Anthony T. Reder, M.D.
- Associate Professor of Neurology
- Department of Neurology
- The University of Chicago
- Chicago, IL
You also explain that multiple gestations are at risk for preterm labor antibiotic classes buy generic cefixime 100 mg on-line, preterm birth iv antibiotics for sinus infection cefixime 100mg discount, placental abnormalities bacteria 25 degrees order cefixime australia, cesarean section due to malpresentation infection list purchase cefixime with american express, preeclampsia antibiotics for uti cats buy cefixime no prescription, and gestational diabetes. In twin-totwin transfusion syndrome, the recipient twin may suffer from which of the following complications The last ultrasound showed only 12% discordance in fetal weights, with baby A estimated to be 200 g larger than baby B. You begin counseling them on the risks and benefits of vaginal birth with twins, including breech extraction, and cesarean section. She is unsure of her last period but reports that she started feeling the baby move approximately 5 months ago. She has not been taking any medications in pregnancy and has had no other exposures. Ultrasound performed in your clinic shows gestational age to be approximately 40 weeks 3 days. The nurse reports that the patient denies any contractions, leaking fluid, or vaginal bleeding. She last felt the baby move once this morning and felt the baby move only twice yesterday. Answer B: Fetal ultrasound to evaluate growth is the next best step in management. At each routine prenatal visit after 20 weeks of gestation, the fundal height is measured to evaluate fetal growth. For each week of gestation over 20 weeks, the corresponding fundal height should match in centimeters. When the fundal height and gestational age are discordant by 3 or more centimeters, a fetal ultrasound is indicated to better assess fetal growth. Group B streptococcus cultures are collected around 35 to 36 weeks of gestation or sooner if preterm birth is suspected. Toxoplasmosis is acquired either by consuming infected undercooked meat or through contact with infected cat feces. One third of women have antibodies to toxoplasmosis, indicating previous exposure. In women who are exposed to toxoplasmosis for the first time in pregnancy, rates of fetal infection are 10% to 15% in the first trimester, 25% in the second trimester, and 60% in the third trimester. Although increasing gestational age is associated with increased risk of infection, the severity diminishes. Fetal rubella infection depends on gestational age and is worse if acquired in early gestation. Fetal growth retardation is the most common effect, followed by sensorineural hearing loss, cardiac lesions, and eye defects. These findings are generally seen only in fetuses infected in the first 12 weeks of gestation. Congenital herpes virus is rare and is associated with growth restriction, eye disease, microcephaly, or hydranencephaly. Amniocentesis can be performed to evaluate for fetal chromosomal abnormalities or intrauterine infection. Tobacco use reduces uterine blood flow to the placenta and impairs fetal oxygenation. Seroconversion in the mother is more common in day care workers, individuals of lower socioeconomic status, as well as those with increased parity, abnormal Pap smear history, and multiple sexual partners. Answer C: Although no one answer is perfect, the best answer is fetal ultrasound every 2 to 3 weeks. It is important to monitor the fetus for interval growth and ensure that fetal growth continues. Delivery is warranted when the benefits of the intrauterine environment are outweighed by the risks to the fetus. Before induction of labor of a 30-week fetus, the mother should receive betamethasone to improve fetal outcomes after birth. Decreased oxygen delivery to the fetus can trigger changes in the vascular smooth muscle tone of the fetus. Changes in the flow resistance through the umbilical artery can be measured and used to predict fetal well-being and placental dysfunction. Late signs of dysfunction such as reversed end-diastolic flow suggest fetal acidemia, and delivery is warranted. Frequent Doppler testing is only performed when abnormalities have been identified on prior testing. Elevated Doppler of the umbilical artery and declining weight raise the concern for fetal well-being. It is possible that this patient may require premature delivery if fetal condition deteriorates further. To improve outcomes in the neonate, betamethasone should be administered at this time. Even with fetal lung maturity documented, one would not deliver on this basis alone. If fetal status changes, such as absent or reversed Doppler flow, delivery will be indicated regardless of fetal lung maturity. Answer D: Cord prolapse is not a direct consequence of oligohydramnios, nor is it strongly associated with oligohydramnios. Answer A: Macrosomic neonates are most at risk for neonatal jaundice, hypoglycemia, birth trauma, hypocalcemia, and childhood cancers such as leukemia, osteosarcoma, or Wilms tumor. Hypoglycemia is thought to be due to maternal hyperglycemia resulting in fetal hyperglycemia and hyperinsulinemia. Beta-cell hyperplasia also occurs, and immediately after birth when the umbilical cord is clamped, the neonate experiences a sudden drop in blood glucose level likely because of an exaggerated insulin release after delivery. In macrosomic infants, as many as 50% can experience hypoglycemia, and this rate is lowered to 5% to 15% when tight glucose control is achieved in the latter half of pregnancy as well as during the labor process. Birth trauma is directly related to the risk of shoulder dystocia in mothers with diabetes and macrosomic infants. Birth injury can be a transient palsy to permanent neurologic deficits or even death. Fetal macrosomia complicates as many as 50% of pregnancies in women with gestational diabetes, including women treated with intensive glycemic control. The Pedersen hypothesis proposes that maternal hyperglycemia results in fetal hyperglycemia and hyperinsulinemia, which in turn results in excessive fetal growth. Target fasting levels are less than 90; 1-hour postprandial values should be less than 140, and 2-hour postprandial values less than 120. Advanced maternal age has been found to be associated with macrosomia but may be related because of an increased rate of diabetes in older women. Postterm pregnancies are at increased risk for fetal macrosomia because of the additional time in utero that the fetus has to grow. It is best to actually give the patient the laboratory slip to obtain the test prior to the 6-week follow-up visit so that the results can be discussed at the visit. This test helps to identify those women who either have type 2 diabetes or who remain at high risk because of insulin insensitivity. Education, diet, and exercise are mainstay treatments to improve insulin sensitivity. Although this patient should eventually lose weight down to and even slightly below her prepregnancy weight, this does not need to occur immediately. She does not need to lose 20% of her body weight, which would potentially make her underweight. Weight loss can be challenging after childbirth, and breastfeeding is a very effective way for women to return toward their prepregnancy weight in the postpartum period. For type 1 and type 2 diabetic patients, prepregnancy doses of insulin are resumed. Answer D: In patients with a history of gestational diabetes, it is valuable to perform an early glucose tolerance test to evaluate for type 2 diabetes. Because she has not had any routine health care in the past 2 years, she has not been screened for development of diabetes. Early diagnosis improves outcomes because patients can be educated on diet and started on insulinlowering medications if indicated. If the patient has elevated blood glucose values that suggest type 2 diabetes, then answer options a, b, c, and e should be performed for the patient at that time. In patients with type 2 diabetes, eye examination is recommended to evaluate for retinopathy, which can worsen in pregnancy. Cleavage at this stage occurs before cells are differentiated to form the trophoblast. Embryo cleavage between days 8 and 13 again occurs after differentiation of the trophoblast but also after formation of the amnion. The placenta has shared vascular connections between monochorionic twins, and in some gestations, these connections are markedly unequal and result in one twin receiving more blood flow than the other. The donor twin is typically smaller, anemic, and has less amniotic fluid, which can lead to hypovolemia, growth restriction, and oligohydramnios. The recipient twin is generally larger, polycythemic, and occasionally hydropic as the result of hypervolemia. Anemia, growth restriction, oligohydramnios, and hypovolemia are all findings in the donor twin. Answer B: In this answer, twin A is 925 g smaller than twin B, so more than 20% discordant (925/3,775). For twins, if both are cephalic, vaginal delivery is usually reasonable to attempt. However, with vertex/breech twins, the second twin should not be more than 20% discordant; if the second twin is significantly larger than the first, then there can be head entrapment during the breech extraction. In fact, some clinicians are uncomfortable with offering breech extraction of the second twin if it is even slightly larger than the first. In all cases, counseling and informed consent should include discussion of the possible need for an emergent cesarean delivery of the second twin should cord prolapse, fetal distress, or placental abruption occur and delivery not be imminent. As a result, we must rely on ultrasound for dating the pregnancy, and ultrasound is not without errors. Ultrasound dating is best when performed in the first trimester and may have up to a 1 week error in either direction of the proposed due date. For pregnancies dated during the second trimester, the error may be as great at 2 weeks, and in the third trimester, as much as 3 weeks. Fetal anomaly is occasionally a cause of postterm pregnancy but is not the most common cause. Delayed presentation to prenatal care is a problem that contributes to delay and inaccurate dating but is not the most specific answer in this case. Answer A: Postterm pregnancy is not associated with transient tachypnea of the newborn, which is seen more commonly in cesarean deliveries and in early term births at 37 and 38 weeks of gestation. Oligohydramnios, macrosomia, meconium aspiration, and intrauterine fetal demise are all risks associated with postterm pregnancy. Answer D: the patient should be seen on labor and delivery triage as soon as possible. Given her gestational age and risk for adverse pregnancy outcome, it is best to perform monitoring this evening. In patients less than 40 weeks of gestation, it may be acceptable to have them perform kick counts at home prior to presentation. Kick counts involve the women resting in a quiet room and counting fetal movements over time. In general, 6 movements in the first hour or 10 movements in 2 hours suggest reassuring fetal status. However, although widely used, there is not strong evidence to support the use of kick counts in predicting fetal well-being. Answer options b, c, and e all delay presentation and evaluation of fetal wellbeing and are therefore not the best answer choices. At 41 2/7 weeks, even if the fetal testing were reassuring, it would be reasonable to recommend induction of labor in this setting. This occurs as a result of decreased systemic vascular resistance starting in the latter half of the first trimester and reaching its nadir in the midsecond trimester. Chronic hypertension is seen increasingly in pregnancy and is associated with increased risk of maternal and neonatal morbidity. Complications from these disorders are consistently among the leading causes of maternal death in both developed and developing countries. Because treatment is delivery, these disorders are also the leading causes of premature delivery. The downstream effects of abnormal placental vascular development are placental underperfusion resulting in possible growth restriction and hypoxia. From a maternal standpoint, the endothelial dysfunction is thought to be primarily related to circulating antiangiogenic factors. This results in increased vascular permeability, activation of the coagulation cascade, microangiopathic hemolysis, and vasoconstriction manifesting clinically as hypertension, proteinuria, and other clinical manifestations of the disease. As outlined in Table 8-2, major fetal complications of preeclampsia are caused by prematurity. Also, the generalized vasoconstriction of preeclampsia can result in decreased blood flow to the placenta.
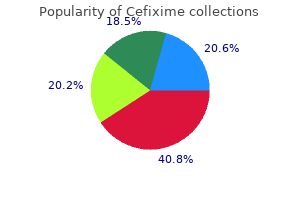
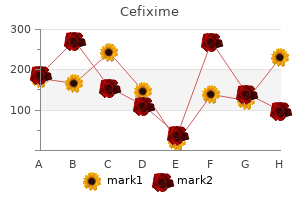
Induction of heart failure by minimally invasive aortic constriction in mice: reduced peroxisome proliferator-activated receptor gamma coactivator levels and mitochondrial dysfunction bacteria that begins with the letter x cheap cefixime line. Echocardiography alone allows the determination of heart failure stages in rats with pressure overload measuring antibiotic resistance (kirby-bauer) order cefixime with mastercard. Load-induced changes in vivo alter substrate fluxes and insulin responsiveness of rat heart in vitro antibiotics overuse order cefixime uk. A comparative serial echocardiographic analysis of cardiac structure and function in rats subjected to pressure or volume overload antibiotics for dogs after surgery discount 100 mg cefixime visa. The production of persistent elevation of systolic blood pressure by means of renal ischemia antibiotics for dogs bacterial infections generic 100mg cefixime with mastercard. Echocardiographic evaluation of size, function, and mass of normal and hypertrophied rat ventricles. Hypertension in Page (cellophane-wrapped) kidney is due to interstitial nephritis. Transition from compensatory hypertrophy to dilated, failing left ventricles in Dahl salt-sensitive rats. Myocardial fibrosis and stiffness with hypertrophy and heart failure in the spontaneously hypertensive rat. Effects of chronic right ventricular pressure overload on myocardial glucose and free fatty acid metabolism in the conscious rat. Effects of age on right ventricular hypertrophic response to pressureoverload in rats. Animal models of mitral regurgitation induced by mitral valve chordae tendineae rupture. Strong association between activated valvular interstitial cells and histopathological lesions in porcine model of induced mitral regurgitation. Serotonin markers show altered transcription levels in an experimental pig model of mitral regurgitation. A model of ischemic mitral regurgitation in pigs with three-dimensional echocardiographic assessment. Left ventricular dilatation and diastolic compliance changes during chronic volume overloading. Left ventricular diastolic and systolic performance during chronic experimental aortic regurgitation. Novel mouse model of left ventricular pressure overload and infarction causing predictable ventricular remodelling and progression to heart failure. Impaired myocardial fatty acid oxidation and reduced protein expression of retinoid X receptor-alpha in pacing-induced heart failure. A canine model of heart failure by intracoronary adriamycin injection: hemodynamic and energetic results. Bovine hereditary cardiomyopathy: an animal model of human dilated cardiomyopathy. High-sugar diets increase cardiac dysfunction and mortality in hypertension compared to low-carbohydrate or high-starch diets. A novel experimental model of giant cell myocarditis induced in rats by immunization with cardiac myosin fraction. Identification of myocarditogenic peptides derived from cardiac myosin capable of inducing experimental allergic myocarditis in the Lewis rat. Retrograde heart perfusion: the Langendorff technique of isolated heart perfusion. The continuing evolution of the Langendorff and ejecting murine heart: new advances in cardiac phenotyping. Crystalloid and perfluorochemical perfusates in an isolated working rabbit heart preparation. An improved isolated heart preparation for external assessment of myocardial metabolism. Contractile and vascular consequences of blood versus crystalloid cardioplegia in the isolated blood-perfused rat heart. However, in reality, the internal (and external) environment for an organism is far from constant. Marked fluctuations occur throughout the lifespan of an organism, on multiple time scales, ranging from seconds/minutes. Indeed, the dynamic nature with which cells/organs fluctuate biological processes is essential for life, facilitating adaptation to different environmental stimuli/stresses. One could argue that a form of rigidity or inflexibility is more conducive to a pathologic, as opposed to physiologic state; this concept is exemplified by cardiac metabolism, wherein the heart exhibits metabolic inflexibility during several disease states [1,2]. At the whole body level, multiple feedforward and feedback mechanisms are employed to maintain nutrients/metabolites within physiologic boundaries. Noteworthy, for a discrete period of time, blood glucose levels are elevated; it is only when this momentary hyperglycemia persists for prolonged periods of time that pathology ensues [4]. More specifically, biological processes fluctuate/oscillate in a time-dependent manner, which are essential for normal physiologic functions. Over the course of a normal day, organisms on earth are subjected to dramatic changes in their environment. These range from alterations in lighting, temperature, and humidity, to availability of food and the presence of predators. It is essential that these processes are orchestrated in a temporally appropriate manner. The same concept applies to metabolism, wherein temporal organization of opposing pathways. Returning to the example of postprandial glucose utilization, increased circulating insulin levels following consumption of a mixed meal during the awake period is a critical component of glucose homeostasis. However, it is important to note that the level of a stimulus is only one half of stimulus-response coupling, the second half involving sensitivity to the stimulus. Not only do stimuli vary over the course of the day, but so too does sensitivity of a cell/organ/ organism to the stimulus. For example, insulin sensitivity increases in humans in the early hours of the morning, perhaps in anticipation of food consumption upon waking, thus synchronizing the level of the stimulus. The purpose of the current chapter is to discuss temporal organization of cardiac metabolism on the 24 h timescale. This discussion will include a detailed overview of known oscillations in cardiac metabolism, information regarding mediators of these oscillations, and the importance of maintaining metabolic synchrony for normal cardiac function. In addition, the experimental implications of these oscillations, in terms of assessment of cardiac metabolism, will be highlighted. On a daily basis, dramatic fluctuations in energetic demand and supply occur, in association with sleep/wake and fasting/feeding cycles. It is therefore not surprising that cardiac metabolism is subject to dramatic swings each and every day, of which the peaks and troughs approach levels often observed in pathologic states. In terms of metabolism, the heart is undoubtedly a different organ during the day versus night. Within this subsection, current knowledge regarding time-of-day-dependent oscillations in cardiac metabolism will be discussed. It is important to note that the majority of these studies have been performed in laboratory rats and mice housed in a 12 h:12 h light:dark cycle. Accordingly, diurnal variations, as opposed to circadian rhythms (which are revealed only under constant conditions; usually constant darkness), have primarily been investigated. Laboratory rodents are nocturnal, meaning that they are more active during the dark phase, and are less active during the light phase. Thus, energetic demands on the heart of laboratory rodents are greatest during the dark phase (which is antiphase relative to humans). Diurnal Rhythms in Metabolic Fluxes Glucose Metabolism In quantitative terms, primary energy sources for the heart are lipid (triglyceride and fatty acids) and carbohydrate (glucose and lactate). It is noteworthy that recent studies suggest a more balanced energetic reliance between lipid, carbohydrate, and ketone bodies in the mouse heart [11]. In addition, myocardial glucose utilization is extremely responsive to insulin, an endocrine factor whose circulating levels are dependent on feeding status [13]. Given daily fluctuations in behaviors such as fasting/feeding and sleep/ wake cycles, it is not surprising that myocardial glucose utilization exhibits a marked diurnal variation at multiple levels (as described in subsequent sections). Initial studies investigated day-night differences in glucose oxidation in ex vivo perfused rat hearts [14]. Rates of glucose oxidation were approximately twofold higher for hearts isolated in the middle of the dark phase, versus hearts investigated in the middle of the light phase. An important point to note here was that glucose oxidation rates were interrogated in an ex vivo setting, where perfusion conditions. In doing so, it was reasoned that acute neurohumoral influences were eliminated, thereby revealing diurnal rhythms in the intrinsic properties of the heart. Subsequent studies in both rat and mouse hearts have confirmed these observations. One important caveat of the original rat heart study was that cardiac function was also higher for ex vivo perfused hearts when isolated during the dark phase [14]. As mentioned earlier, the heart increases reliance on glucose (and lactate) during periods of increased contractility, raising the possibility that day-night differences in glucose oxidation were secondary to energetic demand. However, subsequent studies in ex vivo perfused mouse hearts revealed increased 126 9. Glucose oxidation is not the sole index of glucose utilization that exhibits a diurnal variation in the rodent heart. Consistent with rhythms in glucose oxidation, rates of both glycolysis and glycogen synthesis are elevated in the middle of the dark phase in ex vivo working mouse hearts [16]. A coordinated increase in glycolysis, glucose oxidation, and glycogen synthesis during the dark phase has led to speculation that glucose uptake is increased in the mouse/rat heart at this time. However, time-of-day-dependent oscillations in myocardial glucose uptake have not been reported. Less is known regarding diurnal variations in myocardial glucose metabolism in vivo. Intuitively, one would expect that fluctuations in energetic demand and feeding status would augment day-night differences in myocardial glucose utilization in intact animals. In mice, synchronization between increased workload, circulating insulin levels, and the intrinsic drive to promote glucose uptake during the dark phase would be anticipated to result in augmented rates of glucose utilization at this time. Collectively, these observations have revealed marked diurnal variations in both oxidative and nonoxidative glucose metabolism in rodent hearts. Fatty Acid Metabolism Unlike myocardial glucose utilization, the oxidative metabolism of fatty acids by the heart does not appear to exhibit a marked diurnal variation (at least in an ex vivo setting). Both initial studies in isolated perfused rat hearts, as well as subsequent studies in mouse hearts, were unable to detect significant day-night differences in myocardial fatty acid oxidation rates [14,15,17]. It is noteworthy that these studies were performed using the nonesterified fatty acid oleate, raising the question whether diurnal variations exist in the oxidative metabolism of distinct, quantitatively significant lipid/fatty acid species, such as palmitate or lipoproteins. Previous studies have suggested a differential channeling of oleate and palmitate between oxidative and nonoxidative metabolic fates [18,19]. Interestingly, rates of net triglyceride synthesis exhibits a marked diurnal variation in ex vivo perfused mouse hearts, peaking in the middle of the dark phase [17]. Subsequent pulse-chase tracer studies indicated that rates of lipolysis significantly contribute toward day-night differences in net triglyceride synthesis, with increased lipolysis rates reported during the light phase [17]. Similar to the situation for myocardial glucose utilization, currently no studies have investigated diurnal rhythms in myocardial fatty acid metabolism in the intact animal. However, consistent with ex vivo flux measurements, triglyceride levels oscillate over the course of the day in the rodent heart, with decreased levels observed in the middle of the light phase [15,17]. Collectively, these observations suggest that the rodent heart exhibits increased lipolysis during the less active/sleep phase both in vivo and ex vivo. It is tempting to speculate that decreased insulin levels during the less active/sleep phase, coupled with the intrinsic properties of the heart, synergize to increase lipolysis at this time. Amino Acid Metabolism the heart is considered a metabolic omnivore, which is capable of utilizing essentially all energy substrates [20]. Although quantitatively less important, in terms of being a source of energy for contraction, the heart can readily utilize amino acids in both catabolic. With regards to time-of-day-dependent oscillations in amino acid metabolism, relatively little is known for the heart. Following injection of rats with a bolus of 3H-labeled leucine, Rau and Meyer reported that net incorporation of this radio labeled tracer into myocardial protein was greatest at the end of the light phase [21]. However, it is important to note that this study did not take into account, potential differences in circulating levels of endogenous leucine, or differential rates of leucine oxidation. We have previously reported that several amino acids are elevated in the heart during the sleep phase [22]. In addition, recent unpublished studies suggest increased rates of protein synthesis in the isolated perfused mouse heart during the light phase (M. Collectively, these observations suggest that protein synthesis may be increased during the light phase in the rodent heart, both in vivo and ex vivo. Consistent with this concept, isoproterenol-induced growth of the heart is greatest during the light, versus the dark, phase [23]. These observations appear to be somewhat counterintuitive with the anabolic properties of insulin; increased circulating insulin levels during the dark phase for the rodent would be anticipated to promote protein synthesis. Additional studies are required to elucidate fully time-of-day-dependent oscillations in myocardial amino acid metabolism, and the mechanisms responsible.
Subclinical viral shedding appears to be highest in the first 6 months following acquisition and is more common immediately before and after a clinical outbreak antibiotic nausea purchase cefixime 100 mg otc. Condom use can reduce the risk of transmission of genital herpes but will not prevent the transmission vyrus 987 c3 4v purchase cefixime amex. Both symptomatic and asymptomatic viral shedding can occur in genital areas not covered or protected by a condom different antibiotics for sinus infection trusted 100 mg cefixime. Recurrent outbreaks can be reduced through the use of daily suppressive antiviral drugs virus 360 purchase genuine cefixime on-line. Cesarean delivery is recommended only for those pregnant patients with active genital lesions or prodromal symptoms treatment for uti naturally cefixime 100mg online. With this shift in vaginal flora, there is an accompanied decrease in lactobacilli. Patients usually complain of an increased vaginal discharge that often has a malodorous, fishy amine odor. Alternatives include clindamycin 300 mg twice daily for 7 days or topical formulations of these antibiotics. Azithromycin 1 g orally once is also the correct treatment option for chlamydial infection. On the other hand, empiric treatment of chlamydial infection is recommended in patients infected with N. Although defenses such as ciliary movement creating flow and cervical mucus exist, there is essentially an open tract between the vagina, the pelvis, and abdomen. This can lead to ascending infections of the uterus, fallopian tubes, adnexa, pelvis, and abdomen. It is seen most commonly after cesarean delivery, but also after vaginal deliveries and surgical pregnancy terminations. However, antibiotic prophylaxis is recommended for cesarean sections, surgical terminations of pregnancy, and hysterosalpingography or sonohysterography in women with a history of pelvic infection, or if dilated tubes are demonstrated. Chronic endometritis is often asymptomatic but is clinically significant because it leads to other pelvic infections and, uncommonly, endomyometritis. It is often a polymicrobial infection with a variety of pathogens, including skin and gastrointestinal flora in addition to the usual flora colonizing the lower reproductive tract. Mycobacterium tuberculosis is a rare cause of chronic endometritis in the developed countries but is a leading cause of infertility in endemic countries. Chronic endometritis can be suspected in patients with chronic irregular bleeding, discharge, and pelvic pain. The diagnosis can be made in a nonpuerperal patient with endometrial biopsy showing plasma cells. Treatment course continues until clinical improvement and afebrile status for 24 to 48 hours. In nonpuerperal infections where chlamydial infection may be the suspected cause, doxycycline should be added to the regimen for a total of 14 days. Additionally, the risk of ectopic pregnancy is increased as much as 7- to 10fold, and approximately 20% of women develop chronic pelvic pain during their lifetime. Sequelae, including chronic pelvic pain, dyspareunia, and pelvic adhesions, may also require surgical therapy, contributing to the economic costs and morbidity of this disease. Among sexually active women, the incidence of this disease is highest in the 15- to 25-year-old age group (at least three times greater than in the 25- to 29-year-old age group). Clinical Manifestations the principal symptom of acute salpingitis is abdominal or pelvic/adnexal pain. The character of the pain can range (burning, cramping, and stabbing) and can be unilateral or bilateral. Other associated symptoms include increased vaginal discharge, abnormal odor, abnormal bleeding, gastrointestinal disturbances, and urinary tract symptoms. In practice, a more invasive diagnostic laparoscopic surgical procedure is usually performed only when appendicitis cannot be ruled out by clinical examination or when there is a poor response to treatment with antibiotics. This is a perihepatitis from the ascending infection resulting in right upper quadrant pain and tenderness and liver function test elevations. In particular, hospitalization is recommended for teenagers, nausea and vomiting, pregnant women, concern for follow-up or ability to take medications as an outpatient, those with a high fever, or who have been refractory to outpatient therapy. Findings associated with chronic pelvic inflammatory disease, including tubo-ovarian abscess, adhesions, pyosalpinx, and an abscess located in the posterior cul-desac. Most patients will endorse abdominal and/or pelvic pain (90%) and demonstrate fever and leukocytosis (60% to 80%). Culdocentesis that reveals gross pus is diagnostic but has been used less because advances in imaging studies have been made. Finally, laparoscopy can lead to a definitive diagnosis but is usually used only when the clinical picture is unclear. Unless the abscess is ruptured and causing peritoneal signs or is impenetrable by antibiotics, surgical treatment can often be avoided. Clindamycin (900 mg every 8 hours) plus gentamicin (loading dose of 2 mg/kg, followed by 1. Typically, a repeat pelvic examination is performed after the patient has been afebrile for 24 to 48 hours to monitor for improvement and eventual resolution of tenderness. If responsive to medical management, the patient can be converted to oral antibiotics to complete a 10- to 14-day course with doxycycline plus clindamycin or metronidazole. Since 1984, the incidence has decreased dramatically with only 59 cases reported in 2014. Gastrointestinal disturbances (abdominal pain, vomiting, and diarrhea), myalgias, mucous membrane hyperemia, increased blood urea nitrogen and creatinine, platelet count less than 100,000, and alteration in consciousness can also be seen. Blood cultures are often negative, possibly because the exotoxin is absorbed through the vaginal mucosa. Treatment Because of the seriousness of the disease (2% to 8% mortality rate), hospitalization is always indicated. For more severe cases in which patients are hemodynamically unstable, admission to an intensive care unit may be necessary. Antibiotic therapy consists of clindamycin plus vancomycin for empiric treatment, when specific S. Women account for 19% of all new cases, and 85% of this is through heterosexual sexual transmission. Initially, the infection is entirely asymptomatic, although the individual is a carrier of the disease; this stage can last from 5 to 7 years. This test does have false-positive results, which, in low-risk populations, may occur more often than truepositive results. Another level of confirmation may be obtained, if a viral load is sent and is positive. The approach to this disease is prevention of transmission, prophylaxis of opportunistic infections, and prolonging the lives of infected patients by slowing progression of disease with antiretroviral agents. Delaying the progression of the disease is accomplished primarily with nucleoside analogs and protease inhibitors. Because the action mechanisms of these two groups differ, a synergistic effect is seen with combination therapy known as highly active antiretroviral therapy. Second, the high incidence of invasive cervical cancer in this population requires more aggressive screening than in the general population. Increased transmission can be seen with higher viral burden or advanced disease in the mother, rupture of the membranes, and invasive procedures during labor and delivery that increase neonatal exposure to maternal blood. Vertical transmission can occur intrauterine (20% to 50%), intrapartum (50% to 80%), or postpartum (15%). Cesarean delivery has been shown to lower transmission rates by roughly two thirds compared to vaginal delivery in women on no therapy and particularly without onset of labor or rupture of membranes or in the setting of high viral load. In particular, Efavirenz (category D) has been associated with increased in neural tube defects, and women who are interested in becoming pregnant should be on an alternate regimen. The American College of Obstetricians and Gynecologists currently recommends routine Pap smear within 1 year of initial diagnosis or with first sexual encounter. Her labor course was complicated by prolonged rupture of membranes and stage 2 arrest because of cephalopelvic disproportion resulting in a cesarean delivery. Her postoperative course was uncomplicated, and she had been discharged home stable the day prior to presentation. She reports three new sexual partners in the last 6 months and uses condoms intermittently. Examination shows a soft abdomen and lower quadrant tenderness without guarding or rebound. On pelvic examination, there is a mucopurulent cervical discharge, moderate cervical motion tenderness, and uterine tenderness. On vaginal examination, her cervix is dilated to 6 cm with a bulging bag of water. On examination, her abdomen is diffusely tender with guarding and rebound present. The diagnosis is largely made clinically with findings of fever and uterine tenderness in a postpartum woman. The hematuria in this patient is likely due to contamination from the lochia postpartum. Chorioamnionitis or intra-amniotic infection is a maternal febrile morbidity exclusive to the intrapartum period. Septic pelvic thrombophlebitis is often a diagnosis of exclusion and should be considered in the setting of persistent unexplained fever in the postpartum period. This patient has a normal appearing incision making wound cellulitis very unlikely. Answer E: Postpartum endomyometritis is typically a polymicrobial infection involving both aerobes and anaerobes from the genital tract. Oral antibiotic therapy is not required following successful parenteral treatment. Although retained products of conception can cause endomyometritis, performing a dilation and curettage is not the most appropriate next step. In patients refractory to broad-spectrum parenteral antibiotics, additional imaging should be performed to look for other causes of fever. If retained tissue is found, a dilation and curettage may be necessary to remove the necrotic material. Patients with postpartum endomyometritis should be treated with broad-spectrum parenteral antibiotics. Oral doxycycline is typically used to treat chronic endometritis and chlamydial infections. Exploratory laparotomy is not indicated in a patient with postpartum endomyometritis. The diagnosis of postpartum endomyometritis is largely based on clinical findings. Imaging studies can be helpful in patient refractory to broad-spectrum parenteral antibiotics to look for an abscess, retained products, or septic pelvic thrombophlebitis. Answer A: Cesarean delivery is the most important risk factor for developing postpartum endomyometritis. In the absence of prophylactic antibiotics, there is a 30% rate of developing postpartum endomyometritis after a nonelective cesarean delivery versus 3% for a vaginal delivery. Additional risk factors may include multiple vaginal examinations, prolonged rupture of membranes, internal fetal monitoring, low socioeconomic status, manual removal of the placenta, and prolonged labor. However, clinical manifestations of ectopic pregnancies typically appear 6 to 7 weeks after the last normal menstrual period. Women also typically have vaginal bleeding, pain, and symptoms of early pregnancy. Pyelonephritis should be suspected in a patient with fever, flank pain, and costovertebral angle tenderness. Answer C: Lactobacilli are part of the normal flora of the female genital tract and are not indicative of an infection. Doxycycline 100 mg orally twice daily for 14 days is the treatment regimen for chronic endometritis. For those patients with a cephalosporin allergy, clindamycin can be used with gentamicin. Invasive procedures including artificial rupture of membranes and use of fetal scalp electrodes should be avoided. Women with a viral load greater than 1,000 copies/mL should be offered and recommended a cesarean section. Women with ovarian torsion typically complain of a sudden onset sharp lower abdominal pain. The patient should be monitored with a repeat pelvic examination after the patient has been afebrile for 24 to 48 hours. If the patient is responsive to medical management, the patient can be converted to oral antibiotics with doxycycline plus clindamycin or metronidazole for 10 to 14 days. Ampicillin can also be added to this regimen to increase coverage for gram-positive bacteria. Consulting infectious disease specialist is not appropriate in a potentially unstable patient. This is most often described using the DeLancey levels of vaginal support (Table 18-1). It is helpful to think of pelvic organ prolapse in the same way one views abdominal hernias; a break in the structural fascia leads to the bulging of structures normally held in by that fascia. Damage to the anterior vaginal wall pubocervical fascia can result in herniation of the bladder (cystocele) and/or urethra (urethrocele) into the vaginal lumen. Injuries to the endopelvic fascia of the rectovaginal septum in the posterior vaginal wall can result in herniation of the rectum (rectocele) into the vaginal lumen.
Syndromes
- Birthmarks that are the color of coffee with milk (cafe-au-lait marks)
- Use aerosolized respiratory treatments (inhaled medications) to open the airway
- Frequent urination
- AIDS, hepatitis, influenza, infectious mononucleosis, and other viral infections
- Decreased urine output
- Tests show that changes in your aortic valve are beginning to seriously harm how well your heart works.
- Large hands and feet with thick fingers and toes
- Alpha-1 antitrypsin deficiency
- Fluorescent antibody study to look for substances that are specific to Typhoid bacteria
Anomalies have also been observed in children exposed to carbamazepine with low epoxide hydrolase activity antibiotic 7169 order cefixime 100 mg with amex. Because there is particular evidence that high peak plasma levels of valproic acid may be more teratogenic than constant steady-state levels antimicrobial workout clothes order generic cefixime line, it should be dosed three to four times per day rather than the standard twice per day dosing antibiotic resistance animal agriculture cefixime 100 mg lowest price. However antibiotics tired discount 100mg cefixime mastercard, epileptic patients should be counseled that they are still at a greater risk (4% to 6% vs antibiotic resistance china generic 100mg cefixime amex. Therefore, patients should be advised to take supplemental folate prior to conception, particularly those using either valproic acid or carbamazepine. The decision to perform an amniocentesis routinely for -fetoprotein and acetylcholinesterase is controversial. All care providers-obstetricians, neurology, nursing, anesthesia, and pediatrics-should be informed about an epileptic patient in labor and delivery. Because trauma and hypoxia from a seizure can put both the mother and the fetus at risk, treatment of seizures should be discussed a priori with the group of practitioners caring for the patient. One difference is that the drug of choice in patients with a known seizure disorder is usually phenytoin compared with magnesium used in preeclamptic patients. There have been reports of increased risk of spontaneous hemorrhage in newborns because of the inhibition of vitamin K-dependent clotting factors. Although the risk is small, conservative management is to overcome this theoretical vitamin K deficiency by aggressive supplementation with vitamin K toward the end of pregnancy. Upon delivery, clotting studies can be performed on the cord blood and vitamin K administered to the infant. If the cord blood is deficient in clotting factors, fresh frozen plasma may be required to protect the newborn. The cardiovascular system undergoes a number of dramatic changes in pregnancy with a 50% increase in blood volume, decrease in systemic vascular resistance, increase in cardiac stroke volume, and actual remodeling of the myocardium to accommodate some of these changes. When caring for patients with cardiac disease preconceptionally or during pregnancy, these changes are paramount when counseling them regarding their options and managing their disease. In patients with cardiac disease and an increased risk of maternal mortality, the option to terminate the pregnancy should always be offered and discussed at length with the patient. Unfortunately, as such women often may not be able to adopt because of their illness, they may think of their own pregnancy as the only way to have children. Many of the diseases are stable prior to pregnancy with medical management, but during pregnancy can become quite unstable in response to the physiologic changes. Additionally, medications used during pregnancy may be different from those used outside of pregnancy. In particular, many of the newest antihypertensives and antiarrhythmics have been sparsely studied in pregnant women, and are thus commonly avoided. Of the more common agents, angiotensin-converting enzyme inhibitors, diuretics, and warfarin (Coumadin) have all been associated with congenital anomalies and other fetal effects and are usually discontinued in pregnancy. Patients who would benefit from surgical repair of a lesion as in mitral or aortic stenosis should undergo surgical repair a year or more before becoming pregnant. Because of high maternal risk, those who become pregnant before surgical repair should be offered termination of the pregnancy as the first line of management. It is important that patients and their families are aware of the risks of disabling morbidity and mortality if they decide to continue the pregnancy. Management and early intervention during labor and delivery can help to reduce risk for cardiac patients. Early epidural analgesia to control pain can minimize the cardiac stress of labor and delivery. Likewise, an assisted vaginal delivery (using forceps or vacuum) can diminish the potential detrimental cardiac effect of Valsalva with pushing. In addition, careful fluid monitoring should be maintained, possibly with a central venous pressure monitor and arterial line. After delivery, massive fluid shifts make the immediate postpartum period a particularly dangerous transition for women with congenital heart disease. First, postpartum women have increased venous return because they no longer have an enlarged uterus compressing the vena cava. Second, the uterus clamps down after placental expulsion and demands less circulation, leading to an effective autotransfusion of its blood supply (approximately 500 cc). Small case series show that, if optimally managed, these patients do relatively well in pregnancy. Throughout pregnancy and during labor and delivery, it is important to minimize increased demand on the heart. The most common right-to-left shunts are patent ductus arteriosus and ventricular septal defect, which have reversed as a result of Eisenmenger syndrome. In Eisenmenger syndrome, an initial left-to-right shunt overfills the right heart. This, in turn, leads to increased flow through the pulmonary vasculature, pulmonary capillary damage, and the formation of scar tissue. These patients are chronically hypoxic secondary to the mixing of deoxygenated blood and are encouraged to terminate their pregnancies. Patients who elect to continue their pregnancies are followed with serial echocardiograms to measure the pulmonary pressures and cardiac function. Some have been managed with inhaled nitric oxide, but this has not been shown to significantly improve the measured clinical indicators of disease or the outcomes. Perhaps the greatest concentrated risk of morbidity and mortality is in the postpartum period for approximately 2 to 4 weeks after delivery. It has been hypothesized that this risk is secondary to the sudden changes in hormones. Unfortunately, attempts to counter these changes with progesterone and estrogen supplementation have had little success. Patients with aortic stenosis and aortic insufficiency require a decreased afterload to maintain cardiac output, and thus initially may have diminished symptoms in response to the decreased systemic vascular resistance seen in pregnancy. Patients with mitral stenosis may be unable to meet the increased demands of pregnancy and experience a backup into the pulmonary system leading to congestive heart failure. Patients with pulmonary stenosis who elect to continue their pregnancy may actually undergo valvuloplasty during the pregnancy if they have severe disease. During pregnancy, the hyperdynamic state can increase the risk of aortic dissection and/or rupture, particularly in those patients with an aortic root diameter greater than 4 cm. In order to decrease some of the pressure on the aorta, women are advised to maintain a sedentary lifestyle and are often placed on beta-blockers to decrease cardiac output. Some of these patients likely have a baseline mild cardiomyopathy, whereas others have a postinfectious dilated cardiomyopathy. Patients present with classic signs and symptoms of heart failure and on echocardiogram have a dilated heart with an ejection fraction far below normal in the 20% to 40% range. The risk of permanent declining function is based on the severity of underlying renal disease. In fact, patients with mild renal disease will usually experience improvement in renal function throughout much of pregnancy. Only 10% of patients with mild disease will have permanent changes in glomerular filtration rate. Because of this, it is important to counsel these patients preconceptionally regarding the risks to them from pregnancy-in particular, the increased risk of requiring dialysis and its concomitant morbidities. For patients who have baseline proteinuria and hypertension, the diagnosis of preeclampsia can be difficult to make. Additionally, monitoring platelets and liver function tests can be helpful in delineating preeclampsia from worsening renal disease. It seems that such women will have outcomes similar to women with similar creatinine clearance. These women need to be closely monitored for adverse maternal outcomes because declining renal function in a transplant patient has grave consequences. In addition to closely watching renal function, monitoring the transplant is also important. Commonly, these women will be on immunosuppressants such as cyclosporine, tacrolimus, prednisone, and Imuran. If this is not done, the risk of acute rejection increases due to under treatment. Similarly, because women may be concerned about the effects of these medications on the developing fetus, they may stop taking the medications and be at increased risk for rejection. Medication levels, creatinine, and creatinine clearance are commonly checked monthly in such women. The pathogenesis of this state has not been elucidated, but several mechanisms have been proposed, including increased coagulation factors, endothelial damage, and venous stasis (Virchow triad). The first is that there is an intrinsic increase in coagulability of the serum itself. Turnover time for fibrinogen is also decreased during pregnancy, and there are increased levels of fibrinopeptide A, which is cleaved from fibrinogen to make fibrin. Finally, it has been hypothesized that the placenta synthesizes a factor that decreases fibrinolysis, but there is minimal evidence for this. Another proposed source of hypercoagulability is increased exposure to subendothelial collagen as a result of increased endothelial damage during pregnancy, although no mechanism has been proposed. It has also been hypothesized that endothelial damage in the venous system during parturition increases the amount of thrombogenesis postpartum. This seems feasible, particularly as the etiology of pelvic vein thrombosis, but it does not account for the hypercoagulability throughout pregnancy. Venous stasis may also account for some of the increase in venous thromboses during and after pregnancy. Second, the uterus, as it enlarges, compresses the inferior vena cava, the iliac, and pelvic veins. Finally, the increased estrogen in pregnancy and the initial postpartum state also likely contribute to hypercoaguability. Nevertheless, these hormonal factors likely contribute to the thrombotic state of pregnancy and early postpartum. The diagnosis is usually obvious with a palpable, usually visible, venous cord that is quite tender, with local erythema and edema. On examination, patients will often have edema, local erythema, tenderness, venous distension, and a palpable cord underlying the region of pain and tenderness. When clinical suspicion is high, the patient is usually sent for noninvasive lower extremity studies with the Doppler ultrasound for confirmation of a venous obstruction. Low-molecular-weight heparin has become the preferred option because levels do not need to be checked, and it is also thought to be safer due to a lower risk of heparin-induced thrombocytopenia. When given in the first trimester, it causes warfarin embryopathy, a combination of nasal hypoplasia and skeletal abnormalities. Previously more common, ventilation/perfusion (V/Q) scanning is now used less frequently. In these posterior views, the perfusion lung scan (left) reveals segmental defects that are not matched in the normal ventilation scan (right). Enoxaparin has a long half-life and is thus sometimes switched for unfractionated heparin at 36 weeks of gestation. Arteriogram of the left pulmonary artery showing filling defects, and an unperfused segment of lung as demonstrated by the absence of contrast dye. Of note, the newer direct oral anticoagulants (antithrombin and factor Xa inhibitors) are not well studied in pregnancy and in general are not used. If levels are elevated, the fetus is at risk of developing a fetal goiter and should undergo a fetal survey at 18 to 20 weeks of gestation as well as an ultrasound in the third trimester to look for fetal goiter. Antenatal testing with serial nonstress tests is also recommended given the risk of fetal hyperthyroidism, which can be diagnosed with fetal tachycardia. Occasionally, patients with Graves disease can be tapered off of their medications. Given these issues, it is important to follow both symptoms of hyperthyroidism and the thyroid function laboratory test results closely. Lupus confers a 20-fold increase in risk for maternal mortality and elevated risk of thrombosis, infection, transfusion, cesarean section, preterm labor, and preeclampsia. In general, it also seems that patients who are without flares immediately prior to pregnancy have a better course. Medications such as aspirin and corticosteroids are continued in pregnancy, whereas cyclophosphamide and methotrexate are not. Treatment and prophylaxis with low-dose aspirin, heparin, and corticosteroids have been tried with some improvement in prognosis. Because of this risk, frequent antenatal testing is performed, usually starting at week 32. However, even on these agents, the risks are still higher than those of the baseline population. In addition, lupus flares are often accompanied by active urine sediment, whereas preeclampsia is not. Differentiating between the two conditions is important because the management for each is distinct. These flares can be quite severe and cause skin lesions, hepatosplenomegaly, and low blood counts. Such screening includes serial fetal monitoring and serial fetal echocardiogram to identify cases of potential heart block early in the process. The most commonly used substances are alcohol and cigarettes, both of which contribute to poor outcomes of pregnancy. Finally, even when infants are born with minimal effects from the intrapartum insult, substance abuse is an indicator for other social problems that may contribute to a poor environment for child rearing. The syndrome has a spectrum of increasing severity in children of women who drink more heavily (two to five drinks per day) during pregnancy. Diagnosis is made by a history of alcohol abuse in the mother combined with the constellation of infant abnormalities.
Cheap cefixime line. Complementary feed for poultry with natural essential oils for respiratory comfort / Royal Ilac.
References
- Brown AC, Audisio RA, Regitnig P (2010). Granular cell tumour of the breast. Surg Oncol 20: 97-105.
- Blay SL, Andreoli SB, Gastal FL. Chronic painful physical conditions, disturbed sleep and psychiatric morbidity: results from an elderly survey. Ann Clin Psychiatry 2007;19(3):169-74.
- Buellesfeld L, Gerckens U, Grube E. Percutaneous implantation of the fi rst repositionable aortic valve prosthesis in a patient with severe aortic stenosis. Catheter Cardiovasc Interv. 2008;71(5):579-584.
- Berger S, Lavie L. Endothelial progenitor cells in cardiovascular disease and hypoxia-potential implications to obstructive sleep apnea. Transl Res 2011; 158: 1-13.
- Folli S, Morgagni P, Roviello F, et al. Risk factors for lymph node metastases and their prognostic significance in early gastric cancer (EGC) for the italian research group for gastric cancer (IRGGC). Jpn J Clin Oncol. 2001;31:495-499.
- Kishore K, Raina A, Misra V, Jonas E. Acute verapamil toxicity in a patient with chronic toxicity: possible interaction with ceftriaxone and clindamycin. Ann Pharmacother. 1993;27:877-880.
- Simon BJ, Cushman J, Barraco R, et al. Pain management guidelines for blunt thoracic trauma. J Trauma. 2005;59:1256-1267 45.