Lingye Chen, MD
- Medical Instructor in the Department of Medicine
https://medicine.duke.edu/faculty/lingye-chen-md
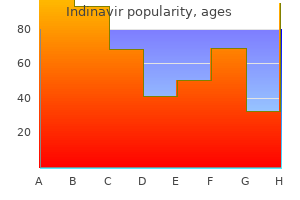
Hypertriglyceridemia-induced acute pancreatitis-treatment with heparin and insulin 94 medications that can cause glaucoma best purchase for indinavir. Heparin and insulin in the treatment of hypertriglyceridemia-induced severe acute pancreatitis medicine q10 cheap 400 mg indinavir overnight delivery. Biphasic effects of low-molecular weight and conventional heparins on chylomicron clearance in rats medicine vs surgery order genuine indinavir on-line. Lower plasma levels of lipoprotein lipase after infusion of low molecular weight heparin than after administration of conventional heparin indicate more rapid catabolism of the enzyme medicine 834 purchase 400 mg indinavir with visa. Decreasing the plasma triglyceride level in hypertriglyceridemia induced pancreatitis in pregnancy: a case report symptoms zinc deficiency adults generic indinavir 400 mg visa. Pancreatitis may occur with a normal amylase concentration in hypertriglyceridaemia medicine while breastfeeding purchase indinavir 400 mg with mastercard. Opportunities in somatostatin research: biological, chemical and therapeutic aspects. Hypertriglyceride Induced Acute Pancreatitis 277 [142] Taniyama Y, Suzuki T, Mikami Y, Moriya T, Satomi S, Sasano H. Systemic distribution of somatostatin receptor subtypes in human: an immunohistochemical study. Somatostatin type 2A receptor immunoreactivity in human pancreatic adenocarcinomas. Microinjection of exogenous somatostatin in the dorsal vagal complex inhibits pancreatic secretion via somatostatin receptor-2 in rats. Changes in somatostatin receptor expression of the pancreas and effectiveness of octreotide in rats with acute necrotizing pancreatitis. Characterization of somatostatin receptor subtype-specific regulation of insulin and glucagon secretion: an in vitro study on isolated human pancreatic islets. Hypertriglyceridemic acute pancreatitis during pregnancy: prevention with diet therapy and omega-3 fatty acids in the following pregnancy. Prescription omega-3 fatty acid as an adjunct to fenofibrate therapy in hypertriglyceridemic subjects. Therapeutic plasma exchange in patients with severe hypertriglyceridemia: a multicenter study. Guidelines on the use of therapeutic apheresis in clinical practice: evidence-based approach from the Apheresis Applications Committee of the American Society for Apheresis. Dietary medium-chain triacylglycerol prevents the postprandial rise of plasma triacylglycerols but induces hypercholesterolemia in primary hypertriglyceridemic subjects. High-monounsaturated fatty acid diets lower both plasma cholesterol and triacylglycerol concentrations. Effect of fibrates on lipid profiles and cardiovascular outcomes: a systematic review. Relapsing acute pancreatitis induced by re-exposure to the cholesterol lowering agent bezafibrate. Efficacy and safety of rosuvastatin and fenofibric acid combination therapy versus simvastatin monotherapy in patients with hypercholesterolemia and hypertriglyceridemia: a randomized, double-blind study. Triglycerides and atherogenic dyslipidaemia: extending treatment beyond statins in the high-risk cardiovascular patient. Effects of prescription omega-3-acid ethyl esters on non-high-density lipoprotein cholesterol when coadministered with escalating doses of atorvastatin. Role of n-3 fatty acids in the treatment of hypertriglyceridemia and cardiovascular disease. Dose-response effects of omega-3 fatty acids on triglycerides, inflammation, and endothelial function in healthy persons with moderate hypertriglyceridemia. In many cases, these anatomic entities can be succesfully treated with radiological interventional methods. It is difficult to correctly interpret the articles that review the treatment of numerous patients because the nomenclature is unclear. The acute fluid collection usually develops around the pancreas but sometimes emerges in the glandular area and does not contain a high quantity of necrosis. Not rarely, it spreads into the chest, mediastinum and/or into the pararenal area. The rich pancreatic enzyme content of the fluid can indicate communication with the pancreatic duct or indicate parenchymal necrosis. They do not have definite walls, and are limited by the walls of the surrounding organs. In a significant number of cases (about 30-50%), spontaneous resolution occurs without surgical or other intervention. If they do not show tendency towards resolution, they can become of significant size and cause clinical symptoms or complications [5,6,33,44]. The most frequent complaints caused by a big, 8-15 cm size acute fluid collection are pain, tension, and increasing abdominal pressure which can significantly worsen the efficiency of breathing [1,9]. In other cases they can cause compression symptoms (jaundice, duodenal obstruction) or bleeding can develop inside of them. The number of acute fluid collections correlate to the severity of the pancreatitis, the length of hospitalization and mortality [19]. Even today the treatment of acute peripancreatic fluid collections is not totally clear. In a small sized fluid collection, conservative treatment (naso-jejunal feeding, the resting of pancreas) is usually effective. The authors do not recommend surgical treatment in the early phase of the illness because of the high morbidity and mortality rates. With the development of interventional radiology and manipulative laparo-endoscopy there are other possibilities to evacuate these fluid collections without operation [1,6,11,14,21,25,35,40,44]. For the treatment of sterile fluid collection percutaneous puncture and drainage are widely applied. It is disputed whether repeated punctures or drainage is the most suitable for the treatment of fluid collections. There are some who are satisfied with the clearing of the fluid collection with only one or repeated punctures in sterile cases. However, this is succesful only in a few cases and drainage or surgical intervention follows [6,28,40,44]. According to those who are pro drainage in the treatment of sterile acute peripancreatic fluid collections, drainage can be applied effectively [1,3,4,14,21,25,34,35,40,44]. Those who are against drainage treatment claim that it is the treatment itself which causes the dreadful complication, the infection of the fluid. According to the literature the rate of iatrogenous infection is about 8-27% [12,25,28,40]. To determine the correct rate of iatregenous infections treated without drainage or puncture a prospective randomized trial should be performed which is not available at this time. With regard to the management of infected acute peripancreatic fluid collections, views are not as varied in these cases: percutaneous drainage is suggested [1,5,8,18,21,22,25,33,34]. Surgery can often be avoided by drainage treatment, and in other cases the intervention is suitable for delaying operative treatment. In such cases, when drainage is not effective, operation is suggested [5,6,8,18,21,22,25,34,35,44]. These cases are equivalent to the pathological entity accepted in the modified Atlanta Classification as postnecrotic peripancreatic/pancreatic fluid collection and walled off pancreatic necrosis. According to other authors the evacuation of necrosis and fluid collection is possible with the help of irrigation through 14-30 F bore drains. For such treatment more catheters should be placed in the cavity [5,10,11,12,18,21,26,29,33,36,38,43]. More than 20% of the patients treated with the minimal invasive method recovered without operation. Necrosectomy during operation is the suitable method in cases of unsuccessfully treated patients [3,6,10,11,12,22,24,26,28, 33,34,36,43]. It often develops in the area of an earlier acute fluid collection which did not show any tendency to resolution. The wall of the pseudocyst contains inflammatory tissues but is not covered by epithelium. It develops most frequently in the environment of the pancreas but mediastinal or pelvic appearances are also known. About 4 weeks are needed for the development of the mutation from the beginning of the disease. Its content is usually sterile but sometimes bacteria can be detected without any clinical manifestation, in other cases it contains pus [5]. Almost 50% of acute pseudocysts do not cause any clinical symptoms and show spontaneous absorbing susceptibility. Especially smaller pseudocysts that are not bigger than 4-6 cm, recover with conservative treatment (eg: naso-jejunal feeding) [18,33,37]. In its cavity pseudoaneurysm can develop which can cause fatal bleeding [2,6,11,14,28,33,37]. In those cases where compressive or respiratory complications or pain develop, surgery or less burdensome percutaneous drainage gives an opportunity for treatment, allowing for the descent of the fluid as well as its bacterological examination [3,4,6,8,11,18,24,33,35]. More drains can be placed in cases of multiple pseudocysts [11,18,35] Operation can be avoided in cases treated this way and drainage can lead to complete recovery, in other cases it is suitable for delaying the time of operation [3,4,6,8,11,18,37,43]. In those cases where the cyst cavity communicates with the Wirsung ductal system, external drainage is not effective. The infected pseudocyst appears as a pancreatic abscess in the late phase of severe acute pancreatitis, at least 4 weeks after the beginning of the disease and needs radiologic 282 Acute Pancreatitis intervention or surgery in each case. It does not contain a considerable quantity of necrotic tissue mass in opposition to the infected liquified necrosis (Post-necrotic Pancreatic Fluid Collection, Walled-off Pancreatic Necrosis). Surgery in these cases involves a lower rate of morbidity and mortality than those performed in the early phase of pancreatitis. Percutaneous drainage treatment can be applied in cases of pancreatic abscess with good results and it can be suggested as the first intervention [4,5,6,8,18,20,29,33,37,38,43]. It is important to carry out bacterological analysis from each abscess one by one because different types of bacteria can be cultured from them. The catheter with the main wire is led into the fluid collection and following verification of its placement the wire is removed (Figure 1-2). The indication of the location and function is that a proper quantity of fluid appears. If there is an abscess, the thicker (14-30F), otherwise the thinner (8 10F), pig-tail catheter is to be used [1,6,8,10,11,12,21,32,36,39]. More drains can be inserted at a time if necessary [5,8,10,11,12,18,21,32,33,35,39,42,44]. If the sterile fluid becomes thickened or purulent, it signifies bacterial infection. If pus appears or the fluid is dense, the irrigation of the cavity is also possible [1,10,11,21,42,44]. Ultrasound examination is the most suitable for the observation of the size of the fluid collection. The cavity filled with contrast material can be well demonstrated and is apt for showing fistulae [1,6,10,11,42,44]. More than 20% of patients (20-50%) recover without surgery, by drainage treatment. If the drained cavity does not decrease during drainage or the septic state does not show a tendency towards resolution, surgical treatment is indicated. In such cases with the application of drainage early operation can be avoided [1,4,6,8,10,11,12,21,26,32,35,39,42]. In an experienced hand the rate of iatrogenic injuries are negligible, less than 2%, generally the injury of the surrounding organs, bleeding can be noticed [1,4,11,12,21,32,35,39,44,]. Sometimes the drain can get clogged or slip out, then its replacement is required [8,35,42,44]. The Role of Percutaneous Drainage in the Treatment of Severe Acute Pancreatitis on the Basis of the Modified Atlanta Classification 283 Fig. More and more authors in selected patients use this method for necrosectomy with a successful rate of 73-92% [2,7,13,15,27,30,31,41]. This procedure must be repeated till the complete emptying of the necroma [7,13,27,30,31]. After the necrectomy it is essential to drain the cavity with pigtail catheters, or stents [13,41]. This method is a possible therapy before or instead of surgery [2,7,13,27,30,31,41]. In well selected cases percutaneous drainage with appropriate caliber drains and supplementary therapy in the greater part of cases leads to complete recovery. References [1] Ai X, Qian X, Pan W, Xu J, Hu W, Terai T, Sato N, Watanabe S: Ultrasound-guided percutaneous drainage may decrease the mortality of severe acute pancreatitis. Therapy should be initiated at the lowest recommended dose and gradually increased. Dosage recommendations for pancreatic enzyme replacement therapy were published following 1,2,3 the Cystic Fibrosis Foundation Consensus Conferences. The Conferences recommend doses of 2,000 to 4,000 lipase units in infants up to 12 months. Patients may be dosed on a fat ingestion-based or actual body weight-based dosing scheme. Infants (up to 12 months) Infants may be given 2,600 lipase units per 120 mL of formula or per breast-feeding. Children Older than 12 Months and Younger than 4 Years Enzyme dosing should begin with 1,000 lipase units/kg of body weight per meal for children less than age 4 years to a maximum of 2,500 lipase units/kg of body weight per meal (or less than or equal to 10,000 lipase units/kg of body weight per day), or less than 4,000 lipase units/g fat ingested per day.
Eldryd got in touch with Humphrey because he knew of his interest 25 medications to know for nclex cheap indinavir 400 mg, and his specialism in internal medicine medicine klimt indinavir 400mg with amex. One of the problems they had when developing the clinical curriculum was that nobody had really talked to the hospitals or to the clinical staff about medical students coming to learn medicine in their hospitals treatment 2015 generic 400mg indinavir visa, so we had to spend a lot of time talking to people and trying to explain why this was needed and how we could collaborate symptoms 0f brain tumor cheap indinavir generic. And then symptoms hyperthyroidism purchase indinavir online from canada, eventually medicine used for anxiety safe indinavir 400mg, all that started to work and the students went to the hospitals and it all did start happening. I was put in touch with the Medical Schools in Kathmandu, and I went over two or three times to teach there, mainly genetics, to try and set up links. Everyone was terribly enthusiastic but when you went away they disappeared into a puff of air. We went to Mumbai and we went up north as well giving mainly cancer genetics courses and things. And we met this chap Rajiv Sarin, who then invited us over another time to run a cancer genetics course. There is a very good centre there in Mumbai, a fantastic lab, really brilliant students, very high quality stuff. But the ones that are beginning to be pushed up in the news, and if you do happen to get your saliva tested by 23andMe, you end up with a whole lot of these very minor genetic variants each with small effect but which may be additive. They have quite a lot of nous to be able to set up potential guidelines for screening for Peutz-Jeghers syndrome or polyposis or the rare diseases. And then understanding then the way tumours develop and all this new stuff now with Mike Stratton showing that different tumours of the same type are completely different from each other. Once you get an idea about how the cancers develop and why they are initiated then you can get better ideas on how to treat them. There are lots of different genes that affect your susceptibility to things, which are of lower penetrance. I think some of the tests may be relatively easy to develop once we know what they are. He is a Fellow of the Royal College of Physicians and Surgeons of Canada, and a Fellow of the Canadian College of Medical Genetics. Patrick MacLeod: I came to consciousness on a beach on a small island on the west coast of Vancouver towards the end of the Second World War. My father was an anti-submarine pilot in the Royal Canadian Air Force, and Japan had been launching fre balloons from submarines hoping to start forest fres in British Columbia. When they realised that there were 300 forest fres in British Columbia that nobody fghts, the Japanese had plan B, they moved progressively down into the States, and these anti-submarine bases moved onto Vancouver Island. My mum and dad had three more children, my sister, my middle brother and my younger brother. I went through the traditional boy scouts, air cadets type of thing, and eventually went into the regular Air Force to fy for a couple of years as a jet navigator. I was a problem child in Grade 3, I know that the nuns had me sit outside the classroom. My mum being a teacher negotiated, next thing I know I go back to school in Grade 5. I went off to do an internship in the States in New Hampshire, at Dartmouth Medical School, because it was a two-year programme that had extensions to the Boston circle * Edited passages from the interview conducted by Professor Tilli Tansey, 6 June 2015, in Glasgow. Then I got this career path change from neurosurgeon to paediatric something or other. In the United States, in that period of time, the National Foundation for the March of Dimes was collecting dimes to cure polio. Once the Salk and Sabin story was played out, the effective vaccines for polio, they were going to dismantle this. They also made available training scholarships and things like that, so when I got to Montreal I must have qualifed for a birth defects fellowship in paediatrics. There was no formal curriculum for medical genetics, you just learned on the job and followed your interests, and serendipity has come to town on many occasions: things have just fallen into my lap without any effort at all, and helped that. I graduated from the University of British Columbia with a career path in neurosurgery, and along the way I met a man at my internship who dissuaded me from being a surgeon. So I had two options as far as he was concerned: I could go to Boston or I could go to Montreal. We lived in central Vancouver and the family doctor did house calls and night calls. There was always this pastoral component, I guess, from the nuns and everything else. Because when I was a boy in frst year medicine we had 30 hours of lectures, labs, a week. The beautiful thing about being a medical geneticist is that the system gives you 90 minutes per patient. Wonderful chunk of time, and you can get so much more done in that sense, you knowfi And I began to look at the fact that every time you went up on the ward there was some mother who was caring for a baby with croup or something, and you could just know that she just struggles a bit.
In borderline resectable cancer 2c19 medications buy cheap indinavir 400mg on line, the cancer is Tests found only in the pancreas but might involve nearby blood vessels or structures symptoms at 4 weeks pregnant order indinavir 400mg visa. When the Consider testing at a hospital or cancer tumor is wrapped around part of the hepatic center that treats more than 15 to 20 people artery treatment hiatal hernia order indinavir without prescription, superior mesenteric artery 911 treatment purchase indinavir 400mg otc, or superior with pancreatic cancer each year symptoms 8 weeks pregnant order indinavir 400mg. Tests for mesenteric vein symptoms 3 days after embryo transfer 400mg indinavir with visa, and there is risk for a positive borderline resectable pancreatic cancer with no margin, then surgery might not be the best option. Surgery should only be used as primary Treatment cannot start without a biopsy to treatment if a team of doctors agree the cancer confrm cancer. A Neoadjuvant treatment core biopsy removes a larger sample of tissue using a wide, hollow needle. Once a biopsy confrms pancreatic cancer, then you will begin neoadjuvant treatment. During surgery, your doctor may fnd that fi If you have a borderline resectable the cancer has spread too far and cannot be pancreatic cancer, you might have fully removed. While you are in the operating Neoadjuvant treatment might be followed room, the doctor may still perform a biliary by chemoradiation. Cancer that involves nearby fi Adjuvant treatment is based on whether blood vessels or other structures that prevent it the tumor was removed during surgery. Cancer that has spread outside the pancreas to distant sites in the body is called metastatic pancreatic cancer. The goal of treatment for locally advanced pancreatic Tests cancer is to stop the cancer from growing and spreading. Tests that are recommended for locally advanced pancreatic fi Clinical trial (preferred) cancer are found in Guide 13. Germline testing will show When frst-line treatment does not stop the if you have any of these mutations. Germline growth or spread of cancer, then a second testing is recommended for anyone with treatment might be an option. For second-line therapy options for locally advanced pancreatic fi Capecitabine cancer, see Guide 16. Talk with your doctor therapy for second-line treatment, no options about what you want from treatment. Other options are available, but systemic therapy options are those that have it depends on many factors. Together, you and Before beginning treatment for the cancer, your doctor should choose a treatment your doctor will frst test for and treat jaundice. Jaundice is a yellowing of the skin and eyes caused by a buildup of bilirubin in the body. It Metastatic pancreatic cancer is cancer that has is a digestive fuid made in the liver. Metastatic tumors are formed when cancer cells spread A tumor in the pancreas can cause jaundice by through the blood or lymphatic system to sites blocking the bile duct that drains bilirubin out or organs that are far away from the pancreas. To relieve symptoms of jaundice, your doctors will place a stent in the bile duct the goals of metastatic pancreatic cancer to relieve the blockage in your bile duct. You treatment are: will not need a stent if you had a biliary bypass during a previous surgery or laparoscopy. The frst-line therapy options for metastatic pancreatic cancer are shown in fi Systemic therapy or Guide 19. Second-line treatment is fi Systemic therapy the next set of treatments given to control the cancer when the frst or previous treatments fi Radiation therapy failed to stop cancer growth. You doctor will Followed by: choose a diferent type of systemic therapy than you had before. You can always if you choose to go with systemic therapy for decide not to continue with systemic therapy. My heart is with all the families who fi A clinical trial is the preferred frst-line are facing this diffcult cancer. If you run into trouble In shared decision-making, you and your having records sent, pick them up and doctors share information, discuss the options, bring them with you. Tell Support groups often include people at your doctors your goals and concerns about diferent stages of treatment. What are the chances you can remove all of the tumor and I will have a negative marginfi How will my age, performance status, cancer stage, and other health conditions limit my treatment choicesfi A test that uses x-rays from many angles to make a picture of the inside of the body. A yellow-brown substance that is removed from blood by the liver and is part of bile. Surgery to re-route the path that eaten food takes from the stomach to the small intestine, celiac plexus neurolysis which absorbs nutrients from food. Use of a thin needle to remove a small amount locally advanced pancreatic cancer of tissue or fuid from the body to test for cancer Cancer that started in the pancreas and has cells. No A small tube in the pancreas that digestive treatment is given during this time. Surgery to remove the widest part (head) of superior mesenteric vein the pancreas and parts of other nearby organs. A tube inserted through a cut in the abdomen supportive care and placed into the stomach to give food. Lurie Comprehensive Omaha, Nebraska Cancer Center of Northwestern Stanford Cancer Institute 800. The incidence of acute pancreatitis does not depend on the diagnosis is usually made based on the increase in gender or race and it is very rare in children. In adults, the pancreas volume and on the changes in structure detected incidence increases in the case of alcohol consumption and on the ultrasound examination. There are Acute pancreatitis complications ultrasonography cases with a single episode of the disease and cases in fluid collections Doppler ultrasonography which relapses occur (4). The aetiology of acute pancreatitis is biliary or alcoholic Rezumat in over 70% of the cases (6). Less frequently, it can be caused by endoscopic procedures (retrograde endoscopic Pancreatita acuta este o afecfiiune relativ frecventa, cu cholangiography), abdominal trauma, surgery with pancreas potenfiial de severitate crescut. Acute pancreatitis may investigafiie imagistica utilizata pentru evaluarea severitafiii occur after drug consumption or during pregnancy. Diagnosticul se formuleaza pe baza crefiterii in children, the aetiology may be of traumatic, infectious or volum a pancreasului fii modificarilor de ecostructura. The diagnosis of acute pancreatitis is made clinically (according to severity and complications fi severe epigastric pain radiating to the back, profuse sweating, vomiting, Introduction intestinal obstruction, shock, fever, etc. The histological changes may be more frequently used for the same reason, ultrasound examinations represent the first imaging diagnostic methods Romanian Journal of Gastroenterology March 2005 Vol. It Clinica Medicala 3 permits pancreas visualisation in about 75 fi 93% of the Str. The external examination is the most mesenteric structures (blood flow anomalies, collections or frequently used. The investigation consists of obtaining enzyme collections are present; study of the large cavities transverse or oblique sections of the epigastric region by delimited by serous membranes (the peritoneum, the pleurae, mildly changing the transducer angle caudally. The the pericardium); description of the collections and transhepatic approach is used in examining the head of the evaluation of size; pancreas; the transplenic approach is used for the d. Administration of the disease (portal vascular system, gastroduodenal artery); gaseous water may improve the image by creating an optimal. Using this technique, tubular-hollow organs that may influenced or may be the whole pancreas including the tail part can be visualised. It has a the diagnosis of acute pancreatitis includes: the homogeneous structure and it is somewhat more echogenic increase in the volume of the pancreas region, structural than the neighbouring liver parenchyma. It is well delimited changes in the parenchyma and significant decrease in being separated by the peripancreatic fat which has an echoes. The increase in volume is assessed qualitatively by intensely echogenic appearance. Anteriorly it comes into noting the displacement of abdominal organs (especially contact with the stomach whereas posteriorly it comes into the stomach and the transverse colon) and quantitatively contact with the splenic vein, the superior mesenteric artery by measuring the anteropostrior diameter at the level of the and the large retroperitoneal vessels (the aorta, the inferior pancreas body. The anteroposterior diameter of the pancreas well as a marked anterior convexity of the pancreas does not exceed 20 fi 22 mm. Wirsungfis duct fi a tubular corresponds to a pathological increase in volume of the structure below 2 mm in diameter can be seen in the middle gland, a fact that is associated with oedema (Fig. Depending on the amount of hypertrophy, a bulging of In characterising the normal pancreas the following the anterior abdominal wall can be noted. In massive oedema there is marked pancreas form, echogenity and size which depend on the hypoechogenity of the pancreas region (Fig. The diagnosis of complications in acute pancreatitis Due to existing technology, the pancreas ultrasound includes: identification of peripancreatic collections, areas allows for the wide evaluation of the retroperitoneal and of necrosis, areas of superinfection, identification of even of the whole abdominal region. Their delimitation may blood to the pancreas, liver, gall bladder and at the level of be indefinite or irregular fi in the case of recent collections fi the large abdominal vessels. They may have a combined with invasive diagnostic procedures (mainly, peripancreatic location fi between the pancreas and the aspiration puncture) and therapeutic ones (ultrasound and/ stomach (Fig. Other diagnostic imaging techniques will accumulation in the right or left pleuro-costal sinus (Fig. The anteroposterior diameter at the level of the pancreas appearance is that of a prolonged, transonic formation located head, body and tail is increased. Collections can also be identified in the fat composing peritoneal space along the colon, at the level of the parieto the mesentery as well as in the fat located in the retro cholic grooves (Fig. The following aspects should be considered: sometimes communicate through fistulous routes, which a. More than four collections corresponding to a high level of oedema and, thus, to a located in different parts of the abdomen and/or in the resorption potential. The presence of echoes in the form of pleurae represent a rate of superinfection of over 50% (1,5); membranes within these collections may suggest a haematic. Their resorption is slow, over weeks or However, parenchymal necrosis may be suspected when months, and characterised by a tendency of pseudotumoral there is an area of hypoechogenity in the pancreatic region organisation; associated with capsule deformation (Fig. In febrile patients not detected within a diffuse exacerbation of blood flow at the responding to therapy such as an ultrasound pattern require level of the pancreatic region. They 6 weeks in the form of a pseudocyst which occurs in 2-7 % 88 Badea of all acute pancreatites (1). The pancreatic pseudocyst re delimited by the presence of peripancreatic inflammatory presents a space replacing structure having 2 mm-thick walls tissue with variable volume which do not respond to treat and a transonic content (Fig. The presence of echoes ment and which are located peripancreatically, sometimes inside it is equivalent with sequestra resulting from the towards the anterior abdominal wall (Fig. The suspicion of infected Relationship with other diagnostic methods collection should be raised clinically, relating to the presence of a septic syndrome not responding to therapy. Another element of alarm is repre of the abdominal cavity have to be detected or when the sented by changes in the ultrasonographic character. However, this method also aspiration puncture with cultivation on culture media has important advantages: its portable character (it can be (Fig. The pseudoaneurysm of the relation with the clinical picture and the biochemical data. The clinical clearly delimited, it has a pulsating character, inside haematic picture should guide all further measures to be taken; if clouds looking like a whirl and intense colour Doppler signal. The Doppler explo ration is useful in order to detect thrombosis and to identify References the moment when the circulation becomes portal again either spontaneously or under anticoagulant treatment. Current Treatment Options in Infectious happens in the form of a multi-channel structure with a Diseases 2000;2:294fi306. Arterial vascular indices increase rapidly in acute pancreatitis: an algorithmic approach to identification the case of pancreas rejection. Gastroenterology 2001; Posttraumatic fistulae and collections can be detected 120:708fi717. Etiology and pathogenesis of acute duct or in patients with posttraumatic duct fractures. J Clin Gastroenterol 2000; 30: ultrasonic appearance is that of collections irregularly 343fi356. Congenital Liver, Cyst, Minimally, Invasive, Laparoscopic, Percu cystic lesions include polycystic liver disease, taneous, Drainage, Fenestration. The infec tious cysts are the hydatid cyst, the amoebic ab Introduction scess, and the pyogenic abscess, whereas the non-infectious cysts are neoplastic cysts and Nowadays, technological advances, lower cost, false cysts. Not only are they used possible minimal therapeutic options along with for abdominal symptoms screening but also for their indications and complications. As a result, clarify the role of minimally invasive techniques cystic lesions of the liver are diagnosed more fre in the management of hepatic cysts. Moreover, in the setting of modern imally invasive, laparoscopic, percutaneous, medicine where minimally invasive technics are drainage and fenestration.
Order indinavir 400 mg. New Device for Opioid Withdrawal?.
You may need to use sanitary protection symptoms 3 days after conception indinavir 400mg for sale, but More than 2 medications errors buy indinavir 400 mg,100 women were questioned in a survey of their continue to use NuvaRing as normal treatment with chemicals or drugs order indinavir amex. If it continues symptoms 6 weeks 400 mg indinavir, becomes heavy or starts again treatment 4 burns buy generic indinavir 400 mg line, tell your Nearly all of the women found NuvaRing easy to insert (96%) doctor treatment croup buy discount indinavir. Most women did not feel NuvaRing once it was in place and 83% of women said they never or rarely felt NuvaRing during intercourse. Similarly, 68% of women said their partners never or rarely felt the ring during intercourse, and 91% reported that their partner did not mind them using the ring. For any unexpected fi enlarged abdomen; effects while taking NuvaRing, contact your doctor or fi fatigue; pharmacist. Talk with your Remove the Do not use a NuvaRing if it was dispensed to you more than doctor or pharmacist ring and call 4 months ago. Symptom / effect Only if In all your doctor or pharmacist severe cases Do not use NuvaRing after the expiry date which is shown on the Uncommon box. Reporting Side Effects You can help improve the safe use of health products for Canadians by reporting serious and unexpected side effects to Health Canada. Your report may help to identify new side effects and change the product safety information. Hospitals by Among patients with the most Procedure, 2010 common procedures in U. The highest 30-day Research indicates that nearly one in five Medicare patients readmission rates were for kidney are readmitted to the hospital within 30 days, about 90 transplant (29. For some Protection and Affordable Care Act (Section 3025) mandates procedures, about one in four a hospital readmissions reduction program whereby Medicare patients were readmitted within 30 payments will be reduced for hospitals with excessive 3 days: procedures to create access readmissions. This Statistical rates, patients aged 65 years and Brief provides an overview of 30-day all-payer, all-cause older consistently had the highest readmissions to U. Factors associated with 30-day readmission rates after percutaneous coronary intervention. Rehospitalization following percutaneous coronary intervention for commercially insured patients with acute coronary syndrome: A retrospective analysis. It presents the most comprehensive national estimates on readmissions by procedure that is available to date. In this Statistical Brief, readmission was defined as a subsequent hospital admission within 30 days following an original admission (or index stay) with a major operating room procedure that occurred from January through November 2010. All-cause readmissions were examined; thus, readmissions may or may not include procedures that were listed during the index stay. Appendix A provides detailed information on readmission rates for most procedures performed in U. The table provides information on the number of index stays for each procedure, the number of all-cause readmissions within 30 days, and the percentage of index stays that were followed by a readmission within 30 days for any cause. Excluded were nonspecific procedures and any procedures with fewer than 5,000 index stays or fewer than 500 readmissions. Findings Readmission rates for the most frequent procedures Table 1 lists the 30 most frequent procedures performed in U. The most frequent procedures and their readmission rates were Cesarean section (2. Among the most frequent procedures, as many as one in five patients were readmitted within 30 days. The lowest readmission rates were for procedures related to childbirth and the reproductive organs (Cesarean section, 2. Procedures with the highest readmission rates Table 2 lists procedures ranked by the highest readmission rates. Across all inpatient procedures, 30-day readmission rates reached a high of almost one in three patients for kidney transplant (29. All-cause 30-day readmissions ranked by the most frequent procedures* performed during the index stay, U. All-cause 30-day readmissions ranked by the highest readmission rates for procedures* performed during the index stay, U. The highest readmission rate was seen for patients with an expected payer of Medicare (25. All-cause 30-day readmission rates for amputation of a lower extremity by age and insurance status, U. Readmission rates progressively were higher with advancing age, increasing from 13. All-cause 30-day readmission rates for debridement of a wound, infection, or burn by age and insurance status, U. Readmission rates were identical for patients with an expected payer of Medicare or Medicaid (20. All-cause 30-day readmission rates for heart valve procedures by age and insurance status, U. All-cause 30-day readmission rates for insertion, revision, replacement, removal of cardiac pacemaker or cardioverter/defibrillator by age and insurance status, U. The readmission rate was highest for patients with an expected payer of Medicaid (19. All-cause 30-day readmission rates for coronary artery bypass graft by age and insurance status, U. Overall, across select procedures with high volume (more than 100,000 index stays) and high readmission rates (at least 15 percent), the 30-day readmission rate consistently was higher for patients aged 65 years and older than for younger adults. In terms of payer, patients with Medicare and Medicaid coverage also consistently had higher readmission rates than patients with private insurance or those who were uninsured. These databases include reliable, verified synthetic patient identifiers that can be used to track a person across hospitals within a State. For 2010, readmissions data were available from 18 States: Alaska, Arkansas, California, Florida, Georgia, Hawaii, Louisiana, Massachusetts, Mississippi, Missouri, Nebraska, New Mexico, New York, South Carolina, Tennessee, Utah, Virginia, and Washington. These 18 States are geographically dispersed and account for 46 percent of the total U. The study population in this readmissions analysis file included discharges from community, nonrehabilitation, nonspecialty hospitals. Weights for national estimates were developed using poststratification on hospital characteristics (Census region, urban-rural location, teaching capabilities, bed size, and control/ownership) and patient age groups. Readmissions the 30-day readmission rate is defined as the number of admissions for each procedure for which there was at least one subsequent hospital admission within 30 days, divided by the total number of admissions from January through November 2010. That is, when patients are discharged from the hospital, they are followed for 30 days in the data. If any readmission to the same or different hospital occurs during this time period, the admission is counted as a readmission. No more than one readmission is counted within the 30-day period, because the outcome measure assessed is "percentage of admissions who are readmitted. In the case of admissions for which there was more than one readmission in the 30-day period, the data presented in this Statistical Brief reflect the characteristics and costs of the first readmission. Every qualifying hospital stay is counted as a separate index (starting point) admission. Thus, a single patient can be counted multiple times during the course of the January through November observation period. In addition, index admissions do not require a prior "clean period" with no hospitalizations; that is, a hospital stay may be a readmission for a prior stay and the index admission for a subsequent readmission. Excluded are long-term care, rehabilitation, psychiatric, and alcoholism and chemical dependency hospitals. This categorization includes patients who are dually eligible for Medicare and Medicaid under Medicare. For this Statistical Brief, categorization of readmission counts by expected payer was based on the index stay. Acknowledgments the authors would like to acknowledge the contributions of Marguerite Barrett and Minya Sheng for work on programming. However, the authors, editors, and publisher are not responsible for errors or omissions or for any consequences from application of the information in this book and make no warranty, expressed or implied, with respect to the currency, completeness, or accuracy of the contents of the publication. The authors, editors, and publisher have exerted every effort to ensure that drug selection and dosage set forth in this text are in accordance with the current recommendations and practice at the time of publication. This is particularly important when the recommended agent is a new or infre quently employed drug. This can be done while learning a single section and again while combining the approaches to several body systems or regions into an integrated examination (see Chap. Maneuvers such as the Timed Get Up and Go test are included in the Special Techniques sections in each chapter. For adults, the comprehensive history includes Identifying Data and Source of the History, Chief Complaint(s), Present Illness, Past History, Family History, Personal and Social History, and Review of Systems. New patients in the office or hospital merit a comprehensive health history; however, in many situations, a more fiexible focused, or problem-oriented, interview is appropriate. Record the following conditions as either present or absent in the family: hypertension, coronary artery disease, ele vated cholesterol levels, stroke, diabetes, thyroid or renal disease, cancer (specify type), arthritis, tuberculosis, asthma or lung disease, headache, seizure disorder, mental illness, suicide, alcohol or drug addiction, and allergies, as well as conditions that the patient reports. Also include lifestyle habits such as exercise and diet, safety measures, and alternative health care practices. This allows you to shift to more specific ques tions about systems that may be of concern. Remember to move major health events to the Present Illness or Past History in your write-up. Usual weight, recent weight change, clothing that fits more tightly or loosely than before; weakness, fatigue, fever. Nose and sinuses: Fre quent colds, nasal stuffiness, discharge or itching, hay fever, nosebleeds, sinus trouble. Throat (or mouth and pharynx): Condition of teeth and gums; bleeding gums; dentures, if any, and how they fit; last dental examination; sore tongue; dry mouth; frequent sore throats; hoarseness. Bowel movements, color and size of stools, change in bowel habits, rectal bleeding or black or tarry stools, hemorrhoids, constipation, diarrhea. Intermittent claudication; leg cramps; varicose veins; past clots in veins; swelling in calves, legs, or feet; color change in fingertips or toes during cold weather; swelling with redness or tenderness. Number of pregnancies, number and type of deliveries, number of abortions (spontaneous and induced), complications of pregnancy, birth control methods. Joint pain with systemic features such as fever, chills, rash, anorexia, weight loss, or weakness. For more problem-oriented, or focused, assessments, the presenting complaints will dictate which segments you elect to perform. Chapter 1 | Overview: Physical Examination and History Taking 9 Refect on Your Approach to the Patient. Ask the patient to move toward you if this makes it easier to do your physical examination. It throws contours, elevations, and depressions, whether moving or stationary, into sharper relief. Then roll the patient onto each side to listen to the lungs, examine the back, and inspect the skin. Roll the patient back and finish the rest of the examination with the patient again supine. If acuity is diminished, check lateralization (Weber test) and compare air and bone conduction (Rinne test). Nose and sinuses: Examine the external nose; using a light and nasal speculum, inspect nasal mucosa, septum, and turbinates. Move behind the sitting patient to feel the thyroid gland and to examine the back, posterior thorax, and lungs. In either sex, inspect the axillae and feel for the axillary nodes; feel for the epitrochlear nodes. Use these observations to decide whether a full musculoskeletal examination is warranted: With the patient still sitting, examine the hands, arms, shoulders, neck, and temporomandibular joints. Listen to the breath sounds, any adventitious sounds, and, if indicated, transmitted voice sounds. Observe the jugular venous pulsations, and measure the jugular venous pressure in relation to the sternal angle. Ask the patient to sit, lean forward, and exhale while you listen for the murmur of aortic regurgitation. With the patient supine, palpate the femoral pulses and, if indicated, popliteal pulses. Examine the legs, assessing the three systems (see next page) while the patient is still supine.
References
- Pieper R, Kager L, Nasman P. Clinical significance of mucosal inflammation of the vermiform appendix. Ann Surg 1983;197:368.
- Symbas PN. Autotransfusion from hemothorax: experimental and clinical studies. J Trauma 1972;12:689-695.
- Nordling J, Anjum FH, Bade JJ et al. Primary evaluation of patients suspected of having interstitial cystitis (IC). Eur Urol 2004; 45: 662-9.
- Choi G, Gomersall CD, Tian Q. Principles of antibacterial dosing in continuous renal replacement therapy. Crit Care Med. 2009;37:2268-2282.
- Martin, D. F., Williams, R. F., Mulrooney, T., et al. Ventralex mesh in umbilical/epigastric hernia repairs: clinical outcomes and complications. Hernia. 2008; 12(4):379-383.