Susie Wiegert Villalobos, MPH, LDN, RD
- Program Coordinator/Dietitian
- Tulane Center for Diabetes/
- Endocrine Weight Management Program
- Tulane Medical Center?akeside Campus
- New Orleans, LA
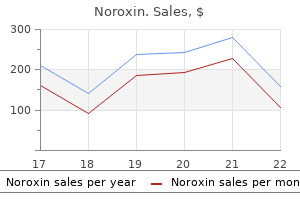
Cyclosporin A (CyA) (24) and methotrexate (25) were initially evaluated in open studies infection game purchase discount noroxin, with a good effect on pain antimicrobial nail polish discount noroxin 400mg line, but a limited effect on urgency and frequency antimicrobial mechanism of action purchase 400mg noroxin with mastercard. In 23 patients antibiotics make me feel weird order 400 mg noroxin free shipping, daily voiding antibiotics for mild acne buy 400mg noroxin amex, maximal bladder capacity bacteria zapper for face buy noroxin 400mg without a prescription, and voided volume improved significantly after 1 year of treatment. However, there were more adverse events in the CyA arm (including induced hair growth, gingival pain and hyperplasia, paraesthesia in the extremities, abdominal pain, flushing, muscle pain and shaking), and only 29 patients completed the 6 months follow-up in both groups. Gabapentin is an antiepileptic drug, which is used as adjunctive treatment in painful disorders. In an uncontrolled dose-escalation protocol with 21 chronic genitourinary pain patients (29), 10 improved with gabapentin at 6 months. No major side effects occurred and therapeutic effects correlated with a reduction in blood eosinophils, IgE and urinary T cells (31). Opioids for chronic prostatitis and interstitial cystitis: lessons learned from the 11th World Congress on Pain. A prospective, randomized, placebo controlled, doubleblind study of amitriptyline for the treatment of interstitial cystitis. Efficacy of pentosan polysulfate in the treatment of interstitial cystitis: a meta-analysis. Randomized, double-blind, dose-ranging study of pentosan polysulfate sodium for interstitial cystitis. Safety and efficacy of concurrent application of oral pentosan polysulfate and subcutaneous low-dose heparin for patients with interstitial cystitis. Treatment of interstitial cystitis with immunosuppression and chloroquine derivatives. Long-term outcome of patients with interstitial cystitis treated with low dose cyclosporine A. Cyclosporine A and pentosan polysulfate sodium for the treatment of interstitial cystitis: a randomized comparative study. In an uncontrolled study, significant immediate symptom relief was reported in 94% of patients and sustained relief after 2 weeks in 80%, using instillations of combined heparin and alkalinised lidocaine [40, 000 U heparin, 2% lidocaine (160 mg), and 3 mL 8. At 3 months, four patients in the pentosan polysulphate sodium group and two in the placebo group achieved significant symptomatic relief. At week 18, the treatment group showed significant improvement in all health-related QoL domains compared to baseline (P 0. In over half of the patients, intravesical heparin controlled the symptoms, with continued improvement after 1 year of therapy. Voiding frequency, pain scores and maximum cystometric capacity were significantly better after 2 and 12 months compared to pretreatment values. Visual analogue scale scores showed symptom relief due to hyaluronic acid therapy, irrespective of bladder capacity. Long-term effects were investigated in a study of 70 patients previously treated with hyaluronan. Intravesical chondroitin sulphate (16) demonstrated beneficial effects in patients with a positive potassium stimulation test, in two non-randomised, uncontrolled, open-label pilot studies. Steinhoff (17) treated 18 patients with 40 mL instilled intravesically once weekly for 4 weeks and then once monthly for 12 months. It did not improve overall symptoms, pain, urgency, frequency, nocturia, or average void volume during 12 weeks follow-up. Among 12 patients (one drop-out for severe pain), the overall satisfaction rate was 58. A placebo-controlled study of intravesical pentosanpolysulphate for the treatment of interstitial cystitis. Urodynamic results of intravesical heparin therapy for women with frequency urgency syndrome and interstitial cystitis. Intravesical hyaluronic acid in the treatment of refractory interstitial cystitis. Do cystometric findings predict the results of intravesical hyaluronic acid in women with interstitial cystitis A real-life multicentre clinical practice study to evaluate the efficacy and safety of intravesical chondroitin sulphate for the treatment of interstitial cystitis. Critical appraisal of dimethyl sulfoxide treatment for interstitial cystitis:discomfort, side-effects and treatment outcome. Followup of patients with interstitial cystitis responsive to treatment with intravesical bacillus Calmette-Guerin or placebo. A light and electron-microscopic histopathological study of human bladder mucosa after intravesical resiniferatoxin application. A prospective, double-blind, randomized cross-over study evaluating changes in urinary pH for relieving the symptoms of interstitial cystitis. In 1957, an uncontrolled retrospective study was presented by Franksson (4), who treated 33 patients with repeated, up to 10-fold, distensions. These results disagree with those of Badenoch (7), who failed to note any improvement in 44/56 patients after hydrodistension. Treatment efficacy in the 33 retrospectively and 32 prospectively studied patients was 38% and 60% at 6 months, and 22% and 43% at 1 year, respectively. Overall, hydrodistension was effective for ~70% of patients for > 3 months, without serious complications. Bladder distension altered levels of urine antiproliferative factor and heparin-binding epidermal-growth-factor-like growth factor towards normal. Significant bladder enlargement was achieved and voiding symptoms and pain decreased. Upon symptom recurrence, treatments were repeated with equal efficacy in 11 patients. Endourological ablation of bladder tissue aims to eliminate urothelial, mostly Hunner, lesions. Relapse was noted in one-third of patients after 2-20 months, while the remaining two-thirds were still pain-free after 2-42 months. Follow-up at 3-15 months revealed no relapse, except for mild recurrent voiding symptoms. In the group without ulcers, only 20 of 49 patients improved, of whom 10 required further therapy within 1 year. None of the patients became symptom-free; two showed only limited improvement in bladder capacity and pain score. To ascertain effect of repeat injections a total of 13 patients were followed up for 2 years, while 58 injections were administered with a mean of 4. Hyperbaric oxygenation resulted in a decrease of baseline urgency and pain (P < 0. Permanent sacral neuromodulation implantation was performed in patients who showed at least 50% improvement in their symptoms with a temporary peripheral nerve evaluation test. Prolonged bladder distension: experience in the treatment of detrusor overactivity and interstitial cystitis. Prolonged hydrodistention of the bladder for symptomatic treatment of interstitial cystitis: efficacy at 6 months and 1 year. Trigonal injection of botulinum toxin A in patients with refractory bladder pain syndrome/interstitial cystitis. A prospective, single-blind, randomized crossover trial of sacral vs pudendal nerve stimulation for interstitial cystitis. The long-term efficacy of sacral neuromodulation in the management of intractable cases of bladder pain syndrome: 14 years of experience in one centre. Intravesically administered oxybutynin was combined with bladder training in one study, with improvement of functional bladder capacity, volume at first sensation and cystometric bladder capacity (10). Oral cimetidine gives effective symptom relief in painful bladder disease: a prospective, randomized, double-blind placebo-controlled trial. Elevated nitric oxide in the urinary bladder in infectious and noninfectious cystitis. Effects of L-arginine treatment on symptoms and bladder nitric oxide levels in patients with interstitial cystitis. Fifteen patients reported a 50% decrease in urgency, frequency and nocturia, and there was a moderate increase in bladder capacity. However, scientific data are limited and dietary restriction alone does not produce complete symptomatic relief. A significant increase in capacity occurred after acupuncture in 52 women with 85% reporting an improvement in frequency, urgency and dysuria and symptoms (9). In a non-randomised comparison in women with urethral syndrome, 128 treated by acupuncture and traditional Chinese medicine were compared with 52 treated by western medicine as controls. Efficacy rates and urodynamic parameters were significantly better in the acupuncture group (11). Hypnosis is a therapeutic adjunct in the management of cancer, surgical disease and chronic pain. Each trigger point was identified by intravaginal palpation and injected with 5 mL of a mixture of 10 mL 0. There were significantly fewer complaints of dyspareunia following treatment (P = 0. Metabolic appraisal of the effects of dietary modification on hypersensitive bladder symptoms. Empowering the patient: hypnosis in the management of cancer, surgical disease and chronic pain. Modified Thiele massage as therapeutic intervention for female patients with interstitial cystitis and high-tone pelvic floor dysfunction. All techniques require substitution of the excised bladder tissue, mostly performed with bowel segments. As early as 1967, Turner-Warwick reported that mere bladder augmentation without removal of the diseased tissue was not appropriate (5). Supratrigonal cystectomy with subsequent bladder augmentation represents the most favoured continence preserving surgical technique. Substituting gastric segments (24, 25) seems to be less helpful because the production of gastric acids may maintain dysuria and persistent pain. In 1966, von Garrelts reported excellent results in 8/13 patients with a follow-up of 12-72 months (12). Although symptoms resolved in two patients, treatment failure in another six necessitated secondary cystectomy and ileal conduit formation (17). Ileocaecal bowel segments showed superior functional results, because in the group augmented with ileum, three patients required self-catheterisation and one a suprapubic catheter. Suprapubic pain disappeared in all cases, as well as lower urinary tract symptoms, with good control of urinary frequency day and night in the immediate postoperative period. While completely curing six patients by supratrigonal resection, there were three failures among 17 subtrigonal resections, and half of the successful subtrigonal resections required self-catheterisation to support voiding of the ileocaecal augmentate (27). Detailed counselling and informed consent must precede any irreversible type of major surgery, which should only be undertaken by experienced surgeons. The appropriate extent of tissue resection should be based on the endoscopic and histopathological findings. Some surgeons recommend preoperative cystoscopy and bladder capacity as a prognostic parameter for operative success (7). After orthotopic bladder augmentation, particularly when removing the trigone, voiding may be incomplete and require intermittent self-catheterisation. Intravesical chondroitin sulphate may be effective according to non-randomised studies. C Consider intravesical lidocain plus sodium bicarbonate prior to more invasive methods. Failure of combined supratrigonal cystectomy and Mainz ileovcecocystoplasty in intractable interstitial cystitis: is histology and mast cell count a reliable predictor for the outcome of surgery Early experience with the use of gastric segment in lower urinary tract reconstruction in adult patient population. Treatment of interstitial cystitis: comparison of subtrigonal and supratrigonal cystectomy combined with orthotopic bladder substitution. Long-term followup of augmentation enterocystoplasty and continent diversion in patients with benign disease. Long-term results of reconstructive surgery in patients with bladder pain syndrome/interstitial cystitis: subtyping is imperative. Scrotal pain syndrome is a generic term and is used when the site of the pain is not clearly testicular or epididymal. Pain in the scrotum can be divided into direct pain localised in the scrotum, or referred pain coming from another place or system in the body. Epididymal pain syndrome is often associated with negative cognitive, behavioural, sexual or emotional consequences, as well as with symptoms suggestive of lower urinary tract and sexual dysfunction. Patients with multiple cysts may have pain caused by the compression that these cysts exert on the epididymis. Chronic epididymis may be associated with signs of inflammation: inflammatory or obstructive chronic epididymitis (2). It is generally accepted that pain after inguinal surgery (hernia) is a consequence of damage to the nerves inside the spermatic cord (4). The pudendal nerve supplies the skin of the perineum and the posterior side of the scrotum. Postvasectomy scrotal pain syndrome is often associated with negative cognitive, behavioural, sexual or emotional consequences, as well as with symptoms suggestive of lower urinary tract and sexual dysfunction. Postvasectomy pain may be as frequent as 1% following vasectomy, possibly more frequent.
Atezolizumab is an Fc-engineered antibiotic resistance ted talk order 400mg noroxin overnight delivery, humanized infection nail bed cheap noroxin online master card, non-glycosylated IgG1 kappa immunoglobulin that has a calculated molecular mass of 145 kDa infection from bee sting buy noroxin 400 mg line. Each 20 mL vial contains 1200 mg of atezolizumab and is formulated in glacial acetic acid (16 antibiotics for acne and alcohol order 400mg noroxin visa. Each 14 mL vial contains 840 mg of atezolizumab and is formulated in glacial acetic acid (11 antibiotic otic drops buy online noroxin. Drug Interaction Studies the drug interaction potential of atezolizumab is unknown antimicrobial versus antibiotic purchase noroxin online from canada. Animal fertility studies have not been conducted with atezolizumab; however, an assessment of the male and female reproductive organs was included in a 26-week, repeat-dose toxicity study in cynomolgus monkeys. Tumor response assessments were conducted every 9 weeks for the first 54 weeks and every 12 weeks thereafter. Thirty-five percent of patients had non-bladder urothelial carcinoma and 66% had visceral metastases. Twenty percent of patients had disease progression following prior platinum-containing neoadjuvant or adjuvant chemotherapy. Both cisplatin-eligible and cisplatin-ineligible patients are included in the study. In this study, the median age was 66 years, 78% were male, 91% of patients were White. Twenty-six percent had non-bladder urothelial carcinoma and 78% of patients had visceral metastases. Nineteen percent of patients had disease progression following prior platinum-containing neoadjuvant or adjuvant chemotherapy. Forty-one percent of patients had received 2 or more prior systemic regimens in the metastatic setting. Seventy-three percent of patients received prior cisplatin, 26% had prior carboplatin, and 1% were treated with other platinum-based regimens. The majority of patients were White (82%), 13% of patients were Asian, 10% were Hispanic, and 2% of patients were Black. Clinical sites in Asia (enrolling 13% of the study population) received paclitaxel at a 2 2 dose of 175 mg/m while the remaining 87% received paclitaxel at a dose of 200 mg/m. Approximately 14% of patients had liver metastases at baseline, and most patients were current or previous smokers (80%). The majority of patients were white (90%), 2% of patients were Asian, 5% were Hispanic, and 4% were Black. Patients with a history of autoimmune disease, symptomatic or corticosteroid-dependent brain metastases, or requiring systemic immunosuppression within 2 weeks prior to enrollment were ineligible. The demographic and baseline disease characteristics of the study population were well balanced between the treatment arms. Approximately half the patients had received a taxane (51%) or anthracycline (54%) in the (neo)adjuvant setting. The majority of patients were White (80%); 17% were Asian, 4% were Hispanic and 1% were Black. Based on central testing, 74% were identified as having a V600E mutation, 11% as having V600K mutation, and 1% as having V600D or V600R mutations. Infusion-Related Reactions Advise patients to contact their healthcare provider immediately for signs or symptoms of infusion-related reactions [see Warnings and Precautions (5. Call or see your healthcare provider right away if you get any symptoms of the following problems or these symptoms get worse: Lung problems (pneumonitis). Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Active ingredient: atezolizumab Inactive ingredients: glacial acetic acid, L-histidine, polysorbate 20 and sucrose Manufactured by: Genentech, Inc. Formulation proposed for inclusion Tablets: 400 mg, 600 mg Injection: 400 mg / 4 ml, 1g / 10 ml 6. Whether listing is requested as an individual medicine or as an example of a therapeutic group Listing is requested on the Model List of Essential Medicines as an individual medicine. Information supporting the public health relevance (epidemiological information on disease burden, assessment of current use, target population) 8. Cancer is the second leading cause of death in developed countries and is among the three leading causes of death in developing countries. A summary of the types of cancer leading to overall cancer mortality in 2002 is presented in Table 1. In terms of incidence, the most common cancers worldwide (excluding non-melanoma skin cancers) are lung (12. As 1 stated in the World Cancer Report (2003), for any disease the relationship of incidence to mortality is an indication of prognosis, similar incidence and mortality rates being indicative of an essentially fatal condition. Thus, lung cancer is the largest single cause of deaths from cancer in the world (1. The burden of cancer is not distributed evenly between the developing and developed world, with specific cancer types displaying different patterns of distribution. As 1 discussed in the World Cancer Report (2003), many differences in the distribution of cancer between regions are explicable with reference to etiological factors. In developing countries for example, populations are vulnerable to cancers in which infectious agents (and associated non-malignant diseases) play a major role. These include cancers of the stomach, uterine cervix, liver and possibly oesophagus. Whereas other cancers such as colorectal and prostate cancers, the burden of disease falls disproportionately on the developed world. Female 27 Bladder 48 53 Thyroid 35 72 Oral cavity 24 39 Pancreas 61 65 Leukaemia 47 54 Non-Hodgkin lymphoma 66 117 Oesophagus 16 132 Liver Less developed 33 75 Corpus uteri More developed 113 101 Ovary 91 192 Stomach 125 161 Lung 175 154 Colorectum 291 379 Cervix uteri 91 471 Breast 579 0 100 200 300 400 500 600 700 Number (Thousands). The principle subtype of paedatric cancer in affluent societies is acute leukaemia where the incidence rate is within the range of 6 5 30-45 per 10 children per year. In the United Kingdom there around 500 new cases of acute leukaemia diagnosed each year in children up to 15 years. Other common childhood cancers include cancer of the brain and other nervous system cancers, soft tissue sarcomas, non Hodgkin Lymphoma, and renal (Wilms) tumors. In the United States advances in the treatment of childhood cancers have led to an improved 5-year survival rate from 56% for 4 patients diagnosed in 1974-1976 to 79% in children diagnosed with cancer in 1995 to 2001. In the case of acute leukaemia, controlled clinical trials of chemotherapy in the United States 5 and Europe have steadily improved the survival of children to 85%. As 80% of children live in developing countries where effective treatment is not available, one in two children diagnosed with 3 cancer will die. Although significant advances have been made in chemotherapy since then the therapeutic use and benefit of chemotherapy is restricted by toxic lesions which are often organospecific. Examples of this include the cardiotoxic effects of doxorubicin, the hepatotoxicity of methotrexate, nephrotoxicity of cisplatin, neurotoxicity of vincristine, pulmonary fibrosis induced by bleomycin, and 6 urotoxicity of the two oxazaphosphorines cyclophosphamide and ifosfamide. The toxicities of chemotherapy can adversely affect both the short and long-term quality of life of patients, it can limit the dose and duration of treatment, can be life-threatening, and may contribute to 7 the medical and non-medical costs of cancer care. To ameliorate the toxicity associated with cytotoxic agents a number of chemoprotectants have been developed to provide site-specific 8 protection for normal tissues, without compromsing antitumour efficacy. Mesna (sodium-2 mercaptoethane sulfonate) was developed as a specific chemoprotective compound against acrolein-induced bladder toxicity, a dose-limiting side-effect of both cyclophosphamide and ifosfamide. Cyclophosphamide was first synthesized in 1958 and was the prototype of the oxazaphosphorines without a direct alkylating action. It is a prodrug of nor-N-mustard requiring biotransformation to hydroxylated intermediates by hepatic cytochrome P-450 9-11 mixed-function oxidase system to exert cytotoxic activity. The hydroxylated intermediates undergo breakdown to form active compounds, phosphoramide mustard and acrolein, a urotoxic agent. Cyclophosphamide is indicated for the treatment of myeloproliferative and lymphoproliferative disorders; disseminated neuroblatoma; ovarian adenocarcinoma; retinoblastoma; breast and lung carcinoma; autoimmune disease; and transplant rejection prevention. The location of the ring chlorethyl side chain significantly slows hydroxylation which produces isofosforamide mustard, the primary alkylating compound, and the urotoxic agent 12 acrolein. This slight modification results in a clinically significant change in the activity and 13 toxicity of ifosfamide compared to cyclophosphamide. Mesna (sodium-2-mercaptoethane sulfonate) is a thiol compound, which functions as a regional detoxificant of urotoxic oxazaphosphorine cytostatic agents, ifosfamide and 8 cyclophosphamide. As described by Links and Lewis (1999), mesna inactivates alkylating metabolites by forming an inert thioether. Upon entering the bloodstream mesna is immediately converted to an inactive disulfide form, dimesna (dithiodiethanesulfate) which is subsequently filtered and secreted by the kidneys, where the enzymes thiol transferase and glutathione reductase reduce dimesna back to mesna. The free sulfhydryl (thiol) groups of mesna combine directly with a double bond of acrolein and with other urotoxic 4-hydroxy oxazaphosphorine metabolites (4-hydroxycyclophosphamide and 4-hydroxyifosfamide) to form stable nontoxic compounds. The metabolite acrolein has been implicated as the major 7 causative agent in oxazaphosphorine-induced urothelial toxicity. These guidelines indicate that in patients treated with ifosfamide without urothelial protection the overall incidence of haemorrhagic cystitis ranges from 18% to 40% and is considered dose-limiting. In the case of high-dose cyclophosphamide, patients treated with aggressive hydration in the context of bone marrow transplantation, the incidence of severe haemorrhagic cystitis ranges from 0. In patients who develop severe bladder haemorrhage mortality rates range 7 from 2% to 4%. Haemorrhagic cystitis is generally graded as mild, moderate or severe according to the degree of pain and haematuria. Severe haemorrhagic cystitis typically includes the presence of gross haematuria with clots and occurrence of clinical complications, it can be extremely painful and debilitating, requiring prolonged and expensive 14 hospitalisation. To maintain adequate urinary prophylaxis, this regimen is given each day that ifosfamide is administered and, if ifosfamide dosage is increased or decreased, dosage of mesna should be adjusted accordingly. Mesna should be administered each day cyclophosphamide is administered, and probably should be continued for at least 24 hours after cyclophosphamide is discontinued. Each individual dose of mesna may be increased to 40% of the dose of the antineoplastic and given 4 times at intervals of 3 hours for children and patients at high risk of urotoxicity; in such cases the total dose of mesna is equivalent to 160% of the antineoplastic given. The oral dose of mesna is 40% of the dose of the antineoplastic given on 3 occasions at intervals of 4 hours beginning 2 hours before the antineoplastic injection; thus a total dose of mesna equivalent to 120% of the antineoplastic is given. Alternatively, the initial dose of mesna may be given intravenously (20% of the dose of the antineoplastic), followed by two oral doses (each 40% of the dose of the antineoplastic) given 2 and 6 hours after the intravenous dose. The final 12-hour infusion may be replaced either by 3 intravenous injections each of 20% of the antineoplastic dose at intervals of 4 hours, the first injection being given 4 hours after the infusion has been stopped, or by oral mesna given in 3 doses each of 40% of the antineoplastic dose, the first dose being given when the 24-hour infusion is stopped, and the second and third doses being 18 given 2 and 6 hours later. The duration of mesna treatment should therefore equal that of the antineoplastic treatment plus the time taken for the concentration of antineoplastic metabolites in the urine to fall to non-toxic concentrations. Urinary output should be maintained at 100 ml/hr and the urine monitored for haematuria and proteinuria throughout the treatment period. Mesna use with ifosfamide the use of mesna is recommended to decrease the incidence of ifosfamide-associated urothelial toxicity. Mesna dosing with standard-dose ifosfamide It is suggested that the daily dose of mesna be calculated to equal 60% of the total daily dose of ifosfamide, administered as three bolus doses given 15 minutes before and 4 and 8 hours after administration of each dose of ifosfamide when the ifosfamide dose is less than 2 2. For use with contiunous infusion ifosfamide, mesna may be administered as a bolus dose equal to 20% of the total ifosfamide dose followed by a continuous infusion of mesna equal to 40% of the ifosfamide dose, continuing for 12 to 24 hours after completion of the ifosfamide infusion. Mesna dosing with high-dose ifosfamide There is insufficient evidence on which to base a recommendation for the use of mesna with 2 ifosfamide doses in excess of 2. The efficacy of mesna for urothelial protection with very high-dose ifosfamide has not been proven. Based on the longer half-life of ifosfamide in these dosages, more frequent and prolonged mesna dosage regimens may be necessary for maximum protection from urotoxicity. Mesna tablets are given in a dosage equal to 40% of the ifosfamide dose at 2 and 6 hours after each dose of ifosfamide. The dosing schedule should be repeated on each day that ifosfamide is administered. Mesna use with cyclophosphamide Mesna plus saline diuresis or forced saline diuresis is recommended to decrease the incidence of urothelial toxicity associated with high-dose cyclophosphamide in the setting of stem-cell transplantation. Surveillance of patients receiving ifosfamide and/or cyclophosphamide and mesna There are insufficient data to make a recommendation regarding specific monitoring for hemorrhagic cystitis in patients who receive mesna to ameliorate ifosfamide-or-high-dose cyclophosphamide associated urothelial toxicity. Recommendations for monitoring reflect the design of clinical trials involving mesna use and the opinion of the Panel. The two most commonly used and relatively simple methods to detect haematuria is urinanalysis and urine microscopy. Urinalysis can be performed by nursing staff using a sample of urine collected from the patient and analysed using a testing dipstick. However, urine microscopy requires urine samples to be sent to specialist testing facilities to be analysed. Given that mesna is given concurrently with ifosfamide and cyclophosphamide, which are frequently combined with other chemotherapy drugs. To restrict and improve the specificity of these searches, three search filters were 19 used.
Buy noroxin 400 mg with mastercard. The development of antibiotic use in Australia.
Do you feel that you are slower when reasoning virus que esta en santo domingo order generic noroxin on line, planning activities antibiotics for acne vibramycin trusted 400 mg noroxin, or ing of antibiotic quality control purchase noroxin 400mg fast delivery, or care giver solving problems Chronic oxygen when stable (non-exacerbated) resting SpO2 88% (or PaO2 55 mmHg) 3 virus 2014 symptoms noroxin 400 mg sale. An individual with frailty is exposed to enhanced vulnerability to stressors antibiotics bladder infection trusted noroxin 400mg, and associated risk of negative health-related outcomes topical antibiotics for acne vulgaris purchase 400 mg noroxin with visa. The most common instruments to measure frailty include the Frailty Phenotype [22] and Frailty Index [23] Feature Frailty Phenotype Frailty Index Clinical defnition Based on presence of signs, symptoms Based on presence of diseases, disabilities (pre-disability syndrome) (accumulation of defcits) How to assess Assessed by fve specifc features [22]: A frailty index is calculated based on the number 1. Sustain and recover physical function impairment and sarcopenia prescribing physical activity with a resistance training component 2. Prescribe vitamin D for individuals defcient in vitamin D, see page 62 (a) Self-reported unintentional weight loss was considered present if exceeding 4. Substitution therapy (opioid replacement therapy) in persons with active drug fbrosis. FibroScan, liver biopsy, serum fbrosis markers(v), see Table on use as a step towards cessation of active drug use should be encouraged. Screening for oesophageal varices upon diagnosis of cirrhosis in co-infected ment, Renal complications are frequent, see page 64 and Diagnosis and Manage mendations-treatment-of-hepatitis-c/) and page 102. Histological remission of liver disease is a less ambitious but more likely achievable goal 9. Cryptococcal infection can also cause a pneumonitis which may be diffcult to distinguish from Pneumocystis pneumonia. See Pre-emptive therapy below Treatment (Cryptococcal meningitis and disseminated cryptococcosis) 14 days induction therapy, then 8 weeks consolidation therapy, then secondary prophylaxis for at least 12 months. Aspergillus galactomanan assays may be helpful to diagnose disseminated infections as cross reactivity occurs. Little clinical evidence is available for the use of voriconazole or posaconazole. Measurement of plasma concentration of itraconazole is advised to guide optimal treatment, and itraconazole oral suspension should be preferred due to better bioavailability. Some experts would add intravitreal injections of ganciclovir (2 mg) or fos carnet (2. Effcacy, safety, and tolerability of dolutegravir-rilpivirine for the mainte at. The Asia-Pacifc Clinical Practice Guidelines for the Infections, Abstract 42 Management of Frailty. Reconsidering medication appropriateness for pa with end-stage renal disease on chronic haemodialysis: an open-la tients late in life, Arch Intern Med 2006 bel, single-arm, multicentre, phase 3b trial. Age Ageing 2015 dolutegravir single tablet regimen in patients with human immunodef 13. Good practice guidelines for the assessment and treatment of adults ciency virus and end-stage renal disease on hemodialysis. Guidelines for the primary and gender-affrming care of transgender and gender nonbinary people. A review of cross-sex hormonal treatments, outcomes and adverse effects in transmen. Hypertens; 2013:7:1281-1357 incident diabetes mellitus: impact of using hemoglobin A1C as a criterion for 7. Standards of Medical Care in Diabe tes 2017 Abridged for Primary Care Providers Clin Diabetes. Increased acute myocardial infarction 1282 rates and cardiovascular risk factors among patients with human immu 15. Boceprevir versus placebo with pegylated interferon alfa-2b and ribavirin for treatment of Benhamou Y, Di Martino V, Bochet M et al. Liver related deaths in persons in-fected with the human immunodefciency virus: the D:A:D study. Antifungal Combinations Gegia M, Winters N, Benedetti A, van Soolingen D, Menzies D. Offcial American Thoracic Society/ Centers for Disease Control and Prevention/Infectious Dis eases Society of America Clinical Practice Guidelines: Treatment of Drug-Susceptible Tuberculosis. Treatment of isoniazid-resistant tuberculosis with frst-line drugs: a systematic review and meta-analysis. Other causes of isolated nephrotic syndrome can be subdivided into two major categories: rare genetic disorders, and secondary diseases associated with drugs, infections, or neoplasia. The cause of idiopathic nephrotic syndrome remains unknown, but evidence suggests it may be a primary T-cell disorder that leads to glomerular podocyte dysfunction. Genetic studies in children with familial nephrotic syndrome have identified mutations in genes that encode important podocyte proteins. Patients with idiopathic nephrotic syndrome are initially treated with corticosteroids. Nephrotic syndrome is associated with several medical complications, the most severe and potentially fatal being bacterial infections and thromboembolism. The first recorded description of nephrotic syndrome dates prevalence of nearly 16 cases per 100 000. Later, Volhard and Fahr1 popularised distinct histological variants of primary idiopathic the term nephrosis, using it to describe a major nephrotic syndrome: minimal-change nephrotic syndrome classification of bilateral renal disease. By the permselectivity barrier of the glomerular capillary wall, contrast, membranous nephropathy is a distinct disease which is no longer able to restrict the loss of protein to less associated with prominent immune complex deposits than 100 mg/m2 body surface per day. Nephrotic-range located between glomerular podocytes and the glomerular proteinuria has been variously defined, including the basement membrane. Membranous nephropathy is rare in increasingly popular use of spot urinary protein-to children. Less commonly, childhood the histological variant and the response to nephrotic syndrome is the consequence of an inflammatory immunosuppressive treatment. In particular, Hispanic or ischaemic glomerular disorder or is due to an inherited and black patients are more likely to have steroid renal disease. Although the pathogenesis of idiopathic unresponsive nephrotic syndrome than are white childhood nephrotic syndrome remains unclear, important patients. Inherited forms of steroid-responsive and steroid Lymphoma resistant nephrotic syndrome are being increasingly Leukaemia recognised. Normally, proteins the size of albumin (69 kd) and larger are excluded from filtration, a restriction that depends substantially on the integrity of the slit diaphragms. B Three observations provide important clues to the primary pathophysiology of idiopathic nephrotic syndrome. Mutations in several podocyte proteins have been identified in families with inherited nephrotic syndrome, highlighting the central importance of the podocyte (figure 2). A plasma factor may alter glomerular permeability, especially among patients with steroid-resistant nephrotic syndrome. Altered T-lymphocyte responses seem to be important; a primary T-cell event could result in the production of a permeability factor that interferes with the expression, function, or both, of key podocyte proteins to cause proteinuria. A higher rate of certain gene polymorphisms among nephrotic patients than among controls suggests the existence of disease susceptibility genes (figure 3). Among children with inherited nephrotic syndrome, investigators have identified mutations in other 5 genes that encode podocyte proteins (figure 2, table 2). The role of podocyte proteins in the pathogenesis of 4 sporadic cases of so-called idiopathic nephrotic syndrome requires further investigation. Genetic mutations have been 7 identified in some children with sporadic steroid-resistant nephrotic syndrome. At least one locus has B: In nephrotic syndrome, slit pores disappear and foot processes been mapped to chromosome 1q25, close to but distinct assume fused appearance. Cytokines and receptors the therapeutic use of plasma exchange is plausible in such Platelet-activating-factor modifiers patients. Cultured T cells isolated from nephrotic patients have been reported to synthesise a factor or factors that produce transient proteinuria when injected into rats34 or impair glomerular podocyte synthesis of glycos aminoglycans. Increased hepatic lipoprotein synthesis, in response to low plasma oncotic Age <1 year pressure, as a consequence of the urinary loss of an as-yet Positive family history unidentified regulatory substance, or both, is thought to Extrarenal disease (eg, arthritis, rash, anaemia) play a key pathogenetic part. A course of corticosteroid treatment water into the interstitial space; secondary sodium without a renal biopsy is indicated for children without retention develops to compensate for intravascular volume atypical features, since responsiveness to steroids is a contraction. The underfill theory is intuitively attractive better indicator than kidney histology of long-term and data showing that nephrotic patients have contracted prognosis for renal function. Renal biopsy is generally intravascular volume, reduced glomerular filtration rate, limited to steroid-unresponsive and steroid-dependent and raised renin and aldosterone concentrations support patients, although it has yet to be shown that this the concept. Therapeutic approaches are nephrotic oedema is a primary defect in sodium excretion. Traditionally, not universally accepted and may not be sufficient to patients receive divided doses but once-daily treatment explain oedema formation in childhood nephrotic also seems to be effective. The underfill and overfill mechanisms are not been a shift in the past decade to longer courses of necessarily mutually exclusive, dependent on the stage corticosteroid treatment for first episodes of nephrotic of nephrotic syndrome, the rate of development of syndromes in an effort to decrease the relapse rate. In hypoproteinaemia, and absolute plasma oncotic support of this approach was the study by the pressure. By contrast, patients with chronic forms of prednisone on alternate days for 6 weeks than among persistent nephrotic syndrome may have continuing patients who received the then standard 8-week sodium retention and thus be more prone to oedema from treatment. In a meta-analysis of the five randomised controlled trials involving children with a first episode of steroid Hyperlipidaemia responsive nephrotic syndrome, longer duration of Hyperlipidaemia, with raised serum cholesterol and treatment significantly decreased the risk of relapse at 12 triglyceride concentrations, is a hallmark of nephrotic and 24 months without an increase in adverse events. Steroid-induced side-effects Although steroid treatment is normally continued beyond develop in a high proportion of these patients. Currently 8 weeks even in steroid-resistant patients, and it remains a there are no data on the preferred second-line drug. Use component of most subsequent treatment, we have no of cyclophosphamide, chlorambucil, ciclosporin, and adequate evidence from randomised controlled clinical levamisole to reduce the risk of relapses is supported by a trials to provide clear guidance for subsequent dosing. In a summary of nine paediatric any 12-month period) reportedly achieve a longer series published in 1984, 30% of steroid-unresponsive remission with alkylating agents than do children with patients responded to cyclophosphamide. Given the risks of seizures also induce remission, whether this route of associated with chlorambucil, cyclophosphamide is more administration is safer or more effective has not been commonly prescribed. Standardised guidelines for the dose and important data on safety and efficacy have been added. To achieve Overall, when used to treat steroid-responsive nephrotic remission, the initial target plasma trough concentrations syndrome, remission can be achieved in 85% of patients. Concerns higher plasma concentrations may be necessary to achieve about nephrotoxic effects mandate careful monitoring of adequate tissue ciclosporin concentrations. Despite the very promising as effective as cyclophosphamide in frequently relapsing initial outcome reported with this therapeutic protocol, nephrotic syndrome. Ethnic composition of the study population is an cases of agranulocytosis, vasculitis, and encephalopathy. Prophylactic treatment with varicella zoster immune globulin is recommended for non-immune patients taking immunosuppressive treatments. No one laboratory test can reliably predict the However, with the high rate of end-stage renal disease real thrombotic risk. Fibrinogen concentration has been among patients unresponsive to traditional doses of proposed as a surrogate marker. Other factors that glucocorticoids and ciclosporin, this approach is often increase thrombotic risk in nephrotic patients include considered. They can be divided into two major subgroups: acute complications related to the nephrotic state, especially infections and thromboembolic disease, and long-term sequelae of nephrotic syndrome and its treatment, especially effects on bones, growth, and the cardiovascular system. A third important area is the psychological impact and social demands on children who have nephrotic syndrome, and their families.
The most common bacterial infection caused by a dog bite is Pasturella multicida antimicrobial laundry additive buy noroxin 400 mg mastercard, which accounts for up to 50% of infections [317] virus 3 weeks cheap noroxin 400mg overnight delivery. Other commonly involved organisms are Escherichia coli antibiotic kills 99.9 bacterial population order noroxin online from canada, Streptococcus viridans antibiotics causing diarrhea buy 400mg noroxin with amex, Staphylococcus aureus antibiotics for sinus infection pregnancy buy generic noroxin 400 mg, Eikenella corrodens infection 2 migrant discount noroxin 400 mg on line, Capnocytophaga canimorsus Veillonella parvula, Bacteroides and Fusobacterium spp. The first choice of antibiotics is penicillin-amoxiclavulanic acid, followed by doxycycline, cephalosporin or erythromycin for 10-14 days [319-321]. If rabies infection is suspected, vaccination should be considered taking into account the geographical location, animal involved, specific nature of the wound and the type of attack (provoked/unprovoked). Besides vaccination, local wound management is an essential part of post-exposure prophylaxis. High-risk patients should be vaccinated with human rabies immunoglobulin and human diploid cell vaccine [322, 323]. For further details, see Guidelines for the Management of Human Bite Injuries [324]. In these cases, the examiner should be aware of the extraordinary emotional situation of the patient and the privacy of the patient respected. Swabs or vaginal smears should be taken for detection of spermatozoa [326] and local legal protocols followed closely. A thorough history and examination (in some cases under anaesthesia), photo documentation, and identification of forensic material may be important. In a recent report, only 38% of the forensic samples tested positive for an ejaculate and/or sperm. This may be due to delayed presentation or lack of vaginal/anal ejaculation [327, 328]. In these cases, only subcutaneous haematoma with intact tunica albuginea may be seen. The most common mechanism of injury is when the penis slips out of the vagina and strikes against the symphysis pubis or perineum. Sixty per cent of cases occur during consensual intercourse [330], and is more likely when the partner is on top. Penile fracture is caused by rupture of the cavernosal tunica albuginea, and may be associated with subcutaneous haematoma and lesions of the corpus spongiosum or urethra in 10-22% [331, 332]. The thickness of the tunica albuginea in the flaccid state (approximately 2 mm) decreases in erection to 0. Penile fracture is associated with a sudden cracking or popping sound, pain and immediate detumescence. Less severe penile injuries can be distinguished from penile fracture, as they are not usually associated with detumescence. A thorough history and examination usually confirm the diagnosis, but in some cases imaging may be useful. Subcutaneous haematoma, without associated rupture of the cavernosal tunica albuginea, does not require surgical intervention. When a penile fracture is diagnosed, surgical intervention with closure of the tunica albuginea is recommended. The approach is usually through a circumferential incision proximal to the coronal sulcus which enables degloving the penis entirely. Increasingly, local longitudinal incisions centred on the area of fracture are currently used and further localisation may be gained with a flexible cystoscopy performed prior to incision, if urethral trauma is suspected and eventually proven. Closure can be obtained by using absorbable sutures, with good long-term outcome, and protection of potency. Post-operative complications were reported in 9%, including superficial wound infection and impotence in 1. It increases complications, such as penile abscess, missed urethral disruption, penile curvature, and persistent haematoma requiring delayed surgical intervention [340]. Late complications after conservative management were fibrosis and angulations in 35%, and impotence in up to 62% [330, 340]. In more significant penetrating penile injuries, surgical exploration and debridement of necrotic tissue is recommended. Even in extended injuries of the penis, primary alignment of the disrupted tissues may allow for acceptable healing because of the robust penile blood supply [312]. The principles of care are debridement of devitalised tissue, with the preservation of as much viable tissues as possible, haemostasis, diversion of urine in selected cases and the removal of foreign bodies. If a subsequent immediate or delayed repair is needed, depending on the type of injury and the extent of tissue damage, it usually takes place 4-6 weeks after the trauma has occurred. The surgical approach depends upon the site and extent of the injury, but a subcoronal incision with penile degloving usually gives good exposure. Initially, a defect in the tunica albuginea should be closed after copious irrigation. If there has been too much tissue loss, the defect can be repaired either immediately or after delay with a patch (either from an autologous saphenous vein or xenograft). If a concomitant urethral injury is suspected, a pre or peri-operative urethrogram or cystoscopy is useful to diagnose any urethral involvement, to define its position, and to decide upon the incision used. The elasticity of genital skin means it is usually possible to manage the loss of a moderate amount of penile skin. However, management is more difficult in extensive injuries with significant skin loss. The tissue chosen for reconstruction following trauma needs to provide good coverage and must be suitable for reconstruction. Split-thickness skin grafting provides good coverage and a dependable take that is reproducible and durable. However, split-thickness grafts contract more than full-thickness grafts and their use on the penile shaft should be kept to a minimum. Full-thickness skin grafting onto the penile shaft gives less contracture, a better cosmetic appearance and more resistance to trauma during intercourse, when eventually re-established [339]. In cases of extensive destruction of deeper tissues, or if later prosthetic placement is being considered, skin flaps, with their secure vascular supply can be used. Acute management involves resuscitation of the patient, who may be compromised from massive blood loss, and preparation for surgical re-implantation of the penis if it has been recovered and is not too badly damaged. Surgical re-implantation should be considered for all patients and should be performed within 24 hours of amputation. If the injury occurred during a psychotic episode, early psychiatric advice and support should be sought. The severed penis should be washed with sterile saline, wrapped in saline-soaked gauze, placed in a sterile bag and immersed in iced water. A pressure dressing or a tourniquet should be placed around the penile stump to prevent excessive blood loss. Re-attachment can be achieved in a non-microsurgical way, a technique which probably gives higher rates of post-operative urethral stricture and more problems with loss of sensation [341]. When operating microscopically, the corpora cavernosa and urethra are firstly aligned and repaired. Subsequently, the dorsal penile arteries, the dorsal vein and the dorsal nerves are anastomosed. The fascia and skin are closed in layers and both a urethral and a supra-pubic catheter are placed. If the severed penis cannot be found, or is unsuitable for re-attachment, then the end should be closed as it is done in partial penectomy. Bilateral dislocation of the testes has been reported in up to 25% of cases [343]. It can be either a subcutaneous dislocation with epifascial displacement of the testis or an internal dislocation. In the latter, the testis is positioned in the superficial external inguinal ring, inguinal canal or abdominal cavity. Traumatic dislocation of the testis is treated by manual replacement and secondary orchidopexy. If primary manual reposition cannot be performed, immediate orchidopexy is indicated. In large haematoceles, non-operative management often fails, and delayed surgery (> 3 days) is often required. Patients with large haematoceles have a higher rate of orchiectomy than patients who undergo early surgery, even in non-ruptured testes [304, 312, 347-349]. Early surgical intervention results in preservation of the testis in more than 90% of cases compared to delayed surgeries which result in orchiectomy in 45-55% of patients [349]. In addition, non-operative management is also associated with prolonged hospital stays. Therefore, large haematoceles should be treated surgically, irrespective of the presence of testicular contusion or rupture. At the very least, the blood clot should be evacuated from the tunica vaginalis sac to relieve disability and hasten recovery. Patients initially treated non-operatively may eventually need delayed surgery if they develop infection or undue pain. It may occur under intense, traumatic compression of the testis against the inferior pubic ramus or symphysis, resulting in a rupture of the tunica albuginea of the testis. Testicular rupture is associated with immediate pain, nausea, vomiting, and sometimes fainting. Others reported poor specificity (78%) and sensitivity (28%) for the differentiation between testicular rupture and haematocele, while accuracy is as low as 56% [352]. However, these techniques did not specifically increase the detection rates of testicular rupture. It is therefore essential to surgically explore equivocal patients whenever imaging studies cannot definitively exclude testicular rupture. This involves exploration with evacuation of blood clots and haematoma, excision of any necrotic testicular tubules and closure of the tunica albuginea, usually with running absorbable sutures. Depending on the extent of the injury, primary reconstruction of the testis and scrotum can usually be performed. In complete disruption of the spermatic cord, realignment without vaso-vasostomy may be considered if surgically feasible [360]. Staged secondary microsurgical vaso-vasostomy can be performed after rehabilitation, although only a few cases have been reported [360]. If there is extensive destruction of the tunica albuginea, mobilisation of a free tunica vaginalis flap can be performed for testicular closure. If the patient is unstable or reconstruction cannot be achieved, orchiectomy is then indicated. Prophylactic antibiotics are recommended after scrotal penetrating trauma, although data to support this approach is lacking. Post-operative complications were reported in 8% of patients who underwent testicular repair after penetrating trauma [249]. Extended laceration of scrotal skin requires surgical intervention for skin closure. Due to the elasticity of the scrotum, most defects can be primarily closed, even if the lacerated skin is only minimally attached to the scrotum [312]. Local wound management with extensive initial wound debridement and washout is important for scrotal convalescence. The incidence of traumatic vulvar haematomas after vaginal deliveries has been reported as 1 in 310 deliveries [361]. Although blunt trauma to the female external genitalia is rarely reported, the presence of a vulvar haematoma is closely related to an increased risk of associated vaginal, pelvic or abdominal injuries. Blunt vulvar or perineal trauma may be associated with voiding problems and bladder catheterisation is usually required. Vulvar haematomas usually do not require surgical intervention, although they can cause a significant blood loss, which sometimes even requires blood transfusion. Data are scarce [362], but in haemodynamically stable women, non-steroidal anti-inflammatory medication and cold packs are generally successfully used. Yet, in cases of massive vulvar haematoma and haemodynamically unstable patients, surgical intervention with lavage and drainage is sometimes indicated [363]. Although antibiotics are often recommended after major vulvar trauma, there is no data to support this approach. It is important to emphasise that vulvar haematoma and/or blood at the vaginal introitus are indications for vaginal exploration under sedation or general anaesthesia. Flexible or rigid cystoscopy has been recommended to exclude urethral and bladder injury [315, 316]. In the case of vulvar laceration, suturing after conservative debridement is indicated. If there are associated injuries to the vagina, these can be repaired immediately by primary suturing. In testicular trauma, surgical exploration is recommended in all cases of testicular rupture and in those B with equivocal imaging. Lessons from civilian trauma networks, the battlefield, and mass casualty events have led to many advances in general trauma care [365, 366]. These include the widespread acceptance of damage control principles, trauma centralisation and recognition of the value of dedicated trauma teams.
References
- Rosenwaks Z. Donor eggs: their application in modern reproductive technologies. Fertil Steril 1987; 47(6):895-909.
- Girman CJ, Jacobsen SJ, Tsukamoto T, et al: Health-related quality of life associated with lower urinary tract symptoms in four countries, Urology 51(3):428n436, 1998.
- Black TR, Gates DS, Lavely K, et al: The percutaneous electrocoagulation vasectomy techniqueoa comparative trial with the standard incision technique at Marie Stopes House, London, Contraception 39:359n368, 1989.
- Diringer MN, Edwards DF. Admission to a neurologic/neurosurgical intensive care unit is associated with reduced mortality rate after intracerebral hemorrhage. Crit Care Med 2001;29(3):635-40.
- Chen H, Li F, Sun JB, et al. Abdominal compartment syndrome in patients with severe acute pancreatitis in early stage. World J Gastroenterol. 2008;14(22):3541-3548.
- Steigen SE, Schaeffer DF, West RB, Nielsen TO. Expression of insulin-like growth factor 2 in mesenchymal neoplasms. Mod Pathol 2009;22(7):914-21.
- Courtney RM, Kerr DA. The odontogenic adenomatoid tumor. A comprehensive study of twenty new cases. Oral Surg Oral Med Oral Pathol 1975;39:424-435.