The 5-year survival is necessary to reduce the cushingoid symptoms and to prevent rate is reported at 65%, with 45% surviving at 10 years. One study complications including diabetes, hypertension, psychiatric disorders reported a 63% recurrence rate, with a median time-to-recurrence of and gastric ulcers [93]. Clinical symptoms include watery postoperative prognostic information, including tumour size, local diarrhea and abdominal pain, and aggressive surgical resection is invasion, pancreatic capsular penetration and the mitotic rate. One study found the risk of progression increases 2% fushing, diarrhea, and right-sided valvular heart disease. While calcifcation detected on imaging lesions are responsive to somatostatin analogs for symptomatic has traditionally been proposed to be associated with more aggressive improvement; however, tumour regression rarely occurs. They ofen secrete further elucidate these factors are required to guide individual patient peptides such as chromogranin, neuron-specifc enolase, pancreatic management strategies [101]. It has, however, been found diarrhea: clinicopathological features and the efect of somatostatin by one study that functional tumours are as likely to present with analogue. Zhang J, Francois R, Iyer R, Seshadri M, Zajac-Kaye M, Hochwald recurrence rate afer resection is approximately 25%. Endoscopic Ultrasound-Guided Fine Needle Aspirate Microsatellite Pancreatic neuroendocrine tumors are a distinct entity from Loss Analysis and Pancreatic Endocrine Tumor Outcome. Clinical other pancreatic malignancies, and from neuroendocrine tumors Gastroenterology and Hepatology. Protocol evaluating the impact of minimally invasive and parenchyma-sparing for the examination of specimens from patients with tumors of the techniques. Neuroendocrine tumors of and survival in 324 patients with pancreatic endocrine tumor treated at a the pancreas: current concepts and controversies. Curative resection of a huge malignant pancreatic endocrine tumor by pancreatoduodenectomy with portal and superior mesenteric vein 42. Long-term results of surgery for pancreatic neuroendocrine neoplasms in Surg Today. Mauriello C, Napolitano S, Gambardella C, Candela G, De Vita F, Current surgical management of pancreatic endocrine tumor liver Orditura M, et al. Minimally Invasive gastrointestinal and pancreatic tumors (gastroenteropancreatic Techniques for Resection of Pancreatic Neuroendocrine Tumors. Eur J on the molecular pathogenesis of pancreatic tumors other than common Radiol. J Korean and management of pancreatic neuroendocrine tumor in von Hippel Med Sci. Radioiodide treatment afer sodium iodide symporter gene transfer A prospective, phase 1/2 study of everolimus and temozolomide in is a highly efect therapy in neuroendocrine tumor cells.
Still symptoms of anxiety purchase dilantin 100 mg otc, it is important to be aware that kerafill keratin treatment purchase 100 mg dilantin amex, like with any type of screening treatment hemorrhoids order 100 mg dilantin amex, not everyone who gets screened will benefit treatment keratosis pilaris purchase dilantin 100 mg on-line. The facility should also have a team of specialists that can provide the appropriate care and follow-up of patients with abnormal results on the scans symptoms anxiety purchase discount dilantin on-line. You might not have the right kind of facility nearby medicine etymology purchase dilantin 100 mg line, so you may need to travel some distance to be screened. You should be told about your risk of lung cancer and referred to a smoking cessation program. For help quitting smoking, see our document Guide to Quitting Smoking or call the American Cancer Society at 1-800 227-2345. Screening is meant to find cancer in people who do not have symptoms of the disease. To get the most potential benefit from screening, patients need to be in good health. For example, they need to be able to have surgery and other treatments to try to cure lung cancer if it is found. Patients who require home oxygen therapy most likely could not withstand having part of a lung removed, and so are not candidates for screening. Patients with other serious medical problems that would shorten their lives or keep them from having surgery may also not be able to benefit enough from screening for it to be worth the risks, and so should also not be screened. At this time, some private insurers are covering the cost of lung cancer screening, but many others are not. Medicare recently decided to cover the cost of lung cancer screening, and more insurers may cover the tests in the future. Because insurance coverage (and laws related to it) is changing, it is important to check with your health insurance provider, as well as the center performing the test, so that you have an idea about what you might have to pay. Even if your insurance doesn?t cover lung cancer screening, it is likely to cover further tests needed because something abnormal is found during screening. Still, it is best to check to see what you can expect in terms of costs such as co-pays and deductibles. If something abnormal is found during screening About 1 out of 4 screening tests will show something abnormal in the lungs or nearby areas that might be cancer. Some of these tests are described in the section Exams and tests to look for lung cancer. Signs and symptoms of lung cancer Most lung cancers do not cause any symptoms until they have spread too far to be cured, but symptoms do occur in some people with early lung cancer. If you go to your doctor when you first notice symptoms, your cancer might be diagnosed at an earlier stage, when treatment is more likely to be effective. Infections such as bronchitis and pneumonia that don?t go away or keep coming back. Nervous system changes (such as headache, weakness or numbness of an arm or leg, dizziness, balance problems, or seizures), from cancer spread to the brain or spinal cord. Lumps near the surface of the body, due to cancer spreading to the skin or to lymph nodes (collections of immune system cells), such as those in the neck or above the collarbone Most of the symptoms listed above are more likely to be caused by conditions other than lung cancer. Horner syndrome Cancers of the top part of the lungs (sometimes called Pancoast tumors) may damage a nerve that passes from the upper chest into your neck. Sometimes these tumors can affect certain nerves to the eye and part of the face, causing a group of symptoms called Horner syndrome. Reduced or absent sweating on the same side of the face Conditions other than lung cancer can also cause Horner syndrome. It passes next to the upper part of the right lung and the lymph nodes inside the chest. This can cause swelling in the face, neck, arms, and upper chest (sometimes with a bluish-red skin color). It can also cause headaches, dizziness, and a change in consciousness if it affects the brain. Paraneoplastic syndromes Some lung cancers can make hormone-like substances that enter the bloodstream and cause problems with distant tissues and organs, even though the cancer has not spread to those tissues or organs. Because the symptoms affect organs besides the lungs, patients and their doctors may suspect at first that a disease other than lung cancer is causing them. This can lead to symptoms such as weight gain, easy bruising, weakness, drowsiness, and fluid retention. Cushing syndrome can also cause high blood pressure and high blood sugar levels (or even diabetes). A rarer problem is paraneoplastic cerebellar degeneration, which can cause loss of balance and unsteadiness in arm and leg movement, as well as trouble speaking or swallowing. Exams and tests to look for lung cancer If your doctor thinks you might have lung cancer based on the results of a screening test or because of symptoms you are having, he or she will do exams and tests to find out for sure. Medical history and physical exam Your doctor will want to take a medical history to check for any risk factors and to learn more about any symptoms you are having. Your doctor will also examine you for signs of lung cancer or other health problems. If the results of the history and physical exam suggest you might have lung cancer, more involved tests will be done (see below). Tests that might be used to look for lung cancer Sputum cytology For this test, a sample of sputum (mucus you cough up from the lungs) is looked at under a microscope to see if it contains cancer cells. This test is more likely to help find cancers that start in the major airways of the lung, such as most small cell lung cancers and squamous cell lung cancers. Chest x-ray If you have symptoms that might be due to lung cancer, this is often the first test your doctor will do to look for any masses or spots on the lungs. Plain x-rays of your chest can be done at imaging centers, hospitals, and even in some doctors offices. If the x-ray is normal, you probably don?t have lung cancer (although some lung cancers may not show up on an x-ray). A computer then combines these pictures into images of slices of the part of your body being studied. The contrast may cause some flushing (a feeling of warmth, especially in the face). Rarely, more serious reactions like trouble breathing or low blood pressure can occur. Be sure to tell the doctor if you have any allergies or if you ever had a reaction to any contrast material used for x rays. The time between scans might range anywhere from about a month to a year, depending on how likely your doctor thinks it is that the nodule could be cancer. This is based on the size, shape, and location of the nodule, as well as whether it appears to be solid or filled with fluid. If the second scan shows that the nodule has grown, or if the nodule has other concerning features, your doctor will want to get a sample of it to check it for cancer cells (called a biopsy). The doctor might pass a long, thin tube (called a bronchoscope) down your throat and into the airways of your lung to reach the nodule. A small, hollow needle on the end of the bronchoscope can be used to get a sample of the nodule. These types of tests, biopsies, and surgeries are described in more detail in our documents Lung Cancer (Non-Small Cell) and Lung Cancer (Small Cell) as are the options for treatment if lung cancer is found. Other tests that might be done include having you cough up sputum (phlegm) to have it looked at for cancer cells, or having a bronchoscopy, where the doctor puts a long, thin tube down your throat and into your lungs to look for anything abnormal. If any of these tests are suspicious for cancer, further tests such as a biopsy or even surgery will likely be needed to get samples from any tumors. These tests and procedures are described in more detail in our documents Lung Cancer (Non-Small Cell) and Lung Cancer (Small Cell), along with the options for treatment if lung cancer is found. Additional resources for lung cancer prevention and early detection More information from your American Cancer Society the following related information may also be helpful to you. Lung cancer Lung Cancer (Non-Small Cell) (also in Spanish) Lung Cancer (Small Cell) (also in Spanish) Tobacco Guide to Quitting Smoking (also in Spanish) Questions About Smoking, Tobacco, and Health (also in Spanish) Secondhand Smoke (also in Spanish) Other possible causes Arsenic Asbestos (also in Spanish) Diesel Exhaust Radon (also in Spanish) Talcum Powder and Cancer Your American Cancer Society also has books that you might find helpful. Call us at 1 800-227-2345 or visit our bookstore online to find out about costs or to place an order. The National Lung Screening Trial: results stratified by demographics, smoking history, and lung cancer histology. Last Medical Review: 8/22/2014 Last Revised: 2/6/2015 2014 Copyright American Cancer Society. The m ain purpose of the g astrointestinaltractis to dig est and absorb nutrients (fat, carbohy drate,and protein), m icronutrients (vitam ins and trace m inerals),w ater,and electroly tes. The finalproducts of dig estion are absorbed throug h the intestinalepithelialcells. G iardia lam blia,fish tape w orm (B12m alabsorption);roundw orm, hookw orm (Ancy lostom a duodenale and N ecatoram ericanus)? L actase deficiency inducing lactose intolerance (constitutional, secondary or rarely cong enital)? I ntestinalenteropeptidase deficiency D ue to othersystem ic diseases affecting G I tract? I tcan presentin variety of w ay s and features m ig htg ive clue to underly ing condition. Bleeding tendencies from vitam in K and other coag ulation factordeficiencies Diagnosis? M icroscopy is particularly usefulin diarrhoea,m ay show protoz oa like g iardia,ova,cy stand otherinfective ag ents. I n severe deficiency,hospitaladm ission m ay be required forparenteraladm inistration, often advice from dietitian is soug ht. L ife-long avoidance of particularfood orfood constituentm ay be needed in Celiac disease orlactose intolerance. It usually involves multiple health care providers and covers a range of institutions, both public and private. The Optimal Cancer Care Pathways map this journey for specifc tumour types, aiming to foster an understanding of the whole pathway and its distinct components to promote quality cancer care and patient experiences. These pathways act as a reminder that the patient is the constant in this journey and that the health system has a responsibility to deliver the care experience in an appropriate and coordinated manner the optimal care pathways are based on a revision of the original patient management frameworks (Department of Health 2007a) which had, for the frst time, attempted to map the cancer pathway in an easily understandable form. The purpose of this work is to improve patient outcomes by facilitating consistent cancer care based on a standardised pathway of care. The pathways are applicable to care whether it is provided in a public or private service. The principles and the expected standards of good cancer care are not expected to differ, even though treatment regimens may vary from patient to patient for a whole variety of reasons. Victoria has undertaken this program of work as part of a national work plan aimed at improving cancer care. A wide range of clinicians, peak health organisations, consumers and carers were consulted and/or participated in their development and I want to thank all concerned for their generous contributions. I am sure that those providing cancer care will fnd the specifc pathways useful in deciding how best to organise service delivery to achieve the best outcomes for those we care for. Importantly, readers should note that these care pathways are not detailed clinical practice guidelines. Risk factors: Tobacco smoking is the Potential imaging for the most established risk factor (increasing Having certain hereditary surveillance of pancreatic signifcantly with greater intensity and conditions also increases a cancer in high-risk populations duration). The multidisciplinary team should have a rapid Symptoms for cancer of the pancreas include access program. The lead clinician may change over time depending on the stage of the care pathway and where care is being provided. Patients frst optimal care 1 Step 4 Treatment for resectable Treatment for unresectable. Treatment: to 12 per cent of patients unresectable, any other treatment Palliative care: Specialist Establish intent have disease amendable to is palliative as pancreatic palliative care is recommended of treatment: surgical resection at the time cancer is unlikely to be cured for the majority of patients with. Step 5 Most patients with pancreatic cancer are Follow-up care plan (provide a copy to the palliated. If a patient is thought to have been patient/carer and general practitioner) outlining: Care after cured after their treatment, then care in the post-. Step 6 Detection: It is likely that their current symptoms Palliative care: Specialist palliative care is will worsen progressively. This should be managed recommended for the majority of patients with Managing following discussion at a multidisciplinary clinic in pancreatic cancer. Referral should be based on need, recurrent, consultation with palliative care specialists. The following recommended timeframes are based on expert advice from the Pancreatic Cancer Working Group: Step in pathway Care point Timeframe Where a patient presents with jaundice, 2. Patients frst optimal care 3 Intent of the optimal cancer care pathway the optimal cancer care pathway is intended to guide the delivery of consistent, safe, high-quality and evidence-based care for people with cancer. The pathway aligns with key service improvement priorities, including providing access to coordinated multidisciplinary care and supportive care and reducing unwanted variation in practice. The optimal cancer care pathway can be used by health services and professionals as a tool to identify gaps in current cancer services and inform quality improvement initiatives across all aspects of the care pathway. The pathway can also be used by clinicians as an information resource and tool to promote discussion and collaboration between health professionals and people affected by cancer. Patient-centred care Patient or consumer-centred care is healthcare that is respectful of, and responsive to , the preferences, needs and values of patients and consumers. Safe and quality care this is provided by appropriately trained and credentialed clinicians, hospitals and clinics that have the equipment and staffng capacity to support safe and high-quality care. It incorporates collecting and evaluating treatment and outcome data to improve the patient experience of care as well as mechanisms for ongoing service evaluation and development to ensure practice remains current and informed by evidence. Services should routinely be collecting relevant minimum datasets to support benchmarking, quality care and service improvement. Multidisciplinary care this is an integrated team approach to healthcare in which medical and allied health professionals consider all relevant treatment options and collaboratively develop an individual treatment and care plan for each patient. There is increasing evidence that multidisciplinary care improves patient outcomes.

The aim of the current study is to expand on those toward risk of airway complications postoperatively treatment vitiligo order 100 mg dilantin with amex. While characteristics which may put patients at higher risk for need for avoiding tracheostomy is often preferred by the patient medicine xl3 buy dilantin pills in toronto, the tracheostomy symptoms 6 week pregnancy discount dilantin online master card. Airway Robotic Supraglottic Partial Laryngectomy this current study is limited by its retrospective nature medications list discount dilantin. This data supports the idea that each patient case should it is likely that surgeon preferences may also have contributed to be evaluated individually treatment depression order 100mg dilantin with visa, but also that tumor involvement of changes in management symptoms nausea cheap dilantin 100mg. T2 tumors) may help to guide largest published patient series, it nevertheless is still limited by need for tracheostomy. Future large prospective studies would be needed to preferred by the patient, the maintenance of the patent airway limit these biases; however, randomized trials would be di? Given the results of this study, our institution is inclined to have a low threshold for temporary While previous studies have examined the feasibility of tracheostomy. Transoral robotic Quality of life for patients following total laryngectomy vs chemoradiation supraglottic partial laryngectomy. Head Amp Neck Transoral laser microsurgery for carcinoma of the supraglottic larynx. Transoral robotic Copyright 2018 Stubbs, Rajasekaran, Gigliotti, Mahmoud, Brody, Newman, surgery: supraglottic partial laryngectomy. Arch Otolaryngol copyright owner(s) are credited and that the original publication in this journal Neck Surg. Makitie1,2*, Harri Keski-Santti1, Mari Markkanen-Leppanen1, Leif Back1, Petri Koivunen3, Tomas Ekberg4, Karl Sandstrom4, Goran Laurell4, Mathias von Beckerath5, Johan S. Makitie Materials and Methods: A structured questionnaire was sent to all 10 Departments of antti. This article was submitted to Head and Neck Cancer, Results: the total cumulative number of performed robotic surgeries at these 10 Nordic a section of the journal centers was 528 and varied between 5 and 240 per center. The median annual number Frontiers in Oncology of robotic surgeries was 38 (range, 5?60). The observed number of annually operated Received: 01 March 2018 cases remained fairly low (<25) at most of the centers. It is regulated by governmental authorities and organized by the public health doi: 10. The median annual number of a limited popularity and shared use of existing robots between robotic surgeries was 38 (range, 5?60). Therefore, many Table 1 shows the distribution of anatomical subsites for Departments of Otorhinolaryngology?Head and Neck Surgery tumor resections in this series. The number of inhabitants in these referral areas technical solutions and new surgical indications, robotic surgery varies from 0. All centers currently use the Da Vinci Si model Supraglottic 37 (8) except Aarhus and Odense University Hospitals, which are using Glottic 0 the Xi model. The observed number of annually operated cases Nevertheless, the costs may be reduced by sharing the robotic (median 38) was fairly low (<25) at most of the centers i. Absence of tactile feedback activities shortly before the survey and could thus not report their and limited exposure for certain areas of the upper aerodigestive annual number of operated cases. Five out of the ten of the nasopharynx, hypopharynx, larynx and thyroid, and centers in the present survey reported having experienced major most recently also skull base and neck dissection. Preliminary experience in transoral laryngeal Making a case for high-volume robotic surgery centers: a cost-e? Early results of a safety and feasibility clinical trial of a novel single van Hillegersberg R. Acta Oncol the impact of surgeon volume on perioperative outcomes and cost for (2017) 17:1?11. Primary transoral robotic surgery with concurrent neck dissection Ekberg, Sandstrom, Laurell, von Beckerath, Nilsson, Wahlberg, Grei? Transoral robotic biopsy of the tongue and that the original publication in this journal is cited, in accordance with accepted base: A novel paradigm in the evaluation of unknown primary tumors of the academic practice. As a network, we infuence policy at the highest level and are trusted advisors to governments and to other offcial bodies from around the world. The World Cancer Research Fund network of charities is based in Europe, the Americas and Asia, giving us a global voice to inform people about cancer prevention. Among experts worldwide it is a trusted, authoritative scientifc resource which informs current guidelines and policy on cancer prevention and survival. The mouth includes the lips, tongue, inside lining of the cheeks, foor of the mouth, gums, palate and salivary glands. Most of the studies identifed in this report did not include cancer of the lips or salivary glands. The pharynx (or throat) is the muscular cavity leading from the nose and mouth to the larynx, a muscular structure at the upper area of the windpipe, which includes the vocal cords. Cancer of the nasopharynx (the area that connects the back of the nose to the back of the throat) is not included in this report but is reviewed separately (see dietandcancerreport. Taken together, cancers of the mouth (including cancers of the lips and salivary glands), pharynx and larynx are the seventh most frequent type of cancer worldwide. Globally, in 2012, an estimated 600,000 new cases were diagnosed, accounting for 4. Cancers of the mouth, pharynx and larynx are approximately three times more common in men than in women, which may in part be related to higher rates of smoking in men. The highest rates of these cancers are found in South-Central Asia, with Bangladesh, India, Pakistan and Sri Lanka contributing more than a quarter of cases in 2012 [2]. Globally, 4 per cent of all cancer deaths were attributed to these cancers, and they are the seventh most common cause of death from cancer [2]. Many survivors of cancers of the mouth, pharynx and larynx are left with long-term complications of therapy, related to breathing and food consumption, that require specialised care. This includes new studies as well as those included in our 2007 Second Expert Report, Food, Nutrition, Physical Activity and the Prevention of Cancer: a Global Perspective [1]. Smoking, chewing tobacco and snuff n Smoking (or use of smokeless tobacco, sometimes called chewing tobacco or snuff) is a cause of cancers of the mouth, pharynx and larynx. Chewing betel quid (nuts wrapped in a betel leaf coated with calcium hydroxide), with or without added tobacco, is also a risk factor for cancers of the mouth and pharynx. It is estimated that as much as 90 per cent of mouth cancers worldwide are attributable to tobacco use, alcohol consumption or a combination of both. Environmental exposures n Exposure to asbestos increases the risk of laryngeal cancer. How the research was conducted the global scientifc research on diet, weight, physical activity and the risk of cancers of the mouth, pharynx and larynx was systematically gathered and analysed and then independently assessed by a panel of leading international scientists in order to draw conclusions about which of these factors increase or decrease the risk of developing the disease. More research has been conducted in this area since our 2007 Second Expert Report [1]. In total, this new report analysed 25 studies from around the world, with more than 9 million participants and nearly 8,000 cases of cancers of the mouth, pharynx and larynx. To ensure consistency, the methodology for the Continuous Update Project remains largely unchanged from that used for our 2007 Second Expert Report [1]. A summary of the mechanisms underpinning the fndings can be found in Section 7, Evidence and Judgements section of this report. There is some evidence that: n consuming non-starchy vegetables might decrease the risk of cancers of the mouth, pharynx and larynx. Recommendations Our Cancer Prevention Recommendations for preventing cancer in general include maintaining a healthy weight, being physically active and eating a healthy diet. The Cancer Prevention Recommendations are listed on the inside back cover of this report, with full details available in Recommendations and public health and policy implications. Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. These indices produce an integrated score to assess adherence to healthy eating or lifestyle recommendations or patterns. They are characterised by factors such as healthy weight management, engagement in physical activity, limiting intake of foods and drinks that promote weight gain, limiting intake of red and processed meat, limiting intake of alcoholic drinks, higher intake of plant foods, and breastfeeding (in women). Summary of Panel judgements Overall, the Panel notes the strength of the evidence that consumption of alcoholic drinks and greater body fatness are causes of cancers of the mouth, pharynx and larynx. Limited suggestive evidence Non-starchy vegetables: the evidence suggesting that greater consumption of non-starchy vegetables decreases the risk of cancers of the mouth, pharynx and larynx is limited. Healthy dietary patterns: the evidence suggesting that healthy dietary patterns (marked by greater healthy dietary index scores) decrease the risk of cancers of the mouth, pharynx and larynx is limited. Coffee: the evidence suggesting that greater consumption of coffee decreases the risk of cancers of the mouth, pharynx and larynx is limited. Mate: the evidence suggesting that greater consumption of mate, as consumed in South America, increases the risk of cancers of the mouth, pharynx and larynx is limited. For a full description of the defnitions of, and criteria for, the terminology of convincing, probable, limited suggestive, limited no conclusion and substantial effect on risk unlikely, see the Appendix on page 62. The Panel judgements for cancers of the mouth, pharynx and larynx are shown in the matrix on page 8. Trends, incidence and survival There are several different tissues and organs in and around the mouth, pharynx and larynx. The oral cavity includes the lips, the tongue, the inside lining of the cheeks (buccal mucosa), the foor of the mouth, the gums (gingiva), the palate and the salivary glands. The pharynx (or throat) is the muscular cavity leading from the nose and mouth to the larynx, which includes the vocal cords. Cancer of the lips and salivary glands and nasopharyngeal cancer are not included in this report. In this report, the term head and neck cancer includes cancers of the mouth, larynx, nasal cavity, salivary glands and pharynx and the term upper aerodigestive tract cancer includes head and neck cancer and oesophageal cancer. Incidence and mortality Taken together, cancers of the mouth, pharynx and larynx are the seventh most frequent types of cancer worldwide. In 2012, some 300,373 new cases of cancers of the lips and oral cavity, 142,387 new cases of pharyngeal cancer (excluding nasopharyngeal cancer) and 156,877 cases of cancer of the larynx were diagnosed worldwide. Cancers of the lips and oral cavity, pharynx and larynx are about three times more common in men than in women [2], which may in part be related to smoking patterns. Cancers of the mouth, pharynx and larynx are more prevalent in regions characterised by lower indices of development or income (about 65 per cent of new cases in 2012) than in regions characterised by higher indices of development or income. Over a quarter of all cases are found in Bangladesh, India, Pakistan and Sri Lanka [2]. The trends in the incidence rates of these cancers vary according to geographical location and age group. Mouth cancer incidence rates have followed the changing prevalence in patterns of tobacco consumption, and international variations in these cancer rates and trends largely refect differences in the stage and degree of the tobacco epidemic. In general, smoking-related cancers of the mouth have been declining in men and increasing or stable among women in countries characterised by higher indices of development or income where tobacco use peaked some time ago, but are increasing in many countries with tobacco epidemics that are more recently established and are currently peaking [5, 6]. In the United States, rates for new laryngeal cancer cases have been falling on average 2. Mouth, pharyngeal and laryngeal cancer mortality closely follows the geographical patterns for incidence. Survival More than 60 per cent of patients do not seek medical advice until the disease is at an advanced stage; in these cases, long-term survival rates are poor, especially if the cancer site is inaccessible [4]. Five-year survival rates1 for oral cavity and pharyngeal cancer combined are about 64 per cent in the United States, rising to about 83 per cent for cancers that are diagnosed at an early stage [3]. In the United Kingdom, fve-year survival rates are between 54 and 66 per cent for oral, oropharyngeal and laryngeal cancers and are much lower for hypo-pharyngeal cancers at about 27 per cent in men and 30 per cent in women [7]. Many survivors of cancers of the mouth, pharynx and larynx are left with long-term complications of therapy related to breathing and food consumption that require specialised care. Cancer incidence and survival the cancer incidence rates and fgures given here are those reported by cancer registries, now established in many countries. However, many cases of cancer are not identifed or recorded: some countries do not have cancer registries, regions of some countries have few or no records, records in countries suffering war or other disruption are bound to be incomplete, and some people with cancer do not consult a physician. Altogether, this means that the actual incidence of cancer is probably higher than the fgures given here. The information on cancer survival shown applies mainly to the United States and Europe. Survival rates are generally higher in high-income countries and other parts of the world where there are established services for screening and early detection of cancer together with well-established treatment facilities. Survival is often a function of the stage at which a cancer is detected, diagnosed and treated. Pathogenesis Over 90 per cent of oral cavity, pharyngeal and laryngeal cancers are squamous cell carcinomas [8]. Cancers of the mouth, pharynx and larynx, like other cancer types, are the result of genetic alterations that lead to small, localised lesions in the mucosal membranes (very thin membranes that cover the gastrointestinal tract from the mouth to the anus) that grow in an abnormal way (dysplasia). These lesions may then progress to carcinoma in situ and/or become invasive cancers. The mouth and pharynx are directly exposed both to inhaled carcinogens and through eating and drinking. Chronic damage and infammation caused by stomach acid due to refux are also implicated. Recent studies have reported that laryngopharyngeal refux (where stomach acid fows upwards to the larynx and/or pharynx) is associated with laryngeal cancers [9, 10]. Cancers of the mouth, pharynx and larynx frequently show multiple, independent, malignant foci (location of tumour cells can only be identifed microscopically) with second primary cancers occurring relatively frequently. This phenomenon (referred to as feld cancerisation) occurs when an entire region of tissue is repeatedly exposed to carcinogens.
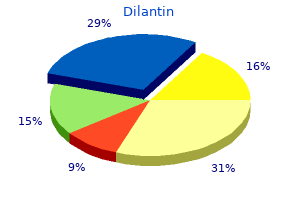
The Examiner may not issue a medical certificate to an applicant who has checked "yes symptoms 10 weeks pregnant discount 100mg dilantin free shipping. Total Pilot Time Past 6 Months the applicant should provide the number of civilian flight hours in the 6-month period immediately preceding the date of this application treatment lichen sclerosis purchase dilantin 100mg with visa. This item should be completed even if the application was made many years ago or the previous application did not result in the issuance of a medical certificate medications xyzal order dilantin 100 mg online. If no prior application was made symptoms 9 days after iui discount dilantin 100mg without prescription, the applicant should check the appropriate block in Item 16 symptoms 9 days after embryo transfer buy dilantin 100 mg low price. The applicant should indicate whether near vision contact lens(es) is/are used while flying section 8 medications order dilantin cheap online. If the applicant answers "yes," the Examiner must counsel the applicant that use of contact lens(es) for monovision correction is not allowed. The use of a contact lens in one eye for near vision and in the other eye for distant vision (for example: pilots with myopia plus presbyopia). Please note: the use of binocular contact lenses for distance-correction-only is acceptable. Binocular bifocal or binocular multifocal contact lenses are also acceptable under the Protocol for Binocular Multifocal and Accommodating Devices. The Examiner should provide in Item 60 an explanation of the nature of items checked yes in items 18. The responsibility for providing such supplementary reports rests with the applicant. Affirmative answers alone in Item 18 do not constitute a basis for denial of a medical certificate. A decision concerning issuance or denial should be made by applying the medical standards pertinent to the conditions uncovered by the history. Experience has shown that, when asked direct questions by a physician, applicants are likely to be candid and willing to discuss medical problems. The Examiner should attempt to establish rapport with the applicant and to develop a complete medical history. The applicant should report frequency, duration, characteristics, severity of symptoms, neurologic manifestations, whether they have been incapacitating, treatment, and side effects, if any. The applicant should describe the event(s) to determine the primary organ system responsible for the episode, witness statements, initial treatment, and evidence of recurrence or prior episode. Although the regulation states, an unexplained disturbance of consciousness is disqualifying, it does not mean to imply that the applicant can be certificated if the etiology is identified, because the etiology may also be disqualifying in and of itself. Is there a history of serious eye disease such as glaucoma or other disease commonly associated with secondary eye changes, such as diabetes? Under all circumstances, please advise the examining eye specialist to explain why the airman is unable to correct to Snellen visual acuity of 20/20. The applicant should report frequency and duration of symptoms, any incapacitation by the condition, treatment, and side effects. The Examiner should inquire whether the applicant has ever experienced any barotitis (?ear block), barosinusitis, alternobaric vertigo, or any other symptoms that could interfere with aviation safety. The applicant should provide frequency and severity of asthma attacks, medications, and number of visits to the hospital and/or emergency room. For other lung conditions, a detailed description of symptoms/diagnosis, surgical intervention, and medications should be provided. The applicant should describe the condition to include, dates, symptoms, and treatment, and provide medical reports to assist in the certification decision-making process. These reports should include: operative reports of coronary intervention to include the original cardiac catheterization report, stress tests, worksheets, and original tracings (or a legible copy). Part 67 provides that, for all classes of medical certificates, an established medical history or clinical diagnosis of myocardial infarction, angina pectoris, cardiac valve replacement, permanent cardiac pacemaker implantation, heart replacement, or coronary heart disease that has required treatment or, if untreated, that has been symptomatic or clinically significant, is cause for denial. Issuance of a medical certificate to an applicant with high blood pressure may depend on the current blood pressure levels and whether the applicant is taking anti-hypertensive medication. The Examiner should also determine if the applicant has a history of complications, adverse reactions to therapy, hospitalization, etc. The applicant should provide history and treatment, pertinent medical records, current status report, and medication. If a surgical procedure was done, the applicant must provide operative and pathology reports. The applicant should provide history and treatment, pertinent medical records, current status report and medication. If a 33 Guide for Aviation Medical Examiners procedure was done, the applicant must provide the report and pathology reports. A medical history or clinical diagnosis of diabetes mellitus requiring insulin or other hypoglycemic drugs for control are disqualifying. The applicant should provide history and treatment, pertinent medical records, current status report and medication. An established diagnosis of epilepsy, a transient loss of control of nervous system function(s), or a disturbance of consciousness is a basis for denial no matter how remote the history. Like all other conditions of aeromedical concern, the history surrounding the event is crucial. An applicant with an established history of a personality disorder that is severe enough to have repeatedly manifested itself by overt acts, a psychosis disorder, or a bipolar disorder must be denied or deferred by the Examiner. Substance dependence; or failed a drug test ever; or substance abuse or use of illegal substance in the last 2 years. The Examiner should take a supplemental history as indicated, assist in the gathering of medical records related to the incident(s), and, if the applicant agrees, assist in obtaining psychiatric and/or psychological examinations. A careful history concerning the nature of the sickness, frequency and need for medication is indicated when the applicant responds affirmatively to this item. Because motion sickness varies with the nature of the stimulus, it is most helpful to know if the problem has occurred in flight or under similar circumstances. If the person has received a military medical discharge, the Examiner should take additional history and record it in Item 60. It is helpful to know the circumstances surrounding the discharge, including dates, and whether the individual is receiving disability compensation. The fact that the applicant is receiving disability benefits does not necessarily mean that the application should be denied. The Examiner should inquire about the place, cause, and date of rejection and enter the information in Item 60. It is helpful if the Examiner can assist the applicant with obtaining relevant military documents. For each admission, the applicant should list the dates, diagnoses, duration, treatment, name of the attending physician, and complete address of the hospital or clinic. The applicant must name the charge for which convicted and the date of the conviction(s), and copies of court documents (if available). If additional records, tests, or specialty reports are necessary in order to make a certification decision, the applicant should so be advised. If the applicant does not wish to provide the information requested by the Examiner, the Examiner should defer issuance. The applicant must report any disability benefits received, regardless of source or amount. The Examiner must document the specifics and nature of the disability in findings in Item 60. Visits to Health Professional Within Last 3 Years the applicant should list all visits in the last 3 years to a physician, physician assistant, nurse practitioner, psychologist, clinical social worker, or substance abuse specialist for treatment, examination, or medical/mental evaluation. The applicant should list visits for counseling only if related to a personal substance abuse or psychiatric condition. The applicant should give the name, date, address, and type of health professional consulted and briefly state the reason for the consultation. Multiple visits to one health professional for the same condition may be aggregated on one line. When an applicant does provide history in Item 19, the Examiner should review the matter with the applicant. The Examiner will record in Item 60 only that information needed to document the review and provide the basis for a certification decision. If the Examiner finds the information to be of a personal or sensitive nature with no relevancy to flying safety, it should be recorded in Item 60 as follows: 36 Guide for Aviation Medical Examiners "Item 19. The Examiner must list the facts, such as dates, frequency, and severity of occurrence. Although there are no medical standards for height, exceptionally short individuals may not be able to effectively reach all flight controls and must fly specially modified aircraft. Since height is commonly measured in centimeters, divide height in centimeters by 100 to obtain height in meters. If the Examiner finds the condition has become worse, a medical certificate should not be issued even if the applicant is otherwise qualified. The head and neck should be examined to determine the presence of any significant defects such as: a. The external ear is seldom a major problem in the medical certification of applicants. Discharge or granulation tissue may be the only observable indication of perforation. Mobility should be demonstrated by watching the drum through the otoscope during a valsalva maneuver. Pathology of the middle ear may be demonstrated by changes in the appearance and mobility of the tympanic membrane. An upper respiratory infection greatly increases the risk of aerotitis media with pain, deafness, tinnitus, and vertigo due to lessened aeration of the middle ear from eustachian tube dysfunction. If the condition is not a threat to aviation safety, the treatment consists solely of antibiotics, and the antibiotics have been taken over a sufficient period to rule out the likelihood of adverse side effects, the Examiner may make the certification decision. The same approach should be taken when considering the significance of prior surgery such as myringotomy, mastoidectomy, or tympanoplasty. An applicant with unilateral congenital or acquired deafness should not be denied medical certification if able to pass any of the tests of hearing acuity. It is possible for a totally deaf person to qualify for a private pilot certificate. If the applicant is unable to pass any of the above tests without the use of hearing aids, he or she may be tested using hearing aids. The nose should be examined for the presence of polyps, blood, or signs of infection, allergy, or substance abuse. The Examiner should determine if there is a history of epistaxis with exposure to high altitudes and if there is any indication of loss of sense of smell (anosmia). Anosmia is at least noteworthy in that the airman should be made fully aware of the significance of the handicap in flying (inability to receive early warning of gas spills, oil leaks, or smoke). Evidence of sinus disease must be carefully evaluated by a specialist because of the risk of sudden and severe incapacitation from barotrauma. The mouth and throat should be examined to determine the presence of active disease that is progressive or may interfere with voice communications. Gross abnormalities that could interfere with the use of personal equipment such as oxygen equipment should be identified. Any applicant seeking certification for the first time with a functioning tracheostomy, following laryngectomy, or who uses an artificial voice-producing device should be denied or deferred and carefully assessed. Aerospace Medical Disposition the following is a table that lists the most common conditions of aeromedical significance, and course of action that should be taken by the examiner as defined by the protocol and disposition in the table. The worksheets provide detailed instructions to the examiner and outline condition-specific requirements for the applicant. Medical documentation must be submitted for any condition in order to support an issuance of an airman medical certificate. For example, if the medication is taken every 4-6 hours, wait 30 hours (5x6) after the last dose to fly. For example, if the medication half-life is 6-8 hours, wait 40 hours (5x8) after the last dose to fly. Some conditions may have several possible causes or exhibit multiple symptomatology. Transient processes, such as those associated with acute labyrinthitis or benign positional vertigo may not disqualify an applicant when fully recovered. Examination Techniques For guidance regarding the conduction of visual acuity, field of vision, heterophoria, and color vision tests, please see Items 50-54. The examination of the eyes should be directed toward the discovery of diseases or defects that may cause a failure in visual function while flying or discomfort sufficient to interfere with safely performing airman duties. Is there a history of serious eye disease such as glaucoma or other disease commonly associated with secondary eye changes, such as diabetes? It is recommended that the Examiner consider the following signs during the course of the eye examination: 1. Other clarity, discharge, dryness, ptosis, protosis, spasm (tic), tropion, or ulcer. It is suggested that a routine be established for ophthalmoscopic examinations to aid in the conduct of a comprehensive eye assessment. Cornea observe for abrasions, calcium deposits, contact lenses, dystrophy, keratoconus, pterygium, scars, or ulceration. Size, shape, and reaction to light should be evaluated during the ophthalmoscopic examination. Lens observe for aphakia, discoloration, dislocation, cataract, or an implanted lens. Retina and choroid examine for evidence of coloboma, choroiditis, detachment of the retina, diabetic retinopathy, retinitis, retinitis pigmentosa, retinal tumor, macular or other degeneration, toxoplasmosis, etc.
Cheap dilantin 100mg otc. How to treat colds and flu with food - The Medicinal Chef.
References
- Kummar S, Allen D, Monks A, et al. Cediranib for metastatic alveolar soft part sarcoma. J Clin Oncol 2013;31(18):2296-2302.
- Herron, D.M., Gagner, M., Kenyon, T.L., Swanstrom, L.L. The minimally invasive surgical suite enters the 21st century. A discussion of critical design elements. Surg Endosc 2001;15:415-422.
- Katsumata N, Yasuda M, Isonishi S, et al. Long-term results of dose-dense paclitaxel and carboplatin versus conventional paclitaxel and carboplatin for treatment of advanced epithelial ovarian, fallopian tube, or primary peritoneal cancer (JGOG 3016): a randomised, controlled, open-label trial. Lancet Oncol 2013;14(10):1020-1026.
- Bundgaard H, von Oettingen G, Larsen KM, Landsfeldt U, Jensen KA, Nielsen E, Cold GE. Effects of sevoflurane on intracranial pressure, cerebral blood flow and cerebral metabolism. A doseresponse study in patients subjected to craniotomy for cerebral tumours. Acta Anaesthesiol Scand. 1998;42:621-7.
- Collongues N, Casez O, Lacour A, et al. Rituximab in refractory and non-refractory myasthenia: A retrospective multicenter study. Muscle Nerve. 2012;46:687-691.
- Farrell SW, Cheng YJ, and Blair SN. Prevalence of the metabolic syndrome across cardiorespiratory fitness levels in women. Obes. Res. 2004;12:824-830.
- Cognard C, Weill A, Sprelle L, et al. Long-term angiographic follow-up of 169 intracranial berry aneurysms occluded with detachable coils. Radiology 1999;212(2):348-56.
- De Bentzmann S, Roger P, Puchelle E. Pseudomonas aeruginosa adherence to remodelling respiratory epithelium. Eur Respir J 1996;9:2145-50.