Caroline Sanders, BSc Hons, PGD, RCN, RN
- Consultant Nurse,
- Alder Hey Children? Hospital, NHS Foundation Trust,
- Liverpool, United Kingdom
The biloma completely resolved after percutaneous drainage and biliary stent placement antibiotic used for mrsa order omnicef 300 mg line. The collection was found to have markedly elevated bilirubin levels antibiotics for acne after accutane omnicef 300mg online, in keeping with a biloma antibiotic resistance neisseria gonorrhoeae buy discount omnicef on-line. Post-traumatic bilomas occur because of disrupted intrahepatic bile ducts and bile leakage into lacerations/hematomas antibiotics for dogs for uti 300 mg omnicef. Liver transplant bilomas are typically due to hepatic arterial stenoses/thromboses antibiotics review order 300mg omnicef overnight delivery. Biliary ischemia leads to bile duct necrosis antibiotics medicine order 300mg omnicef with amex, sloughing, and intrahepatic bilomas. Multiple ischemic and immunological insults may result in the strictures and casts that are characteristic of ischemic cholangiopathy. Brush biopsies of the stricture were negative, and a liver biopsy showed changes compatible with ischemic reperfusion injury. The patient was taken to surgery where the gallbladder was found to be "avulsed" from its hepatic attachment and leaking bile. Melamud K et al: Biliary imaging: multimodality approach to imaging of other significant injuries that require attention biliary injuries and their complications. The bile leak resolved, and the stent was removed subsequently without complication. Concern about biliary injury prompted transhepatic cholangiography, which showed transection of the distal common bile duct within the pancreatic head, and extravasation of bile. A liver transplant was performed with cholangitis, bilomas, and biliary cirrhosis identified within the explant. An elective laparoscopic cholecystectomy for presumed biliary colic revealed cholesterolosis and cholesterol polyps. While the data suggests nodules < 1 cm harbor a very low risk of malignancy, most society guidelines suggest imaging follow-up. Their small size, echogenicity, multiplicity, and stability at follow-up sonography indicate hyperplastic (cholesterol) polyps. Wiles R et al: Growth rate and malignant potential of small gallbladder 0 No consistent relationship with age, gender, or obesity polyps Systematic review of evidence. Assessment of mobility during real-time examination helps to differentiate between polyps and small, nonshadowing stones or sludge. Although tiny polyps are rarely malignant, ultrasound surveillance is typically advocated. How long and at what interval these small polyps should be followed is controversial. This and the size of the polyp prompted elective cholecystectomy, which revealed a solitary but large cholesterol polyp. If considered resectable, such a cancer would undoubtedly require an extended cholecystectomy with radical resection. In many cases, such as this, the site of origin for the mass can be difficult to determine. Patients with familial polyposis have a substantially increased risk of developing ampullary (and other) carcinomas. While this was a pancreaticobiliary type lesion at histology, individual subtypes of ampullary carcinoma cannot be distinguished on imaging. The coronal plane is usually the best way of visualizing the ampulla and assessing a potential mass. Ampullary carcinoma cannot be easily distinguished from a periampullary duodenal carcinoma at imaging, although surgical treatment for both lesions is the same (Whipple procedure). While a large polyp or gallbladder cancer could also be considered, this was a melanoma metastasis. While this could certainly represent a cholangiocarcinoma, this was a metastasis from colon cancer. Bile duct resection confirmed multiple papillary neoplasms associated with invasive carcinoma. The thinner source images are required for segments develop from the ventral bud, which also gives rise optimal multiplanar reformations. Variations of coronal and sagittal planes frequently make Among the most common is pancreas divisum, in which there peripancreatic nodal involvement and local invasion more is little or no communication between the accessory duct of evident, and may even be essential in recognizing a lesion as Santorini and the main duct of Wirsung that drains the being intra or peripancreatic in origin. Both Approach to the Abnormal Pancreas may simulate serious pathology unless one is familiar with Unlike other abdominal organs, the pancreas has only a thin these normal variants. Processes that originate within the pancreas can substantially within the population based on patient age, body easily spread to adjacent structures, including other viscera habitus, and other factors. In patients over the age of 70, the within the anterior pararenal space, such as the duodenum parenchyma atrophies, often develops small foci of and vertical colon segments. Pancreatitis, for instance, often calcification, and the pancreatic duct dilates slightly. These affects the duodenal lumen and may cause inflammation of signs should not be interpreted as evidence of chronic the descending colon as well. Invasion into the lumen of the splenic Ultrasound may be the first study performed in the evaluation vein, which runs within the pancreas, leads to liver metastases, of abdominal pain. The pancreas, however, is often while occlusion of the splenic vein leads to characteristic incompletely evaluated secondary to overlying bowel gas. If a perigastric varices in the absence of esophageal varices or cystic mass is identified, color Doppler should always be cirrhosis. This may constitute the most obvious sign on performed to rule out a vascular lesion. Pancreatic ductal dilation is most frequently due to masses relative to the normal pancreas, while endocrine (islet ductal carcinoma or chronic pancreatitis, but may also result cell) tumors are hypervascular. Hepatic metastases Obstruction of the intrapancreatic bile duct may result from from endocrine tumors may also be evident only on arterial the same inflammatory and neoplastic processes of the phase images. Since some hypervascular pancreas from primary tumors such as lung, breast, or tumors. Clinical history is necessary, as is Hypervascular Pancreatic Mass consideration of the age, gender, and presence of laboratory Common evidence of pancreatitis. Pancreatic neuroendocrine (islet cell) tumors neoplasms occur almost exclusively in young or middle-aged women, while solid and papillary neoplasms occur in girls and Less Common young women. Pancreatic metastases cystic tumors by imaging alone, but usually occur in patients. Serous cystadenoma, pancreas with known pancreatitis and evolve in size much more rapidly. Epithelial (true) cyst, pancreas result in an intrasplenic pseudocyst and pancreatic ascites. Metastases and lymphoma, pancreas potential pitfall in this area is the accessory spleen, which may. Gastric stromal tumor (mimic) be located within the tail and mimic a hypervascular. As the stomach and duodenum elongate, the ventral pancreas and bile ducts rotate clockwise and posteriorly to fuse with the dorsal pancreas. This results embryologically from failure of fusion of the ducts between the dorsal and ventral pancreatic anlagen. The top image (A) is from a 30 year-old woman and the bottom image (B) is from a 78 year-old man. Further evaluation, including biopsy, confirmed a diagnosis of autoimmune (IgG4-related) pancreatitis. Pseudocysts, unlike cystic pancreatic neoplasms, usually evolve in size quickly, which may aid in distinction. The mass has a "honeycomb" or "sponge" appearance, characteristic of serous microcystic adenoma. This represents an aneurysmally dilated and thrombosed portal vein varix in a patient with severe cirrhosis and portal hypertension. No soft tissue mass was seen and all findings were attributed to chronic pancreatitis. There is no pancreatic ductal dilation and these are considered normal senescent changes. This patient has congenital absence of the dorsal pancreas and has had at least 1 episode of acute pancreatitis. There should normally be pancreatic tissue along the anterior aspect of the splenic vein. There is still a hypoplastic pancreatic body, which demonstrates a characteristic rounded margin? While adults with annular pancreas are usually asymptomatic, this patient was experiencing intermittent obstruction and early satiety. There is no communication with the dorsal duct, compatible with pancreatic divisum. The relationship between the pancreatic and common duct is referred to as the crossing duct sign. The characteristic location and the lack of mass effect on the duct are key findings to suggest the diagnosis of focal fatty infiltration. Note the preserved higher signal and lack of dropout from the normal pancreatic tissue in the uncinate process. Ectopic pancreas can appear homogeneous, heterogeneous, or cystic depending on its internal mixture of acini, ducts, and islet cells. Only 45% of patients with ectopic pancreas will have central umbilication on a barium study. At surgery, extensive infected necrosis of the pancreas was found and a necrosectomy was performed. Notice that the collection is simple in appearance without debris or hemorrhage, compatible with a pseudocyst. Walled-off necrosis, unlike a pseudocyst, often requires either a large bore catheter for drainage, or necrosectomy. The location of necrosis in this case raises concern for "disconnected duct" syndrome. Note the extension of the fluid into the interfascial retroperitoneal space between the perirenal and anterior pararenal spaces and into the muscles of the flank. Endoscopic ultrasound biopsy of the mass revealed adenocarcinoma, which presented as pancreatitis. The presence of a dilated pancreatic duct in acute pancreatitis should always prompt search for an underlying mass. Chronic pancreatitis is a scirrhous process that commonly causes stricture or occlusion of the ducts. The patient underwent Whipple procedure due to concern for malignancy, where this was found to be a fibroinflammatory mass related to chronic pancreatitis. Side branch dilatation can be an early sign of chronic pancreatitis, subsequently confirmed in this patient using endoscopic ultrasound. This was found to be segmental (given pancreatic head involvement) groove pancreatitis at surgery. Initially suspected to represent malignancy, this was found to be groove pancreatitis at surgery. Initially suspected to represent a duodenal malignancy, this was found to be groove pancreatitis at surgery. This was found to be groove pancreatitis at surgery, but the presence of fluid tracking in the retroperitoneum is atypical and more common with acute edematous pancreatitis. While this was suspected to represent groove pancreatitis, Whipple procedure was performed to exclude underlying malignancy, a common outcome in these cases. Groove pancreatitis in the chronic setting, as in this case, can appear very similar to traditional chronic pancreatitis (including the presence of calcifications). Endoscopic ultrasound-guided biopsy of the pancreatic head mass revealed autoimmune pancreatitis. The lack of dilatation of the pancreatic duct was an important clue to the diagnosis. The pancreatic duct in this segment is not identified and there is little surrounding inflammation. Serologic testing (IgG4) suggested the diagnosis of autoimmune pancreatitis and steroid therapy was started. This was thought to likely represent autoimmune pancreatitis, and the patient was found to have elevated IgG4. Secondary signs of injury, such as peripancreatic fluid, hematoma, or fat stranding, are almost always present as a clue to the diagnosis. The pancreatic duct was disrupted, and the body and tail of the pancreas were resected at surgery. The fluid collection developed as a result of leakage of fluid from the site of the transected pancreatic duct. In some patients, retropancreatic fluid is the most conspicuous sign of a pancreatic fracture. The pylorus may be removed or preserved, depending on extent of disease and surgeon preference. This was found to be the result of a hepaticojejunostomy leak, but was treated conservatively with a drain. The patient was taken to angiography where a vascular erosion was found to be the cause of the bleed. The donor iliac artery is anastomosed to the donor superior mesenteric and splenic arteries to perfuse the pancreatic allograft (inset). The venous drainage can be to the iliac vein (as drawn) or the superior mesenteric vein. Note the communication between the fluid collection and the duodenum consistent with suture line dehiscence. At resection, infected necrosis of the pancreatic allograft related to pancreatitis was noted. The mass has a sponge or "honeycomb" appearance and is characterized by innumerable small cysts, a central scar, and no obstruction of the pancreatic or bile duct.
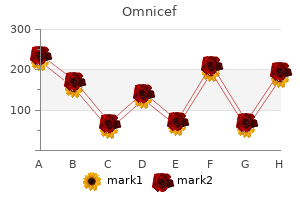
Approximately 5-10% of the cases of acute hepatitis B will become chronic treatment for dogs constipation purchase genuine omnicef line, while in acute hepatitis C infection under eye buy genuine omnicef online, chronicity rate reaches up to 80% of cases (hepatitis C is most frequently anicteric in the acute phase) antibiotics for uti treatment effective 300 mg omnicef. Other causes of chronic hepatitis are autoimmune hepatitis antibiotics for acne and yeast infections cheap omnicef 300mg overnight delivery, drug induced liver disease antibiotic use in poultry purchase omnicef 300mg on-line, cholestatic hepatitis or abnormal metals storage in the liver hemochromatosis (iron) and Wilson disease (copper) virus 86 order discount omnicef online. In patients with chronic hepatitis, etiology (for therapy) and histological staging (for prognosis and therapy) must be established. The clinical signs of chronic hepatitis can be absent, discrete or more rarely noticeable. Chronic hepatitis (both B and C) are to a large extent completely asymptomatic and detected accidentally (most frequently by high aminotransferases levels found during a routine examination). This is why we consider that any patient with increased aminotransferases levels (minimally or slightly increased; even in the event that they return to normal values on a subsequent examination) should be investigated. In Romania, the most frequent cause of increased aminotransferases levels in asymptomatic patients seems to be the infection with the hepatitis C virus (approx. The lack of correlation between the intensity of the physical and intellectual activity and fatigue severity can be a sign suggesting chronic liver disease. Other symptoms in chronic hepatitis are dyspeptic syndrome, exercise or rest hepatalgia, mild jaundice, bleeding gums, purpura, etc. Aminotransferases, the expression of hepatocyte lesion, may increase in all liver disease (however, 1/3 of chronic hepatopathies can evolve with normal aminotransferases). The width or thickness of the spleen is not equally important, but a globulous 11 spleen can be a sign of activation of the reticuloendothelial system. Larger splenomegaly (more than 15 cm) suggests, in a clinical context, liver cirrhosis. It should be emphasized that a normal spleen does not exclude a chronic hepatitis. In a personal study, we aimed to correlate the size of the spleen with the histological activity of chronic hepatitis, but we found only a weak direct correlation (the correlation between the spleen size and Knodell histological score was 0. Ultrasound evidence of hilar adenopathies (lymph nodes of the hepatoduodenal ligament) is relatively common. They can occur in chronic hepatitis B or autoimmune hepatitis, but are extremely frequent in chronic hepatitis C (Fig. Italian studies have reported the presence of adenopathies in the hepatoduodenal ligament in approximately 70% of chronic hepatitis C cases and have monitored the evolution of lymph node size for the evaluation of therapeutic response to interferon. Hilar oval adenopathy in chronic hepatitis C 12 the lymph nodes of the hepatoduodenal ligament are usually oval, 5-10/10-20 mm in size (Fig. Other ultrasonographic signs for chronic hepatitis are non-specific and inconsistent. A discrete hepatic heterogeneity (inhomogeneity) rather suggests liver cirrhosis than chronic hepatitis. The signs of hepatomegaly (particularly the rounding of the caudo-ventral liver margin) are non specific. The thickening or irregular trajectory of the bile ducts are both suggestive signs for cholestatic liver disease (sclerosing cholangitis). Palpation of the liver by an experienced doctor can bring relevant data on the liver size (hepatomegaly) and its consistence. The diagnosis of splenomegaly is made by ultrasound (much more objective than assessment by palpation). The temporal diagnosis (evolution longer than 6 months), and the clinical and biological diagnosis of chronic hepatitis are followed by staging, mandatory both for prognosis and therapy. The biopsy site is localized using ultrasound (avoiding large vascular structures, cysts or hemangiomas), and is usually at the level of the middle axillary line, in the hepatic parenchyma. Some authors use the ultrasound guided technique, in which the needle attached to a pistol is guided into the liver in real time. Ultrasound can be useful for assessing potential complications that can occur during biopsy: hemoperitoneum anechoic or slightly hypoechoic image in the perihepatic space or in the Douglas pouch; subcapsular or intraparenchymal hematoma (anechoic/hypoechoic image under the liver capsule or within the parenchyma). In conclusion, ultrasound examination in chronic hepatitis has a limited value, only splenomegaly and hepatoduodenal ligament adenopathies being relatively constant elements (good sensitivity, but lower specificity). Another etiology is chronic hepatitis C (up to half of the cases have mild steatosis). From a clinical point of view, steatosis most frequently has no subjective symptoms. Clinical examination reveals hepatomegaly, most frequently moderate, of increased consistency. The firm consistency of the liver on palpation suggests the possibility of steato-fibrosis (or even steato-cirrhosis). From an imaging point of view, steatosis can be divided into diffuse liver steatosis and focal liver steatosis. Ultrasound examination is very reliable in the diagnosis of diffuse liver steatosis, in which a fatty loading of the liver higher than 10% will translate into an increased hepatic echogenicity bright liver (Fig. There is a direct correlation between the severity of fatty loading of the liver and the degree of acoustic shadowing. Thus, depending on the intensity of posterior beam attenuation, steatosis is subjectively categorized as mild (discrete attenuation), moderate (obvious attenuation), and severe steatosis (difficult or impossible to visualize the diaphragm). This technique will allow the detection of increased liver density (the fat content of the liver can be evaluated). After assessing the size (hepatomegaly) and consistency of the liver, an abdominal ultrasound will be performed, which allows assessment of both hepatomegaly and liver steatosis severity (based on ultrasound brightness and the intensity of posterior attenuation). Other relevant information can be obtained from biological data: gamma-glutamyl transpeptidase, blood glucose level (possibly glucose tolerance test) and lipids profile (particularly triglyceride values). Liver steatosis can be simple (asymptomatic) or it can be accompanied by secondary hepatic injury (cytolysis). A quarterly reevaluation of the ultrasound appearance of the liver should be performed, until the liver aspect returns to normal. Focal hepatic steatosis is a particular case of fatty loading of the liver, characterized by lipid accumulation within the hepatocytes restricted to a certain area. Another possible explanation for focal steatosis is the fact that in a certain hepatic area, intrahepatocytic fat droplets have different sizes compared to lipid accumulations in other parts of the liver (resulting in a different ultrasound appearance). However, the explanation of excess lipid accumulation restricted to certain areas is currently not very clear. The ultrasound appearance of focal hepatic steatosis is somewhat typical; it translates into a hyperechoic area of variable size in the liver. The background is also defined by steatosis, but in some cases, the rest of liver may present as normal on ultrasound examination. The area affected by focal steatosis generally is not clearly delimited (unlike delimitation in the case of hemangiomas). Focal steatosis may occur without any objective cause, or it can be the consequence of long term corticosteroid therapy. A particular case of focal liver steatosis is the focal fat accumulation in the hepatic hilum. It involves excess fat storage in a typical hepatic area, situated at the portal bifurcation. It is an oval shaped area, usually 3-4/2-3 cm in size, situated at the bifurcation of the portal vein, between its right and left branches. For an experienced ultrasonographist, the diagnosis is relatively easy, but differential diagnosis should be performed in order to exclude a hemangioma or a hepatic tumor of the hilum. The hypoechoic hepatic area is sometimes less clearly delimited, while in other cases there is a clear delimitation between these areas and the normal hepatic parenchyma, through one of the hepatic veins. The ultrasound differential diagnosis of fatty free areas is often difficult, because one must suspect a hypoechoic primary or secondary hepatic tumor occurring in a liver affected by hepatic steatosis. This technique will reveal the same enhancement pattern following contrast bolus in the focal steatosis, fatty free areas and in the adjacent hepatic parenchyma in all vascular phases (arterial, portal and late phase). In cases of difficult differential diagnosis of focal steatosis or fatty free areas, when contrast enhanced ultrasound has not answered the question (extremely rare cases), computed tomography can be used, which will easily differentiate areas with or without fatty loading. Sometimes, focal steatosis areas (less commonly fatty free areas) can be spread into the liver parenchyma, causing hepatic inhomogeneity. Differential diagnosis in these situations is made with hepatocarcinoma and the multicentric form of metastatic liver. In conclusion, we can state that ultrasound is a good, non-invasive technique for assessing liver steatosis, as well as for the quantitative evaluation of steatosis (relatively well correlated with the histological fat loading of the liver). Liver cirrhosis is considered to be an irreversible state of nodular transformation of the liver parenchyma. The etiology of liver cirrhosis is varied, but alcohol abuse and hepatitis viruses B and C are the most frequently incriminated. Thus, in a study carried out for 3 years in the Department of Gastroenterology Timisoara regarding the etiology of liver cirrhosis, hepatitis C virus was the most frequent (33. It goes without saying that in some situations the etiology is multifactorial, the combination of a viral infection with alcohol abuse being extremely common. In addition to the major etiologies of liver cirrhosis (alcohol or hepatitis viruses), 5-10% of cases have rare causes, being secondary to: autoimmune cirrhosis, Wilson cirrhosis (ceruloplasmin deficiency), hemochromatosis, alpha-1-antitrypsin deficiency cirrhosis, primary biliary cirrhosis, drug-induced cirrhosis, and cryptogenic cirrhosis (a rare condition). Thus, in a group of 1200 liver transplants performed in Dallas, almost 10% were performed for cryptogenic cirrhosis. In our group (in an endemic hepatitis virus area), the frequency of cryptogenic cirrhosis is much lower, but this might be due to the fact that cirrhosis is too easily labeled as alcoholic when no other etiological factor can be determined (without taking into account the need for alcohol consumption in a toxic dose for a long enough time). The inspection of the abdomen and chest can reveal collateral abdominal circulation (not a very specific sign) or the presence of spider angiomas (spider naevi) on the chest. Applying pressure makes them disappear, while if the pressure stops they will subsequently reappear, this being a criterion for differentiation of various vascular angiectasis. The patient in dorsal decubitus, with the knees slightly bent for the relaxation of the abdominal muscles, will be asked to perform deep inspiration-expiration movements, which will allow for an accurate liver palpation in order to assess the consistency of the liver. During deep inspiration, the liver will descend (pushed by the diaphragm) and will be easily accessible. After several inspiration/expiration movements, based on palpation, a doctor with good clinical experience will be able to assess if hepatomegaly is present or not, as well as the liver consistency (clinical elastography). We insist on the adequate and correct palpation of the liver, for this method is superior to certain imaging methods used in order to evaluate liver size. Ultrasound examination in liver cirrhosis may reveal multiple changes, but in some cases it can be normal (in up to 20% of cases). Caudate lobe hypertrophy the caudate lobe or the first hepatic segment suffers from hypertrophy in the evolution of liver cirrhosis; therefore it will be frequently enlarged in patients suffering from this condition. Several ways of evaluating the caudate lobe have been described; for example, the calculation of its volume or its relation with the size of the right hepatic lobe. In current practice, the easiest method is to measure the anteroposterior diameter of the caudate lobe by means of ultrasound. In order to differentiate the anteroposterior diameter of the caudate lobe in healthy and cirrhotic subjects, we performed a prospective study which included 200 healthy subjects (126 women and 74 men). Enlarged caudate lobe By comparing these results with a group of 24 cases of known liver cirrhosis, we found that the mean diameter of the caudate lobe in cirrhosis was 47 mm (p<0. These data led us to use the 19 caudate lobe hypertrophy as a sign of liver cirrhosis (Fig. Based on a long ultrasound experience and personal studies, we consider the upper normal limit for the anteroposterior diameter of the caudate lobe to be 35 mm. However, there is an overlapping of normal and cirrhosis cases, so that we generally consider a size of the caudate lobe greater than 40 mm as relevant for cirrhosis (Figs. In current ultrasound practice, approximately 2/3 of cirrhosis cases have a hypertrophic caudate lobe; sometimes with a typical ultrasound appearance (a large, globulous appearance being particularly useful for diagnosis). The caudate lobe size will be used for the diagnosis of liver cirrhosis only in a well known clinical context. Subsequently, the maximum anteroposterior diameter of the caudate lobe should be measured. Measurement of the caudate lobe can be difficult in cases of marked steatosis (ultrasounds are strongly absorbed by fatty tissue) or, more rarely, in the case of ascites. Heterogeneous liver echotexture Liver echotexture changes, particularly hepatic heterogeneity occur in approximately half of cirrhotic cases (Fig. Hepatic heterogeneity is the consequence of fibrous changes that lead to the formation of regenerative nodules. However, there are liver cirrhosis cases without imaging changes of the hepatic echotexture. Liver micronodulation is a histological reality in cirrhosis, but ultrasound cannot evidence these small nodules. The way to accurately diagnose hepatic nodules by ultrasound is to evaluate the liver surface in cases with ascites (Figs. The anterior and, to a smaller extent, the posterior liver surface are easy to examine if ascites is present. Thus, nodules with a size of less than 5 mm in micronodular cirrhosis and more than 5 mm in macronodular cirrhosis can be seen. In ascites-free cirrhosis, it is almost impossible to notice liver surface changes. If a change in the liver architecture (heterogeneity) is found, a possible cirrhogenic liver disease should be suspected. Clinical, biological, and endoscopic examination, as well as elastography (FibroScan) can diagnose cirrhosis that was completely unknown before the ultrasound examination. Studies have shown that these methods are sensitive and specific for diagnosing chronic hepatitis with significant fibrosis (F? Splenomegaly An enlargement of the spleen (over 12 cm long) is frequent in cases of liver cirrhosis (Figs.
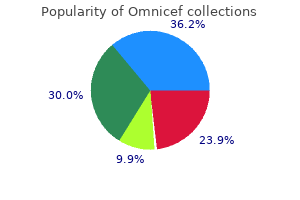
In response to rapid delivery of a higher than 7 points is suggestive of dumping syndrome antibiotic induced c diff buy 300mg omnicef fast delivery. Symp lowed by rapid absorption of glucose into the circula toms of early dumping can be elicited by an oral glu tion antibiotics review pdf buy cheap omnicef 300 mg on-line. Patients should be instructed to avoid liq Table 3 uids for at least 30 minutes after a solid meal bacteria and blood in urine buy omnicef 300 mg fast delivery. Carbohydrate intake should be reduced infection synonym discount 300 mg omnicef with amex, with prefer Shock +5 ence for complex antibiotics dog bite omnicef 300 mg, rather than simple carbohydrates Fainting antibiotic induced colitis purchase omnicef 300mg without a prescription, syncope, unconsciousness +4 (Table 4). Milk and dairy products are not well toler Desire to lie or sit down +4 ated and they should be avoided (22). Increased intake Breathlessness, dyspnea +3 of protein and fat is recommended to meet daily energy Weakness, exhaustion +3 needs. Supplementation of dietary fibers (bran, citru Sleepiness, drowsiness, apathy, falling asleep +3 cel) has been shown to be beneficial in the treatment of Palpitation +3 late hypoglycemia. Pectins, guar gum, and glucoman Restlessness +2 nan are effective by delaying glucose absorption and Dizziness +2 prolongation of small bowel transit time (23). Headaches +1 Most patients with mild symptoms respond well to Feeling of warmth, sweating, pallor, clammy skin +1 Nausea +1 dietary changes. Therefore, a proper patient education Abdominal fullness, meteorism +1 about dietary restrictions is very important. In cases of Borborygmus +1 severe vasomotor symptoms, lying supine for 30 min Eructation 1 utes after meals may reduce the chance of syncope by Vomiting 4 slowing the rate of gastric emptying and improving venous return. A challenge test with higher amounts of glucose Drug Therapy should be avoided, because it can provoke symptoms Medical therapy plays an important role in patients who of dumping in non-dumpers. Several drugs have been breath test after glucose ingestion has been reported to described as beneficial in symptom control, without be 100% sensitive for early dumping. A diagnosis of consistent success, in small studies and case reports, late dumping can often be confirmed by frequent blood including tolbutamide, propranolol, cyproheptadine, sampling after provocation with oral glucose. Two other response to this test, elevated plasma levels of glucose drugs, acarbose and octreotide, have been studied more during the first 60 minutes and reduced plasma glucose extensively and will be discussed in more details. However, induc tion of symptoms after glucose provocation is more Acarbose accurate for diagnosis of late dumping. Efficacy of acarbose in late dumping Gastric emptying scintigraphy can reveal rapid rate of is related to delayed carbohydrate digestion by slowing gastric emptying. An upper endoscopy or barium study conversion of starch and sucrose to monosaccharides can help to exclude ulcer or obstruction. A com plete disappearance of late symptoms, palpitation and Diet dizziness, has been reported with acarbose (50/100 mg Dietary modifications are the mainstay of therapy in t. Unsweetened cereals Sweetened cereals Octreotide has a strong inhibitory Bread, pasta Sweet rolls effect on the release of insulin and Rice, potatoes Pancakes with syrup several gut-derived hormones. It Crackers prevents late hypoglycemia by Fresh fruit Canned fruit in heavy syrup delaying the maximal rise in plasma Unsweetened frozen fruit Sweetened juice Candied fruit glucose level and by reducing peak insulin concentration (28). The other Plain yogurt Milkshakes beneficial mechanisms of action in Skim milk Sweetened yogurt dumping include slowing the rate of Sugar-free pudding/candies Cakes, ice cream, honey, jelly gastric emptying and small intestine Sugar free beverages (coffee, tea) Sweetened drinks (regular soda) transit time, inhibition of postpran dial vasodilation and splanchnic Patient education materials on dumping diet are available on the website of University of vasoconstriction, and increase in Pittsburgh Medical Center at patienteducation. Despite attenuation of blood pressure, packed cell volume and plasma osmo hyperglycemia and reduced rise in plasma insulin with larity in subjects with dumping when compared to acarbose at 50 mg, no statistically significant improve placebo (30). The effectiveness of octreotide in amelio ment was seen in the dumping score, including those rating symptoms of dumping is summarized in Table 6. Use of acarbose the initial recommended dose of octreotide is 25?50 may be limited by the occurrence of diarrhea and flat g administered subcutaneously, 2?3 times daily, ulence secondary to fermentation of unabsorbed 15?30 minutes before meals. The dose can be increased monosaccharides, but its adverse effects subside over to 100?200 g if the smaller dose is not effective. Its role in the therapy of dumping has yet to be In short-term studies relief of symptoms has been clarified. Octreotide has been shown to maintain its effi Table 5 cacy long-term in patients Drugs used in reduction of dumping symptoms with refractory dumping (31). Improvement in qual Drug Dose Effect ity of life has been seen with long-term treatment Tolbutamide (38) 0. Preventing vasomotor symptoms largest study up to date, Methysergide maleate (41) 4?8 mg, b. In summary, therapy with octreotide is jects with further symptom control in 80% of patients safe and it should be offered to patients with severe after three months of therapy. Significant steatorrhea Conservative management is always preferred because has been found with octreotide use. An early morning most patients may expect improvement in dumping diarrhea or steatorrhea associated with long-term ther symptoms over time. It is suggested to follow medical apy can be controlled with an extra dose of octreotide measures, including diet, and behavioral and drug ther before bedtime or pancreatic enzyme replacement. Symptomatic Dumping syndrome is a common complication and improvement in dumping with this type of surgery has important to recognize after gastric surgery. For those nosis of dumping is based on clinical presentation or a patients who already had a Roux-en-Y reconstruction, glucose provocation test in difficult cases. Severe an antiperistaltic jejunal loop interposition should be dumping can be associated with considerable morbid considered. Therefore, it is most important to prevent References development of dumping syndrome by selecting a gas 1. Cause and treatment of certain unfavorable after effect tric procedure associated with less dumping symptoms of gastroenterostomy. A prox results of gastrojejunostomy: Operative cure by disconnecting old imal gastric vagotomy is a preferred surgery for the stoma. Somatostatin and the dumping ing on Weight Loss After Gastric Restrictive Surgery for Morbid syndrome. Dumping syndrome: a com somatostatin analog, in the management of postoperative dump mon problem following Nissen fundoplication in young children. Post-gastrectomy radiology with a physiologic con Pharmacol Ther, 2005; 22:963-969. Should it be parietal cell vagotomy or early dumping syndrome: effects of dumping provocation with selective vagotomy-antrectomy for treatment of duodenal ulcer? A clinical diagnostic index in the diagnosis of the rent insights into pathophysiology, diagnosis and treatment. Changes in plasma volume and blood sugar Scand J Gastroenterol Suppl, 1997; 223:21-27. Effect of acarbose, pectin, a by somatostatin analogue in patients after gastric surgery. Arch combination of acarbose with pectin, and placebo on postprandial Surg, 1991; 126:1231-1235. Octreotide in the treatment of the dumping syn troenterol Hepatol, 1998; 13:1201-1206. Treatment of severe post biochemical responses and clinical symptoms in dumping syn vagotomy/postgastrectomy symptoms with the somatostatin ana drome. In the follow of the National Academies of Sciences, Engineering, ing sections, the authors discuss the challenges in the and Medicine held a workshop titled the Challenge treatment of obesity, followed by the challenges in the of Treating Obesity and Overweight with the objective treatment of severe obesity. The paper concludes with of exploring what is known about current obesity a section on emerging treatments. Presenters described the Treatment of Obesity currently available modalities, including behavioral, medical, and surgical approaches. Emerging treatment Adults modalities, including mobile health, devices, and new the primary modalities used in adult obesity treat pharmacologic approaches were also explored. The authors discuss challenges delivered in person?individually or in groups?can be facing children and adults with obesity, including ac e? A 1 percent reduction in 16 and 17-year-olds in the Supported by extensive evidence, such programs pro United States with obesity and overweight will reduce duce an average weight loss of 5?10 percent of initial the number of adults with obesity by 52,821 in the fu body weight over six months, with continued main ture and increase lifetime quality-adjusted life years by tenance over an additional six months of continued 47,138 years by 2039 [3]. However, barriers such as cost, time, ing consensus indicates an urgent need for e? Interventions delivered remotely by telephone In 2007, the Expert Committee on the Assessment, or electronically lead to less weight loss on average but Prevention and Treatment of Child and Adolescent do have the advantage of being more cost-e? Research to improve the reach and ef a four-stage approach based on age, weight status, fectiveness of remotely delivered behavioral interven presence of comorbidities, and response to treatment tions has the potential to expand access to e? Stage 2 structured weight management, are delivered Despite initial weight loss for many individuals us in the primary care o? Stage 3 cal and environmental factors promoting weight re treatment, or the Weight Management Program, is de gain. Stage 4 treatment, enhance initial weight loss and improve longer-term aimed at youth with severe obesity, includes the use weight maintenance. However, such programs mended that the medication be discontinued for lack are resource-intensive and not universally available [6]. In addition, re sal coverage for comprehensive, intensive behavioral search to identify new or repurposed e? Yet, macologic treatments (including combination therapy) poor reimbursement for childhood and adolescent with acceptable risks is warranted. Advocacy around insurance reimbursement is an im portant gap that must be addressed before compre Page 2 Published September 10, 2018 Clinical Perspectives on Obesity Treatment: Challenges, Gaps, and Promising Opportunities hensive behavioral treatment can become available to ing new technologies into treatment options may also all. Policies and programs driven by multiple sectors present a chance to address disparities in outcomes, and platforms will be integral to making any progress. However, creating an evidence base for the use terventions, and research are necessary steps to im of technology in pediatric obesity care faces the chal prove reimbursement for long-term, sustainable inter lenge of research funding cycles that move at a much ventions. The use of across several medical specialties and public health web-based interventions, mobile apps, and text mes venues. Although the prevalence of obesity overall saging has led to promising results in adult popula has leveled o? Obesity medicine, a rapidly growing among pediatric populations were not achieved [12]. The use of Wi-Fi scales, blood of dietary interventions, behavioral interventions, and pressure cu? Although patient visits may be cov more than 20 percent of patients experience weight ered if comorbid conditions are present, medications regain with recurrence of comorbidities [16,17]. Approximately 50 percent of employers who rent evidence suggests that starting medication at a provide health insurance opt in for anti-obesity medi weight plateau may be more e? Coverage homeostatic control of body weight by hypothalamic has expanded slightly since this publication [22]. In the disease of obesity, there is a disruption of this Bariatric Surgery homeostasis because of impaired neurohormonal sig Bariatric surgery is the most e? In cases of severe obesity, it is critical to think weight loss and maintenance in patients with severe of reasons beyond diet that may have a? Several commonly pre verse events, use is limited to a small fraction of those scribed medicines can contribute to abnormal weight who are eligible for the procedure. Alternatives to these medi currently the most commonly performed bariatric sur cines should be considered and, if possible, changed gical procedure. There are also limited data on safety to those that are weight neutral or to agents that can and e? Comorbid conditions, as evaluated when patients reach plateaus or regain well as functional impairments associated with moder weight after bariatric surgery. In addition, A novel approach to the treatment of severe obesity the weight loss response to standardized intervention, is incorporating the use of technology. Longer-term risks or complications are to be embraced by the bariatric surgical community. Revisions may be performed on patients gery to patients who meet criteria for such surgery re who have lost less than the desirable weight or expe mains as low as 2 percent or less per year in the United rienced undesirable weight regain. More precise data are needed to identify procedure associated with greater weight loss is one the explanation(s) for this low application of bariatric example of such revision. Problematic recurrent hypoglyce candidates as well as low physician reimbursement mia, although rare, may also require reversal. Alcohol rates, as is the case for Medicaid-covered patients, use disorder has been identi? The frequency and etiology of this surgery, although data clarifying these important phenomenon requires further de? The institution or addition increased personalization of this care, it is reasonable of lifestyle intervention as well as pharmacotherapy to to predict that the application of bariatric surgery will patients desiring additional weight loss beyond that increase. Page 6 Published September 10, 2018 Clinical Perspectives on Obesity Treatment: Challenges, Gaps, and Promising Opportunities Children and Adolescents health status of adolescents with severe obesity who One of the signi? In addition to re severe obesity is limited access to appropriate care and porting the baseline prevalence of numerous obesity resources. This is keenly experienced in low-income related comorbid conditions such as dyslipidemia (74. Furthermore, initially favorable short-term ing delivered by primary care providers and dietitians results and complication pro? In a related mass index between the 85th and the 97th percentile, analysis by Inge et al. In addition to providing robust at the time of surgery predict a higher probability of and uniform data, recent studies have also served to resolution of speci? In addition to the need to address related this analysis also served to highlight post-operative professional education, including the ongoing devel nutritional de? Age less than 18 years and cent), dyslipidemia (38 percent versus 86 percent), speci? Collectively, these reports though it is anticipated that these ongoing studies will not only highlight the ongoing challenges faced by the yield additional long-term data and provide important pediatric population with severe obesity, but highlight insights in the future, a number of related opportuni the need for continuous e? In the past, the success the utilization of metabolic and bariatric surgery in the rate in developing safe and e? Newer medications recently prevalence of weight loss operations among adoles introduced or still in development tend to be more se cents has remained relatively low compared with the lective for known weight control targets and hence are a?
Agents known to compromise cardiorespiratory function should be administered only by individuals experienced in airway management and in settings with the capacity for continuous cardiorespira tory monitoring antibiotic guideline best omnicef 300 mg. Intraoperative and Postoperative Pain Management Pain is an inevitable consequence of surgery at any age antibiotics early period cheap omnicef american express. A health care facil ity providing surgery for infants should have an established protocol for pain management antibiotic 1000mg buy omnicef from india, based on a coordinated antibiotics for uti in babies buy on line omnicef, multidimensional strategy antibiotic juice purchase omnicef cheap. Although it is now considered unethical to perform surgery in the newborn without anes thesia antibiotics constipation buy discount omnicef 300 mg online, the appropriate levels of anesthesia for various surgical procedures have not been well investigated. For major surgical procedures, general anesthesia by inhalation of anesthetic gases, intravenous administration of narcotic agents, or regional techniques can be safe and effective. Anesthesia for surgical procedures for all newborns should be administered by specially trained physicians, and the choice of technique and agent should be based on a comprehensive assessment of the infant, efficacy and safety of the drug, and the technical requirements of the procedure. The use of analgesic agents is important in the immediate postoperative period and should be continued as required. Continuous or bolus infusions of opioids and continuous caudal or epidural blockade can be used to provide a steady course of pain relief, but both require careful management and continu ous monitoring of cardiorespiratory and hemodynamic status. Acetaminophen can be used as an adjunct to regional anesthetics or opioids, but there are inadequate data on pharmacokinetics at gestational ages less than 28 weeks to permit calculation of appropriate doses. Because there have been no prospective trials of analgesia for this procedure to date, recommendations based on general principles include slow infiltration of the skin with a local anesthetic and systemic analgesia with a rapidly acting opioid. Removal of the chest drain can also be very painful, and a short-acting, rapid-onset systemic analgesic agent should be considered for this procedure. Although there are insuf ficient data to make specific recommendations, a reasonable approach would be administration of oral sucrose and a topical anesthetic. Nonpharmacologic measures, such as swaddling or nonnutritive sucking, should be used in con junction with these agents. For information on pain management during circumcision, see Circumcision in Chapter 8. Except for emergent intubation during resuscitation, and perhaps for infants with upper airway anomalies, premedication should be used for all endotracheal intubations in newborns. Medications with rapid onset and short duration of action are preferable, and the following principles should be observed. In circumstances when intravenous access is not available, alternative routes, including intramuscular or intranasal administration, can be con sidered Topical Anesthetics for Minor Invasive Procedures Topical anesthetics, such as a mixture of lidocaine and prilocaine, can effectively reduce pain associated with minor invasive procedures, such as venipuncture, lumbar puncture, and intravenous catheter insertion, if the agent is applied for a sufficient length of time before the procedure (at least 30 minutes). These agents Neonatal Complications and Management of High-Risk Infants 365 are not effective for heel-stick blood draws because the pain from heel sticks is primarily from squeezing the heel rather than from the lancet. Medication for Infants Receiving Mechanical Ventilation the routine use of continuous analgesic or sedative agents for mechanically ven tilated infants has not been shown to be helpful and may be harmful; therefore, this practice cannot be recommended. Use of analgesic and anxiolytic agents for amelioration of the discomfort associated with prolonged endotracheal intubation in newborns should be undertaken only after careful consideration of the observed response of the individual infant and the adverse effects of the commonly used agents. A recent Cochrane review concluded that if sedation is required, morphine sulfate is safer than midazolam. Concepts that must be remembered when considering medication for intu bated infants include the following. Chronic use of many sedatives or hypnotics may lead to tolerance, dependency, and withdrawal. The radiologist has the responsibility to create protocols and adjust scanning techniques on the basis 366 Guidelines for Perinatal Care of special considerations of neonatal patients. If the same settings are used for both newborns and adults, newborns will receive an unnecessary and excessive amount of radiation. The transport of an acutely ill infant to the operating room may be associated with a number of risks, including hypothermia, changes in blood pressure, and dislodging of an intravenous catheter or endotracheal tube. Studies have suggested that this approach can be safe and effective and may result in improved outcomes. Personnel should wear appropriate operating room attire, and strict sterile techniques must be used. Such policies should be developed in conjunction with the institutional operating room committee to ensure that all appropriate guidelines are met. Medically stable preterm infants should begin the immunization series at the usual chronologi cal age of 6?8 weeks, unless otherwise indicated. Some very low birth weight infants have been found to have a reduced immune response when the usual timing of immunizations is followed. Additional studies are needed to define the optimal immunization schedule for this group of infants. Vaccine doses should not be reduced for very low birth weight infants or preterm infants. Rotavirus vaccine, which is a live virus vaccine, should not be administered until discharge. Immunization recommendations Neonatal Complications and Management of High-Risk Infants 367 and vaccine safety information are frequently updated and can be verified from the Centers for Disease Control and Prevention Advisory Committee on Immunization Practices web page at. In-Hospital Support and Counseling Bereavement counseling support is important to family members abilities to adjust to their loss and to continue with their lives. Counseling should be tai lored to the specific circumstances surrounding the death; should be sensitive to specific ethical, cultural, religious, and family considerations; and should be provided by specific staff within the hospital. The period after a neonatal death always has an element of confusion because of the continuing grief, the tasks of informing relatives and friends, and the need to make final arrangements. Therefore, involvement of the parents in as much of the bedside care of even critically ill infants as is commensurate with safety and their needs is of major importance. Whether a neonatal death is expected or unexpected, specific management procedures can be useful in facilitating parental adjustment to the loss. Offer the parents, and extended family if desired, an opportunity to see, hold, and spend time with the infant both before and immediately after the death. Even if the parents initially say that they do not want these mementos, they frequently ask for them days, weeks, or months later. The grief of care givers, like that of parents and family, should be addressed and sup ported by appropriate hospital personnel. Anticipate with parents the difficulties they may have in shar ing information about the loss with other children, family, and friends. Provide information and suggestions on how they might handle dif ficult situations or times and information on the availability of support groups. Although there is no substitute for a multidisciplinary group of professionals carefully organized to provide support, written materi als can provide concrete information about specific procedures, such as autopsy and funeral arrangements, as well as guidance on long-term issues, such as grief, marital stress, explanations for young children, and consideration of another pregnancy. These materials can be designed by the individual hospital or obtained through various associations. Neonatal Complications and Management of High-Risk Infants 369 Because families may come from a distance and may not be well acquainted with the attending physicians, it is especially important that referral centers that provide neonatal care designate a member of the team to be an advocate for the family during the hospital stay and after discharge. The designated individual also should be responsible for documenting the management and follow-up of each death. Too often families are lost to follow-up when physicians, nurses, and families avoid sharing the sadness of bereavement. Determining Cause of Death When a neonatal death occurs, a special effort should be made to determine the cause of death. Requesting an autopsy after the death of a newborn must be handled with sensitivity and gentleness. It can be helpful when it is apparent that a newborn is dying, particularly when the underlying cause is uncertain, to introduce the idea of a postmortem examination to the parents. Its value as a means of gaining information that will be helpful in answering their future questions often is perceived as a compelling reason for consent. If there is reluctance for consent for a complete examination of the body, consideration should be given to a limited one, to obtaining specimens of body fluids for microbial culture or other analyses as indicated, and to obtaining postmortem imaging studies if such information could further elucidate the cause of death. In all neonatal deaths, every effort should be made to obtain histopathologic examination of the placenta, membranes, and umbilical cord. When an underlying genetic disorder is suspected and premortem testing is incomplete, advance planning for appropriate specimen retrieval with or with out a full autopsy should occur. In every instance, the family should receive the final written results of the autopsy and other examinations in person, if possible, in conjunction with a verbal explanation of the findings. In addition, when there has been an unexpected clinical deterioration leading to a death, a contemporaneous review of the specific clinical events and decisions with all the involved staff participating can be helpful to resolve interpersonal conflicts, relieve feelings of guilt or failure, and improve both understanding and team interaction. Such sessions usually are best led by the attending neonatologist, although, on occasion, employment of an uninvolved facilitator can be useful. Referral of family members to bereavement support groups or bereave ment counselors Hospital Discharge of High-Risk Infants ^309^322 Discharge Planning Discharge planning for high-risk infants should begin early in hospitalization and includes six critical elements: 1. Determination and designation of follow-up care Neonatal Complications and Management of High-Risk Infants 371 Discharge planning for infants who have been transported back to community hospitals for convalescent care should follow the same principles, and the care plan should be coordinated between the two units before the transfer of the infant occurs. The following recommendations are offered as a framework for guiding decisions about the timing of discharge. It is prudent for each institution to establish guidelines that ensure a consistent approach yet allow some flexibility on the basis of physician and family judgment. It is of foremost importance that the infant, family, and community be prepared for the infant to be safely cared for outside the hospital. Infant Readiness the infant is considered ready for discharge if, in the judgment of the respon sible physician, the following have been accomplished. A sustained pattern of weight gain of sufficient duration has been dem onstrated. Identification of at least two family caregivers, and assessment of their ability, availability, and commitment. Review of available financial resources and identification of adequate financial support In preparation for home care of the technology-dependent infant, it is essential to complete an assessment documenting availability of 24-hour tele phone access, electricity, safe in-house water supply, and adequate heating. Specific modification of home facilities must have been completed, if needed, to accommodate home-care systems. Plans must be in place for responding to loss of electrical power, heat, or water, and for emergency relocation mandated by natural disaster. Caregivers should have demonstrated the necessary capabilities to provide all components of care, including the following. Feeding, whether breast, bottle, or alternative technique, including for mula preparation if required. Basic infant care, including bathing; skin, and genital care; temperature measurement; dressing and comforting Neonatal Complications and Management of High-Risk Infants 373. Infant safety precautions, including proper positioning during sleep and proper use of car seats (see also Parent Education and Psychosocial Factors in Chapter 8). Specific safety precautions for the artificial airway, if any; feeding tube; intestinal stoma; infusion pump; and other mechanical and prosthetic devices, as indicated. Administration of medications, specifically proper storage, dosage, tim ing, and administration; and recognition of signs of potential toxicity. Equipment operation, maintenance, and problem solving for each mechanical support device required. Appropriate technique for each special care procedure required, includ ing special dressings for infusion entry sites, intestinal stomas, or healing wounds; maintenance of an artificial airway; oropharyngeal and tracheal suctioning; and physical therapy, as indicated. Community and Health Care System Readiness An emergency intervention and transportation plan must be developed, and emergency medical service providers identified and notified, if indicated. Follow-up care needs must be determined, appropriate physicians identified, and appropriate information exchanged, including the following. A primary care physician has been identified, and has accepted respon sibility for care of the infant. Within this framework, there are four broad catego ries of high-risk infants that require individual consideration: 1) preterm infants, 2) infants with special health care needs or dependence on technology, 3) infants at risk because of family issues, and 4) infants with anticipated early death. Preterm Infants Criteria for hospital discharge of preterm infants should include physiologic stability rather than attainment of a specific weight. The three physiologic com petencies generally recognized as essential before discharge are 1) oral feeding sufficient to sustain appropriate growth, 2) the ability to maintain normal body temperature in a home environment, and 3) sufficiently mature respiratory con trol. These competencies usually are achieved by 36?37 weeks of postmenstrual age; infants born earlier in gestation and with more complicated medical courses tend to take longer to achieve these physiologic competencies. Preterm infants should be placed supine for sleeping, and hospitals should model this behavior for parents by positioning infants supine after approximately 32 weeks of post menstrual age. Late preterm infants (34?37 weeks of gestation) are at increased risk of feeding problems and hyperbilirubinemia after discharge. These infants require close follow-up after discharge to monitor bilirubin concentrations and weight gain (see also Discharge of Late Preterm Infants in Chapter 8). Infants With Special Health Care Needs or Dependence on Technology Increasing numbers of infants are being discharged from the hospital with continuing medical problems requiring specialized technologic support. When infants are unable to achieve adequate oral feedings to sustain growth, alternatives include gavage or gastrostomy feedings, parenteral nutrition, or both. Gavage feeding has a limited role and should be considered only when feeding is the last issue requiring continued hospitalization and the parents or caregivers have demonstrated competence and comfort with this procedure. When little to no progress is being made with oral feedings, gastrostomy tube Neonatal Complications and Management of High-Risk Infants 375 placement can make hospital discharge feasible and allow the infant to develop competent oral feeding skills if possible. Home parenteral nutrition requires thorough education of caregivers and the availability of a home-care company that is well versed in infant nutritional support and monitoring. Respiratory support can include supplemental oxygen, tracheostomy, or home ventilation. Oxygen saturation levels should be assessed intermittently at home to ensure sufficient oxygen is being delivered during a range of activities and sleep. Some infants who are discharged on supplemental oxygen also are discharged on a cardiorespiratory monitor or pulse oximeter in case the oxygen supply is interrupted. Reducing or stopping supplemental oxygen should be supervised by the physician or other health care professional and attempted only when the infant demonstrates acceptable oxygen saturations (greater than 90%) with good growth velocity and sufficient stamina for usual activity. Home care of the infant with a tracheostomy requires extensive parental teaching and coordinated multidisciplinary follow-up care. Infants with tracheostomy should be discharged on a cardiorespiratory monitor in case the airway should become obstructed.
Purchase omnicef us. Antimicrobial Pre-procedural Mouth Rinses.
References
- THURTELL MJ et al:Tuberculous cranial pachymeningitis. Neurology 68:298, 2007.
- Keidel, M., Rieschke, P., Juptner, M., & Diener, H. C. (1994). Pathological jaw opening reflex after whiplash injury. Nervenarzt, 65(4), 241n249.
- Seymour JF, Presneill JJ, Schoch OD, et al. Therapeutic efficacy of granulocyte-macrophage colony-stimulating factor in patients with idiopathic acquired alveolar proteinosis. Am J Respir Crit Care Med 2001;163:524-31.
- Borin, J.F. Prone retrograde laser lithotripsy facilitates endoscope-guided percutaneous renal access for staghorn calculi: two scopes are better than one. J Endourol 2008;22:1881-1883.
- Wood K, Keys T, Mufarrij P, et al: Impact of stone removal on renal function: a review, Rev Urol 13(2):73n89, 2011.
- Roberts MJ, Williamson DA, Hadway P, et al: Baseline prevalence of antimicrobial resistance and subsequent infection following prostate biopsy using empirical or altered prophylaxis: a bias-adjusted meta-analysis, Int J Antimicrob Agents 43(4):301n309, 2014.
- Glaser JS, Sadun AA. Anatomy of the visual sensory system. In: Glaser JS, editor. Neuro-ophthalmology. ed 3.
- Toma JG, McKenzie IA, Bagli D, Miller FD. Isolation and characterization of multipotent skin-derived precursors from human skin. Stem Cells 23: 727-737, 2005.