James W. Albers, M.D., Ph.D.
- Department of Neurology
- University of Michigan
- Ann Arbor, MI
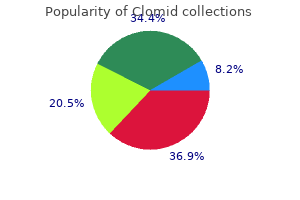
Interestingly women's health queen street york pa buy clomid 50 mg amex, recent work has identified pneumolysin menopause zits buy discount clomid 25 mg, a Pneumococcus-produced toxin pregnancy 9 weeks 100mg clomid amex, as a mediator of disease progression in mouse models of experimentally induced pulmonary fibrosis via injury of the alveolar epithelium [33] women's health clinic brighton generic 25 mg clomid fast delivery. Furthermore breast cancer 6s generic clomid 50 mg without a prescription, and perhaps more interestingly, bacterial burden at baseline predicted the rate of functional decline and risk of death. Notably, the increased risk of death associated with a high bacterial burden (hazard ratio 4. Subsequent pyrosequencing revealed increased reads of Haemophilus, Streptococcus, Neisseria and Veillonella spp. In addition, all 43 subjects had negative bacterial cultures and negative viral serology. Therefore, it is possible that the triggering virus is no longer detectable by the time the exacerbation becomes clinically evident [5]. However, many patients are still treated empirically with systemic corticosteroids, broad-spectrum antibiotics and supportive care. Baseline characteristics, including demographics, clinical characteristics and laboratory results, were similar between the two groups. However, the duration of mechanical ventilation and mortality were similar in both groups. Sirolimus, also known as rapamycin, is a macrolide compound with immunosuppressive and anti-proliferative properties. Sirolimus treatment resulted in stabilisation of lung function decline compared with placebo. Moreover, quality of life measured by the EuroQol scale improved in the sirolimus group and declined in the placebo group (0. However, in patients treated previously with sirolimus, the lung function decline resumed and paralleled that of the placebo group during the subsequent 12-month observation period in which sirolimus was withdrawn. One open-label uncontrolled trial and several case reports support the effectiveness of sirolimus in chylous effusions [54]. Most patients improved, although the recovery was slower than that generally seen with corticosteroids. However, which patients are likely to respond to macrolide therapy, and the appropriate dose and duration of treatment, are yet to be determined. Interestingly, azithromycin reduced both the extent of lung fibrosis and the restrictive lung function pattern. The reason behind the beneficial effect of azithromycin on experimentally induced pulmonary fibrosis can only be speculated, but it may relate to its ability to modulate the innate and adaptive immune response. Conversely, in the per-protocol analysis, cotrimoxazole treatment was associated with a significant improvement in EuroQol-5D-based utility (a measure of health state), a significant reduction in the percentage of patients requiring an increase in oxygen therapy and a significant reduction in all-cause mortality compared with placebo (cotrimoxazole: three out of 53; placebo: 14 out of 65; hazard ratio 0. In fact, patients receiving the "usual" immunosuppressive treatment were more likely to die if they were in the placebo group, whereas baseline immunosuppressive therapy did not have an effect on mortality in the cotrimoxazole group. However, the study had important drawbacks, including the lack of a true placebo arm and a high rate of dropout due to side-effects (mostly rash and nausea) among patients receiving cotrimoxazole (30% (28 out of 92) versus 8% (seven out of 86) in the placebo group). The primary outcome will be the time to death (all causes), lung transplant or the first nonelective hospital admission, with results expected in 2019. Conclusions Infectious agents have the potential to cause alveolar epithelial cell damage and the ability to modulate the host response to injury. The peripheral blood transcriptome identifies the presence and extent of disease in idiopathic pulmonary fibrosis. Acute exacerbation of idiopathic pulmonary fibrosis: incidence, risk factors and outcome. Idiopathic pulmonary fibrosis and high prevalence of serum antibodies to hepatitis C virus. Incidence of hepatitis C virus infection in Italian patients with idiopathic pulmonary fibrosis. Right place, right time: the evolving role of herpesvirus infection as a "second hit" in idiopathic pulmonary fibrosis. Herpes virus infection is associated with vascular remodeling and pulmonary hypertension in idiopathic pulmonary fibrosis. Idiopathic pulmonary fibrosis is strongly associated with productive infection by herpesvirus saimiri. Epithelial endoplasmic reticulum stress and apoptosis in sporadic idiopathic pulmonary fibrosis. Treating idiopathic pulmonary fibrosis with the addition of co-trimoxazole: a randomised controlled trial. Microbial communities in the respiratory tract of patients with interstitial lung disease. Streptococcus pneumoniae triggers progression of pulmonary fibrosis through pneumolysin. The role of bacteria in the pathogenesis and progression of idiopathic pulmonary fibrosis. Idiopathic pulmonary fibrosis: prognostic value of changes in physiology and six-minute-walk test. Acute exacerbation of idiopathic pulmonary fibrosis: an international working group report. Viral infections in patients with an acute exacerbation of idiopathic interstitial pneumonia. A detailed evaluation of acute respiratory decline in patients with fibrotic lung disease: aetiology and outcomes. Acute exacerbation of idiopathic pulmonary fibrosis: frequency and clinical features. Procalcitonin-guided antibiotic use in acute exacerbations of idiopathic pulmonary fibrosis. Long-term efficacy of macrolide treatment in idiopathic pulmonary fibrosis: a retrospective analysis. Sirolimus for angiomyolipoma in tuberous sclerosis complex or lymphangioleiomyomatosis. Official American Thoracic Society/Japanese Respiratory Society Clinical Practice Guidelines: Lymphangioleiomyomatosis Diagnosis and Management. Macrolides: a treatment alternative for bronchiolitis obliterans organizing pneumonia A double blind randomised placebo controlled pilot study of oral co-trimoxazole in advanced fibrotic lung disease. Spagnolo has received personal fees from Roche/Genentech, InterMune, Santhera Pharmaceuticals, Boehringer Ingelheim and Novartis. He has also received nonfinancial support from Roche/ Genentech and Boehringer Ingelheim. Over the past decade there has been a dramatic increase in the prevalence of antimicrobial resistance in respiratory pathogens, which is related primarily to antimicrobial agents in common use. This observation, in both hospital and community settings, indicates that paediatricians must be made aware of the prevalence of antimicrobial resistance and have a basic understanding of its mechanisms, implementing antimicrobial stewardship programmes to ensure that the most appropriate antimicrobials are selected when initiating therapy. It is generally agreed that well-timed and opportune therapy is essential to reduce the impact of this disease [3, 6, 7]. First, it is difficult to obtain secretions of the lower airways during the first years of life and invasive methods. Although the existence of healthy carriers of viruses has been well documented, the presence of viral pathogens in the upper respiratory tract is usually considered to be evidence of a viral aetiology [23]. The most frequent pathogens are Streptococcus pneumoniae and Mycoplasma pneumoniae, although differences have been observed in different age groups. However, a single-site study performed some years ago on a limited sample size showed that M. Regarding other types of bacteria, the main pathogens are Streptococcus agalactiae, Escherichia coli and Chlamydophila trachomatis during the first 3 months of life [7]. Another pathogen that could be detected during the first 3 months of life is Bordetella pertussis. This bacterium continues to circulate despite immunisation programmes in various countries due to the limited persistence of the immunity and the suboptimal efficacy of the acellular pertussis vaccine [34]. Regarding Haemophilus influenzae, the importance of type b (Hib) has been declining since the inclusion of Hib in the hexavalent and pentavalent formulations of vaccines that are universally recommended during the first years of life in the majority of countries [7]. Several studies over the past 20 years have shown that the various different pathogens have several similarities in terms of clinical presentation, laboratory biomarkers and chest radiography [28, 29, 35, 36]. There are different degrees of resistance, ranging from low-level to high-level resistance [38]. Low-level resistance and intermediate-level resistance were the types of resistance most frequently detected in all of the countries. It is linked to three different mechanisms: alterations in the ribosomal target site, production of inactivating enzymes, and production and use of the active efflux pump. The first of these mechanisms is the most frequent and determines high-level resistance with broad cross-resistance to macrolides, lincosamides and streptogramin B [37]. Macrolide nonsusceptibility is higher in most countries than penicillin nonsusceptibility. This result seems to indicate that there is no need to systematically change macrolide use in cases of mild to moderate disease, but other antibiotics should be prescribed if the symptoms persist or if there are signs of clinical deterioration. These cases require the use of active drugs such as glycopeptides and linezolid [6, 7]. This resistance can therefore be overcome by prescribing an aminopenicillin together with an inhibitor or a different -lactam antibiotic that is resistant to -lactamases. The rate varies, but reaches 30% in countries such as Italy, Greece, the Slovak Republic and Spain, as well as in Asian countries [52]. Thus, there has been a dramatic increase in the prevalence of antimicrobial resistance in respiratory pathogens over the past two decades, much of which is related to commonly used antimicrobial agents. These findings, in both hospital and community settings, indicate that paediatricians must be made aware of the prevalence of antimicrobial resistance and have a basic understanding of its mechanism to ensure that the most appropriate antimicrobials are selected when initiating therapy. In this regard, the implementation of antimicrobial stewardship strategies appears extremely important to preserve the activity of existing antimicrobial agents [53]. Complications include empyema, necrotising pneumonia, pneumatoceles and lung abscesses, and in the presence of these conditions long-term intravenous antibiotic administration, in some cases with anaerobic coverage, as well as pleural fluid drainage or other surgical procedures could be required [54]. Age-adjusted tachypnoea is a marker of respiratory distress, although it is not specific because it can be caused by fever, dehydration or concurrent metabolic acidosis [7]. Blood cultures have a low sensitivity and the proportion of positive blood cultures is often <10% [58, 59]. Molecular diagnostic assays of blood and pleural fluid can significantly improve the results obtained from blood cultures, primarily for S. Unlike in adults, sputum in children is often not adequate for contamination with upper respiratory secretions [7]. Similarly, urine collection for pneumococcal antigenuria is not indicated for paediatric patients as false-positive results frequently occur due to the high prevalence of nasopharyngeal pneumococcal colonisation [6, 7]. Regarding serology, its accuracy varies widely, and the need for both acute and convalescent samples limits its utility in epidemiological studies [12]. However, a close follow-up should be assured and re-evaluation considered depending on the evolution of the disease. In neonates, a combination of ampicillin (or amoxicillin) and aminoglycosides (mainly gentamicin) is the first line of treatment, and ampicillin is strongly recommended if Listeria monocytogenes is suspected. Cefotaxime is preferred to ceftriaxone, especially in hyperbilirubinaemic or pre-term newborns, because of the high avidity of ceftriaxone to the serum proteins, including albumin, which transport bilirubin [64]. The use of erythromycin is discouraged in infants <6 weeks of age because of the risk of hypertrophic pyloric stenosis [66]. It is important to note that recent studies have demonstrated that oral amoxicillin given at a high dosage. Experimental data show that macrolides are efficacious for their antimicrobial effect in addition to their immunomodulatory properties [33]. Quinolones should only be used in cases of bacterial resistance that cannot be overcome or in cases of IgE-mediated allergies to -lactams, as they are not approved for the regular treatment of children and can lead to the selection of resistant strains or to adverse events, such as Clostridium difficile colitis or tendon disorders [7]. Finally, neuraminidase inhibitors should be prescribed to paediatric patients with influenza pneumonia during the influenza season [68]. However, this evidence is weakened by the fact that the clinical criteria used may not have appropriately identified children with true bacterial pneumonia necessitating antibiotic treatment. Consequently, it is not possible to compare practices in children living in countries with high resistance rates and low resistance rates.

Finally womens health 50 safe 100mg clomid, before acute catheter placement menstruation pronunciation order clomid us, the team should consider the potential duration of therapy pregnancy tips clomid 100mg visa. If prolonged renal replacement therapy is a possibility womens health quote purchase clomid 100 mg, consideration should be made for tunneled catheter placement breast cancer zit buy cheap clomid. The clearance in intermittent hemodialysis is limited by blood flow, as the dialytic rates are greater than blood flow rates by 1. The recommended blood flow rates in children are prescribed based on weight and range from 3 to 10 mL/kg/min. Our practice is to prescribe 5 mL/kg/min of blood flow in patients greater than 10 kg. An early study by Ronco et al comparing a high dose of ultrafiltration (35 mL/kg/h) to lower dose (20 mL/kg/h) demonstrated benefit in critically ill patients. Furthermore, this population may benefit from convective therapies to allow for improved middle molecule clearance. Furthermore, studies in critically ill patients have shown that the delivered dose may be up to 30% lower than was prescribed. Higher clearances can result in lower drug levels, and as a result many medications need increased dosing. Similarly, higher levels of clearance result in increased clearance of amino acids and can negatively impact the nutritional status. The typical blood volume in infants <10 kg is 80 mL/kg, and 70 mL/ kg in larger children. To prevent hypothermia, the use of patient warmers, heating pads applied to circuit tubing or manufacturer-specific blood warmers, and control of the room temperature should be employed. There are a number of commercially available solutions that can serve as dialysis or replacement solutions (Table 86. Previously, when choosing solutions one could choose from those buffered primarily with lactate or with bicarbonate. Several studies have since demonstrated that bicarbonate-based solutions are superior. It is worth noting that a number of these solutions continue to contain small amounts of lactate. Commercially available solutions contain varying amounts of sodium, potassium, glucose, magnesium, calcium, and phosphorous. However, with the phosphorusbased solutions, calcium must be infused and with the calcium-based solution phosphorus must be infused to the patient. In the appropriate clinical scenario, specific adjustments to solutions or types of solutions may be used to achieve the goals of care. In hyperosmolar states, a sodium concentration of 150 mEq/L or 160 mEq/L may be utilized to prevent rapid osmotic shifts. Similarly high sodium concentrations may be utilized as part of a neuroprotective strategy in the right clinical scenario. This can be exacerbated by low blood flow 1004 Continuous Renal Replacement Therapy in Pediatric Patients rates, turbulent blood flow, and high hematocrits. In adult studies, citrate anticoagulation has been shown to be superior at prolonged filter life with less bleeding complications. This study showed that there was no difference in circuit life in those receiving heparin (44. This study also suggested that there were fewer bleeding complications in children receiving citrate anticoagulation. The decision to perform anticoagulation in the most critically ill children with underlying sepsis and disseminated intravascular coagulopathy or liver failure warrants further discussion. Historically, the approach of no anticoagulation has been utilized in these patient populations. As a result, we discourage the approach of using no anticoagulation in these patients and suggest modifying protocols in these patients. Heparin anticoagulation has been used in dialytic therapies for children for decades. The advantage of heparin is the historical use and familiarity by many nephrologists. The disadvantage of heparin is that it is infused into the patient and can be associated with anticoagulation of the patient. In many patients with multiorgan system failure requiring renal replacement therapy, systemic heparinization may be a detriment and should be avoided secondary to increased risk of bleeding. Citrate-based regional anticoagulation regimens rely on the ability of citrate to chelate ionized calcium, thus removing a critical component for activation of both coagulation cascades and platelets. The majority of calcium-citrate complexes are dialyzed through the filter during dialysis and lost in the effluent. In larger triple-lumen catheters, calcium can be infused in the most distal lumen but should be done cautiously. The second process is to deliver calcium back into the patient to target a physiologic level between 1. Protocols are then used to adjust citrate and calcium infusion rates based on a sliding scale. Regional citrate anticoagulation does have the potential for metabolic complications, including metabolic alkalosis, hypernatremia, hypocalcemia, hyperglycemia, and citrate toxicity. Citrate anticoagulation may result in metabolic alkalosis as a result of the metabolism of citrate to bicarbonate. This is of particular concern when dialysate and replacement solutions with higher bicarbonate solutions are utilized. This occurs when the delivery of citrate exceeds the clearance (dialysis and metabolism) of excess citrate and is typified by low ionized calcium, elevated total serum calcium, and an anion gap acidosis or alkalosis. Citrate toxicity can be monitored by monitoring the total serum calcium to ionized calcium ratio and occurs at a ratio of 2. Patients at the highest risk for the development of these complications include those with impairment of the organ systems that metabolize citrate (liver and muscle). Regional citrate anticoagulation can be safely performed in children with liver failure by using modified protocols that typically start at a lower citrate infusion rate. When citrate anticoagulation is used in children, particular care must be paid to infants less than 10 kg. As a result, in protocols where the citrate is dosed based on blood flow, these children receive higher citrate infusion rates by weight than older children. Membrane and Filter When selecting the appropriate filter for pediatric patients, one needs to take into account the filter size and biocompatibility. As a rule, the filters are permeable to nonprotein-bound solutes with a relative molecular mass less than 40,000 (although this is dependent on the filter fibers of the specific hemofilter). When considering the filter to utilize one must take into account the risks and benefits of each filter. The polysulfone-based filters are not associated with the bradykinin release, but are not available in the appropriate infant sizes in the United States. This membrane reaction is pH dependent and potentiated by angiotensin-converting enzyme inhibitors. In smaller patients who require blood priming, this presents as a potential cause of hypotension because most blood-bank blood has a pH of about 6. One approach to this reaction is to bypass the hemofilter by giving the blood postfilter, synchronizing a saline prime of the filter, and a bicarbonate infusion to the filter (30 mEq over 15 minutes). This, along with judicious use of bicarbonate boluses to the filter during startup, has allowed for the safe use of this membrane. Patient nutrition should be tailored to meet their overall needs with the aim of promoting an anabolic state. It is clear that improved nutrition is associated with decreased morbidity in such patients. Continuous Renal Replacement Therapy in Pediatric Patients 1007 Inborn Errors of Metabolism Hyperammonemia represents a true emergency and warrants prompt treatment. This regimen may provide benefit by avoiding hypotension that may be associated with hemodialysis runs in critically ill neonates. In general, we have found doubling the infusion rate to be adequate and should involve consultation with pharmacists and geneticists. One concern with utilizing the in-line filter is that fluid removal is frequently measured by using an infusion device. Renal replacement therapy in critically ill patients receiving extracorporeal membrane oxygenation. This comprehensve review provides an overview of the management of hyperammonemia with renal replacement therapy. Pediatric convective hemofiltration: Normocarb replacement fluid and citrate anticoagulation. This comprehensve review provides an overview of pediatric continuous renal replacement therapy in children. Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. This comprehensve review provides an overview into important considerations to take into account when considering modality choice for renal replacement therapy in children. Similar to the adult population, cardiovascular disease is the leading cause of mortality in children with kidney disease, and abnormal mineral metabolism, bone disease, and its therapies are closely linked to cardiovascular pathology. Thus, low levels of calcitriol may allow parathyroid cells to proliferate whereas the administration of calcitriol may suppress proliferation of parathyroid cells. These assays are not currently available for clinical practice, however, and their value as predictors of the different subtypes of renal osteodystrophy as well as the response to therapeutic interventions remains to be defined. Traditionally, such lesions have been characterized according to alterations in bone turnover, ranging from high bone turnover (secondary hyperparathyroidism, osteitis fibrosa) to lesions of low bone turnover (adynamic bone disease and osteomalacia). This condition may occur, especially in children treated with maintenance dialysis, because of overaggressive therapy with active vitamin D sterols and calcium salts. In addition to the increased risk for fractures and vascular calcifications that is observed in adults with adyamic bone, this form of bone disease in children treated with dialysis is associated with a further decline in growth. Increases in unmineralized bone (osteoid) in conjunction with delayed rates of mineral deposition are common. Defective mineralization that is associated with low to normal bone turnover is termed "osteomalacia. Defective mineralization in combination with increased bone formation rates is termed "mixed uremic osteodystrophy" and is characterized by wide osteoid seams, prolonged mineralization times, bone marrow fibrosis, and increased bone formation rates. Phosphate depletion, as may occur with frequent dialysis, may also result in osteomalacia. However, bone volume may also be low (termed "osteoporosis"), particularly in individuals with underlying age-related bone loss or in those treated with corticosteroids. In contrast to the calcified atherosclerotic plaques that develop in the vascular intima of aging individuals with normal kidney function, uremia facilitates calcification of the tunica media. This form of calcification is associated with decreased distensibility of blood vessels, causing a rigid "lead pipe" pathology that is associated with increased risk for congestive heart failure. In patients with compromised renal function, the entire smooth muscle layer surrounding arteries may be replaced not only by calcium deposits but by tissue that resembles bone. Boys, younger patients, and those with prior renal transplants are at greatest risk for growth failure. Acidosis has been linked to delayed linear growth in patients with renal tubular acidosis and normal renal function, and its correction often leads to acceleration in growth velocity. Treatment for secondary hyperparathyroidism with large, intermittent doses of calcitriol and calcium-based phosphate binders has been shown to reduce bone formation and suppress osteoblastic activity in both adults and children. Skeletal Deformities and Pain Genu valgum is the most common skeletal deformity in pediatric patients. Radiographic features associated with vitamin D deficiency include metaphyseal widening of the wrist and ankle, craniotabes, and rachitic rosary. The prevalence of slipped capital femoral epiphysis has declined over the past two decades because of better control of 1016 Prevention and Treatment of Bone Disease in Pediatric Dialysis Patients secondary hyperparathyroidism. Myopathy Muscle involvement can range from muscle wasting, diffuse pain, weakness, and numbness to contracture of the extremities. The exact etiology for the myopathy described in renal failure is still unclear, but rapid fluid removal, electrolyte imbalance, low calcitriol, and the presence of calcific uremic arteriolopathy or calciphylaxis may contribute. There are no diagnostic tests available, and muscle biopsy may show severe atrophy without inflammation or the presence of calcification of small and medium-sized vessels. Calcium-rich foods such as dairy products, unfortunately, also are high in phosphorus. Prevention and Treatment of Bone Disease in Pediatric Dialysis Patients 1017 consumption of calcium to meet daily needs is accompanied by excessive intake of phosphorus, which cannot be excreted in the face of renal failure. The development of hyperphosphatemia occurs in the vast majority of patients with advanced renal insufficiency.
Alternate methods of anticoagulation for dialysis-dependent patients with heparin-induced thrombocytopenia breast cancer 5k san diego discount clomid 50mg line. Review of the prevalence women's health group tallmadge ohio 25mg clomid visa, diagnosis pregnancy jewelry buy cheap clomid 25 mg on line, and treatment data regarding heparin-induced thrombocytopenia women's health edmonton clomid 25mg with visa. Use and safety of unfractionated heparin for anticoagulation during maintenance hemodialysis women's health yuma az buy 100 mg clomid free shipping. Case presentation and comprehensive review of different anticoagulation strategies for hemodialysis, with emphasis on heparin, its pharmacology, dosage, and complications. Randomized, clinical trial comparison of trisodium citrate 30 percent and heparin as catheter-locking solution in hemodialysis patients. This prospective study found that the use of a trisodium citrate catheter locking solution reduced the incidence of catheter-related bacteremia and was not associated with any untoward metabolic consequences compared to standard heparin lock. Regional citrate versus heparin anticoagulation for continuous renal replacement therapy: a meta-analysis of randomized controlled trials. The interest in home hemodialysis has been increasing over the past years because of its flexibility and benefits (which will be further discussed in the following section). It is currently experiencing a resurgence in several countries, especially with the interest in more frequent or intensive hemodialysis. In fact, there was a 5-fold increase in patients undergoing home hemodialysis in 2012 (n =7923) versus in 2002 (n = 1563). Basis for Home Hemodialysis Home hemodialysis offers several benefits as compared to conventional facility based hemodialysis. These include improvements in patient outcomes (Blagg et al, 2006), increased freedom of time, cost reduction, as well as an improved quality of life. Improvements in patient outcome with more frequent or intensive home hemodialysis include improved survival (Weinhandl et al, 2012), blood pressure control (Chan et al, 2003), left ventricular geometry (Culleton et al, 2007), phosphate control and mineral metabolism (Walsh et al, 2010), quality of sleep (Hanly et al, 2001), and fertility (Barua et al, 2008). Requirements There are several prerequisites that need to be addressed before commencing on a home hemodialysis program. A home visit should be conducted prior to further discussion of home dialysis to determine its feasibility and assess the necessary modifications. The availability of a checklist for the home visit may facilitate the process (Table 15. Legal the local legal requirements regarding water supply, as well as land and housing, should be established to ascertain if home hemodialysis is feasible. There should be no legal restriction to the use of the building for the purpose of home hemodialysis. In addition, legal requirements concerning waste disposal, sewage, and electrical supply should also be established before the consideration of home hemodialysis. Consideration should be given toward specific policies regarding potentially biohazardous waste. A unit policy should ideally be in place to decide who is financially responsible for the needed modifications to the home that may be necessary in terms of plumbing and/or electrical renovations. Water Preparation, Standards, and Plumbing Home hemodialysis, as compared to conventional in-center hemodialysis, is potentially a more water-intensive procedure, with larger volumes of water being necessary to reconstitute the dialysate (except for the mobile platform). The total dialysate volume can range between 110 and 150 L for a 6- to 8-hour session of dialysis, as compared to 120 L for a typical conventional session. The water supply can come from various sources, for example, municipal water, feed water. It is important for a full chemical analysis of the water for dialysis to be conducted to determine the degree of water purification necessary. The plumbing system modifications should also take into consideration the level in the home in which the dialysis is done. Should dialysis take place on higher floors, additional components, for example, pump systems and feeder tanks, may be needed to provide the necessary water pressure for the reverse osmosis unit and dialysis machine to function properly. Depending on the local water conditions and regulations, other modifications like backflow preventers and blending devices may also be necessary. Electrical Considerations Including Backup Power Supply A stable power supply is necessary to conduct home hemodialysis. There should also be an overcurrent device installed at the service panel board equipped with a 20-ampere fuse. The dialysis machine should also be connected to a separate branch circuit that does not supply any other outlets. For locations that may experience regular power failures, a backup power supply with its accompanying equipment is recommended. The power supply should be compatible with the dialysis equipment, and it may be necessary for an electrician to review for an outlet for the machine with a dedicated circuit to the circuit breaker. It is important to take into consideration measures to manage hemodialysis in the event of power failure, for example, manual wind-back functions of the machine. Lastly, it is essential to establish the local electricity safety regulations and adhere to them. Dialysis Machine Choice and Other Equipment There are different dialysis machines currently available for home hemodialysis. Some offer the advantage of mobility; however, any machine in general is able to provide effective and good home dialysis. In general, a home dialysis machine should be easy to operate and understand, as this facilitates the learning process for the patient and/or the caregiver. The choice of dialysis machine would also determine the ease of dialysis fluid preparation. Some machines require water filtration systems, while others come with pre-packaged dialysate, or are able to generate on-line dialysis solutions. To prescribe dialysis with this system, one would need to decide on the following parameters: i. Frequency of dialysis per week, as well as the target spKt/V (per session as well as per week) ii. The PureFlow system allows ultrapure product water to be produced from tap water, which is then mixed with the sterile concentrate to produce dialysate solution. This allows for an adjustable headrest that will allow the patient to be comfortable sitting up for the entire duration of the dialysis process and also allows the patient to recline. This should also allow the patient to assume a supine position quickly in the event that symptomatic hypotension occurs. Space Considerations and Siting of Dialysis Machine Patients will need storage space, for example, a cabinet/closet to store their dialysis equipment. The space considerations will also determine the choice of dialysis machine and vice versa. The conventional dialysis platforms will generally be larger and less mobile, whereas users of mobile batch dialysis equipment. The dialysis room should allow for the dialysis session to be conducted safely and should also allow for maintenance to be conducted regularly. It should also be uncluttered and ideally have furnishing that is easy to maintain. Clearances reflect median weekly values and are model-based calculations for provided weekly treatment times. Does the patient want to conduct dialysis privately or in the same room as family members If so, the bedroom would be a suitable choice for locating the dialysis machine v. Proximity to a telephone is essential Storage space is also necessary to house the supplies needed for the dialysis treatment. Once patients become familiar with the amount of supplies they need during a particular time period, they may be able to adjust their delivery schedule to better suit their space and storage requirements. The choice of the dialysis location should also take into consideration the space necessary for the water treatment unit. This area should ideally have waterresistant flooring in case of leaks and also have sufficient servicing and drainage access. The noise generated from the reverse osmosis unit will also need to be taken into consideration for locating the unit. The patient may also consider placing a protective vinyl sheet or a tray under the dialysis machine and water treatment unit as an additional safety measure in case of a water leak. Hygiene and Noise the surroundings in which the dialysis is conducted should be clean so as to prevent infections from occurring during home hemodialysis. Proper hand hygiene is also of importance, and proper handwashing techniques should always be adhered to , including the use of soap or alcohol rubs. In general, pets should not be allowed during the dialysis process, as they may pose both a hygiene and safety problem. Even if the pet is supervised, the pet should be kept out of the room during treatment initiation. These hygiene requirements should extend to both the patient as well as any family member who may be assisting with the dialysis process. The participation of the family should also be assessed as part of the home visit prior to the consideration of home hemodialysis. Safety All dialysis machines should be equipped with monitors to detect exact arterial and venous pressures, with settings to narrow alarm ranges. The alarm type is usually sound based but may need to be light based in special circumstances. Leak detectors should be placed around the vascular access site, under the dialysis machine, as well as the water treatment system, to detect either blood, dialysate, or water leaks. Flashlights should be kept within easy reach so that the patient has an alternative light source in the event of a power failure to allow termination of treatment. Twenty-four-hour access to the supporting dialysis care facility or technical support should be available in the event of emergencies. The relevant contact numbers for the dialysis unit and technical support should also be within easy access in the dialysis room. Medical Staff and Technical Support Machine breakdowns may occur, for example, due to electrical or water problems. The dialysis unit supporting the patient should also be informed if a machine breakdown occurs so that the appropriate advice can be given and the technical staff directed to the home to service the machine. Disposal of Waste For most patients, disposal of the effluent via the sewage system provides the best option. Appropriate drainage systems should be taken into consideration during the planning process. All sharps should be collected in a dedicated sharps container for proper disposal. The other waste can be disposed of with the general waste, but should be double-bagged. Recycling of plastic waste can also be considered, given that the dialysis process has a high amount of plastic waste production. The patient Home Preparation and Installation for Home Hemodialysis 213 should check with the dialysis unit providing the dialysis support regarding any extra waste disposal requirements. Conclusion Medical and technical support is essential for the development of a home hemodialysis program and training. With proper preparation, the establishment of home hemodialysis can be facilitated safely and efficiently and allow the patient to benefit from this treatment modality. This article describes how home hemodialysis may allow for improved fertility, which may be an important consideration for female patients in the childbearing age group. Comparison of survival between short-daily hemodialysis and conventional hemodialysis using the standardized mortality ratio. This article describes improved survival for patients on short daily dialysis compared with conventional hemodialysis. Short-term blood pressure, noradrenergic, and vascular effects of nocturnal home hemodialysis. Effect of frequent nocturnal hemodialysis vs conventional hemodialysis on left ventricular mass and quality of life: a randomized controlled trial. This article provides an insight into how nocturnal hemodialysis improves left ventricular mass, an important predictor of cardiovascular disease and mortality. This review article provides an overview of the benefits, risks, as well as the possible target population for intensified home hemodialysis. The cost-effectiveness of contemporary home haemodialysis modalities compared with facility haemodialysis: a systematic review of full economic evaluations. This article compares home hemodialysis and facility-based hemodialysis and reviews the economic benefits of home hemodialysis. The effects of nocturnal compared with conventional hemodialysis on mineral metabolism: a randomized-controlled trial. This article describes how nocturnal dialysis is associated with improvements in phosphate control, as well as reducing the need for phosphate binders. Survival in daily home hemodialysis and matched thrice-weekly in-center hemodialysis patients. This article describes the improved survival for patients on daily home hemodialysis as compared to patients on thrice-weekly in-centre hemodialysis. Although the emphasis during the early years was mainly on optimizing hydraulics and mechanical aspects, the current development goes far beyond filling the abdomen and draining the dialysate. Modern cyclers are highly integrated devices that are designed to communicate and exchange data with other devices.
Further efforts are needed to define the optimal approach to thyroid functional testing in dialysis patients women's health clinic rock springs wy buy generic clomid online. Thyroid Functional Disease and Outcomes in Dialysis Patients the cardiovascular system is a major target of thyroid hormone action menstrual flexible cups purchase cheap clomid line. Thyroid hormone has both genomic and nongenomic effects on a number of cardiac structural and regulatory proteins menstrual questions answered buy discount clomid 50 mg online, membrane ion channels menstrual clots purchase 50mg clomid amex, and cell surface receptors women's health center new prague mn purchase clomid with amex. As a result, thyroid hormone deficiency has been associated with a diverse range of cardiovascular complications in the general population, including impaired systolic and diastolic function, endothelial dysfunction, dyslipidemia, accelerated atherosclerosis, vascular calcification, and conduction abnormalities leading to malignant arrhythmias (Table 57. In the general population, although few studies have examined the prognostic implications of overt hypothyroidism, there have been many studies examining the association between subclinical hypothyroidism and mortality. Findings across studies have been mixed, likely due to heterogeneous cohort characteristics, alternative definitions of hypothyroidism, and variable adjustment for confounders. These findings may have a bearing on dialysis patients who have a high prevalence of structural heart disease and exceedingly high cardiovascular mortality risk. Low Triiodothyronine and Outcomes As cardiac myocytes are unable to locally generate T3 from its T4 prohormone, there has been particular interest in T3 as the biologically relevant thyroid hormone metric for cardiovascular endpoints. It was previously hypothesized that thyroid hormone deficiency is a physiologic adaptation and a means to conserve metabolism in dialysis patients in whom hypercatabolism, malnutrition, and dialytic protein and amino acid losses are frequently observed. Furthermore, some but not all studies have found that low T3 measured at a single point in time is associated with higher mortality in dialysis patients (Table 57. In a study of 210 hemodialysis patients who underwent T3 measurement at baseline and 3-month follow-up, patients with persistently low T3 had a 2. Yet in a subsequent study of 1000 diabetic hemodialysis patients from the Die Deutsche Diabetes Dialyse Studie (4D Study), subclinical hypothyroidism examined separately or in conjunction with overt hypothyroidism was not associated with sudden cardiac death, cardiovascular events, or all-cause mortality; however, the low prevalence of hypothyroidism (1. Treatment Considerations the 2012 United States Renal Data System Annual Data Report indicates that exogenous thyroid replacement therapy in the form of levothyroxine is the 4th and 12th most commonly prescribed medication among predialysis and dialysisdependent Medicare Part D recipients, respectively. In the general population, treatment has been shown to reverse diastolic dysfunction, dyslipidemia, endothelial dysfunction, and atherosclerosis. Low T3 syndrome in peritoneal dialysis: metabolic adaptation, marker of illness, or mortality mediator To date, few studies have examined exogenous thyroid hormone replacement in hypothyroid dialysis patients. In the general population, exogenous thyroid hormone treatment of hypothyroidism with T3 alone or in combination with T4 is typically not advised given wide fluctuations in serum T3 levels that may occur because of its rapid gastrointestinal absorption and short half-life (1 day). Although the investigators indicated that treated patients did not develop clinical symptoms of hyperthyroidism, mean thyroid functional test levels rose to thyrotoxicosis ranges. Given the long 1-week half-life of levothyroxine, steady state is typically achieved 6 weeks after initiation of therapy or dose adjustment. Levothyroxine has a narrow toxic-to-therapeutic window, and overreplacement or unwarranted treatment may lead to angina, myocardial infarction, atrial fibrillation, increased protein catabolism, and accelerated bone loss. Understanding the impact of thyroid hormone treatment on cardiovascular outcomes and mortality may shed greater light into the causal implications of hypothyroidism in dialysis patients. This article reviews mechanisms underlying the association between thyroid functional disease and changes in kidneyfunctionandstructure. Clinical and biochemical implications of low thyroid hormone levels (total and free forms) in euthyroid patients with chronic kidney disease. Thyroid Function, Cardiovascular Events, and Mortality in Diabetic Hemodialysis Patients. Subclinical hypothyroidism is linked to micro-inflammation and predicts death in continuous ambulatory peritoneal dialysis. Are low concentrations of serum triiodothyronine a good marker for long-term mortality in hemodialysis patients Thyroid hormone abnormalities in haemodialyzed patients: low triiodothyronine as well as high reverse triiodothyronine are associated with increased mortality. Correlations of free thyroid hormones measured by tandem mass spectrometry and immunoassay with thyroid-stimulating hormone across 4 patient populations. Clinical implications of subclinical hypothyroidism in continuous ambulatory peritoneal dialysis patients. This is a study demonstrating the association between subclinical hypothyroidism and impaired left ventricular function. Isotopic renal function studies in severe hypothyroidism and after thyroid hormone replacement therapy. Serum and peritoneal dialysate thyroid hormone levels in patients on continuous ambulatory peritoneal dialysis. Consistent reversible elevations of serum creatinine levels in severe hypothyroidism. This book chapter discusses the approach to diagnosing hypothyroidism, including biochemical testing, in the generalpopulation. Thyroid dysfunction and nodular goiter in hemodialysis and peritoneal dialysis patients. Abnormal thyroid function predicts mortality in patients receiving long-term peritoneal dialysis: a case-controlled longitudinal study. This study describes the association between various thyroid function abnormalities and mortality in peritoneal dialysispatients. Increased prevalence of subclinical and clinical hypothyroidism in persons with chronic kidney disease. This is one of the early studies demonstrating a graded association between hypothyroidism and incrementally impairedkidneyfunction. Nonthyroidal illness: a risk factor for coronary calcification and arterial stiffness in patients undergoing peritoneal dialysis Baseline levels and trimestral variation of triiodothyronine and thyroxine and their association with mortality in maintenance hemodialysis patients. Prevalence of clinical and subclinical thyroid disease in a peritoneal dialysis population. Nutritional state alters the association between free triiodothyronine levels and mortality in hemodialysis patients. Levothyroxine treatment of subclinical hypothyroidism, fatal and nonfatal cardiovascular events, and mortality. Thyroid functional disease: an under-recognized cardiovascular risk factor in kidney disease patients. The relationship between thyroid function and estimated glomerular filtration rate in patients with chronic kidney disease. Association of thyroid functional disease with mortality in a national cohort of incident hemodialysis patients. Comparison between serum free triiodothyronine levels and body fluid distribution in hemodialysis patients. This study reports an association between low triiodothyronine levels and interstitial edema in hemodialysis patients. Prevalence of subclinical hypothyroidism in patients with end-stage renal disease and the role of serum albumin: a cross-sectional study from South India. Preservation of renal function by thyroid hormone replacement therapy in chronic kidney disease patients with subclinical hypothyroidism. Measuring serum thyroid-stimulating hormone, thyroid hormones, thyroid-directed antibodies, and transport proteins. The prevalence of low triiodothyronine according to the stage of chronic kidney disease in subjects with a normal thyroid-stimulating hormone. Associations of triiodothyronine levels with carotid atherosclerosis and arterial stiffness in hemodialysis patients. The association between thyroid hormones and arterial stiffness in peritoneal dialysis patients. Correction of metabolic acidosis improves thyroid and growth hormone axes in haemodialysis patients. Thyroid hormone levels and incident chronic kidney disease in euthyroid individuals: the Kangbuk Samsung Health Study. This large observational study reports the association between elevated thyrotropin levels and incident chronic kidneydisease. Common disturbances include erectile dysfunction in men, menstrual abnormalities in women, and decreased libido and fertility in both sexes. These abnormalities are primarily organic in nature and are related to uremia as well as the other comorbid conditions that frequently occur in the chronic kidney failure patient. Fatigue and psychosocial factors related to the presence of a chronic disease are also contributory factors. Sexual Dysfunction in Uremic Men Erectile dysfunction is one of the most common manifestations of sexual dysfunction in men with chronic kidney disease. In addition to abnormalities in blood flow and neural input to the penis, abnormalities in the pituitary-gonadal axis play a prominent role in the genesis of this disorder. Chronic kidney disease is associated with impaired spermatogenesis and testicular damage, often leading to infertility. Semen analysis typically shows a decreased volume of ejaculate, either low or complete azoospermia, and a low percentage of motility. Histologic findings include damage to the seminiferous tubules and interstitial fibrosis and calcifications in the epididymis and corpora cavernosa. The factors responsible for testicular damage in uremia are not well understood but chronic exposure to phthalates in dialysis tubing may play a role. The endocrine function of the testes is also abnormal in chronic kidney disease (Table 58. Low serum testosterone levels are associated with increased mortality in dialysis patients. Elevated plasma prolactin levels are commonly found in dialyzed men primarily as a result of increased production and to a lesser extent reduced metabolic clearance. Both increased parathyroid hormone and zinc deficiency have been implicated as playing a contributory role in the increased levels. This problem most often develops during the initial months of dialysis and then tends to regress as dialysis continues. Although elevated prolactin levels and an increased estrogen-toandrogen ratio seem attractive possibilities, most data fail to support a primary role for abnormal hormonal function. Alternatively, a mechanism similar to that responsible for gynecomastia following refeeding of malnourished patients may be involved. In addition, the psychological effects of a chronic illness and lifestyle limitations may negatively impact sexual function. A history of normal erectile function prior to the development of kidney failure is suggestive of a secondary cause of impotence. Symptoms or physical findings of a neuropathy as in a patient with a neurogenic bladder would be particularly suggestive of a neurologic etiology. Similarly, symptoms or signs of peripheral vascular disease may be a clue to the presence of vascular obstruction to penile blood flow. One should look for the presence of secondary sexual characteristics, such as facial, axillary, and pubic hair. The lack of these findings and the presence of small soft testicles suggest primary or secondary hypogonadism as the cause of the impotence. Neurogenic and vascular causes are more likely to be associated with normal-sized testicles. Even when the history and physical examination point to a specific abnormality, one must also consider that an individual patient may have more than one factor responsible for the erectile dysfunction, and other causes may need to be ultimately evaluated. Antihypertensive medications are common offenders, with centrally acting agents and beta-blockers being the most commonly implicated agents in causing impotence. The angiotensin-converting enzyme inhibitors or angiotensin receptor blockers are associated with a lower incidence of impotence and represent a useful alternative in kidney failure patients with hypertension. Other drugs commonly implicated include cimetidine, phenothiazines, tricyclic antidepressants, and metoclopramide. If the history and physical examination reveal no obvious cause, then a psychological cause of erectile dysfunction may need to be considered. The basis for this test is that during the rapid eye movement stage of sleep, males normally have an erection. The assumption is that a man with a psychological cause of impotence would still experience erections while asleep whereas the absence of an adequate erection would make an organic cause more likely. If a patient is found to have nocturnal erections, then psychological testing and evaluation are indicated. There are tests that may aid the discrimination between a neurogenic and vascular cause of impotence. Tests used to exclude a vascular etiology of impotence include Doppler studies to measure penile blood flow, measurement of penile blood pressure, and penile pulse palpation. Neurogenic impotence is suggested by detecting a prolonged latency time of the bulbocavernous reflex or confirming the presence of a neurogenic bladder. With the availability of sildenafil (see below) to use as a therapeutic trial, such tests are generally reserved for nonresponders who may eventually be considered for surgical placement of a penile prosthesis. As discussed previously, hormonal abnormalities are frequently detected in chronic kidney failure patients. It should be noted that only a small percentage of uremic patients will have prolactin levels greater than 100 ng/mL. Administration of recombinant human erythropoietin has been shown to enhance sexual function likely through the associated improvement in well-being that comes with the correction of anemia although improvement in the pituitary gonadal feedback mechanism has also been reported.

Uremic toxins womens health specialist appleton wi purchase clomid american express, low-grade hemolysis due to shearing by dialysis needles women's health clinic northbridge perth buy generic clomid 25mg on-line, and other factors have all been implicated women's health center houston order clomid 100 mg with mastercard. Shortened half-life (eg breast cancer genetic testing purchase generic clomid online, due to hemolysis) can be compensated for in nonuremic individuals through accelerated erythrocyte production women's health center gretna buy clomid 100mg without a prescription. The etiology is unclear, perhaps because of atherosclerosis, infection, uremic toxins, or other factors yet to be identified. One of the important recent advances in science has been the identification of hepcidin, the key regulator of iron homeostasis. The net effect is to block iron entry into the circulation both by limiting intestinal iron absorption and by greatly reducing movement into the circulation of iron held in storage tissue. In the classic anemia of chronic disease, better termed anemia of inflammation, hepcidin lowers iron in the circulation, thereby limiting iron availability for red cell production. The same occurs frequently in dialysis patients, where the chronic inflammatory state contributes to anemia. Iron is sequestered in storage tissues, raising serum ferritin, and reduced in the circulation, lowering transferrin saturation. This discordant combination of a relatively high serum ferritin in combination with normal or reduced transferrin saturation is a common finding in dialysis patients. Increases in serum hepcidin and reduced availability of iron for erythropoiesis play important roles. Hemoglobin concentrations often decrease in chronic infections but may decline in acute infections as well. One interesting source of occult infection seen in dialysis patients could be their previously used but currently nonfunctioning arteriovenous grafts. The best proof of this relationship may be that after parathyroidectomy, anemia tends to improve whether hyperparathyroidism was primary or secondary to other factors. The decision on whether parathyroidectomy 574 Anemia in Patients With End-Stage Kidney Disease is necessary should not be based on anemia, but rather on more traditional mineral and bone parameters. Medical treatment of hyperparathyroidism does appear to have a beneficial effect on anemia. Goicoechea et al treated 28 patients with hyperparathyroidism with intravenous activated vitamin D therapy. After ruling out iron deficiency and other issues discussed above, pathologic causes of reduced red cell production, sequestration, and hemolysis should be considered. Erythrocyte production defects can result from folic acid or vitamin B12 deficiency, among many other causes. An epidemic of pure red cell aplasia due to antierythropoietin antibodies took place primarily in Europe in the late 1990s. Hemolytic conditions can be acute during hemodialysis, but chronic hemolytic conditions should be considered when unexplained anemia is present and suggestive clinical signs are present. Both benefits and risks of red blood cell transfusions should also be considered in this patient population. The clinical benefit of red cell transfusion primarily includes improvement in symptoms related to anemia. Although rare, transmission of infections remains a concern with red blood transfusion. Another important concern, although disputed, is the risk of allosensitization and resulting diminished subsequent ability to receive a kidney transplantation. For the abovementioned reasons, red blood cell transfusions should be used prudently in this population. Intravenous calcitriol improves anaemia and reduces the need for erythropoietin in haemodialysis patients. A clinical trial demonstrating that intravenous calcitriol therapy improves anemia as it lowers parathyroid hormone levels. An important observation of iron accumulation in the liver of hemodialysis patients. It has been controversial whether dialysis patients absorb iron normally; this may be the most important study on the subject, concluding that iron absorption is unimpaired. Among men, a significant reduction in hemoglobin (Hgb) is seen when calculated creatinine clearance is <70 mL/min and among women when calculated creatinine clearance is <50 mL/ min. Although gender-based thresholds exist for the definition of anemia in the general population (<12 g/dL in women and <13. For unclear reasons, African Americans are more often anemic compared with other racial/ethnic groups. Approximately 40% of women and 20% men have transferrin saturation of <20% irrespective of calculated creatinine clearance. Pathophysiology Systemic Iron Homeostasis Iron is a micronutrient that is ubiquitous and indispensable for life. In order to safeguard against its highly reactive forms, iron is distributed in three distinct pools: functional, storage, and transit. Unlike most ions and minerals, the concentration of which are regulated by the kidney, the regulation of iron content in the body occurs in the small intestine and there is no significant excretion of iron by the kidneys. The link between the functional and storage pool of iron is the transport or transit pool. In contrast to the other pools, the transit pool comprises only a tiny fraction of total body iron (3 mg or 0. The high turnover of this pool provides the much needed iron to the cells for hematopoiesis. It also ensures that free iron, which is highly reactive and capable of damaging various molecules, does not circulate free in blood. The transferrin molecule saturated with iron is important for the delivery of iron to cells expressing transferrin receptors. Thus, this transport pool is crucial for the successful hemoglobinization of erythrocytes. The liberation of nonheme iron from food and its solubilization is aided by the acidic pH of the stomach. Iron absorption is maximal in the duodenum, less in the jejunum, and least in the ileum. Regulation of intestinal iron absorption is crucial for prevention of iron overload. The expression of Dcytb enzyme is regulated by iron deficiency and follows the expected gradient from duodenum to ileum. Once inside the cell, iron can be either stored as ferritin and thus lost from the body when the enterocyte sheds from the mucosa or iron can be exported to the circulation. The resulting endosome is acidified to release iron in the cell and transferrin, devoid of iron, called apotransferrin, is recycled back to the circulation. Iron thus released can be either stored as ferritin in the cytoplasm or exported to be bound to transferrin. Additionally, there is some evidence that heme-iron could also be exported directly by the Bcrp/Abcg2 transporter. These heme-efflux proteins could potentially play a role in preventing toxicity due to heme overload. The understanding of the iron cycle control has been enhanced by elucidation of the roles of its key control elements. Ferroportin, the transporter of iron from cells to the bloodstream, is also the receptor for hepcidin. The binding of hepcidin to ferroportin leads to its internalization and subsequent degradation. This decreases the ability of the cell to export iron to be available for binding to transferrin. Hepcidin production rises in inflammatory and iron overload states, and consequently the gut absorption of iron is suppressed. Furthermore, the release of iron from the reticuloendothelial system is also impaired when hepcidin concentrations are increased. These emerging data on the important role of hepcidin in iron biology shift the focus of regulation of iron absorption from the gut (and iron release from the reticuloendothelial system) to the liver. Importantly, replete and/or overloaded iron stores and inflammation increase hepcidin levels. Increased intensity of erythropoiesis, hypoxia and certain endocrine factors, and steroids and growth factors suppress hepcidin expression. Iron-restricted erythropoiesis can be due to an absolute deficiency of iron or a functional deficiency. Whereas the ferritin is not causal in arresting gut iron absorption, ferritin likely reflects iron sufficiency which in turn arrests gut iron absorption. Heme iron absorption may not be regulated in the same way as inorganic iron as inferred by its physiology. For example, in iron-deficient rats, nonheme iron absorption was increased several fold, but heme iron absorption was unaffected. However, other studies in iron-deficient rats demonstrated 3- to 10-fold increase in absorption of heme iron compared with controls. Whereas data in animals are conflicting, in subjects with serum ferritin concentration of >400 ng/mL heme iron absorption was >10 times greater than when iron was given as non-heme iron. Although these data are provocative, few head-to-head trials exist that help us in choosing between heme or non-heme iron supplements. Ferritin is a marker for evaluation of body iron stores and transferrin saturation is a marker that helps evaluate the ability to deliver iron to tissues that express a need for iron such as erythroblasts. For example, inflammation may increase serum ferritin concentration and reduce transferrin levels, thus masking the presence of iron deficiency. These influences create the pathophysiologic state of functional iron deficiency a difficult diagnosis to confirm. Those patients who may have low transferrin IronUseinEnd-StageRenalDisease 581 saturation and high serum ferritin may still respond to parenteral iron with a rise in Hgb. Some have suggested that the distinction of absolute and relative iron deficiency can be made by bone marrow examination for iron stores. SolubleTransferrinReceptor: Transferrin receptor 1 (TfR-1) is expressed on the surface of cells that require iron such as erythroblasts. Binding of the transferrin molecule to this receptor is responsible for the delivery of iron to these cells. The expression and release in plasma of soluble transferrin receptor (sTfR) are magnified in states of erythropoiesis and iron deficiency. Hepcidin: Measuring hepcidin level has been attempted but is technically complex and has large intraindividual variation. The main issues to be considered in iron therapy are the route of administration, available preparations, and their efficacy, safety, and cost. The major limitations of oral iron are its low bioavailability and adverse gastrointestinal side effects. These include ferrous forms (sulfate, fumarate, glutamate), carbonyl iron powder, and ferric polymaltose complex. Ferric polymaltose complex does not interact with food or drugs and hence can be taken with meals. As stated earlier, oral heme iron absorption occurs independently of iron stores, and through a different pathway. It is possible that oral heme iron is superior in maintaining iron balance than nonheme iron. IronUseinEnd-StageRenalDisease 583 Oral liposomal iron preparations promise better absorption. Not only does it control phosphorus as well as conventional phosphate binders, it has salutary effects on iron stores and anemia. Similar findings were observed in another study that randomized 441 subjects on dialysis to ferric citrate or active phosphate-binding control drug over a 52-week period. However, one of the studies included in this meta-analysis was 6 months long and reported a mean decline in hemoglobin of 0. Mortality and cardiovascular morbidity did not differ significantly, but were reported in only a few studies. It is possible that using 200 mg elemental oral iron may have increased the Hgb further in the oral iron group. Acute allergic and anaphylactic reactions are of major concern when dextran-containing irons are used and are rare with newer preparations. The size and coating of the iron product affects its cellular uptake and disposition in the tissues. These attributes also affect the maximum one-time dose and the rapidity of injection in one sitting. The side effect profile was also similar but these data do not ensure safety beyond 2 months. Ferric pyrophosphate is a water-soluble iron salt delivered through the dialysate.
Generic 50 mg clomid with amex. Advanced Women's Health Care OBGYN commercial.
References
- Hug CC Jr, Burm AG, de Lange S: Alfentanil pharmacokinetics in cardiac surgical patients, Anesth Analg 78(2):231-239, 1994.
- Anand S, et al. Oral anticoagulant and antiplatelet therapy and peripheral arterial disease. N Engl J Med. 2007;357(3):217-227.
- Nelson RG, Knowler WC, et al. Determinants of end - stage renal disease in Pima Indians with type 2 (non - insulin - dependent) diabetes mellitus and proteinuria. Diabetologia 1993; 36:87.
- Wojcik R, Cipolle MD, et al. Long-term follow-up of trauma patients with a vena caval fi lter. J Trauma. 2000;49:839-843.
- Moon MR. Approach to the treatment of aortic dissection. Surg Clin N Am. 2009;89:869-893.