Virginia Fleming, PharmD, BCPS
- Clinical Assistant Professor, Clinical and Administrative Pharmacy
- University of Georgia College of Pharmacy, Athens, Georgia

https://rx.uga.edu/faculty-member/virginia-fleming-pharm-d/
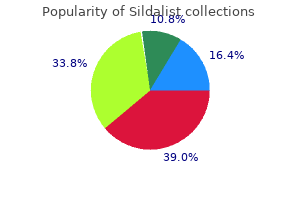
Abscesses in Corynebacterium No Diagnostic sampling is sheep (Caseous pseudotuberculosis antimicrobials erectile dysfunction treatment in egypt buy cheap sildalist. Ureaplasma sp Recurrent medication or poor effcacy of medicines: Sampling every time or at least once a year erectile dysfunction doctors in st. louis sildalist 120 mg with mastercard. Mycoplasma bovis Oxytetracycline Duration of the course: Dairy cows one to two weeks erectile dysfunction pills photos purchase 120mg sildalist with amex. Mycoplasma bovis Oxytetracycline Macrolides the alternative treatment Youngstock and is to be selected if the bulls signs have not eased in two days or they worsen or the disease recurs within a week otc erectile dysfunction pills walgreens effective sildalist 120 mg. The duration of an oxytetracycline course is a minimum of 7 or 2 days after the signs have disappeared erectile dysfunction gene therapy treatment 120 mg sildalist otc. Cryptosporidiosis Cryptosporidium Improvement to the laboratory test is parvum hygiene best erectile dysfunction pills at gnc discount sildalist 120 mg free shipping. Urinary tract Causative First-line Alternative Disease microbe treatment treatments Notes Cystitis Corynebacterium Benzylpenicillin Based on renale, the results of Escherichia coli susceptibility testing. Udder Causative First-line Alternative Disease microbe treatment treatments Notes Streptococcus Str. Staphylococcus β-lactamase Benzylpenicillin Combination of treatments; mastitis negative: systemic and intramammary. Staphylococcus cephalosporins Cloxacillin and frst aureus generation cephalosporins may promote the selection of meticillin-resistant strains. Marbofoxacin Antimicrobials necessary only for newly-calved cows and in severe cases. The animal should be culled, even if the infection is latent and the milk normal in appearance. The mastitis pyogenes, prognosis is poor for the Streptococcus affected quarter; supportive dysgalactiae, therapy. Mastitis in goats Treatment on Special attention should be the basis of a paid to the susceptibility of bacteriological S. If several animals are Escherichia coli, affected, diagnostic sampling other bacteria should be conducted. Other infections Causative First-line Alternative Disease microbe treatment treatments Notes Systemic Several bacterial Trimethoprim Oxytetracycline Prevention is important. If multiple deceased ruminants Trueperella animals are involved, (omphalitis, pyogenes, diagnostic sampling should be polyarthritis, streptococci, conducted. Listeriosis Listeria Benzylpenicillin Oxytetracycline A large dose of monocytogenes benzylpenicillin is used (note the withdrawal period. Caesarean Benzylpenicillin Benzylpenicillin + Longer treatment and section fuoroquinolones a broader spectrum if Oxytetracycline the abdominal cavity is contaminated during the operation. Treatment of a No Benzylpenicillin Intramammary treatment, in teat injury antimicrobials First generation addition to milking at short unless mastitis cephalosporins intervals. Therefore, pig farms should pay attention to the use of antimicrobials, withdrawal periods, the emergence of resistant bacterial strains and alternatives to antimicrobials. Veterinarians are tasked with planning farm-specifc measures, which maintain health and prevent diseases, enabling a reduction in the use of antimicrobials. Factors related to environmental conditions and hygiene, the quality of feed, suffcient supply of colostrum and the minimisation of factors which expose pigs to diseases are important aspects in the prevention of many disease outbreaks. With regard to swine diseases, the division into compartments in accordance with the production phase and animal groups and an all-in/all-out system are the key operational models in preventing disease outbreaks. The terms of the stakeholders health classifcation register for pig farms take into account infections that are signifcant in Finland, such as porcine enzootic pneumonia, swine dysentery and progressive atrophic rhinitis. The primary aim is to maintain pig farms free from such infections and if necessary, to eradicate signifcant pathogens from production units. Medication is administered to individual pigs through injections or to groups of pigs via feed or water. The veterinarian responsible for the farm decides on a case-by-case basis when it is better to shift from treatment of individual pigs to group medication. When morbidity exceeds 20% or mortality 2%, medication is shifted from individuals to groups. In large units, it is often necessary to switch to group medication at an earlier stage, as the administration of medication to a large number of individual pigs becomes too laborious. The advantage of group medication is considered to be its ease and, on occasion, its affordability: less work is required, as an injection does not need to be administered to each pig individually and the animals will not become stressed on account of the treatment. However, sick animals do not eat or drink normally, so the amount of medicine that they receive may be too low. If antimicrobials are administered in feed or water, at least initially animals that do not eat must be individually treated through injections. Some infectious diseases in pigs concern individual animals only; in such cases it is expedient to treat only sick animals individually. Administering medication individually in groups of animals is laborious, and the use of separate pens for sick animals facilitates the targeting of sick pigs in administering medication. A good pen for sick animals helps them to recover, and its use is an integral part of the treatment of sick pigs. In pigs, the absorption of medicines from the gastrointestinal tract is, in principle, similar to that of humans. In parenteral administration of medicines, it must be borne in mind that adult pigs have a thick layer of subcutaneous fat, which makes the technique of intramuscular injections diffcult to master. The absorption of medicine from fat tissue is unpredictable; some medicinal substances may remain in the fat, and suffcient concentrations do not reach the site of the infection. Due attention must be paid to the correct dosage of medicines in newborn piglets: overdoses and concentrated preparations must be avoided. Procaine penicillin is not recommended for pregnant sows because the risk of abortion. The choice of antimicrobials must be based on a diagnosis that is as accurate as possible. This also includes the identifcation of the causative microbe and the antimicrobial susceptibility testing. In order to reach a diagnosis, a post-mortem examination must be performed on the carcasses of a few pigs that had been sick with typical signs, or other samples must be taken for laboratory examination, particularly if a large number of pigs exhibit such signs or they exhibit signs repeatedly. If antimicrobials are administered as group treatments or repeatedly to individual animals due to similar signs, legislation also requires that veterinarians must ensure the microbiological diagnosis and the antimicrobial susceptibility of the causative microbe. A medication plan should be drawn up for each pig farm to ensure that the range of different antimicrobials remains as small as possible. Response to treatment is followed up and, if necessary, samples are sent to a laboratory for antimicrobial susceptibility testing. With regard to group medication, the number of animals to be treated and the duration of the treatment are carefully assessed on a case-by-case basis. If eradication of the pathogen is impossible, and if recurrent cases of disease are detected in a certain age group, herd health measures should be taken to prevent the animals from falling ill. The planning and implementation of preventive measures requires an accurate diagnosis. Special attention must be paid to the prevention of post-weaning diarrhoea caused by enterotoxigenic Escherichia coli bacteria. Recurrent use of antimicrobials increases the risk of resistance to antimicrobials. Dosage of antimicrobials in pigs In the summary of product characteristics, some doses of antimicrobials are too low. Research on effective doses is only accumulated slowly, and knowledge transfer to the feld is challenging. Marketing authorisations for medicines have been granted based on research conducted using specifc doses, and this also determines the withdrawal period. Veterinarians may advise that a medicine should be used in doses higher than those indicated in the summary of product characteristics, or more frequently but, in that case, they must then 20 Recommendations for the use of antimicrobials in the treatment of the most signifcant infectious and contagious diseases in animals: Pigs set a longer withdrawal period. In Sweden, in 2012, the Medical Products Agency gathered information on the use of antimicrobials, including instructions of doses1. The publication includes most recent research on the dosage levels to be used in pigs. Pigs Recommendations for the selection of antimicrobials for pigs in cases where the use of antimicrobials is necessary regarding the diagnosis in question. Medicinal substances or groups of medicinal substances which are most appropriate for treatment of a disease in terms of pathogen, disease, resistance situation and characteristics of the medicinal substance are specifed as frst-line treatment. Thus, medicinal substances which are effective for the most common pathogens of a disease have been selected as the frst-line treatment. For example, regarding diseases from which several different bacterial species can be isolated, treatment is often targeted at the most common pathogens. Respiratory tract Causative First-line Alternative Disease microbe treatment treatments Notes Pleuropneumonia Actinobacillus Benzylpenicillin Tiamulin Vaccination is possible. Condition of being free from the disease is included in the Sikava health classifcation register Porcine enzootic Mycoplasma Tiamulin Tetracyclines Primarily eradication. Gastrointestinal tract Causative First-line Alternative Disease microbe treatment treatments Notes Gastroenteritis, Toxigenic Trimethoprim Based on Vaccinating sows is diarrhoea Escherichia coli sulfonamides the results of recommended for the in piglets Aminopenicillins susceptibility prevention of diarrhoea in testing. Post-weaning Toxigenic Trimethoprim Based on Resistance: Following up diarrhoea 1–14 Escherichia coli sulfonamides the results of the response to treatment days after weaning Aminopenicillins susceptibility is important; some toxigenic testing. Haemorrhagic Clostridium Phenoxymethyl Vaccination of sows must diarrhoea in piglets perfringens, penicillin start immediately. Administration of medication should be continued only as long as the vaccination programme begins to provide protection. Diarrhoea in piglets Clostridium Benzylpenicillin Amino Vaccination of sows 1–7 days old perfringens, penicillins Type A Swine dysentery Brachyspira Tiamulin Based on Primarily eradication. Rare; the diagnosis hyodysenteriae the results of A monthly reported animal must be ensured susceptibility disease. Condition of Lincomycin being free from the Tylosin or disease is included another in the Sikava macrolide health classifcation register 22 Recommendations for the use of antimicrobials in the treatment of the most signifcant infectious and contagious diseases in animals: Pigs Gastrointestinal tract Causative First-line Alternative Disease microbe treatment treatments Notes Diarrhoea Brachyspira Tiamulin Based on caused by other pilosicoli the results of brachyspira species susceptibility (Brachyspira testing: intermedia) Lincomycin Tylosin or another macrolide Proliferative Lawsonia Tylosin or another Tiamulin Other possible concurrent enteropathies intracellularis macrolide Tetracyclines intestinal infections will affect the choice of medication. Salmonellosis Various types of Antimicrobials An animal disease that salmonella must not be used must be controlled by law. Oedema disease Escherichia Trimethoprim Based on coli producing sulfonamides the results of oedema disease Aminopenicillins susceptibility toxin testing. Kidneys and urinary tract Causative First-line Alternative Disease microbe treatment treatments Notes Infammation of the Escherichia coli Trimethoprim Amino Resistance: the bladder (cystitis), sulfonamides penicillins antimicrobial susceptibility urinary tract of E. Urinary tract Actinobaculum Benzylpenicillin Amino infection (cysto suis penicillins pyelonephritis) Reproductive tract Causative First-line Alternative Disease microbe treatment treatments Notes Metritis Coliforms Trimethoprim Based on Resistance: the (endometritis) sulfonamides the results of antimicrobial susceptibility susceptibility of E. Chronic mastitis Gram-positive Benzylpenicillin Amino bacteria penicillins Central nervous system Causative First-line Alternative Disease microbe treatment treatments Notes Meningitis Streptococci, Benzylpenicillin Amino the emergence of S. If necessary, a more detailed monocytogenes, examination of the primary Escherichia coli) cause of central nervous system signs must be performed; viral infections may also give rise to signs in the central nervous system. Musculoskeletal system Causative First-line Alternative Disease microbe treatment treatments Notes Arthritis Streptococci, Benzylpenicillin Aminopenicillins Haemophilus Tetracyclines parasuis, Erysipelothrix rhusiopathiae Mycoplasma Tylosin hyosynoviae Lincomycin Tiamulin Foot infections Fusobacterium Benzylpenicillin Tetracyclines necrophorum, Trueperella pyogenes + other 24 Recommendations for the use of antimicrobials in the treatment of the most signifcant infectious and contagious diseases in animals: Pigs Systemic infection Causative First-line Alternative Disease microbe treatment treatments Notes Swine erysipelas Erysipelothrix Benzylpenicillin Tetracyclines Vaccination is possible. Glässers disease Haemophilus Benzylpenicillin Trimethoprim Vaccination is possible; parasuis sulfonamides a preparation subject to Aminopenicillins a special permit. Tetracyclines Skin Causative First-line Alternative Disease microbe treatment treatments Notes Greasy pig disease Staphylococcus Benzylpenicillin Based on Resistance: Some (exudative hyicus the results of S. Individual strains exhibit resistance to trimethoprim sulfonamides, tetracycline or enrofoxacin. Resistance to tetracycline, lincomycin, macrolides, trimethoprim sulfonamides or enrofoxacin also occurs. Ears Causative First-line Alternative Disease microbe treatment treatments Notes Otitis media Streptococci Benzylpenicillin Trimethoprim sulfonamides Other Causative First-line Alternative Disease microbe treatment treatments Notes Tail biting Several (of oral Benzylpenicillin microfora) Necrobacillosis in Fusobacterium Benzylpenicillin Trimethoprim piglets necrophorum sulfonamides 25 Recommendations for the use of antimicrobials in the treatment of the most signifcant infectious and contagious diseases in animals: Horses Horses While horses are valuable domestic animals, some horses are also food-producing animals. Legislation provides exceptions regarding medication to be administered to horses. These exceptions are based on the fact that horses are identifed and that they have identifcation documents. Horses are food-producing animals and medicines approved for food-producing animals may be used on them. These medicines have a six-month withdrawal period, and information on their administration must always be entered in the identifcation document, unless the equine animal is not intended for slaughter for human consumption. If the equine animal is not intended for slaughter for human consumption, medicines whose usage is prohibited in food-producing animals may also be used on the horse in question. Equestrian organisations have also issued doping-related withdrawal periods for medicines. Some antimicrobials affect the microbes in the colon by disrupting its balance and may in this way, for example, cause fatal diarrhoea in a horse. On account of their undeveloped intestinal microbes, foals are less sensitive to the negative effects of antimicrobials; consequently, a wider range of antimicrobials can be administered to them. Whenever sampling is possible, the treatment of an infection should be based on the identifcation of the pathogen and on the examination of its susceptibility to antimicrobials. Legislation on medication also requires sampling if an animal is repeatedly treated for the same signs or if antimicrobials classifed as critically important are used. Information on the role that various pathogens play in the diseases of different organ groups are indicative only, as the geographical area and the use of medicinal substances select microbes that cause a disease. If the response to treatment when using the selected antimicrobial is poor, it is of vital importance to verify the diagnosis and to attempt to fnd out the pathogen and its susceptibility to antimicrobials. Horses Recommendations as alternatives to selection of antimicrobials for horses in cases where the use of antimicrobials is necessary regarding the diagnosis in question. Medicinal substances or groups of medicinal substances which are most appropriate for treatment of a disease in terms of pathogen, disease, resistance situation and characteristics of the medicinal substance are specifed as frst-line treatment. Thus, medicinal substances which are effective for the most common pathogens of a disease have been selected as frst-line treatment. For example, regarding diseases from which several different bacterial species can be isolated, treatment is often targeted at the most common pathogens.
Probiotics for the prevention of Clostridium difficile–associated diarrhea in adults and children erectile dysfunction treatment comparison 120mg sildalist with mastercard. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic erectile dysfunction gluten purchase 120mg sildalist free shipping. Systematic review: probiotics in the management of lower gastrointestinal symptoms in clinical practice — an evidence-based international guide erectile dysfunction doctor in bhopal buy sildalist toronto. Progress in our understanding of the gut microbiome: implications for the clinician erectile dysfunction options order sildalist no prescription. Prophylactic probiotics for preterm infants: a systematic review and meta-analysis of observational studies zyrtec causes erectile dysfunction buy sildalist 120 mg on-line. Probiotics in nonalcoholic fatty liver disease leading causes erectile dysfunction purchase sildalist 120mg amex, nonalcoholic steatohepatitis, and cirrhosis. Therapies aimed at the gut microbiota and inflammation: antibiotics, prebiotics, probiotics, synbiotics, anti-inflammatory therapies. Treatment and prevention of pouchitis after ileal pouch-anal anastomosis for chronic ulcerative colitis. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Dietary modulation of the human colonic microbiota: introducing the concept of prebiotics. Probiotics are effective at preventing Clostridium difficile-associated diarrhea: a systematic review and meta-analysis. A systematic review and meta-analysis of probiotics for the management of radiation induced bowel disease. The effect of probiotics supplementation on Helicobacter pylori eradication rates and side effects during eradication therapy: a meta-analysis. Clinical trial on the efficacy of a new symbiotic formulation, Flortec, in patients with acute diarrhea: a multicenter, randomized study in primary care. Probiotics for the prevention and treatment of antibiotic-associated diarrhea: a systematic review and meta-analysis. Systematic review with meta-analysis: Saccharomyces boulardii in the prevention of antibiotic-associated diarrhoea. Probiotics reduce symptoms of antibiotic use in a hospital setting: a randomized dose response study. The effect of a multispecies probiotic on the intestinal microbiota and bowel movements in healthy volunteers taking the antibiotic amoxycillin. Is primary prevention of Clostridium difficile infection possible with specific probiotics? Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children. Clostridium difficile pilot study: effects of probiotic supplementation on the incidence of C. Effect of the prebiotic oligofructose on relapse of Clostridium difficile-associated diarrhea: a randomized, controlled study. Probiotics for standard triple Helicobacter pylori eradication: a randomized, double-blind, placebo-controlled trial. Impact of Lactobacillus reuteri Supplementation on Anti-Helicobacter pylori Levofloxacin-Based Second-Line Therapy. Helicobacter pylori infection in clinical practice: probiotics and a combination of probiotics + lactoferrin improve compliance, but not eradication, in sequential therapy. Adjuvant probiotics improve the eradication effect of triple therapy for Helicobacter pylori infection. Kefir improves the efficacy and tolerability of triple therapy in eradicating Helicobacter pylori. Meta-analysis: the effect of supplementation with probiotics on eradication rates and adverse events during Helicobacter pylori eradication therapy. Francavilla R, Polimeno L, Demichina A, Maurogiovanni G, Principi B, Scaccianoce G, et al. Lactobacillus reuteri strain combination in Helicobacter pylori infection: a randomized, double blind, placebo-controlled study. Lactobacillus reuteri in management of Helicobacter pylori infection in dyspeptic patients: a double-blind placebo-controlled randomized clinical trial. Non-absorbable disaccharides versus placebo/no intervention and lactulose versus lactitol for the prevention and treatment of hepatic encephalopathy in people with cirrhosis. Probiotics prevent hepatic encephalopathy in patients with cirrhosis: a randomized controlled trial. Secondary prophylaxis of hepatic encephalopathy in cirrhosis: an open-label, randomized controlled trial of lactulose, probiotics, and no therapy. Probiotics can improve the clinical outcomes of hepatic encephalopathy: An update meta-analysis. Meta-analysis: the effects of gut flora modulation using prebiotics, probiotics and synbiotics on minimal hepatic encephalopathy. Effects of probiotic yogurt consumption on metabolic factors in individuals with nonalcoholic fatty liver disease. Synbiotic supplementation in nonalcoholic fatty liver disease: a randomized, double-blind, placebo controlled pilot study. Effect of a Probiotic and Metformin on Liver Aminotransferases in Non-alcoholic Steatohepatitis: A Double Blind Randomized Clinical Trial. Effect of a probiotic on liver aminotransferases in nonalcoholic fatty liver disease patients: a double blind randomized clinical trial. Bifidobacterium longum with fructo-oligosaccharides in patients with non alcoholic steatohepatitis. Efficacy of prebiotics, probiotics, and synbiotics in irritable bowel syndrome and chronic idiopathic constipation: systematic review and meta-analysis. The efficacy of a synbiotic containing Bacillus Coagulans in treatment of irritable bowel syndrome: a randomized placebo-controlled trial. Therapeutic effects, tolerability and safety of a multi-strain probiotic in Iranian adults with irritable bowel syndrome and bloating. A randomized, double-blind, placebo-controlled multicenter trial of saccharomyces boulardii in irritable bowel syndrome: effect on quality of life. Efficacy of an encapsulated probiotic Bifidobacterium infantis 35624 in women with irritable bowel syndrome. The efficacy of probiotics in the treatment of irritable bowel syndrome: a systematic review. Kajander K, Myllyluoma E, Rajilić-Stojanović M, Kyrönpalo S, Rasmussen M, Järvenpää S, et al. Clinical trial: multispecies probiotic supplementation alleviates the symptoms of irritable bowel syndrome and stabilizes intestinal microbiota. The effects of regular consumption of short-chain fructo-oligosaccharides on digestive comfort of subjects with minor functional bowel disorders. Clinical trial: the effects of a trans galactooligosaccharide prebiotic on faecal microbiota and symptoms in irritable bowel syndrome. Effects of a proprietary Bacillus coagulans preparation on symptoms of diarrhea predominant irritable bowel syndrome. Effect of a double-coated probiotic formulation on functional constipation in the elderly: a randomized, double blind, controlled study. The effect of Lactobacillus reuteri supplementation in adults with chronic functional constipation: a randomized, double-blind, placebo-controlled trial. Fermentation and bulking capacity of indigestible carbohydrates: the case of inulin and oligofructose. Effect of synbiotic in constipated adult women a randomized, double-blind, placebo-controlled study of clinical response. Randomised clinical trial: mesalazine and/or probiotics in maintaining remission of symptomatic uncomplicated diverticular disease-a double-blind, randomised, placebo-controlled study. High-fibre diet and Lactobacillus paracasei B21060 in symptomatic uncomplicated diverticular disease. Probiotics and Synbiotics Decrease Postoperative Sepsis in Elective Gastrointestinal Surgical Patients: a Meta-Analysis. Efficacy of Lactobacillus casei treatment on small bowel injury in chronic low-dose aspirin users: a pilot randomized controlled study. Treatment and prevention of pouchitis after ileal pouch-anal anastomosis for chronic ulcerative colitis. Maintaining remission of ulcerative colitis with the probiotic Escherichia coli Nissle 1917 is as effective as with standard mesalazine. Non-pathogenic Escherichia coli versus mesalazine for the treatment of ulcerative colitis: a randomised trial. Fermented milk containing Lactobacillus casei strain Shirota reduces incidence of hard or lumpy stools in healthy population. Saccharomyces boulardii for treating acute gastroenteritis in children: updated meta-analysis of randomized controlled trials. Lactobacillus acidophilus Yogurt and Supplement in Children with Acute Diarrhea: A Clinical Trial. Probiotics in the Treatment of Acute Diarrhea in Young Children | Kianifar | Iranian Journal of Medical Sciences. Treatment of acute infectious diarrhoea in infants and children with a mixture of three Lactobacillus rhamnosus strains-a randomized, double-blind, placebo-controlled trial. Probiotics for treatment of acute diarrhoea in children: randomised clinical trial of five different preparations. Three-combination probiotics therapy in children with salmonella and rotavirus gastroenteritis. A randomized, double-blind, controlled trial using two different probiotic preparations in Bolivian children. Feeding of Bifidobacterium bifidum and Streptococcus thermophilus to infants in hospital for prevention of diarrhoea and shedding of rotavirus. Effect of long term consumption of probiotic milk on infections in children attending day care centres: double blind, randomised trial. Randomized trial of probiotics and calcium on diarrhea and respiratory tract infections in Indonesian children. Gutierrez-Castrellon P, Lopez-Velazquez G, Diaz-Garcia L, Jimenez-Gutierrez C, Mancilla Ramirez J, Estevez-Jimenez J, et al. Diarrhea in Preschool Children and Lactobacillus reuteri: A Randomized Controlled Trial. A patient-oriented, double-blind, cluster-randomized, placebo controlled, clinical trial. Multicentric study of the effect of milk fermented by Lactobacillus casei on the incidence of diarrhoea. Role of probiotic in preventing acute diarrhoea in children: a community-based, randomized, double-blind placebo controlled field trial in an urban slum. Probiotics for the prevention of allergy: A systematic review and meta-analysis of randomized controlled trials. Benefits of probiotics on enteral nutrition in preterm neonates: a systematic review. Systematic review with meta-analysis: Saccharomyces boulardii supplementation and eradication of Helicobacter pylori infection. Effectiveness of Lactobacillus reuteri in infantile colic and colicky induced maternal depression: a prospective single blind randomized trial. Treating infant colic with the probiotic Lactobacillus reuteri: double blind, placebo controlled randomised trial. Prophylactic use of a probiotic in the prevention of colic, regurgitation, and functional constipation: a randomized clinical trial. Probiotic Escherichia coli Nissle 1917 (EcN) for successful remission maintenance of ulcerative colitis in children and adolescents: an open-label pilot study. Vaginal douching is prevalent practice in Turkey as traditional and religious Aim: this study was conducted to evaluate the improvement for vaginitis symptoms in a vaginal douching cessation education. A subgroup of the douching women were educated regarding unhealthy effects of vaginal douching. The women that had ceased vaginal douching by education were considered as the experimental group of this study, the vaginal doucher women as the 1 control group and non-doucher as the 2st nd control group. Results: the participants presented to the outpatients clinic with symptoms of vaginal discharge, dyspareunia, itching, lower abdominal pain, bad vaginal odour, dysuria and irritation; 62. The difference between the experimental and control groups in terms of improvement was found to be statistically significant. Conclusions: the results indicate that vaginal douching cessation education proved douching ceasing and douche ceasing reduces the risk of vaginal inflammation. Introduction as a consequence, it has a special importance in terms of womens health. The vaginal the vagina is the lower part of the birth ecosystem flora provides protection against canal from which menstrual blood is emptied pathogenic microorganisms. The vagina is the women feel an inherent pressure to perform passage between the female internal and vaginal cleaning. A healthy vagina is the practice of washing the vaginal canal implies sexual and reproductive health, and, Methods It is widely practiced by women all over the Study aim world that consider it an important practice of self-hygiene. This study is an intervention study conducted in a rural area of southern Turkey at the Vaginal douching is a common practice Faculty of Medicines Gynaecology among married women in rural areas of Outpatient Clinic between July and Turkey. Vaginal women between the ages of 18 and 49 who douching is prevalent practice in Turkey as presented at the clinic between these dates.
Delegate Vote: Agree: 97% erectile dysfunction medication new quality sildalist 120 mg, Disagree: 2% muse erectile dysfunction wiki discount sildalist uk, Abstain: 1% (Strong Consensus) Justification: the scientific rationale for antibiotic prophylaxis is to inhibit or eliminate contaminating microorganisms that gain access to the surgical site during the procedure erectile dysfunction genetic generic sildalist 120 mg without prescription, which reduces the probability of an established infection erectile dysfunction joke order sildalist online now. Thus erectile dysfunction doctors tucson az purchase sildalist 120mg with visa, the goal of administering preoperative antibiotics is to allow for adequate tissue (blood erectile dysfunction treatment in tampa purchase sildalist 120mg mastercard, soft tissue, and bone) concentrations by the time of incision. Some studies suggest that within 2 hours of incision is best, while others recommend scheduling the dose as close to surgical incision as possible. In addition to these guidelines, it is critically important to have surveillance measures in place to document compliance with these protocols. Prophylactic antibiotics should be administered within one hour before skin incision. When a proximal tourniquet is used, the antibiotic must be completely infused before 53 2 inflation of tourniquet. Timing < 2hrs: the seminal article on this subject studied the timing of administration of prophylactic antibiotics and the risk of surgical wound infections in clean and clean 5 contaminated cases at a large community hospital. The authors found that the rate of infection was lowest for patients who received 5 an antibiotic from 0 to 2 hours before the incision. Specifically, of the 1,708 patients who received prophylactic antibiotics during this time frame, only 10 (0. However, this study was conducted in 1985 to 1986, when there was considerable variation in timing of administration of the prophylactic antibiotic, and only 35% of patients received their dose within the contemporary standard of one hour prior to incision. The authors found that among other negative predictors, administration of an antibiotic for longer than 60 minutes preoperatively was 7 associated with a higher rate of infectious complications. In a large, retrospective cohort study using National Veterans Affairs data on prophylactic antibiotics of 32,459 surgical procedures from 2005-2009, Hawn et al. When antibiotics requiring long infusion times (eg vancomycin) were excluded, the infection risk following administration of antibiotics within 30 minutes was 1. They found that an interval of 10 minutes prior to tourniquet inflation was necessary to obtain adequate prophylaxis. While the patients obtained adequate levels in bone at 5 minutes, an interval of 10 minutes or more was required for 11 patients to have therapeutic levels in the subcutaneous fat. The median percentage of cefazolin penetration into soft tissue and bone for the 5, 2, and 1 minute groups was 14. The authors did not find a significant difference in the incidence of infection at 3. The authors concluded that administration of antibiotics just 13 prior to release of tourniquet was not inferior to a standard prophylactic regimen. Surveillance Measures: In a study evaluating the impact of a new national project meant to reduce infections in arthroplasty surgery in Sweden, Dahl et al. Question 2: Is there an optimal antibiotic that should be administered for routine perioperative surgical prophylaxis? Consensus: A first or second-generation cephalosporin (cefazolin or cefuroxime) should be administered for routine perioperative surgical prophylaxis. Delegate Vote: Agree: 89%, Disagree: 8%, Abstain: 3% (Strong Consensus) Justification: A first or second generation cephalosporin should be administered for routine perioperative surgical prophylaxis because of its broad spectrum of action, cost-effectiveness, and the need to preserve newer and more expensive therapies for drug-resistant microorganisms and emerging pathogens. These antibiotics cover gram-positive organisms and 6 clinically important aerobic gram-negative bacilli and anaerobic gram positive organism. Additionally, they have excellent distribution profiles in bone, synovium, muscle, and 15 hematomas. The optimal prophylactic antibiotic should be bactericidal (penicillin, cephalosporin, vancomycin, or aminoglycosides), not simply bacteriostatic (clindamycin, which is a lincosamide. The agent should also have a half-life that covers the decisive interval (the first 2 hours after incision or contamination) with therapeutic concentrations from time of incision to wound closure. In Scandinavia and elsewhere, isoxazolyl penicillin, such as cloxacillin, flucloxacillin, nafcilin, or oxacillinis used as an appropriate alternative. Some institutions administer carbapenems (namely imipenem/cilastin and meropenem) to patients with penicillin allergy, as they felt that the potential for cross-reactivity 19 between carbapenems and penicillin is less than traditionally believed. The authors found no statistically significant difference between the two regimens. In a study investigating the bacterial colonization and resistance patterns of a cohort of patients undergoing primary joint arthroplasty in Sweden, Stefansdottir et al. Question 3: What is the choice of antibiotic in patients who have pre-existing prostheses such as heart valves? Consensus: the choice of antibiotics for patients with pre-existing prostheses such as heart valves, is the same as routine elective arthroplasty. The first 9 guidelines (published between 1955 and 1997) were based on low-level evidence; only more recently have the guidelines been stratified based on lifetime risk of infective endocarditis. Infections that complicate heart valve replacement and prosthetic joint replacement have several features in common. It is generally accepted that antimicrobial prophylaxis reduces the frequency of early postoperative infections; however, when such infections do occur, they are difficult to control without removing the prosthesis. Consensus: Curently teicoplanin and vancomycin are reasonable alternatives when routine antibiotic prophylaxis cannot be administered. As vancomycin is more difficult to administer and has a shorter half-life and poorer tolerability profile than teicoplanin, the latter 34 may be a better choice in these settings. Teicoplanin is notable for having a long half-life (32 176 hours), low toxicity, and good tissue penetration, which allows it to achieve therapeutic 33, 35 concentrations in bone and surrounding soft tissues. Additionally, a non significant difference in adverse events was recorded in the two groups, with 3 (0. Consensus: In a patient with a known anaphylactic reaction to penicillin, vancomycin or clindamycin should be administered as prophylaxis. Delegate Vote: Agree: 88%, Disagree: 10%, Abstain: 2% (Strong Consensus) Question 5B: What antibiotic should be administered in a patient with a known non anaphylactic penicillin allergy? Consensus: In a patient with a reported non-anaphylactic reaction to penicillin, a second generation cephalosporin can be used safely as there is limited cross-reactivity. Penicillin skin testing may be helpful in certain situations to clarify whether the patient has a true penicillin allergy. Delegate Vote: Agree: 87%, Disagree: 9%, Abstain: 4% (Strong Consensus) Justification: When patients present with a penicillin allergy, further information should be obtained to determine whether an Immunoglobulin E(IgE)-mediated response (anaphylaxis) occurred. In patients with a documented IgE-mediated response to penicillin, third and fourth generation cephalosporins can be used. First and second generation cephalosporins with R1 side chains similar to that of penicillin (cefaclor, cefadroxil, cefatrizine, cefprozil, cephalexin, or cephradine) should be avoided; first and second generation cephalosporins with different R1 side chains can be given. Vancomycin and clindamycin are recommended as alternative agents for patients who have a true type I β-lactam allergy, manifested by immediate urticaria, laryngeal edema, or 3 bronchospasm. Therefore a second agent should be considered (levofloxacine, moxi-floxacine) in addition to 8 vancomycin. Cross-reactivity between penicillin and cephalosporin is overestimated and much lower than reported in earlier studies. The 10% estimate of risk of allergic reactions to cephalosporins in penicillin-allergic patients is based on data collected and reviewed in the 1960s and 1970s. It is due in large part to the widely referenced reviews of Dash and Petz, which reported allergic reactions in 7. The high cross-reactivity found in earlier studies may be due in part to 39, 40 contamination of the study drugs with penicillin during the manufacturing process. Moreover, the authors of the early studies had a broader definition of allergy and did not account for the fact that penicillin-allergic patients have an increased risk of adverse reactions to 41, 42 any medication. Skin testing in penicillin-allergic patients cannot reliably predict an allergic 43 response to a cephalosporin, particularly to compounds with dissimilar side chains. However, 44 skin testing may be useful in determining whether a true allergy to penicillin exists. Twenty-seven articles on the topic of the cross-reactivity of penicillin and cephalosporin were reviewed, of which 2 were meta-analyses, 12 were prospective cohorts, 3 were retrospective cohorts, 2 were surveys, and 9 were laboratory studies. Moreover, laboratory and cohort studies indicate that the R1 side chain, not the β-lactam ring, is responsible for this cross-reactivity. The authors conclude that the overall cross-reactivity between penicillin and cephalosporin is lower than previously reported, at 10%, although there is a strong association between amoxicillin and ampicillin with first and second generation cephalosporins that share a similar R1 side chain. The overall cross-reactivity between penicillin and cephalosporin in individuals who report a penicillin allergy is approximately 1% and in those with a confirmed penicillin allergy 2. For penicillin-allergic patients, the use of third or fourth generation cephalosporin or cephalosporins (such as cefuroxime and ceftriaxone) with 45 dissimilar side chains than the offending penicillin carries a negligible risk of cross allergy. The relative risk of an anaphylactic reaction to cephalosporin ranges from 1:1,000 to 1:1,000,000 47 and this risk is increased by a factor of 4 in patients with a history of penicillin allergy. Based on an analysis of 9 articles that compare allergic reactions to a cephalosporin in penicillin-allergic and non-penicillin-allergic subjects, Pichichero et al. In a retrospective cohort of 2,933 patients who received a cephalosporin (usually cefazolin) during their procedure, including 413 who were allergic to penicillin, only one of the penicillin allergic patients may have had an allergic reaction to the cephalosporin; and one of the non penicillin-allergic patients developed a rash while the antibiotic was infused, requiring 48 discontinuation of the antibiotic. In a large, retrospective review of 534,810 patients who received penicillin followed by a cephalosporin at least 60 days later, Apter et al. Eighty-five patients with a history of penicillin allergy and positive penicillin skin test and 726 63 patients with a history of penicillin allergy and a negative penicillin skin test were administered a first generation cephalosporin. Five (6%) of 85 cases had an adverse drug reaction to cephalosporin compared to 5 (0. The rate of presumed IgE-mediated adverse drug reactions to the cephalosporin among the cases was 2 50 (2%) of 85 compared to 1 (0. Question 7: Is there evidence to support the routine use of vancomycin for preoperative prophylaxis? Delegate Vote: Agree: 93%, Disagree: 6%, Abstain: 1% (Strong Consensus) Justification: Current data suggest that the role of vancomycin in orthopaedic surgery prophylaxis should be limited. There is ample evidence that vancomycin is inferior against methicillin-sensitive strains of staphylococcal species when compared to cephalosporin and 8, 53 penicillinase-resistant penicillin. Several systematic analyses concluded that no clear benefit in clinical or cost effectiveness has been demonstrated for the routine use of vancomycin compared with cephalosporin for prophylaxis. The choice of drug prophylaxis should take into account the antibiotic resistance patterns in hospital systems. Thirty-three of the 194 infections were diagnosed within a month after the surgery. In a study of deep infections following hip and knee arthroplasty over a 15-year period at the Royal Orthopaedic Hospital and Queen Elizabeth Hospital in England, 22 of 75 hip and knee infections (29%) were caused by microorganisms that were resistant to the antibiotic used for prophylaxis (cefuroxime. The cost-effectiveness review included 5 economic evaluations of glycopeptide prophylaxis. Only one study incorporated health-related quality of 66 life and undertook a cost-utility analysis. A trend toward more methicillin-resistant gram-positive infections was observed in the cefazolin group (4. Question 8: Is there a role for routine prophylactic use of dual antibiotics (cephalosporins and aminoglycosides or cephalosporins and vancomycin)? Delegate Vote: Agree: 85%, Disagree: 14%, Abstain: 1% (Strong Consensus) Justification: Clinical studies have used pre and post-intervention periods to assess the effect of switching to vancomycin for surgical prophylaxis in patients undergoing cardiothoracic surgery. Question 9: What should be the antibiotic of choice for patients with abnormal urinary screening and/or an indwelling urinary catheter? There is no evidence either in support of or against proceeding with surgery in this cohort of patients. In a prospective, multicenter study of 362 knee and 2,651 hip arthroplasty cases, the authors reported a deep joint infection rate of 2. Of 1,934 surgical cases (1,291 orthopaedic surgeries) performed at a Veterans Administration hospital, a preoperative urine culture was obtained in 25% (489) of cases. Of these, bacteriuria 71 was detected in 54 (11%) patients, of which only 16 received antimicrobial drugs. Among the 54 patients with a positive urinary culture, treated and untreated patients were compared. These results led the authors to conclude that in this system preoperative urinary cultures were inconsistently ordered and that when they were, they were rarely positive for bacteriuria. However, the same organism was isolated from the urinary tract and hip in only 3 patients. Another retrospective analysis found 57 (55 asymptomatic, 2 symptomatic) of 299 arthroplasty patients had bacteriuria on admission. Question 10: Should the preoperative antibiotic choice be different in patients who have previously been treated for another joint infection? In these patients, we recommend the use of antibiotic-impregnated cement, if a cemented component is utilized. Intraoperatively, frozen section for evidence of acute inflammation was used to guide decisions on whether the procedure was done as a single or staged procedure. Of note, this was one of the two patients that had been treated in a staged manner and additionally had immunosuppressive comorbidities, including rheumatoid arthritis. The 5 year infection-free survival was 73%±10% in the case group compared with 100% in the control group (p=0. Question 11: Should postoperative antibiotics be continued while a urinary catheter or surgical drain remains in place? There is no evidence to support the support the continued use of postoperative antibiotics when urinary catheter or surgical drains are in place. Urinary catheters and surgical drains should be removed as soon as safely possible. Prophylactic antibiotics should be discontinued within 24 hrs of the end of surgery. The medical literature does not support the continuation of antibiotics until all drains or catheters are removed and provides no evidence of benefit when 2 they are continued past 24 hours. The authors reported a lower incidence of urinary retention in the indwelling catheter group (27% vs 52%, p<0. Moreover, patients who had an indwelling catheter for more than 48 hours had a significantly higher rate of bladder infection (35%) than patients who were straight catheterized 99 and/or who had an indwelling catheter for fewer than 48 hours (6%, p<0. Of the 99 patients who completed the study, 14 patients (5 men, 9 women) developed postoperative bacteriuria.
Syndromes
- Sildenafil citrate (Viagra)
- Dangerous heart arrhythmias
- Atherosclerosis
- Wheezing
- Increased risk for tuberculosis
- Clergy
Target Populations All humans are susceptible to scombrotoxin poisoning; however impotence supplements generic sildalist 120mg with amex, as noted erectile dysfunction and premature ejaculation cheap sildalist on line, the commonly mild symptoms can be more severe for individuals taking some medications drugs for erectile dysfunction philippines generic 120 mg sildalist fast delivery, such as the anti tuberculosis drug isoniazid causes of erectile dysfunction in your 20s order sildalist uk. Because of the worldwide network for harvesting erectile dysfunction only with partner order generic sildalist on-line, processing erectile dysfunction due diabetes cheap generic sildalist canada, and distributing fishery products, the impact of the problem is not limited to specific geographic areas or consumption patterns. Several other analytical procedures to quantify biogenic amines have been published in the literature. Decomposition and Histamine – Raw, Frozen Tuna and Mahi-Mahi; Canned Tuna; and Related Species; Revised Compliance Policy Guide; Availability. Department of Health and Human Services, Food and Drug Administration, Center for Food Safety and Applied Nutrition, Office of Seafood. Molecular Structural Data: Histamine produced by growth of certain bacteria and the subsequent action of their decarboxylase enzymes on histidine. Bad Bug Book Foodborne Pathogenic Microorganisms and Natural Toxins Tetrodotoxin For Consumers: A Snapshot 1. If the chef or trained cutter doesnt cut the fish in exactly the right way, the poison Poisoning from consumption of may get into the meat of the fish, and the person who eats it members of the family may become ill or even die without immediate medical tetraodontidae (pufferfish) – i. In mild cases of pufferfish poisoning, the person pufferfish poisoning – is one of the who eats it may get numbness and tingling in the lips, arms, most dangerous intoxications from and legs, and may feel light‐headed. In severe cases, death is from suffocation – often awake until the end – because of marine species. There are many types (species) of approximately 185 species of pufferfish, and in most of them, only the organs, not the meat, pufferfish worldwide, and they naturally contain the poison. Other types dont contain any of occur in both freshwater and the poison at all, like the puffer from the mid‐Atlantic waters of marine environments. After a fish has been species, the gonads (mainly ovary), cleaned and processed (for example, turned into fillets or fish liver, intestines, and skin can cakes), it can be hard to tell what kind it is. In a few species, the flesh naturally Only certain parts are allowed, and it has to be prepared by contains enough toxin to be lethal, trained fish cutters before its imported. Because of these strict safety limitations, the availability of this pufferfish Among the numerous pufferfish often is limited, and its often expensive. In some toxin distribution among different cases, unsafe importers have tried to get puffers into the organs within individual fish, can country labeled as different fish. However, toxin falsely labeled as monkfish was imported from China in 2007 presence and distribution does and sickened people who had eaten bok go jim (blowfish appear to be fairly consistent casserole) or bok jiri (blowfish stew) in restaurants. The this chapter provides the popular message to take away from all this is that if you choose to eat and scientific names for 22 species pufferfish, eat only those from sources known to be safe. This list is not comprehensive for all species of pufferfish consumed around the world and is not a recommended list of edible species for consumers in the United States. In Japan, the Ministry of Health, Labour, and Welfare provides strict guidance and regulation for the harvesting and consumption of pufferfish. Under this guidance, the flesh for many of these species is considered safe to consume, if prepared properly by a trained expert so as not to contaminate the fishs flesh with toxin from its other tissues. Today, most poisonings in Japan result from consumption of home-prepared dishes from pufferfish that have been caught recreationally. Authorities in Japan prohibit the use of all viscera from all species of pufferfish, especially the liver and ovaries, for use as food. Regulations vary or do not exist in many of the other Indo-Pacific societies that consume pufferfish. For example, in Taiwan, two species of marine pufferfish, Kurosabafugu (Lagocephalus gloveri) and Shirosabafugu (L. This species has been associated with illness not only in Taiwan, where it has been used accidentally as dried fish fillets, but also in other countries, from which it has been exported under false names, such as monkfish and anglerfish. Tetrodotoxin also has been isolated from other animal species, including newts, tropical gobies, frogs, the blue-ringed octopus, starfish, trumpet shells (gastropods), horseshoe crabs, and xanthid crabs. Although occasionally consumed and associated with illness in other parts of the world, none of these species are imported into the U. Disease Mortality: Death is from respiratory-muscle paralysis and usually occurs within 4 to 6 hours, with a known range of about 20 minutes to 8 hours. After the initial slight oral numbness, the next symptom is increasing paraesthesia in the face and extremities, which may be followed by sensations of lightness or floating. Speech is affected, and the victim usually exhibits dyspnea, cyanosis, and hypotension. Paralysis increases, and convulsions, mental impairment, and cardiac arrhythmia may occur. The victim, although completely paralyzed, may be conscious and, in some cases, completely lucid until shortly before death. Toxin binding to the channel blocks the diffusion of sodium ions, preventing depolarization and propagation of action potentials. In 1983, the Japanese Ministry of Health, Labour, and Welfare enacted guidance for pufferfish harvest and consumption, thereby greatly reducing the number of illnesses and mortalities from commercial product. Most of these illnesses were from home-prepared meals made from recreationally harvested fish. Data for other Indo-Pacific countries are not easily available, but fatalities have been reported from consumption of pufferfish, gobies, trumpet shells, and xanthid crabs. It should be noted that certain pufferfish and xanthid crabs have been shown to also contain additional, potentially lethal toxins, such as saxitoxin and palytoxin (see sidebar. These products must be processed in a certified facility by trained personnel and certified as safe for consumption by the Japanese government. Over the past 50 years, sporadic and isolated cases of pufferfish poisoning, including a few fatalities, involved pufferfish from the Atlantic Ocean, Gulf of Mexico, and Gulf of California. There have been no confirmed cases of poisoning from the northern pufferfish, Sphoeroides maculatus, which was once harvested on the U. A case definition is available from the Centers for Disease Control and Prevention. In Japan, it is prepared and sold in special restaurants, where trained and licensed individuals carefully remove the viscera to reduce the danger of poisoning. Due to its import restrictions and high value, there is potential for intentional mislabeling and illegal importation, particularly of prepared, frozen fish products. The alkali degradation products can also be confirmed as their trimethylsilyl derivatives, by gas chromatography. Mass spectrometry methods have been developed and show good sensitivity and selectivity. To date, none of these chemical methods have been validated for regulatory compliance. The quantity eaten by each person was minimal, ranging from approximately ¼ to 1½ oz. Onset of symptoms began approximately 3 to 20 minutes after ingestion, and all three chefs were transported by ambulance to a local emergency department. Three deaths were reported in Italy, in 1977, following consumption of frozen pufferfish imported from Taiwan and mislabeled as angler fish. In 2007, it was reported that fish sellers in Thailand were selling meat from a highly poisonous species of pufferfish labeled as salmon. For several of the poisonings, the product in question was being sold as bok, a Korean term for pufferfish. Tetrodotoxin – Distribution and Accumulation in Aquatic Organisms, and Cases of Human Intoxication. Examples of puffer species considered safe for consumption in Japan*, including which parts are considered edible. Japanese Scientific Name Edible Part Common Name Muscle Skin Male Gonad Kasafugu Takifugu niphobles Yes No No Komonfugu T. People who choose to consume any species of toxic pufferfish do so at their own risk. A Different Toxin in Some Pufferfish State bans harvesting in certain counties Beginning suddenly in 2002 and extending to 2004, there were 28 cases of pufferfish poisoning from New Jersey to Florida, all of which were linked to southern pufferfish (Sphoeroides nephelus) harvested from the Indian River Lagoon system on Floridas east coast. Saxitoxin and tetrodotoxin have nearly identical pharmacology and generate similar symptoms. The initial source of saxitoxins in this lagoon system is the marine algae Pyrodinium bahamense, which is concentrated by small bivalve mollusks, which, in turn, are consumed by puffers, in whose flesh the saxitoxins accumulate. Since the saxitoxin is in the puffers flesh, no method of preparation can make the puffers from this region safe to consume. Florida southern puffers from outside the Indian Lagoon system have been shown to contain substantially less saxitoxin. The additional co‐occurring puffer species Sphoeroides testudineus (checkered puffers) and S. Since 2004, Florida has banned the harvesting of all puffer species in the east coast counties of Volusia, Brevard, Indian River, St. Updates on the status of the pufferfish harvesting ban in Florida can be found through the Florida Fish and Wildlife Conservation Commission web site. Bad Bug Book Foodborne Pathogenic Microorganisms and Natural Toxins Mushroom toxins: Amanitin, Gyromitrin, Orellanine, Muscarine, Ibotenic Acid, Muscimol, Psilocybin, Coprine 1. Toxins For Consumers: A Snapshot Mushroom poisoning is caused by Some wild mushrooms contain poisons that can cause illness, with symptoms ranging from mild to consumption of raw or cooked fruiting deadly. The poisons are not likely to be destroyed bodies (mushrooms, toadstools) of a by washing, cooking, freezing, or canning. The poisonous wild mushrooms are almost impossible term toadstool is commonly used for to tell apart from those that arent poisonous, and poisonous mushrooms. For individuals many cases of poisoning have happened in people who are not trained experts in mushroom who were using field guides and had a lot of identification, there are, generally, no experience, and were sure they had picked the easily recognizable differences between right kind of mushroom. Folklore notwithstanding, there is no reliable rule of thumb for distinguishing Some of the deadliest wild mushrooms dont edible mushrooms from poisonous ones. Most mushrooms that often start out with symptoms that go away after cause human poisoning cannot be made a few hours and seem to be gone for 3 to 5 days, nontoxic by cooking, canning, freezing, making the person think that he or she is better – or any other means of processing. Thus, but then much worse symptoms appear, often the only way to avoid poisoning is to leading to death. Disease you sick even from eating a sauce that contains them, even if you dont eat the mushrooms Mushroom poisonings are generally themselves. Its much safer to get mushrooms acute, although onset of symptoms may from grocery stores that sell the products grown be greatly delayed in some cases, and are on professional mushroom farms. The normal course of the disease varies with the dose and the mushroom species eaten. Each poisonous species contains one or more toxic compounds that are unique to few other species. Therefore, cases of mushroom poisonings generally do not resemble each other, unless they are caused by the same or very closely related mushroom species. Almost all mushroom toxins may be grouped into one of the four categories outlined below. Because the chemistry of many mushroom toxins (especially the less deadly ones) is still unknown, and identification of mushrooms is often difficult or impossible, mushroom poisonings are generally categorized by their physiological effects. A broad overview of the four categories appears below, including a table that summarizes the onset time of symptoms after these poisons are ingested, likely mushroom sources, and likely outcomes. This information is followed by a section containing more detailed descriptions, which includes a miscellaneous category. The protoplasmic poisons are the most likely to be fatal, due to irreversible organ damage. Victims who are hospitalized and given aggressive support therapy almost immediately after ingestion have a mortality rate of only 10%, whereas those admitted 60 or more hours after ingestion have a 50% to 90% mortality rate. However, some of the deadliest mushrooms do not result in symptoms until 6 to 72 hours after ingestion. Some result in symptoms that appear to resolve after a few hours, but, 3 to 5 days later, more serious symptoms begin that often end in death. Life‐Endangering Poisons – the following classes of poisons are generally not life‐ threatening, although death is possible in severe cases in which large amounts were consumed or the patient has additional health complications;. Observation of patients should continue and appropriate support therapy should be provided, as indicated. Symptomatic diagnoses of mushroom poisonings Onset Rapid (15 minutes to 2 hours after ingestion) Symptoms Cause Prognosis Nausea and abdominal Unknown toxins from Generally, rapid and complete discomfort, sometimes with numerous genera recovery; serious cases may last 2 diarrhea and vomiting to 3 days and require fluid replacement Profuse, prolonged sweating, Muscarine from Clitocybe or Generally, complete recovery tearing (lacrimation), salivation Inocybe spp. Poisoning by the amanitins is characterized by a long latent period (range 6 to 48 hours, average 6 to 15 hours), during which the patient shows no symptoms. Symptoms appear at the end of the latent period in the form of sudden, severe seizures of abdominal pain, persistent vomiting and watery diarrhea, extreme thirst, and lack of urine production. If this early phase is survived, the patient may appear to recover for a short time, but this period generally will be followed by a rapid and severe loss of strength, prostration, and restlessness caused by pain. The disease is progressive and causes irreversible liver, kidney, cardiac, and skeletal-muscle damage. Death may occur within 48 hours (large dose), but the disease more typically lasts 6 to 8 days in adults and 4 to 6 days in children. Two or three days after the onset of the later phase of the disease, jaundice, cyanosis, and coldness of the skin occur. If recovery occurs, it generally requires at least a month and is accompanied by enlargement of the liver. Poisoning by this toxin superficially resembles Amanita poisoning, but is less severe. There is generally a latent period of 6 to 10 hours after ingestion, during which no symptoms are evident, followed by sudden onset of abdominal discomfort (a feeling of fullness), severe headache, vomiting, and, sometimes, diarrhea. The toxin affects primarily the liver, but there are additional disturbances to blood cells and the central nervous system. Poisonings with symptoms almost identical to those produced by Gyromitra also have been reported after ingestion of the Early False Morel (Verpa bohemica. The toxin is presumed to be related to gyromitrin, but has not yet been identified.
Purchase sildalist 120mg free shipping. Performance Enhancing Drugs.
References
- Levy R, Benson R, Winstein C, et al., editors. Cortical stimulation for upper-extremity hemiparesis from ischemic stroke: everest study primary endpoint results. New Orleans, LA: International Stroke Conference; 2008.
- Nogales V, Reinhold WC, Varma S, et al. Epigenetic inactivation of the putative DNA/RNA helicase SLFN11 in human cancer confers resistance to platinum drugs. Oncotarget 2016;7(3):3084-3097.
- Available at http://www.cdc.gov/std/treatment/2006/updatedregimens (Centers for Disease Control website, Atlanta GA, USA 2010). 4.
- Staehelin L, Chalpowski F, Bonneville M: Luminal plasma membrane of the urinary bladder: 1. Three-dimensional reconstruction of freeze-etch images, J Cell Biol 53(1):73n91, 1972.