Mark Woodward, MD, FRCS (Paed)
- Consultant Paediatric Urologist, Department of Paediatric
- Surgery, Bristol Royal Hospital for Children, Bristol,
- United Kingdom
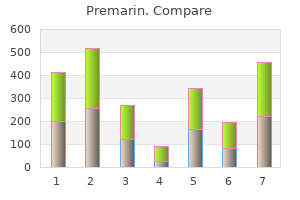
This pain often precedes irregularity of the duodenum resulting from the development of jaundice womens health hours purchase genuine premarin. This is from other causes of obstructive jaundice and from other causes of upper abdominal pain womens health 3 month workout plan premarin 0.625mg visa. However pregnancy resource center grand rapids buy premarin 0.625mg otc, most tumours are approximately 15% of cases menopause groups cheap premarin 0.625 mg with amex, attempted curative inoperable and women's health clinic erina purchase premarin 0.625mg online, even among the 15% which resection may be possible; otherwise women's health editorial calendar buy premarin 0.625mg with amex, palliation is are operable, the long-term prognosis is poor more appropriate. Periampullary growths, however, which planned, but expanding metal stents can be present relatively early, have a reasonably good used in the palliative situation when the prognosis after resection, with about a 25% 5 year diagnosis is clear because they have better survival. Duodenal obstruction can now Palliative chemotherapy currently uses proto also be treated by endoscopic stenting, cols based on gemcitabine. The place of radio potentially allowing the terminally ill patient to therapy is unclear, although some centres do use be spared the additional morbidity of a a combination of radiotherapy and chemotherapy laparotomy and surgical bypass. Recent trials have shown a laparoscopic gastroenterostomy can be used to de nite survival bene t in patients who have palliate duodenal obstruction. Prognosis the outlook for patients with carcinoma of the pancreas itself is gloomy; even if the growth is 33 the spleen Learning objective To know the common causes of splenomegaly, the presentations of a ruptured spleen and the prophylaxis and treatment of post splenectomy syndrome. It then forms a swelling that descends below a Leukaemia: chronic myeloid and chronic the left costal margin, moves on respiration and lymphocytic. Increased pressure in the enormous, there is resonance over the swelling portal system causes progressive enlargement anteriorly, as it is covered by the gas of the spleen and may lead to hypersplenism containing colon. Removal of the spleen in splenectomy predis poses the patient, especially a child, to infection with organisms such as the Pneumococcus. The clinical course is of a fulminant bacterial infec Splenectomy tion, with shock and circulatory collapse, termed overwhelming postsplenectomy sepsis. Splenectomy is indicated under the following Prophylactic immunization with pneumococ circumstances: cal, meningococcal and H. Complications of splenectomy Ruptured spleen Gastric dilatation this is the commonest internal injury produced Following splenectomy, there may be a gastric by non-penetrating trauma to the abdominal wall. Swallowed air causes rapid dilatation of the It usually occurs in isolation, but may coexist with stomach, which may tear ligatures on the short fractures of the ribs, or rupture of the liver, the left gastric vessels on the greater curve of the stomach, kidney, the diaphragm or the tail of the pancreas. Clinical features Rupture of the spleen manifests in one of the fol Thrombocytosis lowing ways: Following splenectomy, the platelet count rises, 1 Immediate massive bleeding with rapid death often to a level of 1000 1 0 9/L (normal is from shock. In time, the count falls, but while it shattering of the spleen or its avulsion from is high the patient is at a greater than normal risk the splenic pedicle, and death may occur in a of deep vein thrombosis and pulmonary embolus. Antiplatelet agents such as aspirin are given as 2 Peritonism from progressive blood loss. There is abdominal microorganisms (such as Pneumococcus, pain, which is either diffuse or con ned to the Meningococcus and Haemophilus in uenzae) left ank. The patient may complain of pain from the bloodstream after they have been referred to the left shoulder tip or admit to this opsonized by the binding of host antibodies to only on direct questioning. There may the spleen 291 be marked generalized rigidity, or it may be exure of the colon, if containing gas, may be con ned to slight guarding in the left ank. This may occur from hours intrasplenic haematoma or a laceration of the up to several days after trauma. Then, following a completely tool in the accident and emergency asymptomatic interval, the signs and department for such cases. Treatment Resuscitation with plasma expanders initially and Special investigations blood replacement as soon as blood is available is the diagnosis of a ruptured spleen is a clinical commenced, and laparotomy performed. If the one, and an unstable patient must be resuscitated spleen is found to be avulsed or hopelessly pulped, aggressively and the surgeon proceed at once to emergency splenectomy is required. In the less acute situation, and only minor laceration of the spleen, an attempt is made after resuscitation has begun, the following inves to preserve it, especially in children and young tigations are useful: adults, in whom there is a greater risk of post splenectomy sepsis. The splenic 34 the lymph nodes and lymphatics Learning objectives To know the causes of lymphadenopathy and the appropriate management. Clinical examination the lymphadenopathies the clinical examination of any patient with a the lymphadenopathies are conveniently divided lymph node enlargement is incomplete unless into those due to local and those due to general the following three requirements have been ized disease. If a patient has an enlarged lymph node in the groin, the Generalized skin of the leg, buttock and lower abdominal 1 Infective: wall below the level of the umbilicus must a acute. The lymph nodes and lymphatics 293 vessels to the para-aortic lymph nodes, and Box 34. In many instances, the cause of the lymphaden opathy will by now have become obvious. It is Differential diagnosis characterized by lymphoedema that is particularly severe below the waist. It has been the diagnosis of lymphoedema depends rst of all arbitrarily divided into lymphoedema praecox, on the exclusion of other causes of oedema, for which develops between puberty and the age instance venous obstruction, cardiac failure or of 35, and the less common lymphoedema renal disease, and, second, on demonstration of tarda, which develops in adult life. It was previ ously taught that lymphoedema could readily be There are three principal pathological processes differentiated from other forms of oedema on the affecting the lymphatic channels in congenital simple physical sign of absence of pitting in the lymphoedema: aplasia, hypoplasia and varicose lymphoedematous limb. However, oedema of any nature, if obliterating the lymphatics following repeated chronic, will have this characteristic. There is Conservative gross lymphoedema, especially of the lower Mild cases will respond to elevation and gradu limbs and genitalia, often called elephantiasis. Although asymmetry of the breasts is normal, complete failure of development of the breast may A lump in the breast occur and is often associated with chest wall defects. The diagnosis of discrete breast lumps is based on a triple assessment that comprises the following: Multicoloured, multiduct discharge 1 Clinical examination. If clinical examination and mammography are 2 Radiological imaging: normal, a diagnosis of duct ectasia is likely and no a mammography, usually in older patients further treatment is required. It is also used to detect local recurrence when ultrasound Bloody nipple discharge and mammography are unhelpful. The presence of blood in the discharge should be 3 Biopsy, usually ultrasound guided: con rmed by cytology. If blood is present, a mam a ne needle aspiration cytology; mogram (for women over 35 years) is performed b core biopsy. If there is discordance between any of the three tests, open biopsy is considered. In addition to a careful clinical exam indrawn nipples may cause problems during lac ination, patients over 35 years should also have tation but are of no other signi cance. Aetiology In addition, the patient is advised to reduce her Fat necrosis may be associated with a history of intake of caffeine and animal fats. The lump usually decreases Causes of non-cyclical mastalgia include the in size with time, but following resolution may following: leave a fat cyst within the breast. In the costochondral junctions and, left alone, absence of a rm diagnosis, an open biopsy is resolves over a number of months; recommended. Duct ectasia Acute in ammation of this is an involutional change in the ducts associ the breast (mastitis) ated with the menopause. The terminal ducts behind the nipple become dilated (ectasia) and There are three causes of acute breast engorged with secretions. Secondary infection in ammation: may lead to retroareolar abscess, and brosis may result in nipple retraction. An associated Acute bacterial mastitis mammary duct stula may be present in the peri the most common and most important acute areolar region. Ultrasound may con rm a thick in ammation of the breast; the majority occur ened or dilated duct or abscess formation. Treatment Non lactational breast abscesses may be associ ated with systemic conditions such as diabetes, Initial treatment is with appropriate antibiotics steroid therapy and rheumatoid arthritis. A mammary duct stula is treated by total duct exci Clinical features sion combined with excision of the stulous track Common symptoms include pain, swelling and between the duct and the skin. The in ammation may be localized, with erythema and tenderness of a segment of the breast, or may spread to involve the entire breast. In the later stages, there may be Chronic in ammatory a uctuant mass and patients may have a pyrexia, conditions of the breast tachycardia and leucocytosis. There are two uncommon chronic in ammatory Treatment conditions of the breast: Cellulitis 1 Lymphocytic lobulitis occurs in patients with autoimmune diseases, particularly type 1 In the early phase of mastitis, appropriate antibi diabetes mellitus, and usually presents with a otics can prevent abscess formation. The diagnosis is made on mastitis, breast-feeding should be continued as it core biopsy, with brosis and lymphoid may speed up recovery. Abscess 2 Granulomatous mastitis may be secondary to systemic conditions (sarcoidosis), infections Patients with clinical or radiological evidence of (tuberculosis, fungal) or foreign material pus should have aspiration performed in addition (silicone). Repeat aspira any organisms cultured and exclusion of tion may be necessary and resolution of the malignancy. If the abscess fails to resolve, or the overlying skin is thin or necrotic, incision and drainage should be performed. Benign breast disease Periductal mastitis From the fourth decade onwards, the breast undergoes a process termed involution. This this is an in ammatory process that occurs process includes microcyst formation and an around dilated milk ducts near the nipple; hence, increase in brous tissue within the breast. It is Aberrations of this process include the formation linked to smoking, and nipple rings may increase of large cysts, which may present as palpable the risk of infection. It occurs in premenopausal masses, and the formation of radial scars and scle women, in contrast to duct ectasia. The breast 299 Cystic disease Cysts are common in the perimenopausal age Non-neoplastic breast group but uncommon after the menopause. Fibroadenoma Clinical features Previously classi ed as a benign neoplasm, but now considered as an aberration of normal devel Cysts often present with a short history as a opment. There is may be uctuant, but tense cysts may mimic a no increased risk of malignancy and the majority solid lump. They appear as well-de ned, rounded opacities on mammography, and are clearly differentiated Clinical features from a solid lump by ultrasound.
Other primary headache disorders (hemicrania continua menopause symptoms bleeding cheap 0.625mg premarin amex, cough headache menstrual hormone chart trusted 0.625mg premarin, exertional headache breast cancer grade cheap premarin amex, hypnic headache womens health 4 garcinia proven 0.625 mg premarin, new daily persistent headache) B womens health 02 2013 chomikuj buy cheap premarin 0.625mg on line. Increased intracranial pressure/mass lesions (pseudotumor womens health and wellness buy premarin 0.625 mg mastercard, neoplasms, subdural and epidural hematomas) 4. Neuropathic pain (small fiber neuropathy, post-herpetic neuralgia, radiculopathies) B. Disorders of the optic nerve and retina (optic neuropathy, papilledema, retinal emboli, retinal infarcts) B. Guidelines for Consultation with Obstetric and Related Medical Services (Referral Guidelines). When a woman declines a referral, consultation, transfer of clinical responsibility, emergency treatment or emergency transport. The Referral Guidelines are based on best practice and are informed by available evidence, expert opinion and current circumstances in New Zealand. This version is based on the 2007 Ministry of Health publication Guidelines for Consultation with Obstetric and Related Specialist Medical Services (Referral Guidelines). Revision of the Referral Guidelines the Ministry intends these Guidelines to be reviewed at fve-yearly intervals; the review of this version should be completed by December 2016. The Guidelines may be partially or wholly reviewed before this date if emerging evidence indicates a review is appropriate; or in the event of a signifcant change in policy or service structure, or any other matter that may affect the way the Guidelines are used. The Ministry of Health wishes to acknowledge and thank the following people for their participation and contribution. Guiding principles the following principles about the care of women, babies and families/wha nau through pregnancy, birth and the postpartum period underpin the Referral Guidelines. The woman, her baby and family/wha nau (as defned by the woman) are at the centre of all processes and discussions. The woman should have continuity of maternity care through a single point of contact regardless of how her care is provided. The woman has the right to receive full, accurate, unbiased information about her options and the likely outcomes of her decisions. The woman has a right to make informed decisions on all aspects of her care, including the right to decline care, and to decline referral for specialist consultation or transfer of clinical responsibility. Practitioners are responsible for their clinical decisions and actions, and for acting within their competency and scope of practice. The approach to referral for consultation, transfer of clinical responsibility and emergency transport will be nationally consistent, with some allowance for local needs and conditions. Communication between all practitioners involved with the woman will include her, and will be open, clear, timely and appropriately documented. Transfer of clinical responsibility is a negotiated three-way process involving the woman, her Lead Maternity Carer and the practitioner to whom clinical responsibility is to be transferred. Practitioners are responsible for appropriately documenting their decisions, including any variation from the Referral Guidelines or other guidelines, and the circumstances of any such variation. This should include discussion of any ongoing management of the condition by the primary care provider. A referral to a primary care provider may result in a referral for consultation or a transfer of clinical responsibility. This responsibility will vary with the clinical situation and the wishes of the woman. Guidelines for Consultation with Obstetric and Related Medical Services (Referral Guidelines) 3 Referral category Consequent action Emergency An emergency necessitates the immediate transfer of clinical responsibility to the most appropriate practitioner available. Responding to an emergency may include providing emergency transport by road or air to a facility able to provide the necessary level of care (see Process Map 5). In such circumstances the clinical roles and responsibilities are dictated by the immediate needs of the mother and/or baby and the skills and capabilities of practitioners available including those involved in providing emergency transport if it is required. All practitioners are responsible for their clinical decisions, including the timing of referral. For these reasons the revised Guidelines do not include timing recommendations for each condition. There may be situations when services required for a woman are not available in the area, or not available at the time she needs them (eg, the woman cannot be seen in outpatient clinic in a timely fashion). The maps are designed to show the critical steps that should be undertaken in each instance. Flexibility is, however, important if the Referral Guidelines are to be used effectively. The aim is a consistent level of service that is delivered according to local needs and conditions. Women should have access to an evidence-based and consistently high standard of care, regardless of where they live. The ways that this standard of care is achieved may differ depending on local situations. Guidelines for Consultation with Obstetric and Related Medical Services (Referral Guidelines) 5 the process should provide a framework for, but not override, local protocols that have been developed involving a multidisciplinary approach to achieve the same outcome in ways that work for local needs and circumstances. Guidelines for Consultation with Obstetric and Related Medical Services (Referral Guidelines) 7 4. There are many health-related conditions that may affect pregnant women and newborn infants. The list of referral criteria does not attempt to cover all of them but instead includes those of particular relevance during pregnancy. Most New Zealand women are enrolled with a general practice or primary health care clinic which holds their medical records and provides care for ongoing medical needs. Many women attend their general practice to confrm pregnancy and receive initial advice. General practice care is partially subsidised, and normally incurs a part charge even when it is provided to women who are pregnant. The referral may result in a recommendation that the condition requires a referral for specialist consultation or a transfer of clinical responsibility, covered by the consultation or transfer process maps. Communication and information sharing by all parties must be timely, appropriate and complete. Guidelines for Consultation with Obstetric and Related Medical Services (Referral Guidelines) 9 4. The specialist consultation may be done by an individual practitioner, and may include review by a secondary services team. In most cases the specialist will be an obstetrician; however in some circumstances a referral to another specialist, such as an anaesthetist, physician, psychiatrist, surgeon or paediatrician, may be appropriate. The specialist may be responsible for management of the specifc condition if that is appropriate and warranted. Guidelines for Consultation with Obstetric and Related Medical Services (Referral Guidelines) 11 4. It will also vary according to geographical considerations; some women may be transferred to the care of a specialist in the nearest main centre due to limited options in their local area. Guidelines for Consultation with Obstetric and Related Medical Services (Referral Guidelines) 13 4. The type of practitioner will depend on the specifc condition and whether the emergency is taking place within a hospital, in the community or at a primary unit. Roles and responsibilities the roles and responsibilities during the emergency will be defned by clinical need. Generally, the most experienced and relevant practitioner will take the lead and advise others of what actions they should take. The transfer of clinical responsibility must be clearly established and documented at the time or as soon as practicable once the situation has stabilised. Communication Effective communication with the woman and her family/wha nau (as defned by the woman) is essential in an emergency. Communication with the woman may be diffcult in some cases due to the nature of the emergency. Although the woman retains the right to decline treatment or transport and also the right to receive complete information, the situation may mean that a comprehensive discussion of benefts, risks and options is not possible. The woman may not be legally competent to make decisions due to the nature of the emergency. Where possible clinical responsibility is transferred to the appropriate specialist and this is clearly documented No Does care plan Move to Process Is transport involve emergency Yes Yes Map 5: Emergency available The emergency is reviewed and explained to the woman * the woman, her baby and family/wha nau (as defned by the woman) are at the centre of all conversations and decisions about her care. Guidelines for Consultation with Obstetric and Related Medical Services (Referral Guidelines) 15 4. Ask the call taker when transport will arrive; prepare for transport * the woman, her baby and family/wha nau (as defned by the woman) are at the centre of all conversations and decisions about her care. Guidelines for Consultation with Obstetric and Related Medical Services (Referral Guidelines) 17 5. This means that a woman can choose to decline treatment, referral to another practitioner, or transfer of clinical responsibility. Guidelines for Consultation with Obstetric and Related Medical Services (Referral Guidelines) 19 6. The referral categories are detailed in Section 3 of these Guidelines (page 3) and the processes that should be used are detailed in Section 4 (page 5). A condition that is normally a cause for a referral to a primary care practitioner may be severe enough on presentation to warrant a specialist consultation. Placing a condition in the Consultation category does not preclude a subsequent transfer of clinical responsibility if that is indicated by the results of the consultation, or if the condition persists or worsens. Take into consideration descent and rotation of fetal head, and changes in strength, duration and frequency of contractions. Refer prior to Transfer delivery 8034 Maternal thrombocytopaenia Consultation Infection 8036 Suspected chorio-amnionitis Fetal tachycardia, maternal pyrexia, Consultation offensive liquor 8037 Temperature instability Temp < 36. Consultations may involve the woman and/or baby being seen by the other practitioner; however, a discussion between practitioners is often appropriate on its own. Consultations can take place in person, by telephone, or by other means as appropriate in the situation. Emergency transport the physical transport of a woman and/or baby in an emergency. Primary birthing unit A community-based birthing unit, usually staffed by midwives. Primary birthing units provide access for women assessed as being at low risk of complications for labour and birth care. Primary care provider A health care provider who works in the community and who is not a specialist for the purposes of these Guidelines. This provider may be a general practitioner, midwife, physiotherapist or lactation consultant, or smoking cessation services, drug and alcohol services or maternal mental health services. Guidelines for Consultation with Obstetric and Related Medical Services (Referral Guidelines) 31 Specialist A medical practitioner who is registered with a vocational scope of practice in the register of medical practitioners maintained by the Medical Council of New Zealand and who holds a current annual practising certifcate. Secondary maternity A hospital that provides care for normal births, complicated pregnancies hospital and births including operative births and caesarean sections plus specialist adjunct services including anaesthetics and paediatrics. As a minimum, secondary facilities include an obstetrician rostered on site during working hours and on call after hours, with access to support from an anaesthetist, paediatrician, radiological, laboratory and neonatal services. Registrars involved in the provision of secondary care are required to follow applicable clinical guidelines endorsed by the relevant professional college. Tertiary maternity A hospital that provides care for women with high-risk, complex hospital pregnancies, by specialised multidisciplinary teams. Tertiary maternity care includes an obstetric specialist or registrar immediately available on site 24 hours a day. In obstetric emergencies, transfer of clinical responsibility will be to the most appropriate available practitioner. Woman When the term woman is used, it includes her baby and family/wha nau, as defned by her. For anyone experiencing stroke, proceed immediately to a hospital, preferably a facility that can provide stroke care. In no way should these recommendations be regarded as absolute rules, since nuances and peculiarities in individual patients, situations or communities may entail differences in specific approaches.
Premarin 0.625 mg free shipping. Jeevanarekha Women's Health | Month 4 Pregancy | 27th September 2016 | Full Episode.
Neurophysiologically breast cancer types 0.625mg premarin visa, akinesia is associated with loss of dopamine projec tions from the substantia nigra to the putamen women's health promotion issues buy premarin 0.625mg amex. However women's health & family services premarin 0.625mg mastercard, many parkinsonian/akinetic-rigid syndromes show no or only partial response to these agents menstrual app purchase premarin 0.625 mg on-line. Frontal release signs menopause estradiol levels buy discount premarin on line, such as grasping and sucking breast cancer 4mm lump 0.625 mg premarin amex, may be present, as may double inconti nence, but there is a relative paucity of upper motor neurone signs affecting either side of the body, suggesting relatively preserved descending pathways. Akinetic mutism represents an extreme form of abulia, hence sometimes referred to as abulia major. Pathology may be vascular, neoplastic, or structural (subacute communicating hydrocephalus), and evident on structural brain imaging. Akinetic mutism may be the nal state common to the end-stages of a number of neurodegenerative pathologies. Akinetic mutism from hypothalamic damage: successful treatment with dopamine agonists. Cross References Aphasia; Aphemia Alexia Alexia is an acquired disorder of reading. The word dyslexia, though in some ways equivalent, is often used to denote a range of disorders in people who fail to develop normal reading skills in childhood. Patients lose the ability to recognize written words quickly and easily; they seem unable to process all the elements of a written word in parallel. They can still access meaning but adopt a laborious letter-by-letter strategy for reading, with a marked word length effect. Alexia without agraphia often coexists with a right homonymous hemianopia, and colour anomia or impaired colour perception (achromatopsia); this latter may be restricted to one hemi eld, classically right-sided (hemiachromatopsia). Pure alexia has been characterized by some authors as a limited form of associative visual agnosia or ventral simultanagnosia. Patients tend to be slower with text than single words as they cannot plan rightward reading saccades. The various forms of peripheral alexia may coexist; following a stroke, patients may present with global alexia which evolves to a pure alexia over the following weeks. Pure alexia is caused by damage to the left occipitotemporal junction, its afferents from early mesial visual areas, or its efferents to the medial temporal lobe. Global alexia usually occurs when there is additional damage to the splenium or white matter above the occipital horn of the lateral ventricle. Hemianopic alexia is usually associated with infarction in the territory of the posterior cerebral artery damaging geniculostriate bres or area V1 itself, but can be caused by any lesion outside the occipital lobe that causes a macular splitting homonymous eld defect. Neglect alexia is usually caused by occipitoparietal lesions, right-sided lesions causing left neglect alexia. There is evidence from functional imag ing studies that alexithymics process facial expressions differently from normals, leading to the suggestion that this contributes to disordered affect regulation. Alexithymia is a common nding in split-brain patients, perhaps resulting from disconnection of the hemispheres. Alexithymia: an experi mental study of cerebral commissurotomy patients and normal control subjects. Other conditions may also give rise to the phenomena of microsomatognosia or macrosomatognosia, including epilepsy, encephalitis, cerebral mass lesions, schizophrenia, and drug intoxication. Alien Grasp Re ex the term alien grasp re ex has been used to describe a grasp re ex occurring in full consciousness, which the patient could anticipate but perceived as alien. These phenomena were associated with an intrinsic tumour of the right (non-dominant) frontal lobe. Cross References Alien hand, Alien limb; Grasp re ex Alien Hand, Alien Limb An alien limb, most usually the arm but occasionally the leg, is one which man ifests slow, involuntary, wandering (levitating), quasi-purposive movements. These phenomena are often associated with a prominent grasp re ex, forced groping, intermanual con ict, and magnetic move ments of the hand. Frontal type: shows features of environmental dependency, such as forced grasping and groping, and utilization behaviour. A paroxysmal alien hand has been described, probably related to seizures of frontomedial origin. Functional imaging studies in corticobasal degeneration, along with the evi dence from focal vascular lesions, suggest that damage to and/or hypometabolism of the medial frontal cortex (Brodmann area 32) and the supplementary motor area (Brodmann area 6) is associated with alien limb phenomena. More gen erally, it seems that these areas are involved in the execution of learned motor programs, and damage thereto may lead to the release of learned motor programs from voluntary control. Slowly progressive aphasia in three patients: the problem of accompanying neuropsychological de cit. Alloacousia Alloacousia describes a form of auditory neglect seen in patients with unilateral spatial neglect, characterized by spontaneous ignoring of people addressing the patient from the contralesional side, failing to respond to questions, or answering as if the speaker were on the ipsilesional side. Cross Reference Neglect Alloaesthesia Alloaesthesia (allesthesia, alloesthesia) is the condition in which a sensory stim ulus given to one side of the body is perceived at the corresponding area on the other side of the body after a delay of about half a second. The trunk and proximal limbs are affected more often than the face or distal limbs. Tactile alloaesthesia may be seen in the acute stage of right putaminal haemorrhage (but seldom in right thalamic haemorrhage) and occasionally with anterolateral spinal cord lesions. The mechanism of alloaesthesia is uncertain: some 20 Allodynia A consider it a disturbance within sensory pathways, others consider that it is a sensory response to neglect. Cross References Allochiria; Allokinesia, Allokinesis; Neglect Allochiria Allochiria is the mislocation of sensory stimuli to the corresponding half of the body or space, a term coined by Obersteiner in 1882. There is overlap with alloaesthesia, originally used by Stewart (1894) to describe stimuli displaced to a different point on the same extremity. Examples of allodynia include the trigger points of trigeminal neuralgia, the affected skin in areas of causalgia, and some peripheral neuropathies; it may also be provoked, paradoxically, by prolonged morphine use. The treatment of neuropathic pain is typically with agents such as carba mazepine, amitriptyline, gabapentin, and pregabalin. Interruption of sympa thetic out ow, for example with regional guanethidine blocks, may sometimes help, but relapse may occur. Cross References Hyperalgesia; Hyperpathia 21 A Allographia Allographia this term has been used to describe a peripheral agraphia syndrome character ized by problems spelling both words and non-words, with case change errors such that upper and lower case letters are mixed when writing, with upper and lower case versions of the same letter sometimes superimposed on one another. These defects have been interpreted as a disturbance in selection of allographic forms in response to graphemic information outputted from the graphemic response buffer. Cross Reference Agraphia Allokinesia, Allokinesis Allokinesis has been used to denote a motor response in the wrong limb. Others have used the term to denote a form of motor neglect, akin to alloaesthesia and allochiria in the sensory domain, relat ing to incorrect responses in the limb ipsilateral to a frontal lesion, also labelled disinhibition hyperkinesia. Altitudinal eld defects 22 Amblyopia A are characteristic of (but not exclusive to) disease in the distribution of the cen tral retinal artery. Central vision may be preserved (macula sparing) because the blood supply of the macula often comes from the cilioretinal arteries. Cross References Hemianopia; Macula sparing, Macula splitting; Quadrantanopia; Visual eld defects Amaurosis Amaurosis is visual loss, with the implication that this is not due to refractive error or intrinsic ocular disease. The term is most often used in the context of amaurosis fugax, a transient monocular blindness, which is most often due to embolism from a stenotic ipsilateral internal carotid artery (ocular transient ischaemic attack). Giant cell arteritis, systemic lupus erythematosus, and the antiphospholipid antibody syndrome are also recognized causes. Gaze-evoked amaurosis has been associated with a variety of mass lesions and is thought to result from decreased blood ow to the retina from compression of the central retinal artery with eye movement. Amblyopic eyes may demonstrate a relative afferent pupillary defect and sometimes latent nystagmus. Amblyopia may not become apparent until adulthood, when the patient sud denly becomes aware of unilateral poor vision. The nding of a latent strabismus (heterophoria) may be a clue to the fact that such visual loss is long-standing. This is a component of long-term (as opposed to working) memory which is distinct from memory for facts (semantic memory), in that episodic memory is unique to the individual whereas semantic memory encompasses knowledge held in common by members of a cultural or linguistic group. A precise clinical de nition for amnesia has not been demarcated, perhaps re ecting the heterogeneity of the syndrome. Amnesia may be retrograde (for events already experienced) or anterograde (for newly experienced events). Retrograde amnesia may show a temporal gradi ent, with distant events being better recalled than more recent ones, relating to the duration of anterograde amnesia. In a pure amnesic syndrome, intelligence and attention are normal and skill acquisition (procedural memory) is preserved. Retrograde mem ory may be assessed with a structured Autobiographical Memory Interview and with the Famous Faces Test. Poor spontaneous recall, for example, of a word list, despite an adequate learning curve, may be due to a defect in either stor age or retrieval. This may be further probed with cues: if this improves recall, then a disorder of retrieval is responsible; if cueing leads to no improvement or false-positive responses to foils (as in the Hopkins Verbal Learning Test) are equal or greater than true positives, then a learning defect (true amnesia) is the cause. The neuroanatomical substrate of episodic memory is a distributed system in the medial temporal lobe and diencephalon surrounding the third ventricle (the circuit of Papez) comprising the entorhinal area of the parahippocam pal gyrus, perforant and alvear pathways, hippocampus, mbria and fornix, mammillary bodies, mammillothalamic tract, anterior thalamic nuclei, inter nal capsule, cingulate gyrus, and cingulum.
In addition to these toxicities women's oral health issues cost of premarin, four patients developed leg ulcers pregnancy videos purchase premarin 0.625mg fast delivery, three developed skin rashes pregnancy journal purchase premarin in india, and two developed significant anemia womens health workouts order cheap premarin online. The final study we reviewed examined the outcomes of 34 patients with polycythemia vera who had been treated with hydroxyurea menstrual vs estrous cycles discount 0.625 mg premarin, 30 with essential thrombocytosis who had been treated with hydroxyurea women's health center nyu purchase 0.625 mg premarin otc, 1 with polycythemia vera who had been treated with busulfan, and 4 with essential thrombocytosis who had been treated with interferon. Of the 34 polycythemia vera patients treated with hydroxyurea for a mean of 86 months, 2 (5. The most frequently reported complication was leg ulcer (66 reports), followed by dermatologic changes (34 reports), including hyperpigmentation, rashes consistent with dermatomyositis, and others. There were 27 reports of skin neoplasms, including epitheliomas, actinic keratoses, basal cell cancers, and, most frequently, squamous cell cancers. Level 1 evidence supports a causal role for hydroxyurea in leg ulcers and in skin neoplasms. Fever was also a frequently reported event (15 reports), with Level 1 evidence to support a role for hydroxyurea. The reported pulmonary complications included two reports of alveolitis, with Level 2 evidence supporting causality; one report of pulmonary fibrosis with only Level 3 evidence; and five reports of interstitial pneumonitis, with Level 1 evidence, supporting the causality of hydroxyurea in this complication. The mean age of these patients was 32 years (range, 43 to 87 years), and 45 percent were female. The mean length of of hydroxyurea treatment was almost 6 years, with a range of 12 weeks to 17 years. As discussed above, it was impossible to describe the causality as being certain or probable in this scoring system, given a condition that cannot regress. The other toxicities with Level 1 evidence included azospermia or a decrease in sperm motility, limbal stem cell deficiency (a corneal condition), and pruritis. The few other findings 66 we noted were that leg ulcers at baseline were associated with leg ulcers while on therapy, and Table 7. Similarly, there was insufficient evidence to allow us to assess whether exposure in utero causes developmental defects, although there was low-grade evidence that the use of hydroxyurea in pregnancy is not commonly associated with adverse perinatal outcomes. There was low-grade evidence, including the efficacy studies that we reviewed, that hydroxyurea is not associated with growth delays in children and adolescents. We graded separately the evidence regarding toxicities of hydroxyurea in adults in the case of patients with sickle cell disease and those with other diseases. We used the evidence from other diseases as indirect evidence regarding toxicities that could be potentially expected in patients with sickle cell disease. The evidence from patients with other diseases also provided low-grade evidence that the drug is not associated with leukemia. High-grade evidence supported that hydroxyurea is not associated with leg ulcers in patients with sickle cell disease, although high-grade evidence supported the claim that it is associated with leg ulcers in patients with other conditions. The evidence was insufficient in sickle cell disease to indicate whether hydroxyurea contributes to skin neoplasms, although high grade evidence in other conditions supported the possibility that it does. Similarly, there was insufficient evidence to indicate whether hydroxyurea is associated with secondary malignancies in adults with sickle cell disease, and the evidence in other diseases was only low-grade. There was also insufficient evidence regarding pregnancy outcomes in treated patients with sickle cell disease, and the evidence from patients with other diseases was low-grade but supported a lack of adverse effects. Low-grade evidence supported the possibility that hydroxyurea is associated 57 with spermatogenesis defects in patients with sickle cell disease, and this relationship was supported by low-grade evidence from other conditions (Table 5). What are the Barriers to the Use of Hydroxyurea Treatment (and other therapies) for Patients who have Sickle Cell Disease and what are the Potential Solutions Characteristics of Studies Addressing Barriers to the Use of Therapies for Sickle Cell Disease Of the studies that addressed this key question, 15 employed a cross-sectional study design to 138-152 test an association between a patient, provider, or system factor and the use of therapy; 18 93,153,153-168 described patient and/or provider-reported barriers to therapy; and 3 used both 155,169,170 methods. Studies employing cross-sectional designs to assess the association between a patient, provider, or system factor and the use of therapies are shown in Appendix C, Evidence Table 25, and studies describing patient and/or provider-reported barriers to therapy are shown in Appendix C, Evidence Table 26. Of the 18 studies using a cross-sectional design (Appendix C, Evidence Table 25), only 1 addressed barriers to the use of therapies to 138 increase Hb F, 8 addressed barriers to the use of established therapies for management of 139-144,169,170 sickle cell disease, 3 addressed barriers to the use of appropriate pain medication 145,146,155 during vaso-occlusive crises, and 6 addressed barriers to the use of routine, scheduled 147-152 care for sickle cell disease. The one study that dealt with therapies to increase Hb F examined factors associated with 138 patient (or parent) decisions to initiate therapy. Of the eight studies that addressed barriers to 139 the use of established therapies, one focused on patient adherence to chelation therapy, while 140-144,169,170 the remainder focused on patient adherence to antibiotic prophylaxis. Of the six studies that dealt with routine, scheduled care, 147,148,150 three directly addressed the use of routine health services, one addressed the transition 149 152 to adult care, one addressed appointment-keeping, and one addressed general adherence. Three of the 18 cross 140 145,155 sectional studies focused on health professionals as study subjects, while the remainder studied patients. Adult patients with sickle cell disease were the targeted patient population of 152 interest in only 1 of the 18 cross-sectional studies. In four of the cross-sectional studies, 147,149,150,155 children and adults were the targeted patient population of interest. The majority were conducted in the United States, 170 while one was conducted in Saudi Arabia and five did not specify a location. Of the 20 descriptive studies of patient and provider-reported barriers to the use of therapies for sickle cell disease (Appendix C, Evidence 93 Table 26), 1 addressed barriers to the receipt of treatment to increase Hb F, 2 addressed 169,170 barriers to patient adherence to established therapies for disease management, 13 addressed 153-155,159-168 barriers to the receipt of pain medications, 1 addressed barriers to bone marrow 158 156,157,171 transplantation, and 3 addressed barriers to generic healthcare quality. About half of the descriptive studies were published in the past decade (1998-2007), with the remainder published in the preceding decade (1988-1997). Most (n=13) descriptive studies occurred in the United States; however, 6 were conducted in the United Kingdom, 154,159,161,163,166,168 170 and one was conducted in Saudi Arabia. Of the 20 descriptive studies, 9 used primarily quantitative descriptive methods. Results of Studies Addressing Barriers to the Use of Therapies for Sickle Cell Disease Results of cross-sectional studies testing associations. Each of the potential barriers and facilitators below was identified in only one study. The factors in each category that were examined but not associated with use of therapies are included in Table 8 but not detailed below. The eight studies that addressed potential barriers to the use of established therapies for disease management found two potential patient-related barriers (family stress and having more children in the home), and one potential system-related barrier (being seen in an academic 139-144,169,170 medical center). These eight studies also identified 11 potential patient-related facilitators of the use of established therapies for disease management (private insurance, sharing of responsibilities between parent and child, more hospital visits, more adults in the home, having a car, no child prior history of transfusion, younger patient age, more caregiver knowledge, greater intent to adhere, greater perceived benefits, and family employment) and two potential provider-related facilitators (provider female gender and pediatric specialty). The three studies that addressed barriers to the use of appropriate pain medication during vaso-occlusive crisis found one patient-related barrier (an increased number of hospital visits was associated with less optimal pain management) and one provider-related barrier (negative 145,146,155 provider attitudes). These studies also found one potential patient-related facilitator (dispositional optimism being associated with better patient use of pain medications) and two potential provider-related facilitators (provider female sex and fewer years in practice). Bivariate results in one of the two studies suggested that rural patients have less utilization when travel distance is not controlled. The six studies that addressed barriers to use of routine, scheduled care for sickle cell 147-152 disease found one potential patient-related barrier (greater community socio-economic distress) and eight potential patient-related facilitators (greater parental knowledge, rural geographic region, higher self-efficacy, female patient sex, higher family problem-solving effort, higher family income, greater illness-related stress, and greater social support). Of note, the studies that found rural location to be a potential facilitator controlled for distance to the clinic, which may have eliminated the typical reason for decreased access by rural patients. The results of studies employing descriptive methodologies to identify patient and provider-reported barriers to the use of therapies are summarized in Table 9. The two studies that addressed barriers to the use of established therapies for disease management both examined patient (caregiver)-reported reasons for missing doses of prophylactic antibiotic medication and found that caregivers reported missing doses as a result of forgetting, being too busy, running out of medication, having the child fall asleep, and the child 169,170 not liking the taste of the medication. Other barriers identified by patients and providers included poor provider knowledge of sickle cell disease (mentioned in five studies), lack of time (mentioned in two studies), inadequate pain assessment tools (mentioned in two studies), and race (mentioned in one study). The one study that addressed barriers to bone marrow transplantation found that providers from bone marrow transplant centers reported that the major barriers to bone marrow transplantation for patients with sickle cell disease were lack of a donor, lack of psychosocial or 158 financial support, a history of patient noncompliance, parental refusal, and physician refusal. The three studies that addressed barriers to general healthcare quality found that patients and providers reported that three patient-related factors (patient race, older patient age, and patient 156,157,171 male sex) may affect the quality of care provided to patients with sickle cell disease. Strength of the evidence of the existence of barriers to the use of therapies in sickle cell disease. There was insufficient evidence to allow us to identify barriers to the use of hydroxyurea. Regarding barriers to the use of established therapies for sickle cell disease, four items were identified as either barriers, facilitators, or neither in more than two studies and thus were eligible for evidence grading. These were patient/family knowledge, number of hospital visits, patient age, and patient sex. We concluded that the evidence that sex is not a barrier to the use of therapies was of a moderate grade. Largely due to the relative paucity of studies and their inconsistency, we concluded that there was only low-grade evidence that patient/family knowledge, the number of hospital visits, and patient age are barriers. The evidence for the remaining barriers to the use of established therapies was insufficient to allow us to draw any conclusions. Regarding barriers to pain management, we identified two factors that were identified as a barrier in more than two studies and were thus eligible for evidence grading. There was insufficient evidence to allow us to identify barriers to the use of routine health services and bone marrow transplantation for sickle cell disease (Table 5). Characteristics of Studies Addressing Interventions to Overcome Barriers to the Appropriate Use of Therapies 172-184 Thirteen studies addressed interventions to increase the appropriate use of therapies. None of these studies focused on interventions to increase the appropriate use of hydroxyurea. Nine focused on provider interventions to increase the appropriate provision of pain medications 172-180 for patients with vaso-occlusive crisis, three focused on patient interventions to improve 181 182 adherence to therapies (desferoxime, antibiotics, and general adherence to health 183 promoting activities), and one focused on a patient intervention to improve the receipt of routine, scheduled health care for sickle cell disease (Appendix C, Evidence Tables 27 and 28). The majority of the provider interventions to improve pain management involved clinical 172-175,178,180 177 protocols/pathways, while one primarily involved audit and feedback, and two 176 involved changing the structure of care through the use of a day hospital or a fast-track 179 admission process. In addition, one of the clinical protocol/pathway interventions included 174 staff sensitivity training. The effect of interventions to improve pain management was measured directly in terms of 173,175 its impact on pain management quality, as assessed by medical record review in six studies 177,179,180 174,179,180 and patient ratings in three studies; the effect of such interventions was also 175 172,174,176,178 assessed indirectly through healthcare utilization in five studies and healthcare 174,175 costs in two studies. No study examined the impact of an intervention directly on patient reported levels of pain. Results of Studies Addressing Interventions to Overcome Barriers to the Appropriate Use of Therapies A summary of the results of studies addressing interventions to increase the appropriate use of therapies is provided in Table 10 (see also Appendix C, Evidence Tables 27 and 28). Four of the studies that measured the impact of an intervention to improve the quality of pain management during vaso-occlusive crisis showed improvement in one or more direct outcomes, 173,179,180,185 while the remaining five studies showed potential improvement either through the suggestion of an improvement on a direct outcome (without a statistical test) or a statistically significant improvement in one or more indirect outcomes. Two of the three studies that focused on patient interventions to improve adherence to 181 therapies showed no effect of the intervention on patient adherence to desferoxime or to 182 antibiotic prophylactic therapy. One of the studies that focused on patient interventions to improve adherence to therapies showed no increase in health-promoting activities as a result of the intervention but did show some improvements in child health-related quality of life and 183 child-parent relationships. The one study that evaluated a patient intervention to improve receipt of routine, scheduled health care for sickle cell disease demonstrated a substantial and significant reduction in the 184 percent of patients who had not attended clinic over the past 2 years. The strength of the evidence addressing interventions to overcome barriers to the use of therapies. The evidence was insufficient to allow us to identify interventions to overcome barriers to the use of hydroxyurea and bone marrow transplantation. None of the three studies testing interventions to improve patient adherence to established therapies for chronic disease management showed any effect on patient adherence. However, due to the small sample sizes and diverse outcome measures, we concluded that there was only low grade evidence that interventions cannot improve patient adherence. We concluded that there was moderate evidence that interventions can overcome barriers to the use of pain medications and moderate evidence to support the contention that interventions Appendixes cited in this report are provided electronically at. Discussion Since its approval for the treatment of sickle cell disease in 1998, hydroxyurea has been under intense study. The body of evidence supporting its use is large but is mainly based on observational data. There have been only two randomized controlled trials of the use of this drug in sickle cell disease, although an additional large trial is nearing completion. The other studies of this drug have included several controlled studies comparing patients receiving hydroxyurea to patients receiving another intervention or usual care, but the vast majority of the studies have been observational studies, including well-described prospective cohorts and many small studies reporting patient experiences pre and post-treatment with hydroxyurea. In addition, the literature is replete with case reports describing toxicities ascribed to hydroxyurea, although the majority of these reports concern diseases other than sickle cell disease. Few studies have specifically identified barriers to the use of hydroxyurea in patients with sickle cell disease. No studies have tested an intervention to improve patient acceptance of this medication or patient adherence. For this report, we opted to review the literature related to barriers to the use of other medications and treatments in patients with sickle cell disease, since we believe that the barriers may often be similar. In this section, we describe key findings from our literature review, describe the limitations of this body of literature, and discuss the limitations of our report. We also describe studies that are in progress and make suggestions, based on the gaps in the current evidence, with regard to studies that should be undertaken in the future. In this Belgian study, the rate of hospitalization and number of days hospitalized per year were significantly 44 lower in the hydroxyurea group than in the placebo group. The small size of this study and the short duration of treatment with the drug (6 months) did not provide adequate data to permit assessment of the long-term responses to hydroxyurea. The results of this trial are supported by data from 20 observational studies in children. Interpretation of many of these observational studies is complicated by their incomplete description of losses to followup.
References
- Rogers J, Dieppe P. Skeletal palaeopathology of the rheumatic diseases. Where are we now? Ann Rheum Dis 1990; 49:885-6.
- Markov AK, Brumley MA, Figueroa A, Skelton TN, Lehan PH. Hemodynamic effects of fructose 1,6-diphosphate in patients with normal and impaired left ventricular function. Am Heart J. May 1997;133(5):541-549.
- Wenger S, Meisinger V, Brucke T, Deecke L. Acute porphyric neuropathy during pregnancy-effect of hematin therapy. Eur Neurol. 1998;39:187-188.
- Sanders RJ, Hammond SL. Etiology and pathology. Hand Clin. 2004;20(1):23-26.
- Cipriano GF, Peres PA, Cipriano G Jr, Arena R, Carvalho AC. Safety and cardiovascular behavior during pulmonary function in patients with Marfan syndrome. Clin Genet 2010;78:57-65.