Emily J. Ozer PhD
- Professor, Community Health Sciences

https://publichealth.berkeley.edu/people/emily-ozer/
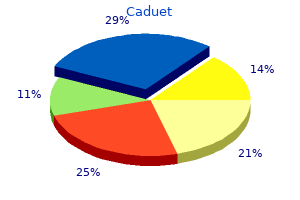
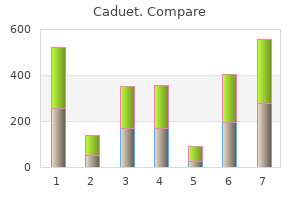
Caution should be exercised in patients with relevant cardiac disorders [see Boxed Warning cholesterol vitamins buy caduet overnight, Warnings and Precautions (5 cholesterol foods to lower buy caduet online pills. In the event of overdose high cholesterol medication erectile dysfunction buy 5mg caduet amex, observe the patient and provide appropriate supportive treatment cholesterol test code buy cheap caduet 5 mg on line. The chemical name of nilotinib monohydrochloride monohydrate is 4-methyl-N-[3-(4-methyl-1H-imidazol-1 yl)-5-(trifluoromethyl)phenyl]-3-[[4-(3-pyridinyl)-2-pyrimidinyl]amino]-benzamide cholesterol upper limit caduet 5 mg amex, monohydrochloride cholesterol hdl ratio reference range order caduet cheap, monohydrate. Its structure is shown below: Tasigna (nilotinib) capsules, for oral use, contain 50 mg, 150 mg, or 200 mg nilotinib base, anhydrous (equivalent to 55 mg, 166 mg, and 221 mg nilotinib monohydrochloride monohydrate respectively) with the following inactive ingredients: colloidal silicon dioxide, crospovidone, lactose monohydrate, magnesium stearate, and poloxamer 188. The capsules contain gelatin, iron oxide (red), iron oxide (yellow), iron oxide (black), and titanium dioxide. Based on exposure-response analyses for safety, a relationship between exposure and a greater likelihood of safety events, including a higher occurrence of total bilirubin elevations, was observed in clinical studies. An increase in serum exposure to nilotinib between the first dose and steady state was approximately 2-fold for daily dosing and 3. The average steady state nilotinib trough and peak concentrations did not change over 12 months. Absorption Relative bioavailability of nilotinib capsule is approximately 50%, as compared to an oral drink solution (pH of 1. Median steady-state trough concentration of nilotinib was decreased by 53% in patients with total gastrectomy compared to patients who had not undergone surgeries [see Warnings and Precautions (5. Single dose administration of two 200 mg nilotinib capsules each dispersed in 1 teaspoon of applesauce and administered within 15 minutes was shown to be bioequivalent to a single dose administration of two 200 mg intact capsules. None of the metabolites contribute significantly to the pharmacological activity of nilotinib. Excretion After a single dose of radiolabeled nilotinib, more than 90% of the administered dose was eliminated within 7 days: 93% of the dose in feces. Specific Populations Age, sex, race/ethnicity, or body weight did not significantly affect the pharmacokinetics of nilotinib. Pediatric Patients Following administration of the approved recommend pediatric dosage of nilotinib, steady-state exposure of nilotinib were within 2-fold to adult patients treated with 400 mg twice daily. No significant change in nilotinib pharmacokinetics was observed when a single 400 mg dose of Tasigna was administered 10 hours after and 2 hours before famotidine (an H2 blocker), or administered 2 hours after and 2 hours before an antacid. Nilotinib induced in the skin and subcutis statistically significant increases in the incidence of papillomas in females and of papillomas and combined papillomas and carcinomas in males at 300 mg/kg/day. In a study where male and female rats were treated with nilotinib at oral doses of 20 to 180 mg/kg/day (approximately 1 to 6. Efficacy was based on a total of 846 patients: 283 patients in the imatinib 400 mg once daily group, 282 patients in the Tasigna 300 mg twice daily group, 281 patients in the Tasigna 400 mg twice daily group. Median age was 46 years in the imatinib group and 47 years in both Tasigna groups, with 12%, 13%, and 10% of patients greater than or equal to 65 years of age in imatinib 400 mg once daily, Tasigna 300 mg twice daily and Tasigna 400 mg twice daily treatment groups, respectively. There were slightly more male than female patients in all groups (56%, 56%, and 62% in imatinib 400 mg once daily, Tasigna 300 mg twice daily and Tasigna 400 mg twice daily treatment groups, respectively). The primary data analysis was performed when all 846 patients completed 12 months of treatment (or discontinued earlier). Subsequent analyses were done when patients completed 24, 36, 48, and 60 months of treatment (or discontinued earlier). The median time on treatment was approximately 61 months in all three treatment groups. Two patients in the Tasigna arm progressed to either accelerated phase or blast crisis (both within the first 6 months of treatment) while 12 patients on the imatinib arm progressed to either accelerated phase or blast crisis (7 patients within first 6 months, 2 patients within 6 to 12 months, 2 patients within 12 to 18 months and 1 patient within 18 to 24 months). Cytogenetic responses were based on the percentage of Ph+ metaphases among greater than or equal to 20 metaphase cells in each bone marrow sample. The definition of imatinib resistance included failure to achieve a complete hematologic response (by 3 months), cytogenetic response (by 6 months) or major cytogenetic response (by 12 months) or progression of disease after a previous cytogenetic or hematologic response. Imatinib intolerance was defined as discontinuation of treatment due to toxicity and lack of a major cytogenetic response at time of study entry. Overall, 73% of patients were imatinib resistant while 27% were imatinib intolerant. Prior therapy included hydroxyurea in 85% of patients, interferon in 56% and stem cell or bone marrow transplant in 8%. Cytogenetic responses were based on the percentage of Ph-positive metaphases among greater than or equal to 20 metaphase cells in each bone marrow sample. The median time to first hematologic response among responders was 1 month (range 1 to 14 months). Efficacy was based on the 96-week analysis data cut-off date, by which time, 91 patients (47. The median actual dose intensity during the 52-week Tasigna consolidation phase was 771. Efficacy was based on the 96-week analysis data cut-off date, by which time, 61 patients (48. In 2 both studies, patients received Tasigna treatment at a dose of 230 mg/m twice daily, rounded to the nearest 50 mg dose (to a maximum single dose of 400 mg). The complete text of the Medication Guide is reprinted at the end of this document. Myelosuppression Advise patients that treatment with Tasigna can cause serious thrombocytopenia, neutropenia, and anemia. Advise patients to seek immediate medical attention if symptoms suggestive of low blood counts occur, such as fever, chills or other signs of infection, unexplained bleeding or bruising, or unexplained weakness or shortness of breath [see Warnings and Precautions (5. Advise patients to seek immediate medical attention if symptoms of abnormal heart beat occur, such as feeling light-headed, faint or experiencing an irregular heartbeat [see Warnings and Precautions (5. Cardiac and Arterial Vascular Occlusive Events Advise patients that cardiovascular events (including ischemic heart disease, peripheral arterial occlusive disease, and ischemic cerebrovascular events) have been reported. Advise patients to seek immediate medical attention if any symptoms suggestive of a cardiovascular event occur, such as chest or leg pain, numbness or weakness, or problems walking or speaking occur suddenly [see Warnings and Precautions (5. Pancreatitis and Elevated Serum Lipase Advise patients that Tasigna can increase the risk of pancreatitis and that patients with a previous history of pancreatitis may be at greater risk. Advise patients to seek immediate medical attention if symptoms suggestive of pancreatitis occur, such as sudden stomach area pain with accompanying nausea and vomiting [see Warnings and Precautions (5. Hepatotoxicity Advise patients that Tasigna can increase the risk of hepatotoxicity and that patients with previous history of liver diseases may be at risk. Advise patients to seek immediate medical attention if any symptoms suggestive of hepatotoxicity occur, such as stomach pain, yellow skin and eyes, and dark-colored urine [see Warnings and Precautions (5. Taking Tasigna Advise patients to take Tasigna doses twice daily approximately 12 hours apart. No food should be consumed for at least 2 hours before the dose is taken and for at least 1 hour after the dose is taken. If the patient missed a dose of Tasigna, the patient should take the next scheduled dose at its regular time. Should patients be unable to swallow capsules, the contents of each capsule may be dispersed in one teaspoon of applesauce and the mixture swallowed immediately (within 15 minutes). Tumor Lysis Syndrome Advise patients that Tasigna can cause tumor lysis syndrome and to seek immediate medical attention if any symptoms suggestive of tumor lysis syndrome occur such as an abnormal heartbeat or less urine production [see Warnings and Precautions (5. Advise patients to seek immediate medical attention if symptoms suggestive of hemorrhage occur, such as uncontrolled bleeding, changes in eyesight, unconsciousness, or sudden headache or sudden confusion in surroundings [see Warnings and Precautions (5. Fluid Retention Advise patients that Tasigna can cause fluid retention and to seek immediate medical attention if any symptoms suggestive of fluid retention such as shortness of breath, rapid weight gain, or swelling occur [see Warnings and Precautions (5. Effects on Growth and Development in Pediatric Patients Inform pediatric patients and their caregivers of the possibility of developing growth abnormalities. Therefore, monitor growth and development in pediatric patients [see Warnings and Precautions (5. Advise patients that musculoskeletal symptoms such as muscle pain, pain in extremity, joint pain, bone pain, or spinal pain, may occur more frequently than before treatment discontinuation [see Warnings and Precautions (5. Drug Interactions Advise patients that Tasigna and certain other medicines, including over the counter medications or herbal supplements (such as St. Embryo-Fetal Toxicity Advise females to inform their healthcare provider if they are pregnant or become pregnant. Inform female patients of the risk to a fetus and potential loss of the pregnancy [see Use in Specific Populations (8. Advise females of reproductive potential to use effective contraception during treatment and for at least 14 days after receiving the last dose of Tasigna [see Warnings and Precautions (5. Lactation Advise lactating women not to breastfeed during treatment with Tasigna and for at least 14 days after the last dose [see Use in Specific Populations (8. The long-term effects of treating children with Tasigna for a long period of time are not known. Tell your healthcare provider right away if you are pregnant, or if you become pregnant during treatment with Tasigna. Your healthcare provider should do a pregnancy test before you start treatment with Tasigna. Do not breastfeed during treatment and for at least 14 days after your last dose of Tasigna. Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins and herbal supplements. If you need to take antacids (medicines to treat heartburn) do not take them at the same time that you take Tasigna. Tasigna can interact with many medicines and supplements and increase your chance for serious and life-threatening side effects. The tests will check your: o heart o blood cells (white blood cells, red blood cells, and platelets). Your blood cells should be checked every 2 weeks for the first 2 months and then monthly. Your healthcare provider may have you stop Tasigna for some time or lower your dose if you have side effects with it. After at least 3 years of treatment with Tasigna, your healthcare provider may do certain tests to determine if you continue to be in remission. Based on your test results, your healthcare provider may decide if you may be eligible to try stopping treatment with Tasigna. Low blood cell counts (red blood cells, white blood cells, and platelets) are common with Tasigna, but can also be severe. Your healthcare provider will check your blood counts regularly during treatment with Tasigna. Call your healthcare provider or get medical help right away if you develop any signs or symptoms of low blood counts including: o fever o chills or other signs of infection o unexplained bleeding or bruising o unexplained weakness o shortness of breath. Get medical help right away if you suddenly develop any of the following symptoms:? Tell your healthcare provider right away if you develop any symptoms of pancreatitis including sudden stomach area pain with nausea and vomiting. People who have had liver problems in the past may be at risk for getting liver problems with Tasigna. Tell your healthcare provider right away if you develop any signs and symptoms of bleeding during treatment with Tasigna. Symptoms of fluid retention include shortness of breath, rapid weight gain, and swelling. Some children and adolescents may have slower than normal growth during treatment with Tasigna. Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not give Tasigna to other people, even if they have the same symptoms that you have. You can ask your pharmacist or healthcare provider for information about Tasigna that is written for health professionals. Active ingredient: nilotinib Inactive ingredients: colloidal silicon dioxide, crospovidone, lactose monohydrate, magnesium stearate and poloxamer 188. The capsules contain gelatin, iron oxide (red), iron oxide (yellow), iron oxide (black), and titanium dioxide. Distributed by: Novartis Pharmaceuticals Corporation, East Hanover, New Jersey 07936 Novartis T2019-109 For more information, go to Most of the complications are associated with a Third molar surgery is the most common procedure greater degree of impaction. There is also a and, where possible, offers a preventive or management strat relation between tooth position based on the Winter classi egy. Complications, such as pain, dry socket, swelling, fication and the appearance of postoperative complications. Factors thought to in with nearly twice as many complications as the other tooth fluence the incidence of complications after third molar re positions [3]. Other authors state that horizontal and moval include age, gender, medical history, oral contracep distoangular impactions are inclined to develop more com tives, presence of pericoronitis, poor oral hygiene, smoking, plications [4]. Deep impacted third molar surgery needs a type of impaction, relationship of third molar to the inferior bigger flap design. Tissues in the neighborhood and mus alveolar nerve, surgical time, surgical technique, surgeon cles can receive more damage because of this wide and large experience, use of perioperative antibiotics, use of topical access flap [5]. These associations For the general dental practitioner, as well as the oral result from the fact that the intervention in older patients and maxillofacial surgeon, it is important to be familiar with lasts longer because of increased bone density. This im maturing of tooth root formation and decreased healing ca proves patient education and leads to prevention, early rec pacity lead to intensive postoperative complications. Key words: third molar surgery, complication, man It seems that female patients show higher accident and dible, maxilla complication rates [1]. Surgical removal of impacted third molars is one of the experience of surgeon also appears to be a deter the most common procedures carried out in oral and maxil mining factor in the development of postoperative compli lofacial surgery. Most third molar surgeries are performed cations and can result in a longer treatment process, social without complications.
Although every effort time in which it is deemed safe for them to be discharged to the care should be made to select appropriately sized equipment before the of a supervising adult (44) cholesterol in eggs mg proven caduet 5 mg. In addition good bad cholesterol foods list caduet 5mg, providing a reasonable start of each procedure definition of no cholesterol purchase 5mg caduet overnight delivery, units should be designed so that access to variety of age-appropriate choices to advance the diet in the scopes of different sizes cholesterol juice recipes buy caduet toronto, as well as their corresponding accessories cholesterol medication pravachol discount 5mg caduet with amex, postprocedural area will help meet the needs of the variety of can occur in a timely manner in cases of an unforeseen scope/size patients who will be encountered cholesterol hdl ratio low cheap caduet american express. As routine biopsies of normal appearing mucosa during allows for the early reuniting of patients and family members in upper and lower endoscopy are still standard practice in the the postprocedural period can alleviate anxiety of family members pediatric population, preparations should be made appropriate and patients alike. As these procedures are performed with decreased help fill this gap and serve as a working reference document for frequency in the pediatric population it is prudent to attempt to those pediatric centers developing endoscopy programs. Endoscopy and Procedures Committee members was also a critical Ann Intern Med 2003;139:843?57. Ethical issues in endoscopy: patient satisfaction, safety in elderly patients, palliation, and relations with industry. Equipment for pediatric digestive disease endoscopy unit: report of the World Endoscopy endoscopy. Interim Protocol for Healthcare Facilities Regarding Surveillance deployment of capsule endoscope in the pediatric population. American Academy of Pediatrics, American Academy of Pediatric Analg 1998;86:896?906. Impact of pre-procedure interventions on no of pediatric patients during and after sedation for diagnostic and show rate in pediatric endoscopy. As per copyright regulations, any unauthorised use of the material or parts thereof as well as commercial reproduction or multiple distribution by any traditional or electronically based reproduction/publication method ist strictly prohibited. Please note: Links to movies, ppt slideshows and any other multimedia files are not available in the pdf version of presentations. Background Embolization is defined as nonsurgical minimally invasive procedure involving the introduction of embolic material in blood vessel in order to achieve its occlusion. Therefore the remaining 20-25% of cases require further intervention, requiring a multidiscplinary approach, involving the interventional radiologist, the surgeon, and the gastroenterologist. The radiologist acts as an element of a multidisplinary team, having a crucial role ranging between the diagnosis and treatment, and has two primordial functions: 1. Try to establish the etiologic diagnosis the imaging techniques used in the context of the gastrointestinal haemorrhage are: However we should refer that indications vary according to institution expertise and availability. References: Medical Imaging Department and Faculty of Medicine, University Hospital of Coimbra, Portugal. References: Medical Imaging Department and Faculty of Medicine, University Hospital of Coimbra, Portugal In both celiac trunk and superior mesenteric artery angiograms imaging is performed until the portal venous phase to document patency of the portal vein Fig. References: Medical Imaging Department and Faculty of Medicine, University Hospital of Coimbra, Portugal. References: Medical Imaging Department and Faculty of Medicine, University Hospital of Coimbra, Portugal. If hemorrhage not evident in the context of upper gastrointestinal bleeding, selective catheterization of the left gastric artery and gastroduodenal artery is performed. Indirect signs of bleeding include pseudoaneurysm, vessel spasm or cut-off, early venous filling and hypervascularity. The presence of abnormal blush may indicate an inflammatory process, which may represent a bleeding source. In mapping aortography detection is only possible with massive bleeding rates (6 mL/min). This patient went to the angiography room and the selective catheterization of the inferior mesenteric artery identified the bleeding site at the vasa recta of the marginal artery (image d). A microcatheter was coaxially introduced into the 5 Fr catheter and successful microcoil embolization of the bleeding vessel was achieved (image e). Pre-procedural knowledge of the haemorrhage allowed for initial catheterization of the inferior mesenteric artery resulting in less delay. References: Medical Imaging Department and Faculty of Medicine, University Hospital of Coimbra, Portugal. In fact this was the second angiography in 3 days, in the first one no active bleeding was detected. So in this case superselective catheterization of the superior mesenteric artery branches was performed and suggestion of bleeding was found in branches of the right colic artery were a small cluster of small arteries was found (arrow in image a). These findings were consistent with angiodysplasia and superselective microcoil embolization at the vasa recta was performed (image b), the patient underwent uneventful clinical and laboratorial recovery. References: Medical Imaging Department and Faculty of Medicine, University Hospital of Coimbra, Portugal Cases of upper gastrointestinal haemorrhage. References: Medical Imaging Department and Faculty of Medicine, University Hospital of Coimbra, Portugal. Before embolization a balloon was inflated (image c) due to the critical status in order to "gain" some time before coil embolization was performed together with gelfoam (image d). The superior mesenteric artery was studied (not shown) and no "backdoor" to the bleeding site was found. References: Medical Imaging Department and Faculty of Medicine, University Hospital of Coimbra, Portugal Page 28 of 51 Fig. Bleeding site was successfully embolized with microcoils achieving stoppage of the bleeding (image c). References: Medical Imaging Department and Faculty of Medicine, University Hospital of Coimbra, Portugal. This patient had already performed a endoscopy that detected fresh blood, but due to the massive haemorrhage the bleeding site could not be detected. Hemodynamically unstable patients such as this one should immediately undergo arteriography with team support of intensive care physician, conversely arteriography in hemodynamically stable patients with low volume haemorrhage is likely to be fruitless, and Page 29 of 51 is best reserved for cases in which all other standard workup has failed to localize or characterize the source of bleeding. The bleeding site once identified was embolized successfully with microcoils, and the patient recovered almost immediately, namely with stabilization of blood pressure. References: Medical Imaging Department and Faculty of Medicine, University Hospital of Coimbra, Portugal. The patient went to the angiography room and the bleeding site was identified and embolized with coils (images b and c) as a palliative measure. References: Medical Imaging Department and Faculty of Medicine, University Hospital of Coimbra, Portugal. Computed tomography (images a and b) disclosed hemorrhage around the biliary prosthesis with extravasation into the bowel lumen (arrows). The bleeding site was identified in the superior mesenteric artery and it was stopped by deploying a covered stent (images c and d). References: Medical Imaging Department and Faculty of Medicine, University Hospital of Coimbra, Portugal. After selective catheterization of the right hepatic artery a pseudoaneurysm is seen (arrows in images a and b), which was occluded by microcoil embolization (image c) and the haemobilia ceased following embolization. References: Medical Imaging Department and Faculty of Medicine, University Hospital of Coimbra, Portugal. After selective catheterization of the celiac trunk (not shown) and superior mesenteric artery a pseudoaneurysm is seen in the dependence of the inferior pancreaticoduodenal artery (images a and b). Successful embolization was achieved wit microcoils occluding the bleeding (image c). Following cessation of active haemorrhage, there is a high risk of recurrence specially within the first 48 to 72 hours. Each episode of bleeding carries a 30% mortality rate and the risk of rebleeding is high (60 to 70%) until the gastro oesophageal varices are treated. Direct portography shows significant collateralization to the left gastric vein, opacifying above the diaphragm, the left portal vein was not seen (image a). After catheterization of the bleeding artery the only coil available was oversized and partial migration into the superior mesenteric artery occurred (image c). This complication was resolved by placing the guidewire downstream the coil and deploying the stent(image d), thus compressing the coil and maintaining normal permeability of the superior mesenteric artery. References: Medical Imaging Department and Faculty of Medicine, University Hospital of Coimbra, Portugal. Minor complications are more frequent and include ileus, abdominal pain, hypotension, etc. At the superior mesenteric artery angiogram a suspicious area at the topography of the right colic artery was seen (image a), and superselective catheterization confirmed the bleeding (image b). Coil embolization was performed, but was not sufficient to stop the bledding (image c), so gelfoam was also applied occluding the haemorrhage. This case is illustrative of the need and utility of computed tomography scans in patients with gastrointestinal haemorrhage and previous surgery. Page 35 of 51 References: Medical Imaging Department and Faculty of Medicine, University Hospital of Coimbra, Portugal. In most instances small areas of infarction are well tolerated and do not require surgery being self-limited. This rebleeding is more frequent with inflammatory lesions and arteriovenous malformations. This patient went to the angiography room and the selective catheterization of the inferior mesenteric artery identified the bleeding site at the vasa recta of the marginal artery (image d). A microcatheter was coaxially introduced into the 5 Fr catheter and successful microcoil embolization of the bleeding vessel was achieved (image e). Pre-procedural knowledge of the haemorrhage allowed for initial catheterization of the inferior mesenteric artery resulting in less delay. In fact this was the second angiography in 3 days, in the first one no active bleeding was detected. So in this case superselective catheterization of the superior mesenteric artery branches was performed and suggestion of bleeding was found in branches of the right colic artery were a small cluster of small arteries was found (arrow in image a). These findings were consistent with angiodysplasia and superselective microcoil embolization at the vasa recta was performed (image b), the patient underwent uneventful clinical and laboratorial recovery. Before embolization a balloon was inflated (image c) due to the critical status in order to "gain" some time before coil embolization was performed together with gelfoam (image d). The Page 43 of 51 superior mesenteric artery was studied (not shown) and no "backdoor" to the bleeding site was found. Bleeding site was successfully embolized with microcoils achieving stoppage of the bleeding (image c). This patient had already performed a endoscopy that detected fresh blood, but due to the massive haemorrhage the bleeding site could not be detected. Hemodynamically unstable patients such as this one should immediately undergo arteriography with team support of intensive care physician, conversely arteriography in hemodynamically stable patients with low volume haemorrhage is likely to be fruitless, and is best reserved for cases in which all other standard workup has failed to localize or characterize the Page 44 of 51 source of bleeding. The bleeding site once identified was embolized successfully with microcoils, and the patient recovered almost immediately, namely with stabilization of blood pressure. The patient went to the angiography room and the bleeding site was identified and embolized with coils (images b and c) as a palliative measure. Computed tomography (images a and b) disclosed hemorrhage around the biliary prosthesis with extravasation into the bowel lumen (arrows). The bleeding site was identified in the superior mesenteric artery and it was stopped by deploying a covered stent (images c and d). After selective catheterization of the right hepatic artery a pseudoaneurysm is seen (arrows in images a and b), which was occluded by microcoil embolization (image c) and the haemobilia ceased following embolization. After selective catheterization of the celiac trunk (not shown) and superior mesenteric artery a pseudoaneurysm is seen in the dependence of the inferior pancreaticoduodenal artery (images a and b). Successful embolization was achieved wit microcoils occluding the bleeding (image c). Direct portography shows significant collateralization to the left gastric vein, opacifying above the diaphragm, the left portal vein was not seen (image a). After catheterization of the bleeding artery the only coil available was oversized and partial migration into the superior mesenteric artery occurred (image c). This complication was resolved by placing the guidewire downstream the coil and deploying the stent(image d), thus compressing the coil and maintaining normal permeability of the superior mesenteric artery. At the superior mesenteric artery angiogram a suspicious area at the topography of the right colic artery was seen (image a), and superselective catheterization confirmed the bleeding (image b). Coil embolization was performed, but was not sufficient to stop the bledding (image c), so gelfoam was also applied occluding the haemorrhage. This case is illustrative of the need and utility of computed tomography scans in patients with gastrointestinal haemorrhage and previous surgery. Percutaneous arterial embolization could be the initial treatment in any patient with bleeding severe enough to require angiography, namely in unstable patients, and in whom superselective catheterization is possible. Personal information Servico de Imagiologia Centro Hospitalar Tondela-Viseu Hospital S. Navuluri R, Patel J, Kang L (2012) Role of interventional radiology in the emergent management of acute upper gastrointestinal bleeding. Current approaches to treatment ofCurrent approaches to treatment of chronic hepatitis Bchronic hepatitis B Drug typesDrug types Treatment durationTreatment duration? In Gothenburg 50% of the patients had alcoholic cirrhosis compared to 29% in Iceland (p<0. Only 9% of patients died in their first variceal bleeding, that is within one week of their first bleeding episode. Of the patients diagnosed with esophageal varices after a bleeding episode, 55% had a bleeding episode during follow-up compared to only 13% of the patients diagnosed without a bleeding episode. Variables predicting mortality in a multivariate analysis were: Child-Pugh class, bleeding before diagnosis, age and bilirubin levels. Causes of death were in 26% of cases liver failure, 19% variceal bleeding and the rest other causes. Patients with liver cirrhosis had 267 times increased risk of hepatocellular cancer. We observed 13 times increased risk of cholangiocarcinoma and also increased risk for esophageal, pancreatic, pulmonary and colorectal cancer than in the general population. Patients with liver cirrhosis and portal hypertension had more motility disturbances in the small intestine compared to those without portal hypertension and seemed to have a higher risk of small intestinal bacterial overgrowth. Conclusions: the incidence of liver cirrhosis is low in Iceland, 24% of the incidence in Gothenburg.
Cheap 5 mg caduet fast delivery. Statins - who needs them anyways?.
Syndromes
- Electrocautery or laser surgery to treat frequent or heavy nosebleeds
- · Do not buy food from street vendors.
- You are unable to care for a person with dementia at home
- Taking "loop diuretics" to reduce potassium and fluid levels if you have chronic kidney failure
- Backflow of bile into the stomach (bile reflux)
- Balance testing (ENG)
- The person has a history of severe allergic reactions (check for a medical ID tag).
References
- Bell WH, Jacobs J, Quejada J. Simultaneous repositioning of the maxilla, mandible, and chin. Treatment planning and analysis of soft tissues. Am J Orthod 1986;89:28-50.
- Sitzia J, Wood N: Patient satisfaction: a review of issues and concepts, Soc Sci Med 45(12):1829n1843, 1997.
- Yag-Howard C: Sutures, needles, and tissue adhesives: a review for dermatologic surgery. Dermatol Surg 40:S3-S15, 2014.
- Bihari D, Gimson A, Waterson M, et al. Tissue hypoxia during fulminant hepatic failure. Crit Care Med. 1985;13(12): 1034-1039.
- Ewy GA. Inotropic infusions for chronic congestive heart failure: medical miracles or misguided medicinals? J Am Coll Cardiol 1999;33:572.
- Khan TZ, Khan RM. Changes in serum potassium following succinylcholine in patients with infections. Anesth Analg. 1983;62(3):327-331.
- Dalmau J, Furneaux HM, Rosenblum MK, Graus F, Posner JB. Detection of the anti-Hu antibody in specific regions of the nervous system and tumor from patients with paraneoplastic encephalomyelitis/sensory neuronopathy. Neurology. 1991;41:1757-1764.