Judy Mastick, RN, MN, FNP
- Research Nurse Coordinator, Department of
- Physiological Nursing, University of California,
- San Francisco, CA, USA
Make sure there is no bleeding from the tunica vaginalis; insert another row of sutures if necessary bipolar depression 45 buy aripiprazola with paypal. Stretch the layers of the dartos to make a pouch for the testis: this will allow any fluid to get absorbed and not re-collect depression symptoms mood swings purchase aripiprazola with amex. Close the wound in 2 layers anxiety 4th hereford purchase generic aripiprazola online, taking the dartos muscle in the first depression symptoms extreme anger buy aripiprazola 20mg on line, and the skin in the second depression nightmares buy aripiprazola toronto, with continuous short-acting absorbable suture anxiety questions order aripiprazola 20 mg with mastercard, to secure haemostasis. A large hydrocoele with a greatly thickened wall, perhaps covered with a layer of cholesterol crystals. If the hydrocoele is very large, resect the redundant scrotal skin, but leaving enough skin remaining to recreate a scrotum. Excise the entire sac of the hydrocoele, except for a cuff 1cm deep around the testis and epididymis (27-21C). A, make an elliptical incision, and excise the skin within the ellipse, (1) the cleft between the testis and epididymis may be after which you can turn the processus vaginalis inside out (B), greatly enlarged by the extension of the hydrocoele, or you can excise it (C). If there appear to be bilateral hydrocoeles, (2) Operate gently and control bleeding before you close start with the biggest side first; the apparent second the skin. Start again through the groin to identify the sac at the internal ring, If mild bleeding persists, insert a drain through the and proceed as for a hernia repair. If the scrotal sac remains large and floppy, secure it to the anterior abdominal wall between 2 pieces If when you open the sac you find altered blood of gauze, for 48hrs. If the patient is a neonate or child, operate through the groin because this type of hydrocoele is actually usually a If you find a malignant-looking testis, start again hernia with fluid in a patent processus vaginalis (18. Torsion of the spermatic cord (strictly speaking) is a Typically, a teenage boy wakes with sudden severe pain in surgical emergency which needs operation without delay. Often, there is severe nausea and vomiting, Occasionally, the tunica vaginalis ends abnormally high and rarely a fever. The testis becomes tender and swollen, up the spermatic cord, so that the cord can twist and and the skin of the scrotum may become red. You will not do harm by exploring orchitis, but antibiotics will not relieve torsion. Do not rely on a Doppler test: the presence of blood flow shows the testicle is still viable, but not that it has not twisted! It is only appropriate in the 1st 2hrs of symptoms, but may buy you time if you cannot operate within 6hrs. Even if it is successful, torsion may recur, so proceed to operation and fixation early. Cut through the subcutaneous tissue and fascial layers down to the tunica vaginalis. You will find it filled with blood-tinged fluid, and you will see the twisted spermatic cord. If there seems no chance that the testis will survive, check that it is really infarcted by cutting into it: if it does not bleed, transfix the spermatic cord and remove the testis (27. Occasionally, the tunic vaginalis ends abnormally high up the If you are not sure if the testis is viable or not, spermatic cord, so that it can twist and obstruct the blood supply to wrap it in a warm moist swab and inspect it again after the testis and epididymis. Bright bleeding when you incise the tunica intravaginal spermatic cord hanging horizontally. D, the cord untwisted and the testis anchored to it, especially if the symptoms have lasted <12hrs, prevent recurrence. Whatever the viability of the twisted testicle, you must always anchor the contralateral testis in the same way: the anatomical abnormality is usually bilateral. Close the dartos and skin in 2 layers with continuous short-acting absorbable suture. If in an infant and especially a neonate, you find that the whole tunica vaginalis with its contained testis and spermatic cord is twisted (supravaginal torsion), deal with it in the same way. If a maldescended testis strangulates, you can mistake it for a strangulated hernia (18. If the torsion reduces spontaneously, advise that it can recur and that bilateral orchidopexy is still necessary. If you find only one testis, the other having been lost to neglected torsion, perform an orchidopexy on the remaining testis. Raise the scrotum, and incise the stretched skin and dartos Or, in treatment of prostate carcinoma (27. Incise the visceral tunica vertically over the globe of the Do not mistake mumps orchitis or epidydimo-orchitis for a testis. This causes rapid enlargement, and some pain substance of the testis from the inner surface of the tunica (which is minimal in the case of a tumour). Control bleeding carefully at the Mumps orchitis may cause little pain, so if you are in upper testicular pole. Remove all testicular tissue, and doubt, wait for a few days rather than remove the testis. Close the scrotum in 2 layers with continuous but beware of its upper end slipping out of the clamp and 3/0 short-acting absorbable sutures, without inserting a retracting out of sight. After 2-3wks, blood clot in the tunica will become haemostasis, before you close the wound. If possible, organized to form a small palpable nodule, not unlike a apply diathermy to the smaller bleeding vessels, and tie off small testis. If it is very thick and track of descent of the testis: the common sites for it are in oedematous, ligate it twice with a fixation suture and the inguinal canal, or inside the abdomen. If the area is infected, leave the wound in the A maldescended testis, however, may lie in the supra scrotum unsutured to drain freely, dress it loosely, inguinal pouch, just superior to the external ring deep to and close it by delayed primary suture. A testis which is absent from the scrotum will produce hormones but not spermatozoa. You will need to remove the cord with the testis, so open So if neither of the testes is in the scrotum, there will be up the inguinal canal as for a hernia with an inguino normal secondary sex characteristics, including potency, scrotal incision (18-7A). Deliver the testis only, there will probably be fertility, but the misplaced from the scrotum by pushing it up from below. Spermatogenesis is normal in If the tumour is large, you will have to extend the opening an incompletely descended testis and in a maldescended in the external inguinal ring. Maldescended testes are usually functional, which can be brought down more readily. Unfortunately, the evidence for orchidopexy improving fertility is still inconclusive. If neither testis is present in a neonate scrotum, the possibilities are commonly, (1) Retractile testes; (2);A genuine undescended or maldescended testis; or rarely, (3),An intersex state. These are complex and include true hermaphroditism and the adrenogenital syndrome. By puberty they will probably be permanently in remove the cord with the testis through the groin. Do not cut through the scrotum as you will then correct position in the scrotum, you should perform an open up a different lymphatic drainage field for the orchidopexy, especially above the age of 2yrs. If there is a hernia and an undescended testis on the You should try to administer adjuvant chemotherapy if same side, perform an orchidopexy at the same time as the testicular malignancy is confirmed (27. Deal with Presentation is with: incomplete descent and maldescent in the same way. Open the inguinal canal from the external to the in which case gonadotrophin production by the tumour internal ring. If there is a hernia (common) dissect off the sac, divide it It loses its normal sensation early. Fix the testis with (3) haematocele following trauma, monofilament in the dartos pouch, outside the muscle (4) testicular torsion (27. If there is a teratoma, treat with postoperative much as you can, and have removed any hernia sac cyclophosphamide, vincristine, methotrexate and present, open the internal inguinal ring further on its dactinomycin gives a 95% chance of complete cure. If you fail to bring down the testis fully, (2) Do not remove the testis through the scrotum. If there is bilateral incompletely descended testes consider carefully whether you wish to tackle this side as well. There may be a need for further mobilization later at a later stage, but this is unlikely to improve fertility. You will have to cut the inner and outer skin of the foreskin, so you will have to infiltrate them both. With the foreskin forward, infiltrate a ring of anaesthetic solution without adrenalin at the site of section (27-25A,B). To do this you may have to infiltrate a little more solution and make a dorsal slit in it. To do this dorsal nerve block at the base of the penis at 2 & 10 you may have to infiltrate a little more and make a dorsal slit. Horrible shrieks used to be heard from the theatre whenever circumcisions were being done. Check that the child has passed urine, and There may be a significant risk, in some cultures, that a look carefully for hypospadias or epispadias. Consider carefully if, because of financial incentives from programme donors, the resources for performing circumcisions are being diverted from other essential surgery! Place it under the foreskin and over the glans, and Insist on adequate bathing pre-operatively. The suture occludes the a tight phimosis prevent you pulling the foreskin back, blood supply to the foreskin, which ultimately drops off use a probe to free up the foreskin from adhesions to the along with the bell. Retract the foreskin if you can (27-26B), clean thoroughly underneath it and then pull it forwards Make the dorsal slit long enough to accommodate the again. Select the Plastibell cap that best fits the feel for the bulge of the corona of the glans. A cap that is too small will Hold the foreskin laterally on both sides with haemostats, not let you remove sufficient foreskin and a cap that is too and make sure the space between foreskin and glans is free big will cause you to remove too much foreskin. Use a haemostat to crush a midline portion of the dorsal foreskin and then blunt-ended scissors to cut a slit in Separate the two sides of the dorsal slit incision to expose exactly this position up to the level of the bulge in the the glans, put the Plastibell device over the glans, and then corona (27-26C). Make sure that the point of the scissors is Then tie the string securely around the foreskin in the not in the meatus. You can cut off any excess foreskin about using any special circumcision clamps and beyond the suture taking care not to cut the suture itself. Use your thumb and first finger of the non-dominant hand If the device does not fall off during this interval, to grasp the foreskin firmly below the tip of the haemostat you must remove it promptly. Slide the Mogen clamp anteriorly to posteriorly just above your fingers to protect the glans when applying the clamp. If the child has difficulty urinating, it may be because Place it at the same angle as the corona with the hollow the ring has slipped proximally from the glans onto the side facing the glans, so that you remove more foreskin penile shaft; this can result in venous obstruction and a dorsally than ventrally. Before locking the Mogen clamp compartment syndrome leading to necrosis of the glans. Cut off the foreskin distal to the not cut the frenulum and there is no free incised edge of clamp with a scalpel. The bells come in 3 sizes; for a correct fit, the edge of the bell should reach the frenulum After performing a dorsal cut of the foreskin, cut the outer and minimally extend over the corona, slightly stretching skin only round the corona (27-26D). One of the purposes of the foreskin is to provide A dorsal slit is not always necessary. On the other hand do not leave too much of the dorsal slit is visible above the rim of the bell. Slip the handle of the bell through the circular Use 3/0 absorbable individual ties to control bleeding, opening of the base plate, without letting the foreskin slip and suture the fringe of the foreskin to the skin of the shaft off. Finally, control bleeding from the the foreskin is not twisted and remains relaxed proximal to frenal vessels with a special encircling suture (27-26G). If it is taut, you can remove too much foreskin Dress the wound with petroleum jelly gauze. No dressing or even cut into the glans;if it is too loose, you will remove is needed after 24hrs. Do not use diathermy on the penis, it can cause Tighten the thumbscrew until snug to crush the foreskin gangrene of the whole organ. Never use adrenaline in a local anaesthetic for the base plate using a scalpel (27-27F). Allow this to granulate on its own, and do not try to graft it with split If too little foreskin is removed, proceed to a formal skin. If an adult has postoperative priapism, If too much foreskin is removed, you may need a skin sedate him (27. If a urethra-cutaneous fistula develops, either from direct injury or because of a periurethral abscess, you can close this if you use a Dartos fascia graft. Measure the fistula, and pass a urethral catheter; decompress the phallus and apply a proximal tourniquet. Insert stay sutures to expose the fistula, and close it using skin flaps (as for hypospadias, 33. Then mobilize the Dartos fascia to place a graft with suture lines not superimposing on each other, using fine 4/0 long-acting absorbable sutures. If a crooked erection develops, there may have been excessive skin removed, or excessive scarring. It is common in adolescence, and is fairly Where the paraphimosis is chronic, there develops a common between 8-14yrs. Part of the foreskin is tight, fibrous band just distal to the corona: you must excise this so that it becomes oedematous distally. Strictures of the meatus have quite a different cause and Squeeze the swollen foreskin between the thumbs and prognosis from the gonococcal urethral strictures (27. The most important acquired If the swelling is severe, wrap layers of gauze coated in cause is infection associated with instrumentation and sugar over it and squeeze them. Apply it into the meatus from the the rounded plastic containers used for disposable needles nozzle of a small tube, which will then act as a dilator.
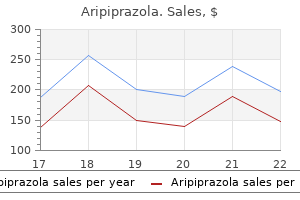
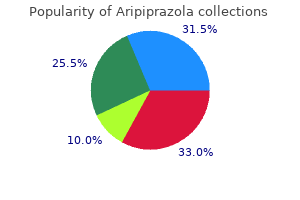
The temperature inside the breast has been measured invasively using thermocouples located at the end of the needle depression clinics order aripiprazola with amex. In addition to Figure 1: Metabolic heat production and growth rate of breast the internal temperature depression symptoms emotional abuse 10 mg aripiprazola visa, all patients have undergone a mammogram carcinomas mood disorder goals order aripiprazola 20mg amex. The data was obtained by observing the progression of and measured the temperature of the skin with a thermal imager depression definition in science order aripiprazola 20 mg fast delivery. In small cancers in patients who initially refused treatment and in total depression experiments purchase aripiprazola 15 mg online, data has been collected from 80 depression in men buy aripiprazola 20mg on-line,000 patients. Doubling time was temperature of 540 patients with invasive cancer has been measured. In addition, temperature measurements have been measurements of temperature and blood fow carried out it, if it taken at symmetrical points of the opposite breasts. D Diameter of tumor in For burning tumors, the 5-year survival was 9%, while survival for cm. Tese studies assessed the level of thermal changes of the tumor as mean value of heat 30-34 mW/cm3. For patients with a low grade of malignancy, values of T3 It should be noted that the data obtained by Gautherie does not (50%) prevailed. Consequently, thermal changes correlate well with the contradict the general concept of increased malignant tumor grade of malignancy. In his famous work, Warburg [18] in 1924 found that the important independent predictor. For this work, he was awarded the Nobel malignant tumor could have considerable prognostic potential. Cells use the anaerobic glycolysis path to dissipate signifcantly more energy, which leads to an increase in temperature of tumors and Kinetics of thermal processes in breast cancer surrounding tissues. The next important question is associated with the kinetics of the The second important conclusion, which can be drawn from the thermal processes in breast cancer. When do the thermal changes analysis of the data presented in Figure 1, is the correlation between associated with malignancy occurfi To answer this question Gautherie heat emissions from tumors and metastases in lymph nodes. Mammographic screening of 19 patients with high heat emission, metastases were present in the did not detect breast cancer (461 women were diagnosed with benign lymph nodes. However, for tumors with low thermal activity, changes, while 784 patients showed no structural changes), but there metastases were detected only in 5 out of 30 patients. All of these patients had annual mammography potential of thermal measurement was also demonstrated by Napalkov for 12 years. Afer 8 years, 38% of patients without structural changes [19], who studied the survival of patients with breast cancer, but with elevated temperature were diagnosed with breast cancer. For patients with thermal changes but an classifcation was used: elevated temperature, this percentage was much higher for 8 years. This rise in indicator for predicting the transition from in situ cancer to invasive temperature cannot be explained by an increased metabolism of carcinoma [27]. Increasing thermal activity of tissues with proliferative characterization of non-invasive cancer. They combined invasive potential for invasive transformation will have a high temperature. In temperature measurement of a malignant tumor and surrounding this regard, Rozhkova et al. In Figure 4, temperature signal (T 4, T 5), despite the small size of initial the vertical axis represents the increase in temperature in tissue tumours. It is known that difuse fbrocystic disease has carried out using electron microscopy. Tus, the density of the microvascular network, and consequently the temperature, appears to be increased at the stage preceding malignant growth. This opens up the opportunities for screening using microwave thermometry, with potential to identify risk groups. Microwave thermometry primarily identifes patients at high risk of potential malignancies, including fast growing tumors. This method allows for multiple readings to be performed at any time interval to continuously monitor potential pathological changes without additional radiation exposure for patients of all ages. The proportion of breast cancers identifed between screening As the growth of tumor cells increases, the cancer becomes cut of rounds (called interval cancers) is an important measure of screening from nutrient sources necessary for survival and division. Cancer may remain in screening of 1000 women, only 20 were detected during screening and situ in this state for many years [24]. In a Stockholm trial interval cancer varied from 25% with the incidence of metastases in a number of solid tumors. This is not an A review of the literature has shown that microwave thermometry unexpected result, as microwave thermography can identify fast can identify fast-growing tumors. It may be benefcial to include as growing tumors and results in fewer false negatives in the 40-49 age part of a comprehensive examination of patients with breast group. Traditional mammography, in turn, identifes cancers, "missed" pathologies and in screening programs [39]. False-negative results do by microwave thermography (tumors with a low degree of malignancy occur with slow-growing tumors, the diagnosis of which is more and low growth rate). Although microwave thermometry cannot replace mammography or ultrasound Monitoring the efectiveness of treatment of mastitis is another because it does not provide information on the structural changes in interesting area of microwave thermography. Slightest changes in the the breast, it can provide additional information about the severity of breasts are mirrored by changes in the thermal activity of breast tissue. This Termal changes, as opposed to structural, can be seen within 10-15 information may in many cases contribute to the development of an days afer the start of treatment. Historical data on treated patients show the estimation of whether the thermal activity increases due to important role of microwave thermography in developing personalized infammation, proliferation and malignant growth or decreases due to therapeutic strategy. In patients with fbrocystic breast disease, thermal changes are not pronounced and do not difer from Tanks to its simplicity, safety and non-invasiveness, microwave the norm related to the age of the patient. In infammatory or radiometry may serve as a promising method for diagnosis, prediction proliferative processes, the thermal activity of tissues increases. It thermal tissue changes can be seen (T3-T5) in 80% of patients with may also have potential as a method for risk stratifcation in breast atypical symptoms [7]. Among other advantages of microwave thermometry are its assess the efect of hormone therapy. It is worth acknowledging that availability, relatively low cost, the absence of radiation and the quick this is a risk-free and painless methodology that provides clear results. Proceedings of Institutes Ser Radiofzika The dynamics of changes in temperature during the course of 24: 1054. The overall temperature can be used to evaluate efciency of results of examination of patients with breast cancer according to X-ray mammography examination and radiometry. Microwave thermography is however a huge step in comparison radiometry mammary glands Tumors of the female reproductive system with the thermal imaging of the past because it allows a glimpse deep 3: 28-35. Shapiro S (1977) Evidence on screening for breast cancer from a mammary glands, Herald of the Kyrgyz-Russian Slavic University 9: randomized trial. Gautherie M (1982) Temperature and blood fow patterns in breast screening for breast cancer in Stockholm. Breast Cancer Res Treat 8: cancer during natural evolution and following radiotherapy. Blamey R, Elston C, Pinder S, Ellis I (2000) When is a patient cured of breast cancer: PhD thesis. Surg Today 33: radiothermometry to evaluate the efcacy of neoadjuvant treatment of 243-248. Weidner N, Folkman J, Pozza F (1992) Angiogenesis tumor: A new screening re-palpable breast tumors. They will then decide if you need referral to a specialist breast clinic for further tests. Breast lumps can involve any of these different tissues, or components, that make up your breast. Common causes of breast lumps Normal (physiological) swelling and tenderness Your breasts change throughout your menstrual cycle each month because of your hormones. At least half of all women who have periods will have some pain, tenderness and lumpiness in their breasts at some time in the month. Pain and lumps (nodules) may occur which are severe enough to need checking by a doctor. Fibroadenoma this is a non-cancerous (benign) breast lump that usually occurs in women under the age of 40. These lumps occur as a result of excess growth of the glands and connective tissue in the breasts. Cysts are more common in women approaching menopause, although they can occur at any age. It is common for them to appear within two weeks prior to your period and then go away (resolve) soon after the period. Cysts cannot turn into cancer and do not always need treating once the diagnosis has been confirmed. Where treatment is needed, it typically involves draining the fluid from the cyst. Infection Alump caused by infection is fairly common in women who are breast-feeding. Fat necrosis Injury or trauma to the fatty tissue in your breast can cause a lump. Lipoma Alipoma is a fatty growth that develops within the fatty tissue of your breast. See separate leaflets called Breast Cancer and Breast Cancer Hereditary Factors for more details. Are you taking a hormone medication such as the contraceptive pill or hormone replacement therapyfi Amale doctor should always offer for a chaperone to be present during the examination. They may want to examine your breasts, with your arms in the air and then by your sides. They may also want to examine your breasts when you are sitting and then lying down. They may also want to examine underneath your arms to feel for any enlarged lymph glands. If you have had any nipple discharge, your doctor may ask you to demonstrate this yourself by asking you to squeeze your nipple. There is more than one right way to examine the breasts and doctors may differ in their approach. If you are under 30 years old, are still having periods and have only just noticed the lump, your doctor may suggest that you return for another examination after your next period. In most cases, the doctor will suggest they refer you to a specialist breast clinic. Here you will see a doctor who has special expertise in dealing with breast problems. The aim is that any woman with a breast lump should be seen in a specialist breast clinic within two weeks. If your doctor feels that you are more likely to have one of the non-cancerous (benign) causes of a breast lump, it may take longer than two weeks for you to be seen. Even if you are referred urgently, you should remember that your lump may still turn out to be benign. What to expect if you are referred to a breast clinic Usually there is a specialist breast nurse who works in a breast clinic. This nurse may be present during your appointment with the doctor and is usually available for any questions afterwards. In some clinics, the specialist nurse runs the clinic and you may only see the nurse. These can include a mammogram and/or an ultrasound scan of your breast (see below). The breast specialist may also suggest that they take a sample (biopsy) of the lump. There are two common ways of doing this, either by fine-needle aspiration or a core biopsy (details below). The specialist uses the scan to identify exactly where the lump is so that they can take the sample. The sample may be taken on the same day in the breast clinic or you may be given an appointment to come back for the procedure. Aperson trained in taking X-rays (a radiographer) will ask you to remove your top and bra. This may feel a little uncomfortable but the discomfort should only last for a few minutes. An ultrasound scan of the breast uses the same technique as an ultrasound scan that women have when they are pregnant. It is a painless test which uses sound waves to create images of structures inside you, in this case the inside of your breast. The ultrasonographer will then move the scanning probe over the surface of your breast.
In contrast to oral administration mood disorder behaviors aripiprazola 10 mg fast delivery, transdermal estradiol does not appear to increase the risk of venous thromboembolic events or gallbladder disease mood disorder due to medical condition buy aripiprazola 20 mg line, though it remains contraindicated in women at high risk for venous thromboembolic disease or those with active liver or gallbladder disease depression young living order genuine aripiprazola. These situations require a thoughtful assessment of potential risks and benefits and documentation of informed patient consent before treatment depression test adults order aripiprazola online. Although sexual problems generally increase with aging anxiety med purchase generic aripiprazola line, distressing sexual problems peak in midlife women (aged 45 to 64) and are lowest in women 65 years or older severe depression just before period aripiprazola 15 mg discount. The etiology of female sexual dysfunction is often multifactorial, including depression or anxiety, relationship conflict, stress, fatigue, prior abuse, medications, or physical problems that make sexual activity uncomfortable, such as endometriosis or atrophic vaginitis. The impact of the menopausal transition on sexual function was examined in a prospective, longitudinal cohort study of approximately 3,000 women who were pre or perimenopausal at baseline and followed for 6 years. Pain during sexual intercourse increased and sexual desire decreased over the menopausal transition, but other factors were unaffected, including sexual arousal, frequency, and pleasure (72). In contrast to menopausal factors, which were unrelated to most aspects of sexual functioning, age, social, health, and psychological factors were strongly linked. Treatment Options Hormone Therapy Estrogen therapy is very effective in treating vaginal dryness and dyspareunia; however, a significant effect of estrogen therapy on sexual interest, arousal, and orgasmic response, independent from its role in treating menopausal symptoms, is not supported by evidence. A woman with distressing low libido concurrent with the onset of bothersome night sweats, sleep disruption, and fatigue likely will experience increased sexual interest with effective treatment of her menopausal symptoms, but this is probably secondary to improved well-being, rather than a direct effect of estrogen therapy on libido. A double-blind, randomized trial of combined oral and vaginal estrogen therapy in 285 sexually active postmenopausal women demonstrated decreased dyspareunia and significant improvements in pleasure of orgasm and sexual interest in women treated with estrogen therapy compared to placebo (73). As this trial used a combination of systemic and vaginal estrogens, it is not possible to determine the relative impact of systemic versus local effects. Potential risks of androgen therapy include hirsutism, acne, irreversible deepening of the voice, and adverse changes in liver function and lipids. As most androgens are aromatized to estrogens, there is potential for an increased risk of cardiovascular events or breast cancer. A transdermal testosterone patch is approved in Europe for the treatment of hypoactive sexual desire disorder in surgically postmenopausal women using concomitant estrogen therapy. Alternatives to Hormone Therapy Although vaginal atrophy and dyspareunia respond very well to estrogen therapy, most other sexual problems may be effectively treated without hormones. In one study, 65% of 365 couples undergoing sex therapy for a range of sexual dysfunctions described their treatment as successful (78). Underlying depression and anxiety should be treated, and antidepressant medication may need adjustment. Despite the fact that sexual problems are common, the majority of women with distressing sexual problems do not seek formal care, but when they do, it is typically the woman, rather than the physician, who initiates the conversation (82,83). Clinicians should routinely ask their menopausal patients whether vaginal dryness, dyspareunia, or another bothersome sexual problem is present, as many effective interventions are available. Summary There are many options available to address the health and quality of life concerns of menopausal women. The primary indication for hormone therapy is the alleviation of hot flashes and associated symptoms. Women must be informed of the potential risks and benefits of all therapeutic options. The effect of hysterectomy on the age at ovarian failure: identification of a subgroup of women with premature loss of ovarian function and literature review. Effects of symptomatic status and the menstrual cycle on hot flash-related thermoregulatory parameters. Treatment of vasomotor symptoms of menopause with black cohosh, multibotanicals, soy, hormone therapy, or placebo. A randomized, controlled pilot study of acupuncture treatment for menopausal hot flashes. Relief of vasomotor symptoms and vaginal atrophy with lower doses of conjugated equine estrogens and medroxyprogesterone acetate. Lowest effective transdermal 17b-estradiol dose for relief of hot flushes in postmenopausal women. Treatment of menopause-associated vasomotor symptoms: position statement of the North American Menopause Society. Venlafaxine in management of hot flashes in survivors of breast cancer: a randomised controlled trial. Citalopram and fluoxetine in the treatment of postmenopausal symptoms: a prospective, randomized, 9-month, placebo-controlled, double-blind study. Eszopiclone in patients with insomnia during perimenopause and early postmenopause. The role of local vaginal estrogen for treatment of vaginal atrophy in postmenopausal women: 2007 position statement of the North American Menopause Society. Vaginal administration of low-dose conjugated estrogens: systemic absorption and effects on the endometrium. A one-year multicenter study of efficacy and safety of a continuous, low-dose, estradiol-releasing vaginal ring (Estring) in postmenopausal women with symptoms and signs of urogenital aging. Endometrial and vaginal effects of low-dose estradiol delivered by vaginal ring or vaginal tablet. A randomized, open, parallel-group study on the preventive effect of an estradiol-releasing vaginal ring (Estring) on recurrent urinary tract infections in postmenopausal women. Prevention of non-vertebral fractures with oral vitamin D and dose dependency: a meta-analysis of randomized controlled trials. Effects of ultralow-dose transdermal estradiol on bone mineral density: a randomized clinical trial. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene. Effect of parathyroid hormone on fractures and bone mineral density in postmenopausal women with osteoporosis. Effects of estrogen or estrogen/progestin regimens on heart disease risk factors in postmenopausal women. Hormone therapy and venous thromboembolism among postmenopausal women: Impact of the route of estrogen administration and progestins. Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. Menopausal estrogen and estrogen-progestin replacement therapy and breast cancer risk. Effects of lower doses of conjugated equine estrogens and medroxyprogesterone acetate on endometrial bleeding. A 5-year follow-up study on the use of a levonorgestrel intrauterine system in women receiving hormone replacement therapy. A randomized, open label, crossover study comparing the effects of transdermal vs. A randomized study of low-dose conjugated estrogens on sexual function and quality of life in postmenopausal women. A field trial of the effectiveness of behavioral treatment for sexual dysfunctions. Bupropion sustained release for the treatment of hypoactive sexual desire disorder in premenopausal women. Sildenafil treatment of women with antidepressant-associated sexual dysfunction: a randomized controlled trial. Efficacy and safety of sildenafil citrate in women with sexual dysfunction associated with female sexual arousal disorder. Lurain Most risk factors for the development of endometrial carcinoma are related to prolonged, unopposed estrogen stimulation. Office endometrial aspiration biopsy is the accepted first step in evaluating a woman with abnormal uterine bleeding or suspected endometrial pathology. Serous and clear cell endometrial carcinomas make up less than 10% of endometrial cancers, yet account for more than one-half of all endometrial cancer deaths. Most patients with endometrial cancer should undergo surgical staging, including hysterectomy, bilateral salpingo-oophorectomy, pelvic and para aortic lymphadenectomy, and peritoneal cytology. Lymphadenectomy may be omitted in patients with negligible risk of lymphatic spread. The most important adverse prognostic variables in endometrial cancer are advancing patient age, nonendometrioid or grade 3 histology, deep myometrial invasion, lymphovascular space invasion, large tumor size, cervical extension, lymph node metastasis, and intraperitoneal spread. Postoperative adjuvant radiotherapy in selected patients with endometrial cancer decreases the risk of local vaginal/pelvic recurrence and improves disease-free survival. Uterine sarcomas are, in general, the most malignant group of uterine tumors and differ from endometrial cancers with regard to risk factors, diagnosis, clinical behavior, pattern of spread, and management. Endometrial carcinoma is the most common malignancy of the female genital tract, accounting for almost one-half of all gynecologic cancers in the United States. In 2011, an estimated 46,470 new cases and 8,120 cancer-related deaths are anticipated. Endometrial carcinoma is the fourth most common cancer, ranking behind breast, lung, and colorectal cancers, and the eighth leading cause of death from malignancy in women. Overall, about 2% to 3% of women develop endometrial cancer during their lifetimes (1). Certain factors are increasing awareness of and emphasis on diagnosis and treatment of endometrial cancer. These factors include the declining incidence of cervical cancer-related deaths in the United States, prolonged life expectancy, postmenopausal use of hormone therapy, and earlier diagnosis. The availability of easily applied diagnostic tools and a clearer understanding of premalignant lesions of the endometrium led to an increase in the number of women diagnosed with endometrial cancer. Although endometrial carcinoma usually presents as early-stage disease and often is managed without radical surgery or radiotherapy, deaths from endometrial carcinoma now exceed those from cervical carcinoma in the United States. Endometrial cancer is a disease that occurs primarily in postmenopausal women and is increasingly virulent with advancing age. The definite role of estrogen in the development of most endometrial cancers is established. Any factor that increases exposure to unopposed estrogen increases the risk for endometrial cancer. The histopathology, spread patterns, and clinicopathologic factors that affect the prognosis of endometrial cancers have become better defined. Management of endometrial cancer evolved from a program of preoperative intrauterine or external pelvic radiation followed by hysterectomy based on clinical staging, to an individualized approach using hysterectomy as primary therapy and employing additional postoperative treatment depending on surgical and pathologic findings. Further analysis and investigation are needed to determine whether this initial operative approach to treatment and staging, followed by targeted postoperative therapy, will translate into improved survival rates and lower morbidity. Type I, accounting for about 75% to 85% of cases, occurs in younger, perimenopausal women with a history of exposure to unopposed estrogen, either endogenous or exogenous. In these women, tumors begin as hyperplastic endometrium and progress to carcinoma. These spontaneously occurring cancers are not associated pathologically with endometrial hyperplasia, but may arise in a background of atrophic endometrium. They are less differentiated and associated with a poorer prognosis than estrogen-dependent tumors. Most of these risk factors are related to prolonged, unopposed estrogen stimulation of the endometrium. Infertility and a history of irregular menses as a result of anovulatory cycles (prolonged exposure to estrogen without sufficient progesterone) increase risk. Natural menopause occurring after age 52 years increases the risk for endometrial cancer 2.
Small bowel obstruction has resulted from direct adhesive processes involving grafts to small bowel (120) mood disorder fun facts aripiprazola 20 mg online. Complete extra peritonealization of the graft using flaps of peritoneum dissected from the prolapsed area and the peritoneum anterior to the sacral promontory and lateral to the right side of the sigmoid colon should prevent this complication anxiety zone symptoms buy aripiprazola canada. However depression symptoms diagnosis cheap 20mg aripiprazola mastercard, loops of bowel have been seen to prolapse through small defects in peritoneal closure with the same effect depression symptoms eyesight order 10 mg aripiprazola with amex. Careful technique with adherence to basic surgical principles may help prevent this and other complications related to laparotomy depression zyrtec buy aripiprazola 10 mg mastercard. Laparoscopic and Robotic Techniques As with most pelvic operations depression definition en francais purchase generic aripiprazola online, sacrocolpopexy has been successfully accomplished by the laparoscopic and robotic route and has the potential to offer patients the benefits of less postoperative discomfort and faster recovery as well as potential lower risks for adhesions and ileus. The applicability of the laparoscopic technique is limited by the need for a relatively high level of technical skill. The authors have also found that straight self-righting needle drivers and non-self-righting curved needle drivers are useful in attaching the mesh to the vagina. The Carter-Thompson suturing device is sometimes helpful to aid in elevating the sigmoid colon away from the pelvic cul-de-sac by tagging the peritoneal edge. The robot has provided an easier platform for a minimally invasive approach to the sacrocolpopexy. Data about its use are limited to several case series that demonstrate comparable short-term results with open and laparoscopic techniques (121). For sacrocolpopexy, whether through laparotomy or laparoscopy, the pelvis should be completely exposed with the lower sigmoid colon stretched cephalad (Fig. A: Illustrates (i) graft attachment to the posterior area of prolapsed vagina to or below the rectal-sigmoid junction after the overlying peritoneum has been dissected and flapped laterally and (ii) exposure of the presacral space with suture placement through the anterior sacral ligament. Prevention of subsequent enterocele and/or sigmoidocele is accomplished by box closure of the cul-de-sac peritoneum lateral to the left side of the sigmoid, attachment of the presigmoid fat to the graft centrally, and reperitorealization of the graft through the right side of the cul de-sac. Two separate loosely woven polypropylene mesh grafts are shaped similar to boat paddles. The paddle portions are secured circumferentially to the fibromuscular layers anteriorly and posteriorly with six to eight monofilament 3-0 nylon sutures and one or two sutures placed centrally (Fig. When the fibromuscular tissue in the area is attenuated, a portion of the vaginal wall is excised and closed, as noted previously. The peritoneum overlying sacral vertebrae 1 and 2 is incised while retracting the sigmoid colon to the left, and careful dissection is employed down to the anterior ligament. Hemoclips are placed caudad and cephalad on the middle sacral vessels if it is felt that this will allow more optimal suture placement. The peritoneal incision is extended into the right cul-de-sac area adjacent to the sigmoid. Closure of the cul-de-sac lateral to the sigmoid on the left and approximation of the distal presigmoid fat to the distal edge of the posterior graft is accomplished with box stitches of 0-delayed absorbable sutures. It is thought that these procedures and the retroperitonealization of the graft through the right side of the cul-de-sac will prevent posterior enterocele and sigmoidocele as well as a Halban or Moschcowitz procedure. Reperitonealization of the graft is then performed using the right cul-de-sac peritoneum and peritoneal flaps dissected from the vaginal apical area; occasionally presigmoid fat is used. Following this procedure, adjunctive procedures, such as paravaginal repair, Burch procedure, midurethral sling, and any transvaginal procedure that is indicated, are performed. When rectocele and pelvic floor defects are present, one option is the sacral colpoperineopexy, as discussed in the posterior compartment section (116). A vaginal pack is inserted for approximately 24 hours to ensure that the graft is well applied to the fibromuscular layer at points other than where sutures are placed. Vaginal Obliterative Procedures Colpocleisis or vaginal narrowing procedures may be appropriate choices for debilitated patients who do not desire vaginal function, because complete vaginal reconstructive procedures may last several hours and are associated with potentially higher blood loss and increased morbidity (132,133). Many variations exist, from partial colpocleisis (where some portion of the vaginal epithelium is left to provide drainage tracts for cervical or upper genital discharge) to total colpectomy (where all of the vaginal epithelium is removed from the hymen posteriorly to within 0. If hysterectomy is performed, blood loss is greater and operative time is longer than procedures without hysterectomy (134). These techniques should include a high perineorrhaphy and often a plication of the puborectalis muscles to reinforce posterior support and to reduce the genital hiatus, with the goal of decreasing the chance of recurrent prolapse. Case series have reported success rates as high as 100%, although the population of patients, by nature of their relatively short life expectancy and limited activity, are probably at lower risk for recurrence. As with the colpocleisis, the success of the procedure is augmented by an extensive perineorrhaphy and puborectalis plication. The prevention or treatment of stress incontinence, voiding dysfunction, and colorectal dysfunction in the context of these procedures can be problematic. Careful preoperative history and evaluation, if indicated, is important so that additional conservative therapies or operative techniques such as pubourethral plications or less invasive tension-free slings may be employed. Management of Urinary Symptoms with Pelvic Organ Prolapse Repair All women who are undergoing surgery for repair of pelvic organ prolapse should be evaluated for urinary incontinence. Women who report stress urinary incontinence and who demonstrate it on preoperative examination and have no contraindications to a continence procedure should have concomitant procedures for the treatment of these symptoms. Women who do not report stress urinary incontinence may also benefit from a prophylactic procedure if they demonstrate incontinence with reduction of their prolapse. There is also evidence that the addition of a continence procedure in the absence of any evidence of urinary incontinence may improve outcomes without significantly increasing the number of complications (135). The addition of continence procedures to prolapse procedures in patients who have both significant stress incontinence and voiding dysfunction remains controversial. Comparison of Abdominal versus Vaginal Approaches In recent years there has been controversy as to whether transvaginal or transabdominal procedures are best for prolapse. One cannot discern which is optimal from reports of retrospective and prospective case series because of the considerable differences in numerous factors, including follow-up, characteristics of the subjects, definitions of success and failure, and the expertise or experience of the surgeons performing the procedures. All three trials showed some increased durability in the sacrocolpopexy group; however, in one of these studies the differences were not statistically significant (138). In the study in which sexual function was examined, there was a greater incidence of dyspareunia in the transvaginal group (137). Most case series reveal that the incidence of serious complications, such as small bowel obstructions, significant hemorrhage, presacral graft infections, pulmonary embolus, and short-term problems. Vaginal scarring, strictures, and vaginal wall erosions or granulation tissue appear more likely in the group undergoing transvaginal surgery. To date, there is no randomized comparison of vaginal procedures using high uterosacral suspensions and innovative repairs of the fibromuscular tissues, which are less likely to produce strictures than was the case 10 or more years ago. Most pelvic surgeons would agree that (i) older, less healthy individuals who are more likely to have surgical and medical complications and cannot or will not tolerate a pessary would derive greater benefit from transvaginal approaches and occasionally obliterative approaches, and (ii) relatively healthy, sexually active women with relatively short vaginas and apical prolapse or with isolated apical defects would derive greater benefit from sacrocolpopexy. For the remainder of the patients with apical prolapse, with or without more distal defects, it would be ideal if surgeons were equally skilled, knowledgeable, and experienced in both abdominal and vaginal approaches to provide care that is truly individualized, rather than emphasizing one approach to the exclusion of another. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. The demographics of pelvic floor disorders: current observations and future projections. Controversies and uncertainties: abdominal versus vaginal surgery for pelvic organ prolapse. Pelvic relaxation and associated risk factors: the results of logistic regression analysis. Case-control study of etiologic factors in the development of severe pelvic organ prolapse. Factors associated with pelvic floor dysfunction with emphasis on urinary and fecal incontinence and genital prolapse: an epidemiologic study. Risk factors associated with pelvic floor disorders in women undergoing surgical repair. The rectovaginal septum revisited: its relationship to rectocele and its importance in rectocele repair. Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Effects of a full bladder and patient positioning on pelvic organ prolapse assessment. Does pelvic organ prolapse quantification exam predict urethral mobility in stages 0 and 1 prolapsefi Nonsurgical management of genital prolapse: a review and recommendations for clinical practice. Multimodality pelvic physiotherapy treatment of urinary incontinence in adult women. Treatment of impaired defecation associated with rectocele by behavioral retraining (biofeedback). Patient satisfaction and changes in prolapse and urinary symptoms in women who were fitted successfully with a pessary for pelvic organ prolapse. Risk factors associated with an unsuccessful pessary fitting trial in women with pelvic organ prolapse. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Long term results following fixation of the vagina on the sacrospinous ligament by the vaginal route. Heterogeneity in anatomic outcome of sacrospinous ligament fixation for prolapse: a systematic review. Recurrent pelvic support defects after sacrospinous ligament fixation for vaginal vault prolapse. Preoperative and postoperative analysis of site-specific pelvic support defects in 81 women treated with sacrospinous ligament suspension and pelvic reconstruction. Bilateral attachment of the vaginal cuff to iliococcygeus fascia: an effective method of cuff suspension. Repair of vaginal vault prolapse by suspension of the vagina to iliococcygeus (prespinous) fascia. Posterior culdoplasty: surgical correction of enterocele during vaginal hysterectomy: a preliminary report. A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. High uterosacral vaginal vault suspension with fascial reconstruction for vaginal repair of enterocele and vaginal vault prolapse. Bilateral uterosacral ligament vaginal vault suspension with site specific endopelvic fascia defect repair for treatment of pelvic organ prolapse. Outcomes of vaginal vault prolapse repair with a high uterosacral suspension procedure utilizing bilateral single sutures. Transabdominal repair of cystocele, a 20 year experience, compared with the traditional vaginal approach. Clinical and urodynamic effects of anterior colporrhaphy and vaginal hysterectomy for prolapse with and without incontinence. Incidence of recurrent cystocele after anterior colporrhaphy with and without concomitant transvaginal needle suspension. Cystocele: a radical cure by suturing lateral sulci of vagina to white line of pelvic fascia. Suprapubic vesicourethral suspension as a primary means of correcting stress incontinence and cystocele. A six-year experience with paravaginal defect repair for stress urinary incontinence. Surgical management of prolapse of the anterior vaginal segment: an analysis of support defects, operative morbidity, and anatomic outcome. Paravaginal defect repair in the treatment of female stress urinary incontinence and cystocele. Anatomic and functional outcome of vaginal paravaginal repair in the correction of anterior vaginal wall prolapse. Fascial and muscular abnormalities in women with urethral hypermobility and anterior vaginal wall prolapse. Infections related to placement of permanent braided and mono-filament suture material through vaginal mucosa. Sexual function and vaginal anatomy in women before and after surgery for pelvic organ prolapse and urinary incontinence. Transanal or vaginal approach to rectocele repair: a prospective randomized pilot study. Selection criteria for anterior rectal wall repair in symptomatic rectocele and anterior rectal wall prolapse. Outcomes after anterior vaginal wall repair with mesh: a randomized, controlled trial with a 3 year follow-up. Tension-free vaginal mesh procedure for pelvic organ prolapse: a single center experience of 310 cases with 1-year follow up. Low-weight polypropylene mesh for anterior vaginal wall prolapse: a randomized controlled trial. Vaginal repair with mesh versus colporrhaphy for prolapse: a randomized controlled trial. Abdominal sacral colpoperineopexy: a new approach for correction of posterior compartment defects and perineal descent associates with vaginal vault prolapse.
Buy cheap aripiprazola 15 mg line. Major Depressive Disorder Symptoms.
References
- Patel CG, Michaelson E, Chen YH, et al. Reduced mortality risk in the recent era in early-stage Hodgkin lymphoma patients treated with radiation therapy with or without chemotherapy. Int J Radiat Oncol Biol Phys 2018;100(2):498-506.
- Corti R., Farkouh ME, Badimon, JJ. The vulnerable plaque and acute coronary syndromes. Am J Med. 2002;113:668-680.
- Meinck HM, Goebel HH, Rumpf KW, Kaiser H, Neumann P. The forearm ischaemic work test-hazardous to McArdle's patients? J Neurol Neurosurg Psychiatry. 1982;45:1144-1146.
- Tonelli M, Wiebe N, James MT, et al: A population-based cohort study defines prognoses in severe chronic kidney disease, Kidney Int 93(5):1217n1226, 2018.
- Muir KW, McNeish I, Grosset DG, et al. Visualization of cardiac emboli from mitral valve papillary fibroelastoma. Stroke 1996; 27:1133-4.