Gerard R. Manecke, Jr., MD
- Clinical Professor of Anesthesiology
- Chair, Department of Anesthesiology
- University of California, San Diego
- La Jolla, California
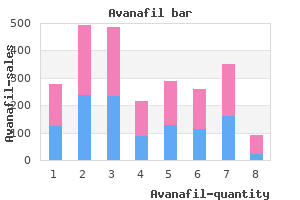
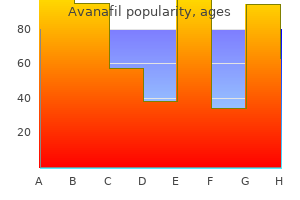
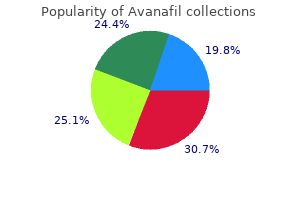
It has a predilection for the head and neck erectile dysfunction 23 years old cheap avanafil on line, a high recurrence rate after excision erectile dysfunction caused by vicodin safe 200mg avanafil, and a propensity to spread through lymphatic channels erectile dysfunction pills cheap purchase avanafil. Collagen fibers separate tumor cells that contain abundant cytoplasmic lumina and are arranged in a single file erectile dysfunction at age 24 avanafil 50 mg fast delivery. An ultrastructural examination of Merkel cell tumors reveals membrane-bound granules erectile dysfunction kuala lumpur order avanafil uk, perineural microfilaments, desmosomes, and actin-containing filaments. Merkel cell lesions may clinically resemble the glomus tumor-a benign vascular hamartoma. Glomus tumors may be solitary or multiple, are tender to touch, and only rarely affect the face and eyelid. Histologic evaluation discloses large, dilatated vascular channels lined by glomus cells. Esmaeli and co-workers167 has reported the feasibility and potential usefulness of sentinel node biopsy as a method of uncovering occult Merkel cell metastatic to head and neck nodes. Peters, Meyer, Shields, and collaborators168 reported 14 cases of Merkel cell carcinoma of the eyelids with patients ranging in age from 48 to 95 years. The mass is located within the dermis, has a firm or rubbery consistency, and enlarges slowly. Zimmerman,171 McMahon and coworkers,172 and Tripathi and associates173 have proposed an aberrant developmental scheme to explain the numerous findings. They believe that surface ectodermal cells that normally form the lens plate and vesicle remain outside the optic vesicle as the embryonic tissue closes. These cells migrate into the inferonasal lid, multiply, and undergo rudimentary differentiation to form this phakomatous choristoma. Mazoujian G, Margolis R: Immunohistochemistry of gross cystic disease fluid protein in 65 benign sweat gland tumors of the skin. Schopf E, Schulz H-J, Passarge E: Syndrome of cystic eyelids, palmoplantar keratosis, hypodontia and hypotrichosis as a possible autosomal recessive trait. Wilson-Jones E, Heyl T: Naevus sebaceus: a report of 140 cases with special regard to the development of secondary malignant tumors. Dalle S, Skowron F, Balme B, et al: Apocine carcinoma developed in nevus sebaceus of Jadasohn. Tappeiner J, Wolff K: Hidradenoma papilliferum: eine enzymhistochemische und elektronenmikroskopische studie. Shintaku M, Tsuta K, Yoshida, et al: Apocrine adenocarcinoma of the eyelid with aggressive biological behavior: report of a case. Varela-Durah J, Diaz-Flores L, Varela-Nunez R: Ultrastructure of chondroid syringoma. Ishlmura E, Iwamoto H, Kobushi Y, et al: Malignant chondroid syringoma: report of a case with widespread metastases and review of pertinent literature. Hernandez-Perez E, Cestoni-Parducci R: Nodular hidradenoma and hidradenocarcinoma: a 10 year review. Hashimoto K, Kanzaki T: Appendage tumors of the skin: histogenesis and ultrastructure. Boi S, DeConcini M, Detassis C: Mucinous sweat gland adenocarcinoma of the inner canthus: a case report. Kivela T, Tarkkanen A: the Merkel cell and associated neoplasms in the eyelids and periocular regions. The section on eyelid melanoma includes information about histologic features, clinical characteristics, preferred biopsy techniques, and classification and staging. Local treatment options, including surgical resection, definition of appropriate surgical margins, and adjuvant postoperative radiation therapy or chemotherapy, are also outlined. The metastatic potential of eyelid melanoma and its association with conjunctival melanoma is emphasized. The chapter also includes a detailed discussion of sentinel node biopsy for ocular adnexal melanomas including indications, surgical technique, and experience to date. Given that melanomas at the eyelid margin can involve the palpebral and tarsal conjunctiva and, if untreated, can extend onto the bulbar conjunctiva, several sections of the chapter include references to conjunctival melanoma. However, a detailed discussion of conjunctival melanoma and its management is beyond the scope of this chapter. We will review the histologic features, clinical characteristics, classification and staging, local therapy, and patterns of regional and distant-organ metastasis for eyelid melanomas. Malignant melanocytic proliferations evolve through a series of discrete stages characterized by distinct histologic features and progressive acquisition of autonomous growth characteristics, and invasive and metastatic potential. Premalignant melanocytic proliferations can be divided into two broad categories: melanocytic nevi and de novo melanocytic proliferations. Melanocytic nevi can be classified as common acquired nevus, congenital nevus, compound nevus of Spitz, cellular blue nevus, or dysplastic nevus. De novo melanocytic proliferations can be classified as lentigo maligna (the superficial form of lentigo maligna melanoma) or melanoma in situ. Type A nevus cells are ovoid, contain small dendritic processes, and often contain coarse melanin granules. Compound nevi contain a junctional component like that of junctional nevi plus a dermal component. Type B cells are round or cuboidal, have a monotonous appearance, and are composed of a non-melanin-containing, often bluish cytoplasm with a small nucleus. Type B cells exist in nests within the papillary dermis and do not infiltrate the reticular dermis. Type C cells are elongated, fibroblast-like cells with a vacuolated nucleus and usually do not contain melanin. It is thought that compound nevi typically progress from intraepidermal type A to dermal type B and then to type C nevus cells. Dermal nevi usually contain type B and type C nevus cells or just type C nevus cells. Common acquired nevi are associated with a small risk of malignant transformation. Some studies suggest that up to 50% of melanomas are associated with a dermal nevic component. A dysplastic nevus is a melanocytic proliferation with features intermediate between those of common acquired nevi and melanoma. Dysplastic nevus is a unique precursor of melanoma and is also a marker for increased risk of melanoma in individuals with a family history of this disease. The diagnosis of dysplastic nevus is mainly based on histologic and architectural features, particularly abnormalities seen in the intraepidermal component. Congenital nevus can also be distinguished from acquired nevus on the basis of histologic findings: only congenital nevi are associated with the presence of nevus cells in the lower reticular dermis or subcutaneous fat in a single-cell array or with the presence of nevus cells in nests in sebaceous glands in the lower portions of hair follicles and in the hair papillae. The presence of nevus cells in the walls of small arteries and veins is also thought to be unique to congenital nevi. Giant congenital nevi can give rise to melanoma, but this is thought to be a rare occurrence. Although melanomas can arise in any component of a congenital nevus, they most frequently arise in the dermal component of giant congenital nevi. The cells of compound nevi of Spitz are usually fusiform or epithelioid and contain granular or coarse melanin. Although the exact incidence is not well documented, Spitz nevi are only rarely associated with malignant transformation. A spectrum of atypia is seen in these nevi, and some have been documented to show metastatic behavior. Lentigo maligna is usually present in elderly individuals in their seventies or eighties in severely sun-damaged skin with solar elastosis. The risk of true transformation to invasive melanoma is somewhat controversial but has been estimated to be as high as 30% in some studies and as low as 5% in others. Cellular blue nevus is an uncommon variant of blue nevus that can rarely give rise to a malignant blue nevus. Cellular blue nevi contain fascicles of relatively amelanotic spindle cells in addition to the dendritic melanocytes. Although the exact incidence is unknown, periorbital cellular blue nevus can lead to ocular adnexal melanoma. Melanocytic Lesions of the Eyelid and Ocular Adnexa There are biologic differences between the radial and vertical growth phases. Most evidence suggests that melanomas in radial growth phase lack the capacity for metastasis. In contrast, melanomas in vertical growth phase represent groups of melanoma cells that have achieved a growth advantage over the surrounding population and have the capacity to metastasize. They generally lose the capacity for pigment synthesis, and thus vertical-growth-phase melanomas often appear amelanotic. However, superficial spreading melanomas and nodular melanomas with similar tumor thickness are associated with a similar prognosis. Lentigo maligna melanoma accounts for fewer than 10% of cases of cutaneous melanoma. Usually it takes a long time for the superficial precursor lesion, lentigo maligna, to evolve into lentigo maligna melanoma. The typical appearance of lentigo maligna melanoma at presentation is a large area of flat, tanbrown pigmentation with areas of irregular mottling of pigment. However, eyelid melanomas may involve the conjunctiva and ocular adnexal structures and thus require unique considerations. The typical patient with eyelid melanoma has a fair complexion and a tendency to sunburn rather than tan after relatively brief exposure to sunlight. A typical eyelid margin melanoma with involvement of both the anterior and the posterior lamella of the lower eyelid. Diffuse involvement of the upper palpebral, lower palpebral, and bulbar conjunctiva with invasive melanoma of the eyelid that has extended onto the surface of the globe. The risk of a second primary melanoma in patients who have already been diagnosed with melanoma is greater than the risk of a first melanoma in unaffected individuals in the general population. In patients with melanoma, the lifetime risk of developing a second primary melanoma varies from 3% to 5% according to different series. A heightened awareness and histologic confirmation are key to correct diagnosis of melanocytic lesions of the eyelid, regardless of the degree of pigmentation. Lesions that grow rapidly and double in size within days are more likely to be inflammatory conditions such as chalazion or pyogenic granuloma than melanoma. Malignant pigmented lesions can be clinically distinguished from benign pigmented lesions because malignant lesions exhibit disorganized and chaotic pigment and color patterns whereas benign lesions tend to have order and symmetry in their coloration, regular borders, and uniform surface characteristics. Benign lesions that are occasionally confused with melanoma include seborrheic keratosis, compound nevus of Spitz, junctional nevus, lentigo, hemangioma, blue nevus, and tattoo spots. This is particularly true in patients whose lesions change in size, color, or shape. A rapidly growing nodular melanoma with a Breslow thickness of at least 12 mm that started on the lower eyelid margin in the skin parallel to the lash line and then rapidly grew onto the surface of the globe and diffusely involved the bulbar and palpebral conjunctiva in a period of less than 4 weeks. An amelanotic lesion in the lower eyelid that was initially mistakenly diagnosed as a chalazion and on examination of the final excisional biopsy specimen was discovered to be invasive melanoma. Melanocytic Lesions of the Eyelid and Ocular Adnexa Excisional biopsy is almost always preferred over other biopsy techniques; however, if the lesion is large and involves multiple areas of the conjunctiva or the entire lower eyelid margin, an incisional biopsy of the most worrisome area is a reasonable alternative. Several studies have disproved concerns that incisional biopsy of a melanoma could promote seeding or dissemination of melanoma cells. The biopsy method chosen must yield a specimen that provides information about tumor thickness. For conjunctival melanomas, special care is required in specimen handling and processing of the primary tumor specimen. In addition, most conjunctival melanoma specimens are quite small and thin compared to cutaneous melanoma specimens. These factors together frequently lead to tangential cutting of conjunctival melanoma specimens. Controversy exists regarding the role of frozen sections for determination of tumor thickness and resection margin status for melanoma. At present, the consensus seems to be that frozen-section diagnosis of melanoma is not as accurate as diagnosis made using paraffin-embedded sections. Uniform classification and staging of melanoma are of paramount importance: useful comparisons of treatment regimens and results from different centers can only be made if patient populations are similar with respect to tumor load, distribution of disease, and potential for a poor outcome. Curling-up of the edges of the surgical specimen led to tangential cutting and inability to determine the depth of invasion of the melanoma. The Breslow thickness can be determined accurately and is measured from the epithelial surface to the deepest area of invasion of tumor. From Esmaili B et al: Surgical specimen handling for conjunctival melanoma: implications for tumor thickness determination and sentinel lymph node biopsy. En bloc excision of an invasive melanoma of the eyelid and conjunctiva with involvement of the canaliculi and the palpebral and bulbar conjunctiva. Such specimens are presented to the pathology lab in total and over a drawing of the eye and eyelid to clearly outline the margins of interest and orientation for the pathologist. The goal of surgical treatment is to remove all melanoma cells and thus achieve local control and possibly increase the probability of cure.
The Retina Society Terminology Committee: An updated classification of retinal detachment with proliferation vitreoretinopathy impotence 21 year old purchase discount avanafil line. Hagedorn M erectile dysfunction treatment tablets cheap avanafil uk, Esser P erectile dysfunction diagnosis treatment avanafil 100 mg free shipping, Wiedemann P erectile dysfunction treatment australia order 200mg avanafil overnight delivery, Heimann K: Tenascin and decoverin in epiretinal membranes of proliferative vitreoretinopathy and proliferative diabetic retinopathy erectile dysfunction drugs south africa order avanafil 100 mg otc. Grisanti S, Heimann K, Wiedemann P: Origin of fibronectin in epiretinal membranes of proliferative vitreoretinopathy and proliferative diabetic retinopathy. Esser P, Heimann K, Wiedemann P: Macrophages in proliferative vitreoretinopathy and proliferative diabetic retinopathy: differentiation of subpopulation. Ashton N, Henkind P: Experimental occlusion of retinal arterioles (graded glass ballotini). Nakissa H, Rubin P, Strohl R, Keys H: Ocular and orbital complications following radiation therapy of paranasal sinus malignancies and review of literature. Garner A, Ashton N, Tripathi R, et al: Pathogenesis of hypertensive retinopathy: an experimental study in the monkey. Uyama M: Histopathological study of vesicular changes especially on involvements in the choroidal vessels in hypertensive retinopathy. Patz A: Retinal neovascularisation: early contributions of Professor Michaelson and recent observations. Faulborn J, Bowland S: Microproliferations in diabetic retinopathy and their relation to the vitreous: corresponding light and electron microscopic studies. Baird A, Esch F, Gospodarowicz D, Fuillemin R: Retina- and eye-derived endothelial cell growth factors: partial molecular characterization and identity with acidic and basic fibroblast growth factors. Smith L, Kopchick J, Chen W, et al: Essential role of growth hormone in ischemia induced retinal neovascularization. Review of the literature, diagnostic criteria, clinical findings and plasma lipid studies. Baudouin C, Fredj-Reygrobellet D, Lapalus P, Gastaud P: Immunohistopathologic finding in proliferative diabetic retinopathy. Report of the committee to investigate and revise the classification of certain retinal conditions. Kremer I, Hartmann B, Haviv D, et al: Immunohistochemical diagnosis of a totally necrotic retinoblasatoma: a clinicopathological case. Matsuo N, Takayama T: Electron microscopic observations of visual cells in a case of retinoblastoma. Ikui H, Tominaya Y, Konomi I, Ueono K: Electron microscopic studies on the histogenesis of retinoblastoma. Sasaki A, Ogawa A, Nakazato Y, Ishido Y: Distribution of neurofilament protein and neuron-specific enolase in peripheral neuronal tumors. Kivela T: Neuron-specific enolase in retinoblastoma: an immunohistochemical study. Virtanen I, Kivela T, Bugnoli M, et al: Expression of intermediate filaments and synaptophysin show neuronal properties and lack of glial characteristics in Y79 retinoblastoma cells. Vrabec T, Arbizo V, Adamus G, et al: Rod cell-specific antigens in retinoblastoma. He W, Hashimoto H, Tsuneyoshi M, et al: A reassessment of histological classification and an immunohistochemical study of 88 retinoblastomas. Lemieux N, Leung T, Michaud J, et al: Neuronal and photoreceptor differentiation of retinoblastoma in culture. Harris N, Jaffe E, Stern H, et al: A revised European-American classification of lymphoid neoplasm: a proposal from the International Lymphoma Study Group. Cravioto H: Human and experimental reticulum cell sarcoma (microglia of the nervous system). Corriveau C, Esterbrook M, Payne D: Lymphoma simulating uveitis (masquerade syndrome). Wagenmann D: Ein Fall von multiplier Melanosarkomen mit eigenartigen Komplikationen beider Augen. They may play a role in keeping the intertrabecular spaces free of potentially obstructive debris. Many factors are believed to cause reduced cell density but the exact etiology remains unknown. Intraocular pressure depends on rate of aqueous humor production and the resistance to its outflow. From the inner to the outermost part, the layer of tissue closest to the anterior chamber is the uveal meshwork followed by corneoscleral meshwork and juxtacanalicular region. Ultrastructurally, the uveal and corneoscleral regions consist of a single layer of trabecular cells, a subcellular basal lamina, and a central connective tissue core. A second unconventional pressure-independent aqueous outflow pathway is the uveoscleral pathway. The changes are variable and include generalized or focal loss of the neuroretinal rim. Other disk changes include peripapillary atrophy, nerve fiber layer hemorrhage, arterial narrowing, and acquired optic nerve pits. The biochemical factors involved in the optic nerve changes are complex and likely multifactorial. Tissue ischemia due to elevated intraocular pressure along with genetic and immunologic factors may play a role in susceptibility of the optic nerve and retinal ganglion cells. This promotes degradation of extracellular matrix, which may cause degenerative changes in the optic disk and progression of neuronal damage. This response leads to enhanced expression of proteolytic enzymes such as matrix metalloproteinases that might contribute to the development and progression of optic- disk cupping. A new view of human trabecular meshwork using quick-freeze, deep-etch electron microscopy. The hallmark of retinal ganglion cell degeneration is apoptosis or programmed cell death. Factors promoting apoptosis in glaucoma include tissue ischemia, tissue necrosis factor alpha, nitric oxide, serum autoantibodies, hypoxia-inducible factor1a, p53 activation, mutation in the optineurin gene, and heat-shock protein. This decreases the ability of endogenous heat-shock protein to stabilize actin cytoskeleton, thereby facilitating apoptosis of retinal ganglion cells or glial cells. Glaucomatous cupping of the optic disk with loss of retinal nerve fiber layer (arrowheads). This adversely effects the compliance and resiliency of the lamina cribrosa and its ability to adapt to changes in intraocular pressure. The cornea may undergo endothelial decompensation, and develop chronic edema and secondary changes: bullous keratopathy, band keratopathy, degenerative pannus formation, and corneal scarring. The iris stroma becomes atrophic and fibrotic and may show degeneration of the pupillary margin. Choroidal atrophy is found in the peripapillary area, where changes in the retinal pigment epithelium also occur. Stretching of the corneoscleral tissue may also occur, particularly in young eyes with relatively immature collagen. In infants, this may involve the entire globe to produce buphthalmos, whereas in adults localized staphylomas result, principally in proximity to sites of neural and vascular penetration where the sclera is weakest. Patchy loss of subcapsular lens epithelium (arrow) with intact peripheral lens epithelium (arrowhead) and underlying changes in the lens cortex fibers. Pathogenesis the rise of intraocular pressure in primary open-angle glaucoma is probably caused by increase in resistance to aqueous outflow through the trabecular meshwork. Some changes in the extracellular matrix of the trabecular meshwork as described ahead may result in the increased resistance to outflow. Modifications in glycoprotein composition and distribution may, because of their hydrophilic properties, contribute significantly to an increase in outflow resistance. Loss of protein function may decrease the threshold for retinal ganglion cell apoptosis. This may explain retinal ganglion cell death via apoptosis when intraocular pressure is not elevated. This association suggests that normal-tension glaucoma may, in some instances, be a hereditary optic neuropathy with a pathophysiology based in mitochondrial dysfunction. Recent studies have shown that patients with normal-tension glaucoma had significantly lower diastolic blood pressure at night and a significantly greater mean decrease in diastolic blood pressure at night than patient with anterior ischemic optic neuropathy. Enlargement of the trabecular cells and thickening and fusion of the lamellae can result in complete obstruction of the uveal and corneoscleral aqueous pathways. The mechanisms by which myocilin mutations result in glaucoma remain unclear but overexpression can influence adhesion, spreading, migration, phagocytosis, and apoptosis of human trabecular meshwork cells and can render them in a de-adhesive and vulnerable state. It is more frequent in hyperopic eyes in which the size of the lens and the anterior chamber are disproportionate. However, it is also suggested that there are dynamic, physiological differences between primary angle-closure eyes and eyes with the same anatomic measurement at baseline. Greater iris contact with the anterior lens capsule increases resistance to the passage of aqueous humor through the pupil (relative pupillary block). The likelihood of pupillary block-related angle-closure occurring is greatest when the pupil is in mid-dilated position. The histopathologic changes in angle-closure glaucoma are the result of a rapid and marked elevation of intraocular pressure. The changes include ischemic necrosis of the dilator and sphincter muscles leading to irregularities in pupillary shape. Multiple, small, subcapsular, anterior white lens opacities may be observed (glaukomflecken), corresponding to foci of epithelial cell necrosis with adjacent areas of subcapsular cortical degeneration. Other changes observed are corneal edema, optic disk edema, and central retinal vein occlusion. Secondary congenital glaucoma may be present at birth owing to intrauterine insult. It can occur as an isolated condition (trabeculodysgenesis) or can be associated with other systemic. Genes responsible for development defects of ocular anterior segment are located on chromosome 13q14, 4p, 16q, and 20p. Two chromosomal regions that are likely to contain the gene for pigment dispersion have been identified as 7q36 and 18q22. Note anterior insertion of iris root and ciliary body (arrowhead), poorly delineated trabecular beams (arrow) and poorly developed scleral spur (double arrows). These materials include melanin pigment, lens proteins, pseudoexfoliative material, inflammatory cells, red blood cells, and ghost cells. Secondary angle-closure glaucoma may be caused by a variety of conditions that result in apposition of the peripheral iris to angle structures, often with the formation of peripheral anterior synechiae. The angle remains open anatomically and no peripheral anterior synechiae are present. Pigmentary Glaucoma this is a type of open-angle glaucoma associated with pigment deposition in anterior and posterior segment of eye. The iris assumes a concave configuration in eyes predisposed to pigmentary glaucoma. Pigment deposition results in an exaggerated phagocytic response of the trabecular endothelial cells. The endothelial cells degenerate, migrating off the trabecular beams, causing regional trabecular collapse and loss of intratrabecular spaces adjacent to the juxtacanalicular region. Upregulated genes include myocilin, decorin, insulin-like growth factor binding protein 2, ferritin L chain, fibulin 1-c while downregulated genes include nitric oxide synthase gene and the chloride channel gene. All these factors likely contribute to development of increased intraocular pressure following steroid use. Lens Particle Glaucoma Following surgery or trauma to lens, large lens pieces spontaneously fragment into small particles that eventually migrate to the anterior chamber and initiate a macrophagedriven inflammatory reaction. This eventually obstructs aqueous outflow by accumulation of lens debris and inflammatory components in the trabecular meshwork. These ghost cells contain intracellular globules consisting of denatured hemoglobin adherent to the cell membrane (Heinz bodies). They can then circulate forward into the anterior chamber after disruption of the anterior hyaloid surface, such as occurs after accidental trauma, cataract extraction, or vitrectomy. Traumatic Glaucoma Ocular trauma may cause mechanical obstruction of the trabecular meshwork by accumulation of erythrocytes, inflammatory cells, and blood products. The latter pathologic change correlates with the gonioscopic findings of a widened ciliary body band and posteriorly displaced iris. The recession is a marker for more subtle damage that occurs over time, resulting in scarring and other changes in the trabecular meshwork without obvious peripheral anterior synechiae that culminate in outflow obstruction. Hemolytic Glaucoma After a large intraocular hemorrhage, fragments of hemolyzed red blood cells, red blood cell debris, free hemoglobin, and hemoglobin-laden macrophages may cause obstruction of trabecular meshwork resulting in increased resistance to aqueous outflow. Sickle cell anemia patients have abnormal sickle-shaped red blood cells due to polymerization of the abnormal hemoglobin-S. This abnormal hemoglobin is also present in smaller amounts in red blood cells in individuals with sickle trait, and sickling can occur in these individuals if the red blood cells are exposed to abnormal metabolic conditions such as hypoxia or metabolic acidosis. If these conditions occur in the anterior chamber, the red blood cells assume a sickle Steroid induced Glaucoma Glucocorticoids increase intraocular pressure by several mechanisms. Phacolytic Glaucoma this is a lens-induced open-angle glaucoma in which a mature or hypermature cataract leaks its soluble proteins into the anterior chamber while the lens capsule is macroscopically intact. A macrophage response to lens protein in the anterior chamber coupled with high molecular weight lens protein results in blockage of the trabecular meshwork causing outflow obstruction. It is suggested that exfoliation syndrome may be a stress-induced elastosis or elastic microfibrillopathy. In addition, tumor cells floating from the iris or posterior segments may obstruct the trabecular meshwork.
Some of these benign conditions are considerably more common than the malignant neoplasms affecting the uvea erectile dysfunction pills nz purchase avanafil 50mg without a prescription. Assessment of the degree of pigmentation plays an important role in the clinical and pathologic formulation of a differential diagnosis and in the classification of uveal tumors impotence pregnancy generic 200 mg avanafil. The absence of melanin in a lesion protocol for erectile dysfunction order discount avanafil online, however can erectile dysfunction cause low sperm count 50 mg avanafil with mastercard, does not totally exclude the diagnosis of malignant melanoma impotence definition inability generic avanafil 200mg line. Melanocytic proliferations are the most common primary intraocular neoplasms, including both nevi and malignant melanomas. A variety of histopathologic features are correlated with prognosis for survival in ciliochoroidal melanoma. These include cell type, size, extrascleral tumor extension, and intrinsic microvascular patterns. Medulloepithelioma is a tumor derived from the ciliary neuroepithelium that typically affects children. Other benign and malignant neoplasms may arise from the ciliary epithelium and are rare. Choroidal osteoma is a bony, choristomatous lesion of the peripapillary choroid that typically occurs in young women. Leiomyoma is a benign neoplasm of smooth muscle origin that can occur rarely in the ciliary body and may be mimic amelanotic melanoma. However, metastatic Pathology of the Uveal Tract such a diagnosis, because melanin is present in both benign melanocytic nevi and neuroepithelial cell neoplasms. Another consideration affecting the classification of uveal neoplasms is information gleaned from embryologic studies of the cells from which tumors are ultimately derived. For example, during embryologic development, two groups of melaninproducing cells become established in the uveal tract249: 1. Pigmented epithelial cells of the iris, ciliary body, and retina, which are derived from the neuroepithelium of the optic cup. Uveal melanocytes, which probably migrate from their site of origin in the neural crest into the uveal stroma. The stroma is mesectodermal, despite a probable origin in the cranial neural crest. Pigmented neuroepithelial cells of the iris and ciliary body have relatively large melanosomes, but these cells have a limited ability to undergo neoplastic growth. Uveal melanocytes, however, have much smaller and finer melanosomes and have a much greater potential for proliferation, forming both nevi and malignant melanomas (note that here we use the term nevus to denote a benign melanocytic neoplasm, in preference to the term benign melanoma, which we believe should be discarded because the term melanoma is frequently used as a synonym for malignant melanoma). Knowledge of the developmental and behavioral differences between the neuroepithelial cells and melanocytes allows uveal tumors to be classified broadly into the groups seen in Table 271. However, the behavior of specific neoplasms within this classification may vary according to the precise site of the lesion within the uveal tract. Thus, cells from iris nevi may migrate over the surface of the iris in a way not seen in nevi in the ciliary body or the choroid, and the behavior of malignant melanoma of the iris also differs significantly from that of the same tumor in the posterior uvea, as is discussed later. The overall incidence of uveal nevi is high, but it varies considerably in the several clinical and pathologic studies,244 the latter giving rise to figures such as 8. Plump polyhedral cells (the most common cell type), with abundant melanin granules, a small round or oval nucleus, and an inconspicuous nucleolus. If the nevus consists almost entirely of these cells, it is termed a melanocytoma (further ahead). Slender spindle cells (the second most common cell type), with little or no pigment and a slender, very basophilic nucleus. Plump fusiform and dendritic cells (intermediate between plump polyhedral and slender spindle cells), with moderate pigmentation, a slightly larger nucleus, and occasionally a small nucleolus. Balloon cells, which are large, amelanotic, and polyhedral with distended finely vacuolated cytoplasm. Compared with malignant melanomas, most small choroidal and ciliary body nevi have minimal effects on adjacent tissues. Yanoff and Zimmerman263 suggested that most malignant melanomas of the choroid and ciliary body arise in preexisting nevi, as they demonstrated that 73 of 100 consecutive malignant melanomas had nevus cells within or along their edges. It is not clear, however, whether individual nevus cells are intrinsically more likely to undergo malignant transformation than are isolated stromal melanocytes, or whether malignant melanomas are more likely to develop in nevi merely as a function of increased melanocyte numbers and density in these lesions. In a single study, RodriguezSains264 reported that patients with the dysplastic nevus syndrome have an increased incidence of uveal nevi. Melanocytoma is a rare heavily pigmented lesion, which is clinically important because in the past, it was frequently misdiagnosed as malignant melanoma and was treated inappropriately by enucleation. Melanocytoma is the most common primary neoplasm of the optic nerve head, where it was originally diagnosed, but it is also seen throughout the uveal tract, including in the ciliary body and iris and occasionally in the choroid. In contrast to malignant melanoma, optic disk melanocytomas are more common in heavily pigmented races than in whites, although 80% of ciliary body melanocytomas occur in whites. Macroscopically, melanocytomas are composed of plump polyhedral nevus cells, with cytoplasm distended by heavily pigmented melanosomes. Melanin bleach preparations to confirm that cell nuclei are small and round, without nucleoli or mitotic figures. Ciliary body and iris melanocytomas often undergo spontaneous necrosis, and this may cause seeding into the anterior chamber angle and secondary open-angle melanomalytic glaucoma. In rare cases, malignant melanomas have arisen in uveal and optic nerve head melanocytomas. These conditions are caused by a failure of migration of melanocytes to their normal resting position in the surface epithelium. Oculodermal melanocytosis, affecting the eyelid skin and episclera (a), with (b) diffuse choroidal pigmentation. Pathology of the Uveal Tract the pigmentary change is confined to the sclera and episclera without involvement of the skin, the term ocular melanosis is used. Clinically, this condition gives rise to slate gray or bluish appearance of the sclera, as opposed to the dusty brown appearance of primary acquired melanosis or racial melanosis. The pigment within the sclera has the distinctive feature of outlining the blood vessels. The diffuse involvement of the uveal tract can give rise to iris heterochromia and a darker appearance to the fundus on the affected side. Gonder and associates284 estimated the prevalence of ocular melanocytosis to be 0. In the same study, the prevalence of oculodermal melanocytosis in black patients (6915 patients examined) was found to be 0. The prevalence of ocular melanocytosis in the Asian population is higher, with a reported prevalence between 0. Two studies have calculated ocular melanocytosis to be 30 to 35 times more common in patients with uveal melanoma. Uveal malignant melanoma is rare in black patients: it occurs in 1% of African Americans301 and possibly even less in African black persons. Although the nevus of Ota is more common in black and Asian persons than in whites, progression to malignant melanoma occurs in both races, but it is more common in affected white than in affected black persons. It appears that individual members of these families have a low absolute risk of developing tumors, even though this risk is considerably higher than for individuals in the general population. However, no specific genetic defects have been found in most patients with uveal malignant melanoma. Specific nonrandom chromosomal abnormalities are common in uveal and, in particular, ciliary body malignant melanomas. The association between uveal malignant melanoma and preexisting uveal nevi, melanocytosis, and dysplastic nevus syndrome was discussed earlier. Although the rate of death from other cancers appears to be high, the risk of developing these tumors is no higher than in the general aging (and age-matched) population in which most uveal malignant melanomas occur. Malignant Neoplasms Posterior uveal (choroidal and ciliary body) malignant melanoma the term uveal malignant melanoma is recommended by the World Health Organization289 and the Armed Forces Institute of Pathology to name the malignant neoplasm arising from uveal tract melanocytes. Ideally, the term melanoma should not be used alone (without the qualifier malignant), because some pathologists continue to use melanoma incorrectly to include both benign and malignant neoplasms. Congenital uveal malignant melanoma is known but extremely rare,294,295 and Shields and colleagues296 reported that only 1. The incidence of uveal malignant melanoma was higher in men (55%) than in women (45%) in 4995 patients in the Armed Forces Institute of Pathology Registry of Ophthalmic Pathology in the United States in 1994,245 and a predominance Clinical features the clinical features of uveal malignant melanoma depend on the site and the stage of the tumor. Malignant melanomas of the iris are easily visible and are usually detected when they are small. Asymptomatic, discovered incidentally on routine eye examinations; small tumors confined to the uvea, with possible small scotoma associated with degeneration of overlying retina Stage 2. Progressive blurring and loss of vision resulting from retinal degeneration and detachment Stage 3. Ocular pain due to associated glaucoma (pupillary block, rubeosis, or angle invasion) or inflammation Stage 4. Effects of extraocular extension, such as subconjunctival mass and proptosis Between 1936 and 1975, the Registry of Ophthalmic Pathology at the Armed Forces Institute of Pathology recorded 2627 cases of uveal malignant melanoma: 3% presented at clinical stage 1, 64% at stage 2, 32% at stage 3, and 1% at stage 4. This finding suggests that the process of metastasis occurs relatively early in the natural history of the disease. As the tumor enlarges, the overlying retina undergoes atrophic or cystoid degenerative changes, with progressively more extensive exudative retinal detachment. Large, nodular tumors may eventually invade and destroy adjacent intraocular tissues, filling the posterior chamber. Subsequent enlargement may displace the iris and lens anteriorly, causing progressive narrowing of the anterior chamber angle and eventual obliteration of the anterior chamber. Scleral invasion is more common in the diffuse than in more nodular tumors,244 and they tend to cause disproportionately large orbital tumor deposits. They commonly invade the iris root and the drainage structures of the anterior chamber. Displacement of the lens, lenticular notch, and cataract formation are also possible consequences of ciliary body malignant melanomas. Diffuse infiltrating malignant melanoma also occurs in the ciliary body, where it may produce a circumferential ring growth pattern. Disproportionate extraocular spread is a common consequence of this type of malignant melanoma and it has a poor ocular and systemic prognosis. Histologically (c) there is perivascular and intravascular (vortex vein) invasion. Diffuse infiltrating malignant melanoma (a) is flat, with extensive subretinal extension. This tumor (b) is less than 2 mm thick and is highly pigmented, with amelanotic areas. This ciliary body malignant melanoma has a rounded profile and invades the iris (center) and anterior chamber angle (bottom left) (cornea left). Tumor-induced scleral necrosis or surgically induced defects or weakness may also allow extraocular tumor invasion. Most uveal malignant melanomas with extraocular extension are large, but small and diffuse malignant melanomas may have disproportionately large extraocular tumor components. The relatively low frequency of observed intravascular tumor invasion of vortex veins probably indicates that invasion of small intratumoral blood vessels is the most important source of hematogenous metastasis. Peripapillary choroidal malignant melanomas often invade the optic nerve head, but retrolaminar invasion of the optic nerve is rare, unlike retinoblastoma. Uveal melanoma may, therefore, present as a blind, painful eye, with glaucoma or with a prominent inflammatory reaction. Microscopic findings the most important microscopic feature of posterior uveal malignant melanomas is the morphology of the tumor cells, and this remains one of the most reliable indicators of prognosis for individual tumors. Spindle A cells: fusiform (spindle-shaped) cells, with a slender nucleus, often with a longitudinal fold; fine chromatin and indistinct nucleolus. Spindle B cells: fusiform cells with relatively plump, ovoid nuclei, coarser chromatin and more prominent, often eosinophilic nucleolus. Epithelioid cells: larger, more rounded or polyhedral cells with abundant cytoplasm, and distinct cell border resulting from loss of cohesion with adjacent cells. Nuclei are large and more angular, with coarse and marginated cytoplasm and extremely large eosinophilic nucleoli. Callender 321 classified tumors into six groups, based on the aforementioned three cellular subtypes and two further histologic features. Fascicular (with nuclei arranged in parallel around blood vessels or in stripes across the tumor) 4. Wilder and Paul322 found that tumors fell into two broad prognostic groups of relatively good and poor prognosis. The remaining spindle A-type and B-type tumors had a similar prognosis, and they are now combined into a single spindle-cell category. Disagreement exists about the proportion of spindle cells allowed in an epithelioid tumor (most have at least some spindle cells), and in practice, all uveal malignant melanomas containing epithelioid cells are designated as mixed cell neoplasms at the Armed Forces Institute of Pathology. Immunostaining for these antigens can be used to distinguish them from other cell types. The incidence of iris nevi is unclear, but they are reported to be more common in light-skinned individuals than in black persons,336 and Albert and associates337 found iris and choroidal nevi to be more common in patients with cutaneous malignant melanomas than in control patients. There is no conclusive association between iris nevi and posterior uveal malignant melanoma. Nevus cells may therefore extend into and beyond the trabecular meshwork, causing glaucoma,338 although this behavior is seen more commonly in malignant melanoma. Iris nevi contain intranuclear cytoplasmic invaginations (nuclear pseudoinclusions), which are rare in choroidal and ciliary body nevi. Iris nevi may include multinucleated epithelioid nevus cells not seen elsewhere in the uvea.
Abnormalities in this category may include lid malposition or atony erectile dysfunction at 30 purchase avanafil 50 mg, punctual stenosis or malposition erectile dysfunction after radiation treatment prostate cancer purchase 200mg avanafil otc, canalicular stenosis erectile dysfunction causes cycling purchase avanafil 200 mg otc, and nasolacrimal duct obstruction erectile dysfunction treatment centers purchase avanafil 200mg line. As with all chief complaints erectile dysfunction drugs in canada avanafil 100mg sale, details of the quality, quantity, aggravating and alleviating factors, and associated symptoms should be ascertained. Ascertaining whether the problem is unilateral or bilateral and under what conditions the tearing occurs or worsens may provide insight into the cause. Although there are exceptions, unilateral, constant tearing suggests insufficient lacrimal outflow, while intermittent bilateral tearing that is worse in cold or wind suggests tear film instability and/or aqueous deficiency with secondary reflex tearing. A history of tearing since childhood raises the possibility of untreated congenital nasolacrimal duct obstruction. A history of seasonal allergies is often present in this situation, but environmental exposures should also be considered. It should be noted that allergic rhinitis can also result in epiphora, presumably due to obstruction of the outflow pathway resulting from edema of the nasal mucosa. Patients with dacryolithiasis tend to be younger than those with primary acquired nasolacrimal duct stenosis and usually have intermittent rather than constant tearing. Pain within the eye itself can cause tearing, so trichiasis, corneal abrasions or foreign bodies, and intraocular inflammation must always be considered. While careful attention must be given to this possibility, investigation may not result in an identifiable cause. The patient should be asked about systemic diseases, particularly immunologic disorders including arthritis and thyroid disease, which may be associated with corneal problems that are manifested by tearing such as dry-eye syndrome, lagophthalmos, and superior limbic keratitis. Systemic inflammatory disorders such as sarcoid, Wegeners and certain neoplasms such as lymphoma can involve lacrimal drainage system and result in epiphora. In most cases the systemic lymphoproliferative disorder will be known about prior to developing epiphora due to infiltration of the lacrimal drainage pathways. A history of systemic malignancies should also be documented, as certain chemotherapeutic agents may impede lacrimal drainage outflow (see further ahead). Treatment with radioactive iodine (I131) for thyroid carcinoma may result in epiphora by causing stenosis within the nasolacrimal duct, common canaliculus, and/or distal canaliculus. Additionally, canalicular lacerations not recognized or repaired can result in epiphora. However, several deserve particular attention due to their common use and the clear between use and risk of tearing. These include topical antivirals, Phospholine iodide, topical Epinephrine-containing compounds, topical or systemic 5Flurouracil, which can cause punctal and/or canalicular obstruction,5,6,7 and Docetaxel (Taxotere). Docetaxel is commonly used in treating breast cancer and can result in epiphora by causing canalicular stenosis. Finally, the history would be incomplete without determining how bothersome the symptoms are to the patient. Does the eye feel wet, or does the patient need to wipe their cheek as the tears spill on to it It is important to realize that patients with very similar objective findings often vary significantly in terms of how bothered they are. Defining the burden to the patient is essential in determining their motivation to proceed with treatment. Of course, those patients with nasolacrimal duct obstruction should be warned of the risk of dacryocystitis. We have found that for some patients, this information motivates them to want to reduce the risk of infection and proceed with surgery even when their symptoms of tearing are mild. While certainly valuable, this technique should be only one step in a comprehensive evaluation. In order for tears to leave the ocular surface via the lacrimal drainage pathway, the lids must be in normal position and have adequate tone. In terms of position, the lids should be wellapposed to the ocular surface and have proper orientation. This is essential both to keep punctum well positioned in relation to the tear lake and to ensure that lashes do not contact the eye surface. The patient should also be examined with their glasses on, as glasses may induce lower lid ectropion. When it is lower, lateral canthal 3498 Evaluation of the Tearing Patient minimizing contact between the speculum and septum to minimize patient discomfort. Examination should note the presence of masses, mucosal inflammation, hypertrophic turbinates, and adhesions between septum and the lateral wall of the nose. Nasal examination is also essential for surgical planning if Jones tube placement is considered to determine if adequate space exists to allow for the presence of the tube within the nose. It is particularly useful in assessing the size and position of the ostium after dacryocystorhinostomy. Slit-lamp examination is an essential component in the evaluation of the tearing patient. Presence of debris or exudate in the tear film and tear breakup time should be determined. Rapid tear breakup indicates tear film inadequacy and is usually seen in the setting of blepharitis. Some patients with a complaint of tearing have an obviously elevated tear lake, while for other, this elevation may be subtle. The puncta should be evaluated for size, position in relation to the tear lake, apparent patency, presence of discharge, and evidence of swelling. It usually affects the proximal lacrimal outflow pathway and may be associated with other developmental disorders, although the majority of cases are usually isolated. On occasion an enlarged caruncle (megalocaruncle) can cause epiphora by occluding the opening to the punctum or by displacing the punctum away from globe. The forniceal and palpebral conjunctiva should be inspected for follicles and papillae of reactive inflammatory disorders and allergic conjunctivitis. Conjunctivochalasis is a condition of unknown etiology in which redundant conjunctiva may drape over and cover the punctum, preventing tear outflow. Resection of excess conjunctiva can be effective in reducing tearing in these patients. Examination of the cornea should be done before the application of drops such as topical anesthetics that might alter the tear film and corneal surface. Finally, subtle abnormalities in the eyelid position (entropion/ectropion), eyelid margin (blepharitis), and eyelash position (trichiasis) can be identified with slit-lamp biomicroscopy. It is not uncommon to find more than one potential cause of tearing and failure to address each may lead to incomplete resolution of symptoms. However, it is often difficult to determine the relative contributions of each to tearing. For example, a patient may have concurrent lid laxity, ectropion, punctal stenosis, and partial nasolacrimal duct stenosis. From top: punctal dilator; Bowman probe, irrigating cannula/syringe; nasal speculum. In this situation, the angle formed by the lower lid may not be favorable for tears to reach the punctum. Loss of lid tone (from aging or seventh nerve dysfunction) or disruption of lid position can alter tear dynamics. Incomplete blinking may result in rapid tear breakup, corneal irritation, and reflex tearing as well as a poor lacrimal pump. Adequate lid tone is also necessary for tears to leave the ocular surface properly. Loss of tone can reduce the efficacy of the lacrimal pump, the process in which the cycle of opening and closing of the lids forces the tears into the canaliculi. Although lower lid laxity is a more common cause of tearing, significant upper lid laxity may also cause tearing, such as is seen in floppy eyelid syndrome. In some patients all lids may have significant laxity, and the most frequent symptom in these patients is epiphora. This is relevant in the tearing patient, as aberrant regeneration of the facial nerve can result is tearing while chewing. Finally, lid retraction and lagophthalmos may increase exposure and tear evaporation, thus leading to reflex tearing. Visible or palpable fullness of the lacrimal sac, erythema of the overlying skin, and/or reflux of mucus or exudate from the lacrimal puntum with palpation of the lacrimal sac suggest dacryocystitis and, therefore, identifies nasolacrimal duct obstruction as present. Tumors of the lacrimal sac and mucoceles may also present as palpable masses in the region of the medial canthus. Unlike dacryocystitis, these entities may extend above the medial canthal tendon and would be less likely to be tender. The external examination should conclude a nasal examination as obstructions with the nose can impede lacrimal drainage. A high-powered light source (such as an indirect ophthalmoloscope) and nasal speculum provide the ability to examine the septum, nasal floor, and turbinates. If history and examination before canalicular irrigation suggest lacrimal obstruction but canalicular irrigation reveals that the lacrimal drainage system is patent, then the patient likely has either functional nasolacrimal duct obstruction or a dacryoliths. Forceful irrigation of saline into the canaliculus may result in reflux from the opposite punctum causing the false impression that an obstruction is present. Likewise, if a partial obstruction is present in the lacrimal drainage pathway, forceful irrigation may be able to overcome the partial blockage and lead the examiner to conclude that no obstruction is present. If reflux occurs from the same punctum (canalicular obstruction) probing should be performed to determine the site of obstruction. If an obstruction is encountered, the probe is grasped with forceps at its entrance to the punctum and then withdrawn. The distance from the forceps to the end of the probe gives the location of the canalicular obstruction. However, proximal or mid-canalicular obstruction typically requires placement of a Jones tube. Reflux from the opposite punctum usually indicates nasolacrimal duct obstruction but it can occur in the setting of common canalicular obstruction. Probing can allow for these to be distinguished as the latter will result in a distal soft stop to passage of the probe. Probing the nasolacrimal duct is painful and has no value in adults as either a diagnostic test or a therapeutic modality. The Jones tests can assist with determining whether lacrimal drainage outflow problem is anatomic (blockage) or functional (reduced outflow in the absence of blockage). The primary dye test involves placing fluorescein dye into the conjunctival culde-sac. After 5 min, the presence of dye in the inferior meatus is recovered from the nose with a cotton applicator. This requires anesthetizing the inferior turbinate and meatus prior to beginning the test. Lack of recovery of dye from the nose indicates anatomic or functional blockage is present. If fluorescein-stained solution is recovered, the Jones secondary dye test is positive, indicating that fluorescein had entered the lacrimal sac during the Jones primary test. This indicates a functional upper drainage system and an anatomically patent, but a nonfunctional, lower drainage system. Recovery of clear fluid indicates that fluorescein did not enter the lacrimal drainage system during the Jones primary test and indicates a nonfunctional upper system. Application of topical anesthesia prior to performing this test should eliminate reflex tearing due to irritation induced by contact between the filter paper and the ocular surface. After topical anesthesia of the ocular surface, fornices are gently dried and strips of 41 Whatman filter paper are placed in the inferior fornix and the patient instructed to close their eyes gently. It should be emphasized that while patients with severe aqueous deficiency may experiencing tearing due to reflex, findings of a low value on Schirmers testing does not eliminate the possibility of lacrimal drainage obstruction. Two percent fluorescein solution or a fluorescein strip moistened with saline solution or artificial tears is applied to the lower conjunctival cul-de-sac of both eyes. The volume of the tear lake is then noted with a cobalt blue-filtered pen light in small children or at the slit lamp in either children or adults. The patient is instructed not to wipe the eyes with the hand or a tissue and the tear lakes are examined 5 min later at which time the relative volume of the tear lakes is determined and compared. A narrow tear strip several minutes after placing the dye in the tear film suggests adequate lacrimal function, while elevation of the tear lake after 5 min suggests obstruction of lacrimal drainage, although the site of lacrimal drainage obstruction cannot be determined by this test. Probing and irrigation allows for identification of, and differentiation between, canalicular, common canalicular, and nasolacrimal duct obstruction when present. It not only provides information regarding whether an obstruction in the lacrimal drainage system is present, but allows for localization within the outflow tract, permitting the clinician to determine appropriate treatment strategy. The punctum is gently dilated with a punctal dilator by advancing the tip vertically into the punctum with a gentle twisting motion for 2 mm. Severe punctal stenosis observed on the external and slit-lamp biomicroscope examination may preclude dilation. The dilator is then rotated to a horizontal position (consistent with the course of the canaliculus) and the dilator is advanced slightly. Lateral traction should always be applied to the eyelid during this maneuver to reduce the risk of creating a false passage. The dilator is withdrawn and a lacrimal cannulao on a syringe containing saline is advanced into the canaliculus while maintaining lateral traction on the lid. The cannula should advance easily and should be advanced into the mid-to-distal canaliculus. Remaining too proximal in the canaliculus while irrigating may result in reflux during irrigation creating a false impression of obstruction.
A biphasic incidence profile has been reported with peaks in young children and young adults impotence yohimbe generic 50mg avanafil with visa. The diagnosis is based on recognition of the characteristic lesions and histopathologic confirmation erectile dysfunction journals purchase avanafil with amex. Incision with scalpel blade erectile dysfunction vascular causes order avanafil 50 mg free shipping, followed by expression of the viral bead using a chalazion curette erectile dysfunction self injection purchase avanafil 100 mg, is usually curative erectile dysfunction 18 years old buy avanafil with paypal. Recalcitrant and disseminated disease in immunocompromised individuals may require topical and intravenous Cidofovir. Clinical appearance of molluscum contagiosum of the left upper eyelid margin shows a dome-shaped nodule with smooth contour and central umbilication. Vaccinia lesions of the eyelid are seen in various stages of evolution from vesicles to umbilicated pustules. Because of the virtual impossibility of contracting smallpox, the production of smallpox vaccine for general use was discontinued in 1982. Conjunctival disease manifests as follicular or papillary conjunctivitis with occasional ulcerations and membrane or pseudomembrane formation. Punctate, dendritiform, or geographic corneal epithelial keratitis, interstitial keratitis, and corneal ulceration may complicate blepharoconjunctival involvement. Late sequelae include madarosis, scarring and punctual stenosis, symblepharon or corneal scarring. Topical antiviral agents (Trifluridine or Vidarabine) are recommended for prophylaxis after direct ocular contact with the vaccinia vaccine, for treatment of conjunctival or corneal involvement, and can be considered as preventative measure with isolated eyelid involvement. It is most prevalent in the southeastern United States and the Ohio and Mississippi river basins. Primary, but often subclinical, pulmonary infection occurs after inhalation of the conidia. The fungus then spreads hematogenously to involve various organs, but most frequently, skin, bone, and the internal genitalia are involved. Although lid involvement was previously reported to occur in 25% of patients with systemic disease, Bartley73 found eyelid involvement in only 1 of 79 patients (1. The diagnosis is established by microscopic examination of potassium hydroxide-treated preparations of drainage from skin lesions. Hematogenous dissemination occurs in the setting of immune system compromise, and most often spreads to the central nervous system, although the skin, liver, kidneys and lymph nodes can be involved. Less commonly, lesions can present as violaceous papules, vesicles, crusted plaques, or subcutaneous nodules. Confirmation of the clinical diagnosis is based on culture of the organism from skin lesions, cerebrospinal fluid, blood, or urine. Of the available serodiagnostic tests that can indicate the presence of cryptococcal infections, the latex agglutination test is the most valuable. Presents as single or multiple nodules with or without superficial ulceration, or as localized eyelid edema Coccidioidin skin testing valuable in establishing the diagnosis, confirmed when organism is identified on culture or tissue biopsy specimen Treatment consists of oral azoles. Although worldwide in distribution, it is found most often in Central and South America. Three forms occur, the cutaneouslymphatic form, the pulmonary form, and the disseminated form. Cutaneous inoculation usually occurs from a thorn or splinter in a finger or hand. Eyelid involvement is exceedingly rare, although a few isolated cases have been reported. Diagnosis is often established by culture; organisms are relatively scant within the lesions and seropurulent exudates. Invasive aspergillosis is a significant cause of morbidity and mortality in immunocompromised patients. As an opportunistic mycosis in immunocompromised individuals, it is second only to Candida. Infection of the lids is rare, but chronic granulomatous lesions have been reported. The diagnosis is secured by the demonstration of the organism in cultures and smears. Pulmonary involvement, which may be subclinical, occurs during the summer and fall, the dry and dusty months of the year. Eyelid involvement has only been reported with disseminated disease, presenting as single or multiple nodules with or without superficial ulceration, or as localized eyelid edema. These may occur with other ocular manifestations, such as granulomatous conjunctivitis, keratitis, or chorioretinitis. Coccidioidin skin testing and serologic testing (tube precipitin or complement fixation) are valuable in establishing the diagnosis. Oral azoles are the therapy of choice for extrapulmonary, nonmeningeal disseminated disease, including eyelid involvement. For rapidly progressive lesions, or those involving critical sites, intravenous Amphotericin B may be warranted. Immunocompromised patients may require prolonged or potentially lifelong treatment. Primary eyelid infection with Candida is rare; it usually occurs as a secondary infection, with the mouth being the primary site of infection. It is the most common opportunistic fungus occurring in children and debilitated or immunocompromised adults. There is a white, slightly adherent, membranous deposit on a reddened base in the mouth. On the lids, milder cases show scaly, gray or reddish, definitely marginated lesions, whereas in more severe cases, vesicles develop and rupture, leaving oozing areas and small, whitish yellow pustules enclosed by undermined epidermis. Candida appears to play an important role in promoting severe chronic inflammation in such patients. Treatment consists of topical Nystatin, Clotrimazole, or Miconazole and correction of underlying causes, such as control of diabetes mellitus or cessation of the administration of systemic corticosteroids. Patients with chronic mucocutaneous or disseminated disease should receive intravenous Amphotericin B with or without oral Flucytosine. Cutaneous sinus tracts can form as a result of abscess drainage Positive Mantoux reaction with prior exposure or infection. Presumptive diagnosis with identification of acid-fast bacilli on tissue or exudates. Clinical suspicion is largely based on appearance of the lesion, positive Mantoux reaction, and failure to respond to antibiotics. Definitive diagnosis is based on positive culture results, which unfortunately can be time-consuming. Presumptive diagnosis can be made based on the findings of acid-fast bacilli on tissue or exudates specimens; however, false-negative results are common. The American Thoracic Society recommendations for treatment consists of 2 months of Isoniazid, Rifampin, and Pyramidazine, followed by a 4-month course of Isoniazid and Rifampin. However, for ocular and ocular adnexal disease, serial cultures are not feasible, and treatment response should be surveyed by clinical exams. Atypical mycobacteria are widespread in soil; animal and human feces; house dust; vegetation; and water in lakes, rivers, and swimming pools. Treatment is guided by antimicrobial susceptibility testing of the mycobacterial isolate. Large doses of Erythromycin, Doxycycline, Amikacin, or Sulfamethizole have appeared helpful in isolated cases. Cicatricial and paralytic eyelid changes can lead to lagophthalmos and corneal scarring Treat with Dapsone, Rifampin, and Clofazimine. The diagnosis of leprosy is based on clinical findings of characteristic cutaneous lesions, thickening of peripheral nerves, and hypesthesia. Four variants of the disease are recognized: indeterminate, tuberculoid, borderline, and lepromatous. The robust cellular response limits the disease with discrete, well-defined granulomas. Lepromatous leprosy is characterized by absence of cellular immunity which allows uncontrolled proliferation and dissemination of the bacilli. The clinical manifestations include a symmetric disseminated cutaneous macules, papules, and nodules with progressive thickening of the skin. Involvement of the cutaneous adnexa and dermal nerves results in alopecia and sensory loss, respectfully. Individuals with borderline leprosy have labile cellular immunity to Mycobacterium leprae with clinical features intermediate to tuberculoid and lepromatous variants, and may change to either form depending on the immune status. The indeterminate type is the earliest manifestation of leprosy and presents as a single slightly hypopigmented macule. Madarosis and loss of eyebrow cilia is the most common finding of the ocular adnexa, occluding in as many as 25% of cases with ocular involvement. Lagophthalmos, trichiasis, ectropion, and entropion occur less commonly, but may be more ominous as individuals are predisposed to corneal anesthesia. In both tuberculoid and lepromatous leprosy, involvement of the eyelid gives rise to a number of secondary changes. Common findings include loss of eyebrows and eyelashes, misdirected lashes, lagophthalmos and exposure keratitis, paralytic ectropion with secondary punctal eversion, and reduction of the blinking rate. Because primary and secondary resistance to Dapsone has been increasing, multiple-drug therapy has been recommended. For combined chemotherapy, Dapsone, Rifampin, and Clofazimine should be prescribed. Adjunctive measures to treat all contacts and delouse personal affects are needed the crab louse, Phthirus pubis, is usually found in the hairs of the genital region; however, infestation of the axilla, beard, eyebrows, and eyelashes may occur. Transmission is by direct contact with infested individuals and occasionally by contact with infested personal articles. Children may be infested through close personal contact such as sleeping with an infested parent. Lid hygiene scrubs were found to reduce the density of mites, but not eradicate them. That several studies have shown a statistically significant increase in Demodex in rosacea suggests that the organism may play a role in its pathogenesis. Diagnosis is suggested by the clinical findings of a semitransparent, almost plastic, thin, tubelike crusting of the skin around the lashes. Preauricular lymphadenopathy and secondary infection at the site of the lice bites may occur. A thick occlusive application of ophthalmic ointment smothers the ectoparasite but does not kill the nits. The application of 1% benzene hexachloride is effective but may cause ocular irritation, and reapplication in 5 to 6 days is necessary to eliminate the newly hatched nits. Physostigmine eye ointment, although often recommended, causes miosis and ciliary spasm and is ineffective against the nits. The application of a smothering coat of antibiotic or physostigmine ointment would have to be continued for up to 14 days to kill the lice emerging from the eggs. Disinfection can be accomplished by machine washing in hot water and drying using the hot cycle of the dryer or by dry cleaning. Any other affected body areas should be treated with permethrin (1%) cream (Nix) or lindane 1% shampoo (benzene hexachloride). Patients should be reevaluated after 1 week; retreatment may be necessary if lice or eggs are found. In the United States, conjunctival-external myiasis is usually caused by the cattle botfly (Hypoderma bovis). Myiasis of the eyelid has been reported as result of infestation with Cuterebra larva120 and Dermatobia hominis. A cilium (long arrow) is broken off flush with the skin surface adjacent to the nodule. The diagnosis is established by demonstrating the organisms in fluid aspirated from the ulcer bed128 or by finding the organisms in stained slit-skin smears taken from nonulcerated parts of the lesion. There are many modes of therapy, but generally, the treatment of choice in the United States is systemic sodium stibogluconate (Pentostam); however, this agent has been associated with a number of side effects, including nausea, vomiting, skin rashes, elevated liver enzyme levels, nephropathy, and cardiac arrhythmias.
Discount 200mg avanafil mastercard. Herbal Ayurvedic Sex Medicines Manufacturers India.
References
- Klutke C, Siegel S, Carlin B, et al: Urinary retention after tension-free vaginal tape procedure: incidence and treatment, Urology 58:697n701, 2001.
- Wipff J, Kahan A, Hachulla E, et al. Association between an endoglin gene polymorphism and systemic sclerosis-related pulmonary arterial hypertension. Rheumatology (Oxford) 2007;46(4):622-5.
- McNamara MJ, Pierce WE, Crawford YE, et al. Patterns of adenovirus infection in respiratory diseases of naval recruits. A longitudinal study of two companies of naval recruits. Am Rev Respir Dis. 1962;86:485-494.
- Robertson CS, Hannay HJ, Yamal, JM, et al. Effect of erythropoietin and transfusion threshold on neurological recovery after traumatic brain injury. A randomized clinical trial. JAMA. 2014;312(1):36-47.
- Acebal-Bianco F, Vuylsteke PL, Mommaerts MY, De Clercq CA. Perioperative complications in corrective facial orthopedic surgery: a 5-year retrospective study. J Oral Maxillofac Surg 2000;58:754.
- Tsukasaki K, Tsushima H, Yamamura M, et al. Integration patterns of HTLV-I provirus in relation to the clinical course of ATL: frequent clonal change at crisis from indolent disease. Blood 1997;89(3):948-956.
- Thalassemia. Care and Control in the New Millennium. VP Choudhry and JS Arora (Eds) Novortes publications 2000.
- Gustgavsson S, Wesling A: Laparoscopic adjustable gastric banding: Complications and side effects responsible for the poor long-term outcomes. Semin Laparosc Surg 9:115, 2002.