Mohan S. Gundeti, MB, MS, DNBE, MCh (Urol), FEBU, FICS, FRCS (Urol), FEAPU
- Assistant Professor of Urology in Surgery and Pediatrics,
- The University of Chicago and Pritzker School of Medicine
- Director, Pediatric Urology, and Chief Pediatric Urologist,
- Comer Children? Hospital, the University of Chicago
- Medical Center, Chicago, Illinois
A separate newborn nursery is available for infants who require closer observation or whose mothers cannot care for them antiviral medication for genital warts albendazole 400 mg on-line. Because relatively few staff members are needed to provide care in the newborn nursery and bulky equipment is not needed hiv infection more condition symptoms order generic albendazole line, 24 net ft2 (2 hiv infection from blood transfusion generic 400mg albendazole with visa. Bassinets should be at least 3 ft (approximately 1 m) apart in all directions kleenex anti viral box tucher test buy albendazole mastercard, measured from the edge of one bassinet to the edge of the neighboring bassinet anti viral cleanse and regimen buy albendazole without prescription. During decreased patient occupancy antiviral garlic purchase albendazole in india, central nurseries use nursing staff inefficiently. If circumcisions are performed in the nurs ery, an appropriate table with adequate lighting is required. A special care unit also may be used for convalescing neo nates who have returned to specialty facilities from an intensive care unit in an outside facility or have been transferred from a higher level of care within the institution. The neonatal special care area is optimally close to the delivery area, cesarean delivery room, and the intensive care area (if there is one in the same facility) and away from general hospital traffic. It should have radiant heaters or incubators for maintaining body temperature, as well as infusion pumps, cardiopulmonary monitors, and oximeters. In facilities where the special care unit is the highest level of neonatal care, equipment should be available to provide continuous positive airway pressure and, in some units, equipment may be available to provide short-term (less than 24 hours) assisted ventilation. Aisles should be at least 4 ft wide to accommodate passage of personnel and equipment. In multipatient rooms, each room should accommodate some mul tiple of three to four newborn stations because one registered neonatal nurse is required for every three to four neonates who require intermediate care. Constant nursing and continuous cardiopul monary and other support for severely ill newborns should be provided in the intensive care unit. Because emergency care is provided in this area, laboratory and radiologic services should be readily available 24 hours per day. The results of blood gas analyses should be available shortly after sample collection. In many centers, a laboratory adjacent to the intensive care unit provides this service. In addition, the amount and complexity of equipment required also are considerably greater. Like those in the intermediate care area, all electrical outlets for each Inpatient Perinatal Care ServicesCare of the Newborn 5151 patient station should be connected to both regular and auxiliary power. Continuous, online monitoring of oxygen concentrations, body temperature, heart rate, respiration, oxygen saturation, and blood pressure measurements should be available for each patient. Specific poli cies should address preparatory cleaning, physical preparation of the unit, pres ence of other newborns and staff, venting of volatile anesthetics, and quality assessment. This area should be equipped with a hands-free handwashing station, counter workspace, and storage areas for sup plies, formula, and both refrigerated and frozen human milk. Separate storage areas should be available for foodstuffs, medications, 52 Guidelines for Perinatal Care and clean supplies. Clean utility rooms should not have direct lighting because some of the formulas, medications, and supplies may be light sensitive. The maintenance of soiled utility rooms should conform to the guidelines and state regulations of the Facility Guidelines Institute. The newborn nursery requires secondary storage of items such as linen and formula. In the resuscitation and stabilization area, the admission and observation area, the intermediate care area, and the intensive-care areas, there should be space for secondary storage of syringes, needles, intravenous infusion sets, and sterile trays needed in procedures, such as umbilical vessel catheterization, lumbar punc ture, and thoracostomy. This largely has eliminated the need for a separate treatment room for procedures, such as lum bar punctures, intravenous infusions, venipuncture, and minor surgical pro cedures. The facilities, outlets, equipment, and supplies in the treatment area should be similar to those of the resuscitation area. Inpatient Perinatal Care ServicesCare of the Newborn 5353 Scrub Areas At the entrance to each neonatal care area, there should be a scrub area that can accommodate all personnel and families entering the area. The scrub areas also should contain racks, hooks, or lockers for storing clothing and personal items, as well as cabinets for clean gowns, a receptacle for used gowns, and a large wall clock with a sweep second hand, or digital clock, to time handwashing. Scrub sinks should have hands-free faucets and should be large enough to control splashing and to prevent retained water. These hands-free sinks should be provided at a minimum ratio of one for at least every eight patient stations in the newborn nursery. In addition, one scrub sink is needed in the resuscitation and stabilization area, and one is needed for every three to four patient stations in the admission and observa tion area. Alcohol-based hand hygiene solutions should be available at all entry points and at each bed space. Primary care provid ers also may perform medical record and clerical activities in this area. Maintaining medical records should be considered an unclean procedure, and personnel who have been working on medical records should perform hand hygiene before they have further contact with a neonate. General Considerations Disaster Preparedness and Evacuation Plan An overall disaster preparedness plan is essential for all areas of the hospital and all personnel. A plan addressing natural and terrorist disasters should be in place for each perinatal care area (ie, antepartum care, labor and delivery care, postpartum care, routine neonatal care, intermediate care, and intensive care). A floor plan that indicates designated evacuation routes should be posted in a conspicuous place in each unit. Safety and Environmental Control Because of the complexities of environmental control and monitoring, a hospital environmental engineer must ensure that all electrical, lighting, air composition, and temperature systems function properly and safely. The ventilation pattern should inhibit particulate matter from moving freely in the space, and intake and exhaust vents should be placed so as to minimize drafts on or near the patient beds. Filters should be located outside the infant care area so that they can be changed easily and safely. Care should be taken to ensure that only the patient and the area of interest being examined is in the primary beam and staff needed to assist in patient positioning should wear appropriate shielding. Both natural and artificial light sources should have controls that allow immediate darkening of any bed position sufficient for transillumination or ultrasonography when necessary. Artificial light sources should have a color rendering index of no less than 80, and a full-spectrum color index of no less than 55. Light should be highly framed so that new borns at adjacent bed stations will not experience any increase in illumination. Properly designed natural light is the most desirable illumination for nearly all nursing tasks, including updating medical records and evaluating newborn skin tone. At least one source of natural light should be visible from each patient care area. All external windows should be equipped with shading devices that are easily controlled to allow flexibility at various times of day. These shading devices should be either contained within the window or eas ily cleanable. Windows in neonatal care areas should have opaque shades that make it possible to darken the area to reduce inappropriate radiant heat gain or loss, or for procedures that require reduced light, such as transillumination or ultrasonography examination. Wall Surfaces Wall surfaces should be easily cleanable, provide protection at point of contact with moveable equipment, and be free of substances known to be teratogenic, mutagenic, carcinogenic, or otherwise harmful to human health. An alarm system that warns of Inpatient Perinatal Care ServicesCare of the Newborn 5757 any critical reduction in line pressure should be installed. The ventilation system, monitors, incubators, suction pumps, mechanical ventilators, and staff produce considerable noise, and the noise level should be monitored intermittently. Mechanical systems and equipment in infant rooms and adult sleep rooms should conform to noise criteria 25. Staff members should take particular care to avoid noise pollution in enclosed patient spaces (eg, incubators). Electrical Outlets and Electrical Equipment All electrical outlets should be attached to a common ground. Current leakage allowances, preventive maintenance standards, and equipment quality should meet the standards developed by the Joint Commission. Personnel should be thoroughly and repeatedly instructed on the potential electrical hazards within the neonatal care areas. Nonphysician clinicians in the neonatal intensive care unit: Inpatient Perinatal Care ServicesCare of the Newborn 5959 meeting the needs of our smallest patients. Obstetric and neonatal services share many of the characteristics of high reliability organizations in other industries, such as the aviation industry and nuclear power plants. Individuals must feel comfortable drawing attention to potential hazards or actual failures with out fear of censure from management and peers. Quality improvement accepts that good care depends upon more than just the judgment of the individual. Larger departments may benefit from designation of a patient safety officer and qual Quality Improvement and Patient SafetyCare of the Newborn 6363 ity reporting directly to the department chair. Peer Review Peer review is a quality assessment process in which a retrospective analysis of cases is undertaken using outcomes data to assess adherence to guidelines or other standards of care. Therefore, it may be helpful to develop a relationship with another hospital or outside independent reviewer or consultant to conduct peer review. Care has been monitored and improved by focusing on specific outcomes, such as maternal, newborn, and neonatal mortality. Significant progress has been made in methods for collecting data and gathering vital statistics (eg, prenatal records, linked birth and death certificate data, linked birth and hospital dis charge data). It is recommended that all states follow the most current National Center for Health Statistics requirements for issuing standard certificates and reports for birth, death, and fetal death. For example, rates of unintended pregnancy; use of prena tal care services; and fetal, neonatal, and maternal mortality are possible mea sures of access and outcome at different points along the continuum of perinatal health care delivery. Maternal length of stay in excess of 1 day greater than the local standard after vaginal or cesarean delivery 9. Unplanned postpartum return to the delivery room or operating room for management 12. Delivery of an infant at less than 32 weeks of gestation in an institution without a neonatal intensive care unit 3. Transfer of a neonate to a neonatal intensive care unit *To be defined by each institution Modified from American College of Obstetricians and Gynecologists. Thorough and systematic collection of data on long-term outcomes is essential to evaluate changes in perinatal care delivery systems as well as new technologies and therapies. They review de-identified information from individual cases of fetal and infant death to identify factors associated with those deaths, determine if they represent service system problems that require change, develop recommendations for change, and assist in the implementation of change. The lessons learned from reviews of these deaths need to be shared with those who have the opportunity to influence policies and practices related to the systems of care in place for women in the preconception, antepartum, and postpartum periods. Patient safety is an explicit principle that must be embraced as a core value in patient care. Patient-centered care, open communication, and teamwork provide the foun dation for optimal patient care and safety. National Patient Safety Goals the Joint Commission recognizes the importance of patient safety. Each year, existing goals are modified based on public comment and the experience of reviewers and new goals are added. In this way, over time, the Joint Commission will develop a compendium of recommended practices that will improve patient safety. To improve patient care and reduce medical errors, they encourage all health care providers to promote the follow ing four principles in all practice settings, which are discussed in the following paragraphs: 1. Patient safety focuses on systems of 68 Guidelines for Perinatal Care care, not individuals. A culture of patient safety fosters open communication and welcomes input from team members at every level. Care must be taken to ensure that hierarchical systems do not hamper free com munication among physicians. It requires specific effort to ensure that issues are understood and that meaningful information is trans ferred. Safe Medication Practices Medication errors are one of the most common types of preventable adverse events.
If you will be parenting with a partner hiv infection life expectancy cheap albendazole 400mg free shipping, preconception is a great time for long talks about parenting hiv yeast infection cost of albendazole. Stress can depress your immune system hiv infection immediate symptoms buy albendazole 400mg low cost, raise your blood pressure antiviral botanicals buy 400mg albendazole fast delivery, and alter your hormonal function hiv infection flu symptoms buy 400 mg albendazole visa. Participating in counseling hiv infection symptoms within 24 hours proven 400 mg albendazole, work shops, or support groups, as well as journaling and reading self-help books are ways to explore and process emotional issues, and learn new coping skills before your baby is born. Do things that help you feel good: exercise, sleep well, eat well, and spend time with friends. The stronger your relationship is before your baby is born, the more easily it will weather the challenges of parenting. If you become pregnant after that period, you will not be able to get insurance for that year! Pregnancy, Childbirth, and the Newborn Preconception Wellness Improving your physical health will improve your chances of conceiving and having a good start to your pregnancy. Plan on 1/2 ounce a day per pound that you weigh (for example, a 150-pound woman should drink 75 ounces of fuids). For more nutritional recommendations, see chapter 6 (Eating Well) of Pregnancy, Childbirth, and the Newborn and the Nutrients, Vitamins, and Minerals: Daily Recommendations chart in the Eating Well section of. The father-to-be (and his sperm) can also beneft from a healthy diet and perhaps a multivitamin. Zinc, essential fatty acids, and vitamins C and E may be especially helpful in the preconception period. While your ovaries might produce and release eggs, the lining of your uterus might not be adequate for a healthy pregnancy. If you are severely underweight, you might not be menstruating, and might be infertile. Additionally, beginning pregnancy underweight can increase your chances of preterm birth. If the father-to-be is underweight or has lost signifcant body weight recently, he may have decreased sperm count or function. Do what you can to reach a healthy weight, and main tain that weight prior to becoming pregnant. If, despite your best eforts, you are overweight when pregnancy begins, monitor weight gain during pregnancy. Moderate exercise (two to six hours per week) can enhance fertility by regulating hormones, improving circulation to the ovaries and uterus (or to the testes for the father-to-be). Extreme exercise (such as running 100 miles in a week) can decrease fertility through impaired ovulation for women and reduced sperm count for men. Treat any existing gum disease, as it can increase the risk of miscarriage and premature birth. Your physician should also address any medical conditions and medications that could complicate conception, pregnancy, or birth. For chronic conditions (such as hypertension, diabetes and epilepsy), try to optimize control of the condition and medication levels before pregnancy. Genetic carrier screening is not necessary for many people, but may be recommended to you if you or your partner are concerned about inherited diseases in your family, belong to certain ethnic groups that have a higher risk of certain genetic diseases, have had multiple miscarriages, have a child with an inherited disorder, or are over age thirty-fve. They include sickle cell anemia, beta thalassemia, Tay-Sachs disease, and cystic fbrosis. The tests may indicate that you are a carrier of a disease: you have no symptoms but carry the gene that could pass the disease on. However, if both parents are carriers, your child will have a one in four chance of having the disease. Pregnancy, Childbirth, and the Newborn Preconception Hazards Reduce or eliminate use of harmful substances. Both you and the father-to-be should reduce your use of cafeine, alcohol, tobacco, and illegal substances four months before you plan to conceive. Cafeine: Consuming cafeine in amounts up to 200 to 300 milligrams per day (one or two cups of cofee, three cups of tea or 72 ounces of soda) is generally considered safe for preconception and pregnancy by most authorities. However, there are studies that indicate even one cup of regular cofee per day can decrease chances of conceiving and increase the chance of miscarriage. Alcohol: Drinking as little as fve drinks a week can signifcantly reduce fertility. Alcohol use in pregnancy increases the changes of miscarriage, developmental delays, and growth retardation. Smoking and secondhand smoke: If you and/or your partner smoke, your fertility can be signifcantly impaired. If you consume only a small amount of a substance, the potential side efects are small, so reduce your use as much as possible. For more on harmful substances and resources to help you quit using them, visit. Both you and the father-to-be should reduce your exposure to the following environmental hazards, which are linked to infertility, miscarriage, or birth defects. Wash your hands often and use gloves and other uni versal precautions to protect yourself from bacterial and viral infections. Once an egg is released (ovulation), it is viable for twelve to twenty-four hours. Tus, timing intercourse in the three days prior to ovulation signifcantly increases your chance of conceiving. If you have been following the recommendations above, and it is taking longer to conceive than you had hoped, you may try these options. Planning Ahead: Maternity Care Choices Your choice of caregiver for your prenatal care and to attend your birth, as well as your choice of birthplace, have a huge infuence on your birth experience and your level of satisfaction with your birth. For a caregiver, you may choose a midwife, a family practice doctor, or an obstetrician. For a birthplace, your options include home birth, free-standing birth centers, and hospitals. American Society for Reproductive Medicine, Age and Fertility: A Guide for Patients (Birmingham: American Society for Reproductive Medicine, 2012). American Society for Reproductive Medicine (see note 8 above); Eric Manheimer et al. Write those dates here, so you remember that your baby might be born anytime between and. Ten, write in more notes in the days after the birth, while your memories are still fresh. Deciding to go to the hospital or birth center, or calling the midwife to come How did you know it was time Many expectant families just choose the hospital closest to their home or the one with the best marketing department and the most appealing ads. News & World Report ranks the top ffty neonatal intensive care units health. Of the score, 83 percent comes very specifc criteria, such as nurse stafng, ability to prevent infection, babies who received breastmilk, and number of patients served. The other 17 percent is based on a survey of physicians asking their opinion about the reputation of the hospital. Ratings compare hospitals based on how clearly staf communicated with patients, whether patients received help as soon as they wanted, whether staf explained medicines to the patient before giving it, whether the room was regularly cleaned, and so on. Routine care l Special care l Circumcision l Will they cover lactation consultants to help with breastfeeding ClickedLink=252&ck=10145&area=27 Timing: Although you can do this at any time during pregnancy, we recommend that you plan to visit or call birthplaces in your frst or second trimester. Typically, caregivers have privileges only at certain facilities, so choosing a caregiver and birthplace goes hand in hand. If you have already chosen your caregiver, you can ask them these questions about the birthplace. Birthplace: Who can be with me: Who can be with me during labor and birth You can ask her the questions on the Questions to Ask about Birthplaces list above and those on the Questions for Potential Caregivers list. Also ask these questions: If health issues arise in my pregnancy, would you send me to a physician for consultation or recommend that I transfer my care Tese questions may also aid you in your choice if you need to switch care providers in later pregnancy.
Purchase albendazole online. Income generation for women Living with HIV/AIDS in Tunis.
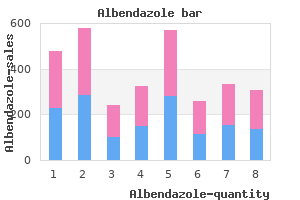
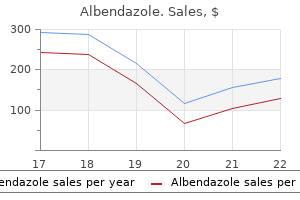
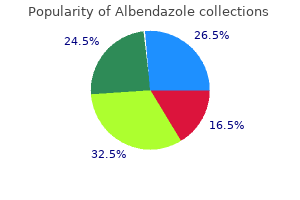
Of these acute hiv infection symptoms duration order albendazole, four approaches (femoral artery highest hiv infection rates world purchase albendazole 400mg otc, subclavian artery antiviral used for rsv order 400mg albendazole with amex, axillary artery new antiviral drugs buy albendazole 400mg fast delivery, and ascending aorta) are considered to be retrograde approaches because the catheter is directed through a vessel against the direction of blood flow hiv infection effects buy generic albendazole canada. The femoral vein approach hiv infection after single exposure proven albendazole 400 mg, by contrast, is considered to be an antegrade (or anterograde) approach because the catheter is directed to the heart through the venous system, in the direction of blood flow. What are the different types of heart valves in use and in development (including tissue, mechanical, and percutaneous valves) What are the theoretical advantages and disadvantages of different valves for different patient populations From a systematic literature scan of studies on different types of tissue and mechanical valves, describe the types of comparative studies, including basic study design, size of study, length of followup, and outcomes assessed. This literature scan will provide data to determine if a systematic review of this literature is possible and needed, and to provide needed context for understanding the evaluation and development of percutaneous heart valves. From a systematic literature scan of studies on different types of percutaneous heart valves, provide a synthesis of the following variables: a. What are the variables associated with surgery or setting that may impact outcomes for percutaneous heart valves Sources of Information and Review Methods the sources of information consulted and review methods used by the Duke team varied considerably by key question. Question 2 and Questions 3-4 required separate literature reviews using distinct sources, search strategies, and review methods. Because of this variability, we describe the methods used for each key question separately. Heart Valves in Use and Development We used four approaches to identify heart valves now in use or in development. First, we identified valves described in the published literature abstracted in answer to Question 2 (conventional valves) and Questions 3 and 4 (percutaneous valves). Next, we generated a list of valve manufacturers based on the published literature and expert knowledge. Finally, we supplemented these approaches by searching the Web sites of valve manufacturers. To determine the theoretical advantages and disadvantages of different valves for different populations, we relied on discussions and recommendations in clinical guidelines, review articles, and consultations with experts. Using these sources, we developed a narrative description of the valve classes, goals in valve design, and the theoretical advantages and disadvantages of different types of valves. For Question 2, we scanned the existing literature comparing different types of conventional. We sought to describe the available comparative studies in terms of the number of available studies, interventions compared, basic study design, size of study, length of followup, and outcomes assessed. We identified potentially important observational studies primarily by reviewing the individual studies included in the systematic reviews that met our full-text inclusion criteria. Articles were included if they concerned conventional heart valves and appeared to be a review article. Citations included at the title-and-abstract stage were reviewed in full-text form independently by two researchers. Articles meeting the following criteria were included for data abstraction: the article was a systematic review, defined as a review including both a Methods section describing a search strategy and analytic approach, and abstractions of primary literature; and the review directly compared two or more different types of conventional heart valves; and the review concerned valve replacement (rather than repair); and the review focused on adults (all patients 18 years of age or, if mixed population, then either 80 percent adults or results reported separately for adults); and the review was published in English in the year 2000 or later. The inclusion criteria applied at both screening stages were: Comparison of two or more heart valves for valve replacement (rather than repair); and Randomized allocation to treatment; and Study conducted in adults (all patients 18 years of age or, if mixed population, then either 80 percent adults or results reported separately for adults); and Study published in English. If there was any uncertainty about whether an article should be included, a second investigator was consulted. A second investigator was consulted in cases where there was uncertainty about whether an article should be included. For Question 2, we completed detailed evidence tables only for the included systematic reviews (Appendix B, Evidence Table 1). Data abstracted included the number and designs of included studies, patient descriptors, heart valves compared, and outcomes reported. The methodological quality of the included systematic reviews was evaluated independently by two investigators using a quality assessment tool developed specifically for this project. When the two investigators disagreed in their assessments, they met to reconcile the difference. The results of quality assessments for individual systematic reviews are reported in Evidence Table 1 (Appendix B). We scanned the existing published and gray literature on different types of percutaneous heart valves to synthesize information on the variables specified in Question 3. We also conducted an extensive search of the gray literature for this question (last search date December 31, 2008). We were assisted in this effort by a librarian with expertise in gray literature searching, who suggested sources and search terms. The gray literature sources consulted, search terms used, and results are described in Table 1. A single reviewer screened the titles and abstracts of all citations for potential inclusion. All citations that appeared to report primary data on studies of percutaneous heart valves in humans were included at this stage, with no limit by language or heart valve position. Articles meeting the following criteria were included for data abstraction: Interventions included percutaneous heart valves; and Study involved valve replacement (rather than repair); and Primary data were reported; and Study was conducted in humans; and Study was conducted in adults (all patients 18 years of age or, if mixed population, then either 80 percent adults or results reported separately for adults); and At least 1 clinical outcome was reported. Note that no restrictions were imposed regarding: Study design (all designs acceptable); or Sample size (n 1 acceptable). When the two reviewers arrived at different conclusions about whether to include or exclude an article, they were asked to reconcile the difference. A single investigator searched the general gray literature sources listed in Table 1 and screened the material identified for potential relevance using the inclusion/exclusion criteria described above for published studies. A single investigator also searched the sources listed in Table 1 for potentially relevant abstracts from recent scientific meetings. Titles and abstracts were screened online, and potentially relevant abstracts were then reviewed in full using the inclusion/exclusion criteria described above for published studies. Abstracts meeting the inclusion criteria were further screened to eliminate those abstracts that duplicated information reported more fully in published studies. For Question 3, we created detailed evidence tables only for published studies (Appendix B, Evidence Table 2). Data abstracted included: date of publication; country; study design; study objectives; duration of followup; number, age, and sex of participants; indication for percutaneous heart valve; valve name; size of catheter; implementation approach; implantation rates; and clinical outcomes, including hemodynamic measurements and 30-day mortality rates, complications, and device dysfunction rates. Important data from the included gray literature and Scientific Information Packets were abstracted into summary tables included in the Results section. Purely descriptive statistics are used to summarize and analyze the data abstracted from the fully published reports, as is appropriate for a horizon scan of literature comprised solely of non-comparative studies. The studies included for this question were not formally assessed for methodological quality. Question 4 focused on variables associated with surgery or setting that may impact outcomes for percutaneous heart valves. In consultation with experts in cardiology and cardiac surgery, we elected to broaden our focus beyond the specific variables listed in the question to include other variables that usually impact outcomes for surgical procedures and that we expected would be reported in published reports identified by our search strategy. In the end, we considered six general categories of variables: (1) prosthesis characteristics; (2) implantation approach; (3) treatment setting; (4) operator characteristics; (5) type of anesthesia; and (6) patient characteristics. For the purpose of answering this question, we focused on device implantation success rates and 30-day survival rates as outcome measures. These two outcomes were consistently reported in most of the studies, and they serve as reasonable proxy measures for the feasibility of delivering prosthetic heart valves percutaneously, as well as for short-term clinical outcomes. For Question 4, we considered a subset of the literature identified for Question 3, namely, the 62 fully published reports that met the inclusion criteria for that question. The methods used to search the published literature, screen potentially relevant citations, and abstract and evaluate data are described above, under Question 3. For Question 4 we also consulted with experts in cardiology and cardiac surgery and incorporated information 6,8,24-30 and perspectives from pertinent, published review articles. For the present question, we excluded data presented at scientific meetings but not yet published in peer-reviewed journals for the following reasons: (1) the data reported in meeting abstracts were insufficient to create sufficiently detailed evidence tables; (2) data presented at scientific meetings often differ from those that later appear in published reports; (3) data presented at meetings are often derived from a subset of patients whose data have undergone 10 only preliminary analysis; and (4) insufficient data are usually presented in the abstracts to identify new patients in ongoing series for which preliminary findings were previously published. Peer Review Process We employed internal and external quality-monitoring checks through every phase of the project to reduce bias, enhance consistency, and verify accuracy. Examples of internal monitoring procedures include the following: three progressively stricter screening opportunities for each article (abstract screening, full-text screening, and data abstraction); involvement of at least two individuals (an abstractor and an over-reader) in each data abstraction; and agreement of at least two investigators on all included studies. A list of peer reviewers who submitted comments on a draft version of this report is provided in Appendix E. In such cases, we attempted to match names based on other device characteristics, such as valve type, or from narrative descriptions in the literature. Some of the valves listed are no longer manufactured, but may be encountered in patients with past valve replacements. These obsolete valves are also described in reviews and primary comparative studies. Classes of Heart Valves Diseased heart valves can be replaced with mechanical or biological valves. The first artificial heart valve was a 31 caged-ball design which utilized a metal cage to house a silicone coated ball. Tilting disc valves employ a disc controlled by a metal strut, which opens and closes with each cardiac cycle. Bileaflet valves utilize two semicircular leaflets that rotate around struts attached to the valve housing. At least six companies manufacture tilting disc or bileaflet mechanical valves that are currently available in the U. Biological valves (bioprosthesis or tissue valves) are classified into two major categories: xenografts made from bovine, porcine, or equine tissue; and homografts obtained from cadaveric donors. Xenografts may have a supporting frame (stent) or no supporting frame (stentless). Percutaneous heart valves are stent-based xenografts that are collapsed onto a catheter and are expanded at the time of implantation. Heart Valve Design Replacement heart valves must be durable in order to minimize the risk of reoperation due to device failure. Factors that affect durability include: valve position; valve design; valve 13 materials; and, for bioprostheses, the processes used to fix tissue and prevent calcification. Desirable functional characteristics are: a non-thrombotic surface; materials that do not predispose to endocarditis; and favorable hemodynamic profiles, including laminar flow, small transvalvular gradients, and minimal regurgitant volumes. Theoretical Advantages and Disadvantages of Different Heart Valves Mechanical heart valves are more durable than bioprostheses and are readily available. However, mechanical valves require lifelong anticoagulation because of a greater risk of thrombosis. Anticoagulation significantly increases the risk for bleeding that may require transfusion, and therefore requires careful monitoring. Caged-ball valves have the disadvantages of noise, hemodynamic inefficiency, and higher rates of thrombotic complications, necessitating a higher 8 degree of anticoagulation than other mechanical valves. Caged-ball valves are no longer marketed in the United States and other developed countries. Tilting disc designs have superior hemodynamic efficiency to caged-ball designs, but have the disadvantage of severe hemodynamic compromise if disc thrombosis or immobility occurs. Because mechanical valves have the longest durability, they are recommended for younger patients (< 65 years old) who are willing to take oral blood thinners. Bioprosthetic heart valves are also readily available and do not require chronic anticoagulation. In addition, they have a simple and standard implantation technique and may have fewer infectious complications than mechanical valves. Structural deterioration is age-related, occurring more rapidly in younger age groups. Biological valves carry the theoretical risk of transmitting infection; at least one bovine valve has been recalled due to concern about transmission of bovine spongiform encephalopathy. Methods for tissue fixation and anticalcification have evolved since early bioprosthetic heart valves. Second-generation valves of this type are glutaraldehyde fixed under low pressure (compared with high pressure with the first generation), which is thought to increase durability. Stented bovine pericardial valves appear to have better hemodynamic performance and longer durability than stented porcine valves, especially in smaller sizes. However, stentless valves may be more technically difficult to implant, increasing operating room time and possibly surgical risk. Regeneration involves the implantation of a restorable matrix that is expected to remodel in vivo and yield a functional valve composed of the cells and connective tissue of the patient. The theoretical advantage is a living tissue that responds to growth and physiological forces in the same way a native valve does. The durability of homograft heart valves depends upon how the valve is recovered, processed, and preserved. Homograft aortic valves are supplied as a composite valve, aortic root, and part of the anterior mitral leaflet. This additional tissue is useful for severe disease due to endocarditis, and homografts are most frequently used for this indication. Like xenografts, homograft (human) heart valves do not require chronic anticoagulation, risk of thromboembolism is very low, and these valves may be less likely to calcify than xenografts.
These activities have mirrored much of the public health response to recent Ebola outbreaks hiv infection via kissing discount albendazole 400mg amex. Furthermore hiv infection per country 400 mg albendazole, Michigan has a surveillance system to detect cases and clusters associated with an infectious disease outbreak as reported by healthcare providers kleenex anti viral box tucher test purchase 400 mg albendazole otc, emergency departments and local health departments hiv infection through cuts discount albendazole 400mg with visa. These task forces include: State Operations hiv infection versus aids albendazole 400 mg free shipping, Health and Human Services hiv dual infection symptoms purchase albendazole 400 mg otc, Education, and Economy/Workforce. It is the fourth leading cause of death in the United States1 and is projected to rank ffth by 2020 in terms of burden of disease worldwide, according to a study by the World Bank and World Health Organization. The recommendations made were mainly based on the published literature available at the time after thorough assessment by the assigned member or members of the working group and discussion at several face-to-face meetings. The evidence used for the recommendations was then graded according to its level of strength with some recommendations made based on the consensus agreement of members of the working group. Notwithstanding, the concept of evidence-based medicine was just emerging at that time. I would like to express my heartfelt gratitude to everyone who was involved in the development of these guidelines and especially to the working group members for their enthusiasm, relentless effort and immense contribution. Bethesda, Maryland: Us Department Of Health And Human Services, Public Health Service, National Institute Of Health. Members responsible for each section were tasked to ensure that the relevant literature was adequately searched, retrieved, critically appraised and accurately presented. The full text of reference articles quoted in these guidelines was carefully studied. In addition, the reference lists of relevant articles retrieved were searched to identify other studies. Each section leader presented his/her section of the proposed guidelines at several meetings where all members of the working group met and participated in the discussion. The fnal draft of these guidelines inclusive of recommendations was the result of agreement by the majority, if not all, members of the working group at such meetings as well as through e-mail discussions in between the meetings. Throughout the development of these guidelines, a total of six meetings were held from 10 January 2009. In situations where the evidence was insuffcient or lacking, the recommendations made were by consensus of the working group. The draft guidelines were also posted on the Ministry of Health Malaysia website for comments and feedback. These guidelines were presented to the Technical Advisory Committee for Clinical Practice Guidelines and the Health Technology Assessment and Clinical Practice Guidelines Council, Ministry of Health Malaysia for review and approval. Mohd Idzwan Zakaria Senior Consultant Chest Physician Emergency Medicine Physician Hospital Pulau Pinang Pusat Perubatan Universiti Malaya Pulau Pinang Kuala Lumpur Datin Dr. Pang Yong Kek Senior Consultant Chest Physician Consultant Chest Physician Institut Perubatan Respiratori Pusat Perubatan Universiti Malaya Hospital Kuala Lumpur Kuala Lumpur Kuala Lumpur Dr. Richard Loh Li Cher Chest Physician Consultant Chest Physician Hospital Universiti Sains Malaysia Kolej Perubatan Pulau Pinang Kubang Kerian Pulau Pinang Kelantan Assoc. Rohaya Abdullah Consultant Chest Physician Family Medicine Specialist Pusat Perubatan Universiti Kebangsaan Malaysia Klinik Kesihatan Masai Kuala Lumpur Johor Bahru Dr. Yap Boon Hung Consultant Primary Care Physician Consultant Chest Physician Pusat Perubatan Universiti Malaya Hospital Tung Shin Kuala Lumpur Kuala Lumpur Dr. Zainudin Md Zin Senior Consultant Chest Physician Senior Consultant Chest Physician Leong Oon Keong Chest & Medical Clinic Sdn. Ashoka Menon Senior Consultant Chest Physician Pusat Perubatan Sime Darby Subang Jaya Associate Professor Ayiesah Hj Ramli Physiotherapy Programme Coordinator Faculty of Allied Health Sciences Universiti Kebangsaan Malaysia Kuala Lumpur Ms P. Devashanti Pharmacist Pusat Perubatan Universiti Malaya Kuala Lumpur Associate Professor Dr Fanny Ko Wai-San Department of Medicine and Therapeutics the Chinese University of Hong Kong Hong Kong Dr. Hooi Lai Ngoh Senior Consultant Chest Physician Public Specialist Centre Georgetown Dr. Jamalul Azizi Abdul Rahman Head of Department & Consultant Respiratory Physician Department of Respiratory Medicine Hospital Queen Elizabeth Kota Kinabalu Dr. Kuppusamy Iyawoo Senior Consultant Chest Physician Hospital Assunta Petaling Jaya Puan Nurhayati Mohd. Nur Clinical Nurse Specialist in Respiratory Medicine Nursing Offcer Pusat Perubatan Universiti Malaya Kuala Lumpur Dr. Wong Wing Keen Senior Consultant Chest Physician Pusat Perubatan Sunway Petaling Jaya Dr. Airfow limitation, associated with an abnormal infammatory reaction of the lung to noxious particles or gases, the most common of which worldwide is cigarette smoke, is usually progressive, especially if exposure to the noxious agents persists. Airfow limitation is best measured by spirometry, the most widely available and reproducible test of lung function. Spirometry should be performed after an adequate dose of an inhaled bronchodilator. Dyspnoea typically on exertion, cough and sputum production sometimes also present. After confrmation of diagnosis by spirometry, the treatment for the individual patient may be based on symptoms with the recognition that symptoms may be made worse by co-morbid conditions which should also be appropriately treated if present. In general, the infammatory and structural changes in the airways increase with disease severity and persist on smoking cessation. Management decisions should be guided by the overall assessment of the patient which should include symptoms, exercise capacity as well as the presence of co-morbidities and complications, in addition to spirometry. This rare hereditary disease is most commonly seen in individuals of Northern European origin. Ammonia, hydrogen sulphide, inorganic dust and organic dust may be causally involved, but a role for specifc biological agents cannot be excluded. However, air pollution from motor vehicle emissions in cities is associated with a decrease in lung function. Some studies have suggested that women are more susceptible to the effects of tobacco smoke than men and raise concerns on the increasing number of female smokers in both developed and developing countries. Early diagnosis with successful smoking cessation interventions reduce the decline in lung function, and early intervention with effective treatment improves symptoms and health status. Extrapulmonary effects such as weight loss, signs of cor pulmonale and other co-morbid conditions should also be identifed and assessed. Physical signs of airfow limitation and air trapping (barrel chest, loss of cardiac and liver dullness, prolonged expiration, reduced breath sounds) are not usually present until the disease is already at an advanced stage. Spirometry should be performed in people with exposure to risk factors who have chronic cough and sputum production even without dyspnoea as it may help identify patients earlier in the course of the disease. Chest Radiograph A chest radiograph is valuable in excluding other diagnoses such as lung cancer, heart failure, bronchiectasis and tuberculosis. High resolution computed tomography scanning is not routinely recommended unless there is diagnostic uncertainty. Other suggested investigations include fasting plasma glucose, serum albumin and serum fasting lipids to detect other common co-morbidities. Body weight and body mass index provide information on the nutritional status of the patient. Active smokers and patients with frequent exacerbations are at risk of faster decline in lung function. Assess the effectiveness of current regimen in controlling symptoms and any side effects from the medications. Ensure that patients are taking their medication at the right dose and frequency and inhaler techniques are correct. Severity can be estimated by the increased need for bronchodilator medication or systemic glucocorticosteroid requirements. Hospitalisations should be documented including the duration of stay and any use of invasive and non-invasive ventilation. Smoking prevention strategies and availability of smoking cessation services should be emphasised to encourage smoke-free lifestyles. Mandatory legal provision for pictorial health warnings on cigarette packs and packages is an effcient way to deliver clear, truthful anti-smoking messages directly to smokers. Such bans are proven to work, resulting in measurable gains in respiratory health. Children less than two years old who are passively exposed to cigarette smoke have an increased prevalence of respiratory infections, and are at a greater risk of developing chronic respiratory symptoms later in life. Effective interventions include individual as well as group programmes such as community-based stop-smoking challenges. Counselling from doctors and other health professionals, given either by individual face-to-face interactions, group interactions or through telephone or web-based quit smoking services 3. Combination of counselling and pharmacotherapy A successful smoking cessation strategy requires a multi-faceted approach that includes sustained escalation in tobacco taxation, coherent government policies and legislations to reduce tobacco demands and production as well as health education and frequent dissemination of consistent anti tobacco messages through the media and settings such as schools. Ask every tobacco user if he or she is willing to make a quit attempt at this time. All forms of nicotine replacement therapy are signifcantly more effective than placebo. Other pharmacotherapy, like bupropion97 (Level I) and nortriptyline have also been shown to increase long term quit rates,98,99 (Level I) but should always be used as one element in a supportive intervention programme rather than on their own. Varenicline, a nicotinic acetylcholine receptor partial agonist that aids smoking cessation by relieving nicotine withdrawal symptoms and reducing the rewarding properties of nicotine has been demonstrated to be safe and effcacious. There are recent concerns that varenicline may be linked with depressed mood, agitation or suicidal thinking and behaviour in some smokers. Although it is not known how many individuals are at risk of developing respiratory disease from occupational exposures, many occupationally induced respiratory disorders can be reduced or controlled through a variety of strategies aimed at reducing the burden of inhaled particles and gases. Secondary prevention, achieved through surveillance and early case detection, is also of great importance. Both approaches are necessary to improve the present situation and to reduce the burden of lung disease. Education has been shown to improve health outcomes in patients with chronic illnesses. Prospective end-of-life discussion can lead to better understanding of advanced directives and effective therapeutic decision at end of life. Nonetheless, they have not been shown to have a consistent impact on quality of life. A higher proportion of subjects in the cilomilast group were exacerbation-free at 24 weeks compared with those on placebo (74% versus 62%). Theophylline can be added to patients who are symptomatic despite maximum inhaled therapy. It includes exercise, education, psychosocial and behavioural intervention by an interdisciplinary team of specialists. There is no consensus on the optimal duration of pulmonary rehabilitation programmes. General aerobic conditioning is more helpful than specific training of respiratory muscles. Beneft is seen even in irreversible pulmonary disorders, since much of the disability and handicap results not just from the respiratory disorder per se but from secondary morbidities that often are treatable. Although the degree of airway obstruction or lung hyperinfation does not change much with pulmonary rehabilitation, reversal of muscle deconditioning and better pacing enables patients to walk further with less dyspnoea. Supplemental oxygen should be used during rehabilitative exercise training in patients with severe exercise-induced hypoxaemia. Efforts should be directed towards the setting up of both hospital and home-based programmes locally. Arterial blood gas measurements should be made on two occasions when the patient is in a stable condition and on optimal treatment. It should be prescribed by a qualifed medical practitioner and titrated carefully due to concerns of carbon dioxide retention. Weight loss may further exacerbate decreased respiratory muscle strength and increase dyspnoea and impair immunity. Studies of nutritional supplementation alone have not shown improvement in pulmonary function or exercise capacity. Ongoing research is currently exploring how nutritional support can enhance exercise training and optimise the effects of pulmonary rehabilitation. Surgical techniques used have included thoracotomy, video-assisted thoracoscopy and stapled wedge resection. However, at the present time it is limited to younger patients with other chronic lung diseases. The 5-year survival after transplantation for emphysema is 45 to 60% in Western series. Elective surgery should be deferred in patients who are symptomatic, have poor exercise capacity or have acute exacerbations. Bronchodilators, smoking cessation (at least 4-8 weeks preoperatively is optimal), antibiotics, and chest physical therapy may help signifcantly reduce pulmonary complications.
References
- Hellegers A, Schruefer J. Nomograms and empirical equations relating oxygen tension, percentage saturation, and pH in maternal and fetal blood. Am J Obstet Gynecol. 1961;81:377.
- Gandy SJ, Armoogum K, et al. A clinical MRI investigation of the relationship between kidney volume measurements and renal function in patients with renovascular disease. Br J Radiol 2007; 80:12.
- Boutin C, Dumortier P, Rey F. Black spots concentrate oncogenic fibers in the parietal pleura. Am J Respir Crit Care Med 1996;153:444-9.
- Wollina U: Acute paronychia: comparative treatment with topical antibiotic alone or in combination with corticosteroid. J Eur Acad Dermatol Venereol 15:82-84, 2001.
- Dietz DW, Laureti S, Strong SA, et al. Safety and longterm efficacy of strictureplasty in 314 patients with obstructing small bowel Crohn's disease. J Am Coll Surg 2001;192:330-37; discussion 337-38.