Ada Hamosh, M.D., M.P.H.
- Dr. Frank V. Sutland Professor of Pediatric Genetics
- Professor of Genetic Medicine

https://www.hopkinsmedicine.org/profiles/results/directory/profile/0002818/ada-hamosh
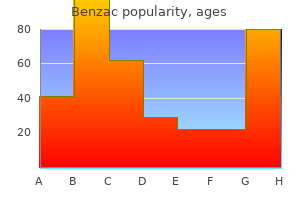
The brain and part of the calvaria are removed to demonstrate the sinuses related to the falx cerebri and tentorium cerebelli skin care nz buy benzac with american express. Although they are valveless and blood may flow in both directions acne practice purchase 20 gr benzac fast delivery, flow in the emissary veins is usually away from the brain skin care wiki buy benzac 20gr lowest price. C acne rosacea pictures best order benzac, confluence of sinuses; I skin care cream discount benzac 20 gr with amex, internal jugular vein; S, sigmoid sinus; T, transverse sinus. A posterior condylar emissary vein may also be present, passing through the condylar canal, connecting the sigmoid sinus with the suboccipital venous plexus. Anteromedially, it passes between the laminae and through the intervertebral foramina to communicate with the internal vertebral venous plexus and veins around the vertebral artery. The trabeculae are composed of flattened, irregularly shaped fibroblasts that bridge the subarachnoid space (Haines, 2006). Small areas of dura are supplied by other arteries: meningeal branches of the ophthalmic arteries, branches of the occipital arteries, and small branches of the vertebral arteries. Sensory endings are more numerous in the dura along each side of the superior sagittal sinus and in the tentorium cerebelli than they are in the floor of the cranium. A space may develop in the dural border cell layer as the result of trauma, such as a hard blow to the head (Haines, 1993, 2006). The subarachnoid space separates the two layers of the leptomeninges, the arachnoid and pia. Because of these connections, an infection of the face may spread to the cavernous sinus and pterygoid venous plexus. Blood from the medial angle of the eye, nose, and lips usually drains inferiorly through the facial vein, especially when a person is erect. Hence, space-occupying lesions, such as tumors in the supratentorial compartment, produce increased intracranial pressure, and may cause part of the adjacent temporal lobe of the brain to herniate through the tentorial notch. The innermost part of the dura, the dural border cell layer, is composed of flattened Bulging of Diaphragma Sellae Pituitary tumors may extend superiorly through the aperture in the diaphragma sellae, or cause it to bulge. Distension of the scalp or meningeal vessels (or both) is believed to be one cause of headache (Green, 2010). The infection usually involves only one sinus initially, but it may spread to the opposite side through the intercavernous sinuses. Septic thrombosis of the cavernous sinus often results in the development of acute meningitis. The bacteria may enter the subarachnoid space through the blood (septicemia, or "blood poisoning"), or spread from an infection of the heart, lungs, or other viscera. Because these venous channels are valveless, compression of the thorax, abdomen, or pelvis, as occurs during heavy coughing and straining, may force venous blood from these regions into the internal vertebral venous system and from it into the dural venous sinuses. Head Injuries and Intracranial Hemorrhage Extradural (epidural) hemorrhage is arterial in origin. Blood from torn branches of a middle meningeal artery collects between the external periosteal layer of the dura and the calvaria. The blood does not collect within a preexisting space, but rather creates a space at the Fractures of Cranial Base In fractures of the cranial base, the internal carotid artery may be torn, producing an arteriovenous fistula within the cavernous sinus. Arterial blood rushes into the cavernous sinus, enlarging it and forcing retrograde blood flow into its venous tributaries, especially the ophthalmic veins. Dural border hemorrhage usually follows a hard blow to the head that jerks the brain inside the cranium and injures it. Some subarachnoid hemorrhages are associated with head trauma involving cranial fractures and cerebral lacerations. Each cerebral hemisphere is divided for descriptive purposes into four lobes, each of which is related to , but the boundaries of which do not correspond to , the overlying bones of the same name. From a superior view, the cerebrum is essentially divided into quarters by the median longitudinal cerebral fissure and the coronal central sulcus. The central sulcus separates the frontal lobes (anteriorly) from the parietal lobes (posteriorly). The posteriormost point of the posteriorly projecting occipital lobe is the occipital pole. The medulla oblongata (medulla) is the most caudal subdivision of the brainstem that is continuous with the spinal cord; it lies in the posterior cranial fossa. The cerebellum is the large brain mass lying posterior to the pons and medulla and inferior to the posterior part of the cerebrum. The parieto-occipital sulcus demarcating the parietal and occipital lobes is seen on the medial aspect of the cerebrum. It is divided into the posterior cerebellomedullary cistern (cisterna magna) and the lateral cerebellomedullary cistern. The choroid plexuses consist of fringes of vascular pia mater (tela choroidea) covered by cuboidal epithelial cells. Clinically, the internal carotid arteries and their branches are often referred to as the anterior circulation of the brain. Each internal carotid artery enters the cranial cavity through the carotid canal in the petrous part of the temporal bone. The cervical parts of the vertebral arteries ascend through the transverse foramina of the first six cervical vertebrae. The bilaterally paired internal carotid and vertebral arteries deliver an abundant supply of oxygen-rich blood. The orientation drawing (left) indicates the plane of the coronal section that intersects the carotid canal (right). The cervical part of the internal carotid artery ascends vertically in the neck to the entrance of the carotid canal in the petrous temporal bone. It emerges from the canal superior to the foramen lacerum, closed in life by cartilage, and enters the cranial cavity. A, anterior cerebral artery and its branches; I, the four parts of the internal carotid artery; M, middle cerebral artery and its branches; O, ophthalmic artery. The left temporal pole is removed to show the middle cerebral artery in the lateral sulcus of the brain. Consciousness may be lost for only a few seconds, as occurs in most knockdowns during boxing. With a more severe injury, such as that resulting from an automobile accident, consciousness may be lost for hours and even days. If a person recovers consciousness within 6 hr, the long-term outcome is excellent (Rowland, 2010). The needle is carefully inserted through the posterior atlanto-occipital membrane into the cistern. The sudden stopping of the moving head results in the brain hitting the suddenly stationary cranium. The absence of loss of consciousness does not mean that the concussion is any less serious. The bruising results either from the sudden impact of the still-moving brain against the suddenly stationary cranium, or from the suddenly moving cranium against the still-stationary brain. Lacerations result in rupture of blood vessels and bleeding into the brain and subarachnoid space, causing increased intracranial pressure and cerebral compression. Aqueductal stenosis (narrow aqueduct) may be caused by a nearby tumor in the midbrain or by cellular debris following intraventricular hemorrhage or bacterial and fungal infections of the central nervous system (Corbett et al. This condition squeezes the brain between the ventricular fluid and the calvarial bones. In elderly persons, the anastomoses of the arterial circle are often inadequate when a large artery. The most common causes of strokes are spontaneous cerebrovascular accidents, such as cerebral thrombosis, cerebral hemorrhage, cerebral embolism, and subarachnoid hemorrhage (Rowland, 2010). The posterior communicating arteries are absent in some individuals; in others there may be two anterior communicating arteries. An embolus separates from the plaque and is carried in the blood until it lodges in an artery, usually an intracranial branch that is too small to allow its passage. Quickly restoring oxygen to the blood supply may reverse the brain damage (Elkind, 2010). The optical axes (axes of gaze, the direction or line of sight) for the two eyeballs, are parallel, however, and in the anatomical position run directly anteriorly ("looking straight ahead"), the eyeballs being in the primary position. This anterolateral view allows a view of the orbit and apex, which lie in the sagittal plane and are not well seen in an anterior view. Kucharczyk, Professor and Neuroradiologist Senior Scientist, Department of Medical Imaging, University Health Network, Toronto, Ontario, Canada. The bone forming the orbital margin is reinforced to afford protection to the orbital contents and provides attachment for the orbital septum, a fibrous membrane that extends into the eyelids. Anterolaterally, a shallow depression in the orbital part of the frontal bone, called the fossa for lacrimal gland (lacrimal fossa), accommodates the lacrimal gland. Anteriorly, the medial wall is indented by the lacrimal groove and fossa for lacrimal sac; the trochlea (pulley) for the tendon of one of the extra-ocular muscles is located superiorly. Much of the bone forming the medial wall is paper thin; the ethmoid bone is highly pneumatized with ethmoidal cells, often visible through the bone of a dried cranium. The inferior wall is demarcated from the lateral wall of the orbit by the inferior orbital fissure, a gap between the orbital surfaces of the maxilla and the sphenoid. Its posterior part separates the orbit from the temporal and middle cranial fossae. The lateral walls of the contralateral orbits are nearly perpendicular to each other. The bones forming the orbit are lined with periorbita, the periosteum of the orbit. The conjunctival sac is the space bound by the palpebral and bulbar conjunctivae; it is a closed space when the eyelids are closed, but opens via an anterior aperture, the palpebral fissure (L. The inferior eyelid has been everted to show the reflection of conjunctiva from the anterior surface of the eyeball to the inner surface of the eyelid. The semilunar fold is a vertical fold of conjunctiva near the medial angle, at the lacrimal caruncle. Their ciliary margins are free, but they are attached peripherally to the orbital septum (palpebral fascia in the eyelid). In this dissection of the orbit, the eyelids, orbital septum, levator palpebrae superioris, and some fat have been removed. Structures receiving lacrimal drainage from the conjunctival sac are seen medially. The junctions of the superior and inferior eyelids make up the medial and lateral palpebral commissures, defining the medial and lateral angles of the eye (G. The septum constitutes in large part the posterior fascia of the orbicularis oculi muscle. Accessory lacrimal glands may also be present, sometimes in the middle part of the eyelid, or along the superior or inferior fornices of the conjunctival sac. The eyelids come together in a lateral to medial sequence pushing a film of fluid medially over the cornea, somewhat like windshield wipers. From this sac, the fluid passes to the inferior nasal meatus of the nasal cavity through the nasolacrimal duct. It drains posteriorly across the floor of the nasal cavity to the nasopharynx and is eventually swallowed. In addition to cleansing particles and irritants from the conjunctival sac, lacrimal fluid provides the cornea with nutrients and oxygen. The presynaptic parasympathetic secretomotor fibers are conveyed from the facial nerve by the greater petrosal nerve and then by the nerve of the pterygoid canal to the pterygopalatine ganglion, where they synapse with the cell body of the postsynaptic fiber.
Although a small percentage of the normal popula tion will exhibit a blood pressure differential between the upper extremities skin care 101 cheap benzac on line, a blood pressure differential 20 mmHg in this clinical context should be considered highly s uspi cious acne 30s female discount generic benzac uk. That said skincare for men generic benzac 20 gr with amex, the absence of a blood pressure differen tial does not exclude aortic dissection acne 10 purchase 20 gr benzac. Perform a focused neurologic examination acne on arms 20gr benzac, looking for signs of hemiplegia or paraplegia. Although relatively easy and quick to perform, transthoracic echocardiography is only 59. Coronal co mputed tomography ang iogra m of a 49 -year-old male with a Sta nford type A aortic dissection. Always consider alterna tive life-threatening conditions in your differential diagnoses, including acute myocardial infarction, pulmo nary embolism, abdominal aortic aneurysm, and tension pneumothorax. Numerous medica tions are available for this purpose, and regardless of the specific agent(s) employed, the target heart rate is <60 bpm and target systolic blood pressure is 90- 1 20 mmHg. Initiate treatment in all patients with a high clinical suspicion before a confirmatory diagnosis is made. Beta-blockers are generally considered the first-line therapy for acute dissection given their ability to reduce both blood pressure and heart rate. Because of its short duration of action and rapid onset, esmolol is an excellent first-line agent. Start with a loading dose of 500 meg/kg given over 1 minute followed by a continuous infusion at 50 meg/kg/min. If the desired ventricular response has not been achieved within 5 minutes, repeat the loading dose and increase the infusion to 1 00 meg/kg/min. In such situations, begin a continuous infusion of an arterial vasodilator such as nitroprusside (0. Regardless of which medication is used, never initiate vasodilator therapy until the heart rate is adequately suppressed with beta-blockers to avoid reflex tachycardia and propagation of the dissection. As an alternative, labetalol is a reasonable single agent due to its selective a 1 and nonselective beta-blocking prop erties. If the desired blood pressure and heart r ate are not achieved within 10 minutes, administer escalating doses (ie, 20 mg, 40 mg, 80 mg, 1 60 mg) at 1 0-minute intervals to a cumulative maximum dose of 300 mg. If necessary, additional boluses of N labetalol can be given while concurrently titrating the infusion to more rapidly achieve the goal heart rate and blood pressure. Stanford type A dissections require prompt cardiothoracic consulta tion for operative repair, whereas type B dissections are typically managed medically. Patients with known chronic aortic dissections can be safely dis charged provided their blood pressure is adequately con trolled and their presenting complaint is unrelated to the underlying dissection. Acute aortic dissection in the emergency department: Diagnostic challenges and evidence-based man agement. That said, fewer than 1% of all patients with hypertension will ever develop a hypertensive emergency. Evaluating a patient with severe hyperten sion should focus on the rapid distinction between hyper tensive emergency or hypertensive urgency, as the treatment and disposition differ dramatically. Hypertensive urgency is less clearly defined, but can be thought of as a severe elevation in blood pres sure without evidence of acute end-organ dysfunction. The suggested mechanism behind hypertensive emer gency requires a sudden increase in systemic vascular resistance due to an unregulated surge in circulating vaso constrictors. The injured endothelium produces pathologic increases in vas cular permeability, activation of the platelets and coagula tion cascade, and the localized deposition of intraluminal fibrin. Secondary fibrinoid necrosis of the arteriolar end organ circulation results in significant tissue hypoperfu sion and consequent organ system dysfunction. Most individuals presenting with hypertensive emer gency will carry a previous diagnosis of hypertension. Chronic hypertension forces a shift in cerebral autoregulation, allowing patients to tolerate signifi cant elevations in blood pressure without any signs of cere bral end-organ damage. Always remember that treating blood pressure based on numbers alone, without considering the clinical context, can be altogether quite harmful for the patient. Start with a focused history and comprehensive review of systems, inquiring about the presence of chest pain, back pain, shortness of breath, hematuria or decreased urine output, and neurologic complaints including numbness, weak ness, headache, confusion, and visual disturbances. Patients with hyperten sive encephalopathy present with neurologic complaints including altered mental status, severe headache, seizures, vomiting, and visual disturbances. Patients with intracranial hemorrhage present with severe headache (often sudden onset), focal neurologic deficits, and/or altered mental status. Variable associated symptoms include orthopnea, hemoptysis, and chest pain or pressure. Patients with acute coro nary syndrome usually present with chest pain, although subtle signs of congestive heart failure may be the only presenting complaint. Associated symptoms include neurologic deficits, syncope, and abdominal pain, as well as constitutional symptoms such as nausea, vomiting, or diaphoresis. Patients may also present with swelling of the lower extremities or shortness of breath due to significant fluid retention. Focal neurologic findings may also be present and do not always follow the normal vascular distributions associated with stroke syndromes due to the global breakdown of the entire cerebral autoregulatory system. Meningeal irritation (eg, nuchal r igid ity) may be present in a patient with hemorrhage in the subarachnoid space. Lower extremity edema, j ugular venous distention, and an acces sory gallop (S3 or S4) may be noted. Patients will often be dia phoretic and may have evidence of heart failure on e xam. A blood pressure differential of >20 mmHg between arms or a new aortic insufficiency mur mur suggests the presence of an aortic dissection. Physical exam may reveal evidence of fluid overload but is often rather unremarkable. Obtain a urinalysis (specifically looking for hema turia or proteinuria) and serum blood urea nitrogen and creatinine to evaluate for acute kidney injury. Check a urine pregnancy test on all females of reproductive age to rule out evolving eclampsia. Order cardiac enzymes in patients complaining of chest pain, back pain, or shortness of breath. The width of the cuff bladder (inflatable por tion of the cuff) should equal approximately 40% of the arm circumference. Perform a detailed physical exam, focusing on the neurologic, cardiac, pul monary, and abdominal examinations. A more detailed description of expected f mdings related to specific diag noses follows. Always tailor your choice of agent to its mechanism of action to ensure the optimal management of individual hypertensive emergencies (Table 1 8- 3). Discharge Severely hypertensive patients without evidence of acute end-organ damage (ie, hypertensive urgency) can be safely discharged with oral antihypertensive medications and close outpatient follow-up. The event is classi cally followed by a spontaneous recovery to normal menta tion. The etiology of syncope encompasses a wide variety of disorders ranging from the benign to the acutely life-threatening. That said, a careful history and physical exam combined with the appropriate ancillary testing will help identify high-risk individuals who require hospital admission for further work-up and management. Syncope occurs secondary to impaired blood flow to either the reticular activating system or the bilateral cere bral hemispheres. The reduction in cerebral perfusion produces uncon sciousness and a loss of postural tone. A reflexive sympa thetic response combined with the recumbent positioning of the patient results in restored cerebral perfusion and a return to a normal level of consciousness. Patients who experience the sensation of nearly "passing out" without an overt loss of consciousness are termed near-syncope or presyncope. From a clinical standpoint, both near-syncope and syncope are approached in the same manner. Examples include neural mediated (reflex), orthostatic, cerebrovascular, and cardiac. The resulting combination of bradycardia and vasodilation reduces the overall cardiac output and thereby inhibits adequate cerebral perfusion. Prodromal symptoms are common and include subjective feelings such as dizziness, warmth, or lightheadedness. Certain situations involving increased vagal tone such as forceful coughing, micturi tion, and defecation can also initiate this reflex. This occurs because of transient arterial hypotension after a positional change to either sitting upright or standing. The underlying mechanism depends on either significant volume depletion (bleeding, dehydration) or intrinsic autonomic dysfunction. Elderly patients t end to be the most prone to autonomic dysfunction secondary to blunted sympathetic responses and medication side effects. That said, loss of conscious ness can occur after a subarachnoid hemorrhage when the intracranial pressure rises suddenly and the cerebral perfu sion is transiently lowered. Patients typically have a pro longed post-event recovery, which helps to differentiate cerebrovascular syncope from alternative e tiologies. This occurs when either structural heart defects or cardiac dysrhythmias transiently impair cardiac output. These events frequently occur without warning, which helps to distinguish cardiac syncope from alternative etiologies. In cases of structural heart disease, the syncopal event typically occurs during or immediately following exercise. Of note, cardiac syncope t ends to have the worst prognosis, with 1 -year mortality rates of 1 8-33%. The cardiovascular exam should include a detailed auscultation of the heart, listen ing for arrhythmias or any murmurs s uggestive of underly ing structural heart disease. Laboratory Routine laboratory evaluation is useful only when indi cated by the history and physical exam. Check a complete blood count in all patients with a history of bleeding or a positive stool guaiac. Order a basic metabolic panel with any concern for cardiac dysrhythmia secondary to significant electrolyte abnormalities. Finally, check cardiac markers in patients with antecedent chest pain or shortness of breath. History A comprehensive history is critical and may identify the etiology in up to 40% of cases. It is very important to clarify all of the events immediately preceding, during, and after the episode. Interview all family members and emer gency medical service personnel present during the event. Patients with significant cardiac histories are at higher risk of arrhythmia, whereas elderly patients on multiple medications are predisposed to orthostatic syncope. Antecedent dizziness, nausea, and diaphoresis or symptoms occurring after moving from a recumbent or sitting to upright position suggest a benign vasovagal or orthostatic episode respectively. Syncope that occurs either suddenly without prodrome or with physical exer tion suggests arrhythmia or structural heart disease (aor tic stenosis, hypertrophic cardiomyopathy). Indications include signs and symptoms sugges tive of a cerebrovascular etiology such as an antecedent headache, focal neurologic deficits on physical exam, or a prolonged recovery phase after the syncopal event. Indications include syncope that occurs without prodrome or is preceded by chest pain or shortness of breath. Tailor any ensuing laboratory and imaging studies to abnormalities discovered during the history and physical exam. Identify and avoid any poten tially contributing medications that the patient might be taking (eg, beta-blockers, nitrates). Quinn J, McDermott M, et al: Prospective validation of the San Francisco rule to predict patients with serious outcomes. Further work-up including Holter monitoring or tilt-table testing can be arranged in the primary care setting. Hyperventilation is ventilation that exceeds metabolic demands, such as can be caused by a psychological stressor (eg, anxiety attack). This can begin at the mechanical level, with any possible cause of airway obstruction, and can end at the cellular level, with any chemical inability to offload oxygen to tissues. If time p ermits, a systematic walk-through from airway to tissue can help elucidate the more difficult diagnoses. However, treatment for life-threatening severe respiratory distress must be initiated during, or even before, the diagnostic work-up. If the patient cannot oxygenate, there will be anoxic injury, espe cially brain injury, within seconds to minutes. The inability to perform the act of breathing (failure to ventilate) leads to carbon dioxide buildup, and the ensuing acidosis can lead to cardiac dysfunction. Finally, if the patient cannot maintain an open airway (due to brain injury, mechanical occlusion, etc. Recognizing and promptly intervening on the rapidly reversible causes of severe respiratory distress can prevent the need for intubation. Imagine the patient had to run for his or her life (in many ways, this is what the patient is doing). Consider all of the following in this assessment: airway, chest walUmusculature, diaphrag matic excursion, posture, age, body mass index, car diopulmonary status, and baseline exercise tolerance. If the patient has poor reserve or already has respiratory fatigue, it may be wiser to intubate ing situation. In these cases, there is a temporal relationship between exposure and onset of dyspnea.
A functional test that detects reduced perfusion to a segment of the lung is likely to add information to that provided by an anatomic image alone acne fulminans buy discount benzac 20gr online. Asymmetrical pulmonary venous stenosis results in redistribution of flow throughout the lungs acne quistico benzac 20gr with amex. Primary pulmonary vein stenosis is characterized by focal narrowing of the junction between one or more pulmonary veins and the left atrium acne keloidalis nuchae pictures order benzac with a mastercard. Length skin care cream benzac 20 gr overnight delivery, stenosis morphology and severity can vary from short weblike lesions to long diffusely diseased segments skin care with honey purchase discount benzac on line. All postoperative patients in which the left atrium was manipulated should routinely have their pulmonary veins evaluated, because pulmonary vein stenosis can develop long after the surgical procedure. Ostial ablation is associated with an approximate 8% reduction in ostial diameter. Focal narrowing is most prevalent in the left inferior pulmonary vein, likely due to more medial location within the cardiac silhouette, leading to less precise localization of the pulmonary ostium and energy delivery within the pulmonary vein rather than in the preferred ostial location. Findings of pulmonary vein stenosis after radiofrequency ablation include extensive fibrosis in the perihilar tissues. Stenoses usually begin approximately 1 to 2 mm lateral to the ostium and extend peripherally for variable lengths of up to 35 mm. Imaging from a 25-year-old man with refractory paroxysmal atrial fibrillation treated with radiofrequency ablation. Differential Diagnosis Pulmonary vein "pseudo-stenosis" variant is a rare radiological finding of the left inferior pulmonary vein, with a waistlike narrowing involving the venous ostium. Clinical Issues Patients with the pediatric form of pulmonary vein stenosis, either primary or secondary, have a very poor prognosis without treatment. Most of these patients suffer from pulmonary hypertensive crisis, recurrent pulmonary infection, or hemoptysis. Various treatment options are balloon dilatation, stenting, and/or lung transplantation. In adults, clinical success rates of up to 80% have been documented for atrial fibrillation ablation procedures. However, ostial ablation of the pulmonary veins is associated with increased risk of pulmonary vein stenosis, which occurs in 1 to 3% of patients. Other associated severe complications include endocardial charring, pulmonary vein dissection, stroke, hemopericardium, hemothorax, pulmonary vein thrombosis, and atrial or pulmonary vein perforation. Pulmonary vein thrombosis and hemodynamically significant pulmonary vein stenosis can lead to pulmonary venous infarction, fibrosing mediastinitis, pulmonary veno-occlusive disease, and pulmonary arterial hypertension. Less severe complications include small pleural or pericardial effusions and transient small atrial septal defects. Post-radiofrequency ablation pulmonary vein stenosis is mostly treated by endovascular techniques. Risk factors for restenosis include small reference vessel diameter and longer time from pulmonary vein ablation to intervention for pulmonary vein stenosis. Key Points Noninvasive tests are generally sufficient to diagnose pulmonary vein stenosis. Approximately one-half of patients with primary pulmonary vein stenosis have associated cardiac defects. Evaluation for stenotic pulmonary veins is indicated in any young patient with severe pulmonary hypertension. Symptomatic patients after radiofrequency ablation procedures should have a thorough evaluation for possible pulmonary vein stenosis. Pulmonary vein stenosis is a rare cause of pulmonary hypertension and is associated with significant morbidity and mortality. It is imperative that radiologists be familiar with left atrium and pulmonary vein variant anatomy. Multimodality imaging assessment of anatomic and functional pulmonary vein stenosis. Symptoms and signs of significant left-to-right shunt include congestive heart failure, tachypnea, cardiomegaly with enlargement of right heart, and tachycardia. Signs of congestive heart failure, including cardiomegaly and pulmonary vascular prominence, may be seen with significant left-to-right shunting, although these findings are not specific. Limitations include the requirement for intravenous contrast and exposure to ionizing radiation. Axial (b) and coronal (c) views show the anomalous vessel (arrowhead) draining into the left brachiocephalic vein (arrow). Patients may present with tachypnea, cardiomegaly with enlargement of right heart, and tachycardia. For children with scimitar syndrome, however, there is a high incidence of postoperative pulmonary venous obstruction and decreased right lung perfusion. Note the enlarged pulmonary artery suggestive of a significant left-to-right shunt and right-sided heart strain. Outcomes after surgical treatment of children with partial anomalous pulmonary venous connection. The anomalous right pulmonary vein gently curves down in a vertical course in the right mid-lung, traversing the right medial cardiophrenic angle, and resembles a Turkish sword (scimitar), hence the name. The syndrome is also referred to as hypogenetic lung syndrome and congenital pulmonary venolobar syndrome. However, Scimitar syndrome specifically is exceedingly rare, with an incidence of just 2 per 100,000 births. With the return of oxygenated blood to the right atrium, an extracardiac left-to-right shunt is produced. The shunt is often hemodynamically insignificant but when significant can produce right heart volume overload and pulmonary hypertension, depending on the size of the shunt. Scimitar syndrome is also associated with cardiac anomalies 25% of the time, and other anomalies such as diaphragmatic and spinal anomalies can also be seen. Adult: asymptomatic and detected incidentally on chest radiograph Prognosis for those with Scimitar syndrome without associated cardiac anomalies is quite good, as these individuals have a normal or near-normal lifespan. Prognosis is moderate to poor, however, for those who present in the neonatal period, as irreversible pulmonary hypertension can result. Clinical Features Scimitar syndrome is clinically silent in approximately 50% of patients who maintain subclinical left-to-right shunts. Patients may also present with paradoxical embolization if a septal defect is present. The most common signs and symptoms depend on age at presentation and size of left-to-right shunt: Newborn: right heart volume overload, congestive heart failure, pulmonary hypertension Older child: recurrent infections in right lung base Anatomy, Physiology, and Pathophysiology Unilateral pulmonary hypoplasia during embryogenesis is the primary abnormality in Scimitar syndrome, and the anomalous pulmonary venous return develops secondarily. The degree or severity of pulmonary hypoplasia ranges from mild to marked, and it most commonly affects the upper and/or middle lobes. The right pulmonary artery and mainstem bronchus display a similar degree of hypoplasia as the right lung. The right lung additionally often has morphological features of the left lung, including a hyparterial bronchus and absence of the minor fissure. Also, there is sometimes systemic arterialization of the right lung base; however, this entity is distinguished from pulmonary sequestration by having normal lung parenchyma in the affected right lower lobe. The right lung hypoplasia results in volume loss that produces a rightward shift of the mediastinum and dextroposition of the heart. This does not represent true dextrocardia, as the heart maintains normal orientation with the apex directed left. The anomalous pulmonary venous return delivers oxygenated blood to the right atrium, which creates a left-toright shunt with increased blood flow to the pulmonary vessels. If the shunt is significant enough, the right heart may become volume overloaded and enlarged. Finally, if the shunt is right to left 2:1 or greater, pulmonary hypertension may develop, producing Eisenmenger physiology if irreversible. Angiography can be used to visualize filling of the scimitar vein during the venous phase of pulmonary artery angiogram. Angiography is useful, however, for treatment purposes, with embolization of anomalous venous supply undertaken to reduce the size of the shunt. Also, anomalous arterial supply to the right lower lobe may be embolized before planned surgical intervention in order to reduce bleeding complications. Clinical Issues In half of affected patients, Scimitar syndrome produces a very small shunt and is asymptomatic. For those with more significant shunts presenting in the neonatal period, the prognosis is moderate or poor, as irreversible pulmonary hypertension may develop. For the subset of patients with left-to-right shunts greater than 2:1, endovascular or open surgical intervention is recommended to ligate or coil embolize anomalous venous drainage or restore pulmonary venous flow to the left atrium. Finally, when there is a systemic arterial supply, it is often embolized before any operative intervention in order to minimize bleeding complications. Note that the caliber of the anomalous vein does not taper as the vein progresses distally, unlike a normal pulmonary vein. It is a spectrum disorder with clinical signs, symptoms, and prognosis dependent on the severity of left-to-right shunt and age of presentation. Surgical and/or endovascular intervention is required if there are cardiac anomalies or left-to-right shunt is greater than 2:1 to ligate or embolize the anomalous pulmonary vein and/or arterial supply. Suggested Reading Berrocal T, Madrid C, Novo S, Gutierrez J, Arjonilla A, Gomez-Leon N. Congenital anomalies of the tracheobronchial tree, lung, and mediastinum: embryology, radiology, and pathology. The Scimitar syndrome: anatomic, physiologic, developmental, and therapeutic considerations. Horseshoe lung: clinical, pathologic, and radiographic features and a new plain film finding. Instead, the pulmonary veins drain to systemic veins or directly to the right atrium. The left atrium and ventricle may be normal or small secondary to low systemic blood flow. The presence of pulmonary venous obstruction determines the severity and clinical features. The snowman pattern is less specific in infancy because of prominence of the thymus. Cardiac catheterization may be seldom needed to answer questions not solved by echocardiography. The left atrial cavity is small, secondary to the lack of incorporation of the common pulmonary vein into the left atrium during its development, although the left atrial appendage often has a normal size and morphology. The size of the interatrial communication must be identified on cross-sectional imaging or echocardiography to determine the presence of restrictive flow to the left atrium, which is a cause of obstruction to pulmonary venous drainage. Note the vertical vein (arrow), which drains into the left innominate vein, in the left mediastinum. In the right mediastinum, an enlarged superior vena cava (arrowhead) is seen with an enlarged right atrium. The appearance of the congested venous system gives the "snowman" appearance of the cardiothymic silhouette. One must also identify the structure to which the pulmonary veins connect and the presence or absence of anatomic stenosis. Any imaging modality may demonstrate enlargement of the right atrium, right ventricle, and pulmonary arteries secondary to volume overload from the systemic and pulmonary venous return to the right atrium. Notice the congestion of the venous circulation compared to the systemic circulation. Preoperatively, prostaglandin E1 may be used to dilate the ductus venous and ductus arterious to improve systemic perfusion; however this is not effective with severe obstruction. Long-term prognosis after surgery is determined by several factors including preoperative hypoplastic/stenotic pulmonary veins, associated complex cardiac abnormalities, postoperative pulmonary hypertension, and postoperative pulmonary venous stenosis. A mean 3-year survival of 85% following surgical intervention has been documented. Total anomalous pulmonary venous connection: morphology and outcome from an international population-based study. Orellana Definition Cor triatriatum, also referred to as cor triatriatum sinister, is a congenital anomaly in which a fibromuscular septum divides the left atrium into an anteroinferior and posterosuperior compartment. These chambers often communicate through fenestrations in the intra-atrial septum. Clinical Features Most patients with cor triatriatum present in infancy, especially if the intra-atrial septum fenestrations are small or nonexistent. Cor triatriatum discovered in adulthood is often an incidental finding and is usually asymptomatic. Symptomatic presentation conversion commonly involves fibrosis of the fenestrations in the membrane as well as development of valvular insufficiency and atrial arrhythmias. Patients can present with symptoms similar to mitral stenosis or pulmonary venous thrombus, including dyspnea, hemoptysis, chest pain, right heart failure, and syncope. Anatomy, Physiology, and Pathophysiology the anteroinferior division is also known as the true atrium and contains the mitral valve orifice, vestibule, and the left atrial appendage. The posterosuperior division, also known as the false atrium, receives the pulmonary veins. Cor triatriatum can be classified into three groups based on the number of fenestrations in the dividing membrane. According to the Loeffler classification system: the etiology of cor triatriatum is debatable.
The proximal and distal vessel calibers to the area of stenosis are used to evaluate the restriction in lumen surface area; in this case skin care 29 year old discount benzac master card, there is greater than 70% stenosis acne help order benzac no prescription, which is indicative of severe disease acne 7-day detox purchase benzac 20gr visa. Sensitivity and specificity results for proximal coronary segments were 93% and 95% skin care brand crossword discount 20gr benzac fast delivery, respectively skin care mask generic benzac 20gr on line, with similar results for mid-segments; distal segments showed a sensitivity of 80% and a specificity of 97%. Conventional coronary angiography is the gold standard for evaluation of coronary artery stenosis. However, it is limited in its ability to visualize calcified plaques and small noncalcified plaques, which renders it inadequate in the evaluation of coronary artery disease in low- and intermediate-risk patients. Differential Diagnosis (for Symptoms of Chest Pain) Coronary artery spasm Mitral valve prolapse Aortic stenosis Acute myocarditis Aortic dissection Pulmonary embolism Gastroesophageal reflux disease Peptic ulcer disease Musculoskeletal disease of the chest wall Clinical Issues Treatment of coronary artery disease is classified into medical therapy and revascularization. Most patients with coronary artery stenosis of greater than 70% derive more benefit from revascularization than from medical therapy. In addition, patients are encouraged to reduce their risk factors for acute coronary events by initiating exercise, ceasing smoking, and maintaining blood pressure, glycemic, and lipid control. Frequency and distribution of thin-cap fibroatheroma and ruptured plaques in human coronary arteries. Noninvasive assessment of coronary artery disease anatomy, physiology, and clinical outcome. Orellana Definition A coronary artery aneurysm (also known as ectasia) is defined as a segment of greater than 1. There are several complications that result from aneurysm formation, such as thrombosis, embolism, vessel rupture, arteriovenous fistula formation, and spasm. Thrombosis is a sequela of slow blood flow and can result in myocardial ischemia or embolization. Rupture of the vessel remains a rare complication due to early detection, but can result in cardiac tamponade. Clinical Features Aneurysms are a common incidental finding on coronary angiography. Patients with coronary artery aneurysms can be asymptomatic or present with angina, congestive heart failure, myocardial infarction, or sudden death. Clinical presentation usually stems from the underlying coronary artery disease and is not specific to coronary artery aneurysm formation. In one study, the majority of patients with coronary artery aneurysms also had significant coronary artery stenoses. The most common etiology of coronary artery aneurysm formation in the United States is atherosclerosis, accounting for 50% of cases. Aneurysm formation is thought to result from intimal plaque formation leading to an adjacent degenerated tunica media causing plaque rupture and wall dilatation. These aneurysms form from hemorrhage in the adventitia and do not usually involve all How to Approach the Image Conventional coronary angiography is the gold standard for diagnosing coronary artery aneurysms. A disadvantage of this modality is underestimation of aneurysm size when thrombus is present. However, its inferior spatial resolution and inability to demonstrate peripheral linear calcifications within the aneurysm makes it a less favorable option. Differential Diagnosis Cardiac chamber aneurysm Post-traumatic pseudoaneurysm of the ascending aorta or pulmonary trunk Coronary artery fistula Cardiac or pericardial tumor Mediastinal mass. Medical treatment of coronary artery aneurysms involves the use of anticoagulants and antiplatelet agents. Coronary artery aneurysms: a review of the natural history, pathophysiology, and management. Key Points Coronary artery aneurysm, or ectasia, is defined as a segment greater than 1. The underlying etiology is unknown, but it is hypothesized to be related to a combination of infectious agents, abnormal immunological response, and genetic factors. The overall annual incidence in the United States is 17 to 27 per 100,000 children younger than 5 years of age. Up to one-third of such aneurysms thrombose; they are associated with myocardial infarction, arrhythmias, or sudden death. Other cardiac manifestations include myocarditis with depressed cardiac function, coronary arteritis without aneurysm formation, valvulitis, and pericardial effusion. Echocardiography, however, is less sensitive for detecting distal lesions and worsening coronary stenoses in arterial segments affected by aneurysms. Both techniques are optimized with heart rates of less than 70 beats per minute, which may necessitate the use of beta-blockers. Patients with aneurysms may also undergo periodic nuclear stress testing for inducible ischemia. As previously noted, no contrast is seen within and distal to the second aneurysm, signifying complete vascular occlusion. However, contrast is seen distal to the third aneurysm, likely owing to retrograde flow from collateral vessels. Approximately 50% of these may regress to a normal luminal diameter within the first 2 years of onset, but regression does not typically occur after 2 years. Coronary artery aneurysms may be associated with thrombosis or stenoses with resulting ischemia, arrhythmias, or sudden death. Fate of coronary aneurysms in Kawasaki disease: serial coronary angiography and long-term follow-up study. Muta H, Ishii M, Egami K, et al: Early intravenous gamma-globulin treatment for Kawasaki disease: the nationwide surveys in Japan. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Detection of coronary artery aneurysms, stenoses and occlusions by multislice spiral computed tomography in adolescents with kawasaki disease. Stunning can be the result of a single ischemic event, as in "acute stunning," or of multiple episodes of ischemia, termed "repetitive stunning. A second state of myocardial dysfunction, known as "hibernating myocardium," is the result of chronically reduced resting perfusion, which can be reversed with restoration of adequate perfusion. When hibernating myocardium is identified in patients with poor left ventricular function, revascularization has been demonstrated to markedly reduce morbidity and mortality. Therefore, clinicians must identify patients in whom revascularization can be expected to improve cardiac function. Once myocardial dysfunction is identified, it must be determined whether the region of dysfunctional myocardium is viable or scarred, as only viable myocardium will benefit from revascularization. Hibernating myocardium may be limited to a small focus, where left ventricular function is not significantly compromised, or may involve the left ventricle globally, leading to severe hypokinesis. Symptoms and signs are those of ischemic cardiomyopathy and congestive heart failure and include the following: Anatomy, Physiology, and Pathophysiology In both stunned and hibernating myocardium, ischemia is the cause. It is the timing of the ischemia, however, that differentiates the pathophysiology. Stunned myocardium results from a single acute event or repetitive episodes of ischemia. Following these ischemic events, high intracellular calcium levels cause myofilament desensitization and lysis. Reperfusion leads to generation of oxygen free radicals that disturbs ion pump and mitochondrial function. This leads to remodeling of myocytes, including dedifferentiation, reduced production of contractile proteins, reduced size of mitochondria, interstitial fibrosis, and glycogen accumulation. While normally perfused myocardium preferentially utilizes fatty acids for energy, hibernating myocardium demonstrates relatively increased uptake of glucose, as glucose can be metabolized anaerobically. Dyspnea on exertion Exercise intolerance Angina Fluid retention Reduced ejection fraction/cardiac output Infarct Arrhythmia How to Approach the Image Identification of hibernating and viable myocardium by imaging is made possible by the physiological differences between well-perfused, poorly perfused, and infarcted and scarred myocardium. A variety of imaging modalities have been used to successfully differentiate hibernating and viable myocardium from infarcted and scarred myocardium. In the upper row, blood flow imaging using rubidium 82 in short-axis view shows markedly decreased perfusion, extending from distal to basal slices in the apical, inferior, inferolateral, and septal regions of the left ventricle at rest. Reproduced with permission from Macmillan Publishers Ltd: Nature Clinical Practice Cardiovascular Medicine, 2008. In the first-pass/blood pool phase, normal and stunned myocardium is well perfused, while infarcted and scarred and hibernating and viable myocardium will demonstrate lack of perfusion. Because infarcted and scarred myocardium has an expanded extracellular space relative to viable and stunned myocardium, tracer will accumulate in infarcted tissue in the steady-state phase, resulting in delayed contrast enhancement. This necessitates identification of patients who will likely benefit from revascularization or from medical management. Some myocardial tissue identified as viable does not demonstrate functional recovery after revascularization; therefore, the term hibernating myocardium is a retrospective description, and viable myocardium is a prospective description. On the other hand, anterior and lateral infarctions are often associated with development of ventricular dysrhythmias. The coronary artery circulation is divided into a right-, left- or co-dominant circulation. Microscopic findings mainly comprise eosinophilic coagulative necrosis, which can later evolve into granulation tissue and a fibrous scar. Additionally, nuclear scintigraphy can detect a reduced or absent tracer uptake during stress and rest images. Other features include lack of redistribution of thallium-201 and reinjection uptake of technetium-99m radiotracer. Thrombolysis can also be administered within the first 12 hours of development of symptoms (in the absence of contraindications for thrombolysis). As a last resort, coronary artery bypass graft surgery can be performed in an acute setting. Noninvasive imaging techniques to aid in the triage of patients with suspected acute coronary syndrome: a review. Transmural extent of acute myocardial infarction predicts long-term improvement in contractile function. In the event of acute coronary occlusion, ischemic myocardial necrosis begins within 20 minutes and spreads to most of the myocardial wall within roughly 6 hours. Depending on the duration of infarct development, biochemical markers indicative of acute injury may approach normal limits. These include substernal chest pain with or without radiation, palpitations, nausea, vomiting, and/or dyspnea. This is often the case in diabetic patients as neuropathy precludes normal pain sensation. The segment nomenclature along the circumference is basal anterior, basal anteroseptal, basal inferoseptal, basal inferior, basal inferolateral, and basal anterolateral. The attachment of the right ventricular wall to the left ventricle can be used to identify the septum. The segment names are apical anterior, apical septal, apical inferior, and apical lateral. These individual segments may be assigned to specific coronary artery territories with the recognition of the anatomic variability that may exist. Chest radiography is typically performed given the likely cardiopulmonary etiology based on presenting symptoms. Radiographic findings may include calcification of myocardium, pulmonary venous congestion, and cardiomegaly. The left ventricle is divided perpendicular to the long axis of the heart into equal thirds. This generates three circular sections of the left ventricle-basal, mid-cavity, and apical-and an apical cap representing the tip of the ventricle where there is no real cavity. It is important clinically because it can lead to embolic phenomena, including stroke. Other complications, including ventricular aneurysm or valvular regurgitation, can also be diagnosed using cross-sectional imaging in addition to echocardiography. Delayed enhancement and T2-weighted cardiovascular magnetic resonance imaging differentiate acute from chronic myocardial infarction. Dissociation between changes in intramyocardial function and left ventricular volumes in the eight weeks after first anterior myocardial infarction. Differentiation of recent and chronic myocardial infarction by cardiac computed tomography. Transmural progression of necrosis within the framework of ischemic bed size (myocardium at risk) and collateral flow. Discrimination of myocardial acute and chronic (scar) infarctions on delayed contrast enhanced magnetic resonance imaging with intravascular magnetic resonance contrast media. Left ventricular end-systolic volume as the major determinant of survival after recovery from myocardial infarction. Pathological findings vary from myocardial wall edema to vascular occlusion and myocardial necrosis. This hypoenhanced zone is the core where the microvascular obstruction occurs and is usually surrounded by a hyperenhancement zone of delayed enhancement. Oblique (a) and four-chamber (b) views with delayed contrast enhancement demonstrate a rim of delayed enhancement (arrows) surrounding a core of myocardial necrosis. Short- (a) and long-axis (b) views of delayed contrast enhancement surrounding a zone of myocardial necrosis (arrows). Note the extent of infarct involves the entire myocardial thickness and is therefore transmural.
The skin ligaments also anchor the skin to the underlying deep fascia (plantar aponeurosis) skin care before wedding purchase discount benzac on line, improving the "grip" of the sole acne gel 03 purchase benzac without a prescription. The skin of the sole is hairless and sweat glands are numerous; the entire sole is sensitive ("ticklish") skin care routine order generic benzac on-line, especially the thinnerskinned area underlying the arch of the foot acne in early pregnancy order benzac 20 gr with mastercard. It resembles the palmar aponeurosis of the palm of the hand but is tougher acne xia buy benzac 20gr line, denser, and elongated. From the plantar aspect, muscles of the sole are arranged in four layers within four compartments. The skin and subcutaneous tissue have been removed to demonstrate the deep fascia of the leg and dorsum of the foot. Thinner parts of the plantar fascia have been removed, revealing the plantar digital vessels and nerves. A large central and smaller medial and lateral compartments of the sole are created by intermuscular septa that extend deeply from the plantar aponeurosis. Concurrently, they are also able to refine further the efforts of the long muscles, producing supination and pronation in enabling the platform of the foot to adjust to uneven ground. The muscles of the foot are of little importance individually because fine control of the individual toes is not important to most people. Although the adductor hallucis resembles a similar muscle of the palm that adducts the thumb, despite its name the adductor hallucis is probably most active during the push-off phase of stance in pulling the lateral four metatarsals toward the great toe, fixing the transverse arch of the foot, and resisting forces that would spread the metatarsal heads as weight and force are applied to the forefoot (Table 5. The 2nd layer consists of the long flexor tendons and associated muscles: four lumbricals and the quadratus plantae. The 3rd layer consists of the flexor of the little toe and the flexor and adductor of the great toe. The posterior tibial artery terminates as it enters the foot by dividing into the medial and lateral plantar arteries. Branching of the parent neurovascular structures that give rise to plantar vessels and nerves. After coursing between and supplying the fibular muscles in the lateral compartment of the leg, the superficial fibular nerve emerges as a cutaneous nerve about two thirds of the way down the leg. It then supplies the skin on the anterolateral aspect of the leg and divides into the medial and intermediate dorsal cutaneous nerves, which continue across the ankle to supply most of the skin on the dorsum of the foot. Its terminal branches are the dorsal digital nerves (common and proper) that supply the skin of the proximal aspect of the medial half of the great toe and that of the lateral three and a half digits. It innervates this area as the 1st common dorsal (and then proper dorsal) digital nerve(s). The medial plantar nerve, the larger and more anterior of the two terminal branches of the tibial nerve, arises deep to the flexor retinaculum. Its distribution to both skin and muscles of the foot is comparable to that of the median nerve in the hand. The level of junction of these branches is variable; it may be high (in the popliteal fossa), or low (proximal to heel). The dorsalis pedis artery begins midway between the malleoli and runs anteromedially, deep to the inferior extensor retinaculum between the extensor hallucis longus and the extensor digitorum longus tendons on the dorsum of the foot. The dorsalis pedis artery passes to the first interosseous space, where it divides into the 1st dorsal metatarsal artery and a deep plantar artery. The latter passes deeply between the heads of the first dorsal interosseous muscle to enter the sole of the foot, where it joins the lateral plantar artery to form the deep plantar arch. The arcuate artery runs laterally across the bases of the lateral four metatarsals, deep to the extensor tendons, to reach the lateral aspect of the forefoot, where it may anastomose with the lateral tarsal artery to form an arterial loop. The medial and lateral plantar arteries are terminal branches of the posterior tibial artery. The deep plantar artery and perforating branches of the deep plantar arch provide anastomoses between the dorsal and the plantar arteries. Unlike the leg and thigh, however, the venous drainage of the foot is primarily to the major superficial veins, both from the deep accompanying veins and other smaller superficial veins. These veins drain to the dorsal venous arch of the foot, proximal to which a dorsal venous network covers the remainder of the dorsum of the foot. The larger superficial branch of the medial plantar artery supplies the skin on the medial side of the sole and has digital branches that accompany digital branches of the medial plantar nerve, the more lateral of which anastomose with medial plantar metatarsal arteries. As it crosses the foot, the deep plantar arch gives rise to four plantar metatarsal arteries; three perforating branches; and many branches to the skin, fascia, and muscles in the sole. The plantar metatarsal arteries divide near the base of the proximal phalanges to form the plantar digital arteries, supplying adjacent digits (toes); the more medial metatarsal arteries are joined by superficial digital branches of the medial plantar artery. The lateral superficial lymphatic vessels drain the lateral side of the dorsum and sole of the foot. The fibularis brevis tendon can easily be traced to its attachment to the dorsal surface of the tuberosity on the base of the 5th metatarsal. Its position should be observed and palpated so that it may not be mistaken subsequently for an abnormal edema (swelling). Superficial lymphatic vessels from the lateral foot join those from the posterolateral leg, converging to vessels accompanying the small saphenous vein and draining into the popliteal lymph nodes. The pain is often most severe after sitting, and when beginning to walk in the morning. A neglected puncture wound may lead to an extensive deep infection, resulting in swelling, pain, and fever. A well-established infection in one of the enclosed fascial or muscular spaces usually requires surgical incision and drainage. Calcaneus (C) Calcaneal spur (arrow) Bursa (not seen in radiograph) C Sural Nerve Grafts Pieces of the sural nerve are often used for nerve grafts in procedures such as repairing nerve defects resulting from wounds. In thin people, these branches can often be seen or felt as ridges under the skin when the foot is plantarflexed. Injections of an anesthetic agent around these branches in the ankle region, anterior to the palpable portion of the fibula, anesthetizes the skin on the dorsum of the foot (except the web between and adjacent surfaces of the 1st and 2nd toes) more broadly and effectively than more local injections on the dorsum of the foot for superficial surgery. A diminished or absent dorsalis pedis pulse usually suggests vascular insufficiency resulting from arterial disease. The five P signs of acute arterial occlusion are pain, pallor, paresthesia, paralysis, and pulselessness. In these cases, the dorsalis pedis artery is replaced by an enlarged perforating fibular artery. Hemorrhaging Wounds of Sole of Foot Puncture wounds of the sole of the foot involving the deep plantar arch and its branches usually result in severe bleeding, typically from both ends of the cut artery because of the abundant anastomoses. Medial plantar nerve compression may occur during repetitive eversion of the foot. Infections on the lateral side of the foot initially produce enlargement of popliteal lymph nodes (popliteal lymphadenopathy); later, the inguinal lymph nodes may enlarge. Palpation of Dorsalis Pedis Pulse the dorsalis pedis artery pulse is evaluated during a physical examination of the peripheral vascular system. Arteries of foot: the dorsal and plantar arteries of the foot are terminal branches of the anterior and posterior tibial arteries, respectively. It also contributes to formation of the deep plantar arch via its terminal deep plantar artery. The heavy, prominent acetabular rim of the acetabulum consists of a semilunar articular part covered with articular cartilage, the lunate surface of the acetabulum (text continues on p. The lower limb joints are (A) those of the pelvic girdle connecting the free lower limb to the vertebral column, (B) the knee and tibiofibular joint, and (C) tibiofibular syndesmosis, ankle joint, and the many joints of the foot. The joint was disarticulated by cutting the ligament of the head of the femur and retracting the head from the acetabulum. Relative strengths are indicated by arrow width: Anteriorly, the muscles are less abundant but the ligaments are robust; posteriorly, the muscles predominate. In this coronal section of hip joint, the acetabular labrum and transverse acetabular ligament, spanning the acetabular notch (and included in the plane of section here), extend the acetabular rim so that a complete socket is formed. The angle of Wiberg (see text) is used radiographically to determine the degree to which the acetabulum overhangs the head of the femur. Several different lines and curvatures are used in the detection of hip abnormalities (dislocations, fractures, or slipped epiphyses). A fossa that crosses the line suggests an acetabular fracture with inward displacement. The acetabular rim and lunate surface form approximately three quarters of a circle; the missing inferior segment of the circle is the acetabular notch. This ligament blends with the medial part of the iliofemoral ligament, and tightens during both extension and abduction of the hip joint. The ligaments and peri-articular muscles (the medial and lateral rotators of the thigh) play a vital role in maintaining the structural integrity of the joint. In all synovial joints, a synovial membrane lines the internal surfaces of the fibrous layer, as well as any intracapsular bony surfaces not lined with articular cartilage. Its wide end attaches to the margins of the acetabular notch and the transverse acetabular ligament; its narrow end attaches to the fovea for the ligament of the head. The malleable nature of the fat pad permits it to change shape to accommodate the variations in the congruity of the femoral head and acetabulum, as well as changes in the position of the ligament of the head during joint movements. In other words, in assuming the upright position, a relatively small degree of joint stability was sacrificed to maximize weight-bearing when erect. Even so, the hip joint is our most stable joint, owing also to its complete ball and socket construction (depth of socket), the strength of its joint capsule, and the attachments of muscles crossing the joint, many of which are located at some distance from the center of movement (Palastanga et al. Because the joint capsule does not attach to the posterior aspect of the femur, the synovial membrane protrudes from the joint capsule, forming the obturator externus bursa to facilitate movement of the tendon of the obturator externus (shown in part C) over the bone. The degree of flexion and extension possible at the hip joint depends on the position of the knee. Not all of this movement occurs at the hip joint; some results from flexion of the vertebral column. During extension of the hip joint, the fibrous layer of the joint capsule, especially the iliofemoral ligament, is taut; therefore, the hip can usually be extended only slightly beyond the vertical except by movement of the bony pelvis (flexion of lumbar vertebrae). From the anatomical position, the range of abduction of the hip joint is usually somewhat greater than for adduction. In addition to its function as an adductor, the adductor magnus also serves as a flexor (anterior or aponeurotic part) and an extensor (posterior or hamstrings part). The gluteus maximus serves as the primary extensor from the flexed to the straight (standing) position, and from this point posteriorly, extension is achieved primarily by the hamstrings. Retinacular arteries arising from the medial circumflex femoral artery are most abundant, bringing more blood to the head and neck of the femur because they are able to pass beneath the unattached posterior border of the joint capsule. Retinacular arteries arising from the lateral circumflex femoral must penetrate the thick iliofemoral ligament and are smaller and fewer. Colored Arrows = the arrows show the direction of rotation of femoral head caused by activity S of functional groups. Although the knee joint is well constructed, its function is commonly impaired when it is hyperextended. The stability of the knee joint depends on (1) the strength and actions of the surrounding muscles and their tendons, and (2) the ligaments that connect the femur and tibia. The hip bone and proximal femur are included to demonstrate the Q-angle, determined during physical examination to indicate alignment of the femur and tibia and to evaluate valgus or varus stress at the knee. The fibrous layer of the joint capsule is relatively thin in some places and thickened in others to form reinforcing intrinsic (capsular) ligaments. Modifications of the anterior aspect and sides of the fibrous layer include the patellar retinacula, which attach to the sides of the quadriceps tendon, patella, and patellar ligament, and incorporation of the iliotibial tract (laterally) and the medial collateral ligament (medially). The fibrous layer has a few thickened parts that make up intrinsic ligaments, but for the main part, it is thin and is actually incomplete in some areas (5. The fibrous layer attaches to the femur superiorly, just proximal to the articular margins of the condyles. The synovial membrane lines the internal surface of the fibrous layer laterally and medially, but centrally it becomes separated from the fibrous layer.
Cheap benzac american express. TOM FORD FOR MEN SKINCARE AND GROOMING COLLECTION -- The Film.
References
- Szczeklik A, Stevenson DD. Aspirin-induced asthma: advances in pathogenesis, diagnosis, and management. J Allergy Clin Immunol 2003; 111(5):913-21.
- Studenski S, Duncan PW, Chandler J, et al. Predicting falls: the role of mobility and nonphysical factors. J Am Geriatr Soc 1994;42:297-302.
- Jones RB, Ferraro AJ, Chaudhry AN, et al. A multicenter survey of rituximab therapy for refractory antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum 2009;60:2156-68.
- Marder VJ, Chute DJ, Starkman S, et al. Analysis of thrombi retrieved from cerebral arteries of patients with acute ischemic stroke. Stroke 2006;37:2086-93.
- Lyman GH, Papahadjopoulos D, Preisler HD. Phospholipid membrane stabilization by dimethylsulfoxide and other inducers of Friend leukemic cell differentiation. Biochim Biophys Acta. October 19, 1976;448(3):460-473.