Linda Shore-Lesserson, MD
- Professor of Anesthesiology
- Chief, Cardiothoracic Anesthesiology
- Montefiore Medical Center
- Bronx, New York
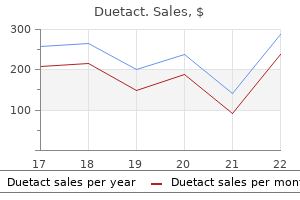
Commensurate with the magnitude of the hemorrhage managing diabetes and pregnancy buy cheap duetact 17 mg online, it is stressed that simultaneous activation of multidisciplinary diagnostic and therapeutic strategies will facilitate the best patient outcome diabetic peanut butter purchase duetact without prescription. In the cirrhotic patient, liver transplantation is often the only definitive treatment. The differential diagnosis of ascites is usually clarified to the calculation of an albumin ascites gradient. In portal hypertension associated with cirrhosis, systemic and splanchnic circulation is vasodilated, but renal blood flow is compromised and renal cortical blood flow is shunted to the medullary region of the kidney. Thus, ascites contributes to a confusing physiologic state in which patients have excess body sodium but an even greater excess of free water and thus serum hyponatremia. Renal physiology acts as if the patient is intravascularly depleted and alterations in aldosterone metabolism simultaneously add to the sodium retention. Once the pressure of ascites increases in the abdominal compartment, it further compromises renal blood flow due to venous compression. The mainstay of medical management of ascites is a reduction of sodium balance using dietary sodium restriction, free water restriction, and diuretics. Loop diuretics such as furosemide will interfere with sodium reabsorption while potassium-sparing diuretics can further increase sodium excretion, renal functioning permitting. Monitoring the serum albumin levels and giving albumin replacement when the level is below three are advised strategies to enhance control of ascites, as it may assist in increasing oncotic pressure. Newer medical strategies that may be considered for the control of ascites include midodrine, terlipressin, and vasopressin V2 receptor antagonists. Midodrine is an alpha adrenergic receptor agonist that results in an increase in mean arterial pressure in cirrhosis. Terlipressin is a vasopressin analog that acts on the V1 receptor in the splanchnic vasculature to cause splanchnic vasoconstriction, therefore decreasing splanchnic inflow and lowering the portal pressure. Vasopressin V2 receptor antagonists (vaptans) are agents that compete with vasopressin for attachment onto the V2 receptors at the renal collecting duct to inhibit water reabsorption at that site, thereby inducing an aquaresis and reduced serum water content. There has been evidence that vaptans are also able to reduce the extent of ascites in cirrhotic patients. Beyond the control of the hemorrhage, the overriding goal involves decompressive strategies to treat the underlying etiology of the hemorrhage. As with any portal decompression procedure, a reduction in total hepatic blood flow with an associated reduction in hepatic function is always a major concern. In acute variceal hemorrhage, efforts must be directed primarily at the control of hemorrhage. A mesocaval shunt is a good choice to create nonselective portosystemic decompression and control bleeding. The operative management of patients with the coagulopathy and severe portal hypertension should involve a surgeon experienced in a liver transplantation and hepatobiliary surgery. As with all complications of portal hypertension, the goal of management is often to create an opportunity window for orthotopic liver transplantation. Pleural effusion is a result of either the increased formation of pleural fluid or decreased absorption of hepatic hydrothorax in which large volumes of fluid from the abdomen are transferred to the pleural space. The defects in the diaphragm are usually associated with the lymphatic fenestra but may also be due to larger defects, such as an iatrogenic injury to the diaphragm. Hepatic hydrothorax occurs most commonly on the right side and is associated with the bare area of the right triangular ligament. The negative pressure of the thoracic cavity favors a unidirectional flow of ascites from the abdomen to the chest. Once a hepatic hydrothorax occurs, it rarely subsides and thus is considered an agonal finding associated with the end-stage liver disease. The patients in this study met the criteria of a known diagnosis of cirrhosis, pleural effusion, and pleural fluid consistent with the known characteristics of hepatic hydrothorax and not of an infection, malignancy, or other etiologies. The data suggest that some patients with hepatic hydrothorax die from complications arising from their pulmonary disease rather than from liver failure. The overall outcome of the patients was poor, with approximately half of the patients dying within one year of presentation. Pleural effusions associated with ascites are consistent with abdominal ascites and thus are, transudative. It should be noted that the hepatic hydrothorax can also be associated with more complex fluid collections in the chest (such as empyema), which may be spontaneous in nature or associated with prior infections of the pleural space. The etiology of empyema in the setting of hepatic hydrothorax is not completely understood. The primary reason hepatic hydrothorax represents such a difficult treatment dilemma is the risk of converting the hydrothorax to an empyema with iatrogenic manipulation. This is because the chest tube removal may be difficult to achieve, and the risk of contamination with leaving it in place is very high. Generally, no more than 2 L of pleural fluid should be removed to avoid pulmonary edema from lung expansion. Therefore, controlling the ascites becomes a very high priority for controlling the hepatic hydrothorax. The principles of managing the hepatic hydrothorax are similar to those presented in the ascites section but are more acute. Lung collapse associated with a substantial hepatic hydrothorax puts the patient at a high risk for a parenchymal lung infection. Whereas thoracentesis is the preferred method over pigtail or chest tube thoracostomy, empyema may still result. Ultimately, as in many of the complications of portal hypertension, a liver transplant is the only successful therapy since hepatic hydrothorax represents severe decompensation and, thus, is appropriately considered an agonal finding. The clinical scenario is usually one of acutely decompensated chronic liver failure and cirrhosis or in the setting of acute liver failure. In this syndrome, the kidneys are morphologically intact; however, there are functional abnormalities resulting from renal cortical medullary blood flow derangements, which in turn can cause increases in afferent arteriolar resistance in the renal cortex. This results in renal cortical hypoperfusion and excessive sodium absorption in the tubular medullary areas of the kidney. Aldosterone metabolism and alterations in the renin-angiotensin axis, as well as multiple mechanisms that support vasoconstriction, further exacerbate the pathophysiology. Furthermore, systemic peripheral vascular resistance and splanchnic vasodilation associated with the shunting of the cirrhotic state result in lower mean arterial pressure and gross reduction in renal perfusion. In light of the above changes in pathophysiology, it is not surprising that patients who present with ascites can also have such complications such as hemorrhage, hyponatremia, and worsening encephalopathy. All medications should be reviewed for their risk-benefit ratio as it relates to exacerbation of renal toxicity. Vasoconstrictors may be of a transient benefit as well as beta-blockers to reduce splanchnic vasoconstriction. The ability to assess when these severely ill patients are ready for a liver transplant is difficult. Contraindications to liver transplantation include active infection, extrahepatic malignancy, or a new malignancy. Of course, the primary focus of critical care management for a listed transplant patient is to optimize the patient for transplantation. Portal hypertension is defined as the presence of a raised portocaval pressure gradient that leads to many subsequent physiologic abnormalities. Gastrointestinal bleeding is the most life-threatening complication of portal hypertension, and its treatment requires expedited multidisciplinary assessment and treatment. Ascites, hepatic hydrothorax, hepatorenal syndrome, and hepatic encephalopathy are other complications of portal hypertension that require prompt recognition and expert medical and sometimes therapeutic intervention. In cases in which liver disease, or even more important, cirrhosis, is involved, the complications of portal hypertension and a critical illness of the patient will be magnified. Liver transplant should always be an underlying consideration and the potential goal for those with liver cirrhosis and portal hypertension as this will provide the ultimate and best treatment. This procedure not only treats portal hypertension but also the source of portal hypertension, liver cirrhosis, as well. Without the option of liver transplantation, 5-year survival of patients with Child C cirrhosis and variceal bleeding is approximately 25%, whereas the 5-year survival after a liver transplant is as high as 75%. The indication, listing, and timing of a transplant are complex and must be conducted by a complete liver transplant team.
In addition diabetic kitchen purchase discount duetact on-line, diabetic cystopathy and nephropathy may be complicating factors in the urinary tract diabetic jelly discount 16 mg duetact visa. In pyelonephritis, usually, a switch to insulin or insulin-analogous therapy is necessary. Operations or trauma may cause hypothermia, tissue hypoxia, and hemodynamic alterations that result in kidney dysfunction and impaired mucosal perfusion. Viral pathogens are only found in patients with severe immunosuppression, such as after bone marrow transplantation. Nonfermenters such as Pseudomonas aeruginosa, gram-positive cocci such as staphylococci and enterococci, and Candida species may also play an important role. The microbial spectrum is likely to differ over time and from one institution to the other. Early infections (up to 3 months after transplantation) are differentiated from late infections (more than 3 months after transplantation). There is, however, a risk of obstructive fungal balls leading to candidemia or invasion of the anastomosis in renal transplant recipients. Long-term indwelling catheters (more than 30 days) are associated with a selected microbial spectrum of difficult-to-treat uropathogens. A general adaptation strategy is the formation of hypermutator strains, which show 100- to 1000-fold increased mutation frequencies, enabling the pathogens to rapidly adapt to challenging environments and thus develop effective mechanisms for antibiotic resistance. Biofilm infections develop not only around foreign bodies such as urinary catheters or stents but also in urinary stones, scar or necrotic tissue, obstructive uropathies, or even chronic bacterial prostatitis. A biofilm has been defined as an accumulation of microorganisms and their extracellular products, forming a structured community on a surface. Attachment of microorganisms followed by microbial adhesion and anchorage to the surface by exopolymer production 3. Growth, multiplication, and dissemination of the organisms the basic structural unit of a biofilm is a microcolony-that is, a discrete matrix-enclosed community consisting of bacteria of one or more species. Surface film as an outer layer, where planktonic organisms can be released to float freely and spread on the surface Bacteria within biofilms differ both in behavior and phenotypic form from the planktonic, free-floating bacteria. Furthermore, antimicrobial binding proteins are poorly expressed in these slow-growing bacteria. Bacteria within a biofilm activate many genes that alter the cell envelope and molecular targets by altering the susceptibility to antimicrobial agents (intrinsic resistance). These phenotypic changes are likely to play a more important role in the development of antimicrobial resistance than external resistance (biofilm matrix, glycocalyx). At present, combination therapy with fluoroquinolones and macrolides or fosfomycin seems to be most effective against biofilm infections. During an acute febrile phase of biofilm infection, antimicrobial therapy is essential and can be effective because the planktonic bacteria are responsible for the febrile reactions and not the bacteria covered in the biofilm. However, to eradicate pathogens from the biofilm, the biofilm itself has to be removed. The physical examination should include inspection and palpation of the costophrenic area, lower abdomen, pubic region, inguinal lymph nodes, and genitals and a digital transvaginal or transrectal examination. Ultrasound is an important diagnostic device, and its use should be frequently considered because of the close proximity of the urogenital organs to the intestine, spleen, liver, pancreas, gallbladder, ovary, or uterus. Because urine from catheters has to be collected into a closed system, the urine specimen should be taken from the puncture site at the catheter after disinfection, without opening the closed system. There are different complementary methods for laboratory examination of the urine specimen. Some common uropathogens such as Enterococcus and Staphylococcus lack nitrate reductase and will therefore not be detected using this parameter, independent of their urinary concentration. To be of value in determining a nosocomial infection, urine specimens must be obtained aseptically using an appropriate technique such as clean catch collection, bladder catheterization, or suprapubic aspiration. Chamber counting of uncentrifuged urine (standard values for urine shown in Table 123-2). However, centrifugation methods are never quantitative in counting erythrocytes and leukocytes because of variable loss during centrifugation. Microbiology To differentiate contamination in urine from significant bacteriuria, quantitative microbiology is needed. Moreover, microbial resistance patterns must be considered in the choice of antibiotics. Increasing antibiotic resistance, especially among Enterobacteriaceae, makes prudent antibiotic therapy increasingly difficult. To diminish the selection pressure for resistant pathogens, antibiotics from different classes should be used. Synergism with aminoglycosides, which inhibit protein synthesis and thus block the formation of toxins or virulence factors, might be useful for initial therapy, but side effects have to be considered. It may represent harmless colonization, but it can also be an early sign of systemic candidosis. In critically ill patients, systemic therapy for Candida species should be started according to susceptibility testing or species differentiation (see Table 123-2). Complicating factors such as diabetes mellitus or urologic abnormalities should be treated concomitantly. For this reason, the interstitium of the renal medulla is more affected in pyelonephritis than the cortex. Focal nephritis is limited to one or more renal lobules, which is comparable to that in lobular pneumonia. Ultrasonographic findings are circumscribed lesion with interrupted echoes that breaks through the normal cortex/medulla organization. As differential diagnoses, renal abscess, tumor, and renal infarction must be taken into account. Emphysematous pyelonephritis characteristically shows gas formation in the renal parenchyma and perirenal space. Fermentation of glucose in Enterobacteriaceae occurs via two different metabolic pathways: mixed acid fermentation and the butylene glycol pathway. Organisms of the Klebsiella-Enterobacter-HafniaSerratia group and, to a lesser extent, E. The primary aim of acute therapy is improved urinary flow, with minimal patient contamination by infected urine. The best prophylaxis is to avoid a catheter or, if catheterization is necessary, to minimize catheter duration. Silver coating of catheters may exert a bactericidal effect, but the concentration of free silver ions must be high, whereas the exposure to albumin and chloride ions has to be low because silver-chloride complexes can precipitate. General hygienic procedures such as aseptic catheter insertion, wearing of disposable gloves, and hygienic hand disinfection to prevent cross-contamination or crossinfection are mandatory. Respiratory insufficiency, hemodynamic instability, or reflectory paralytic ileus occurs frequently. Frequent signs of renal abscess formation are fever and leukocytosis for more than 72 hours, despite antibiotic therapy. The fascial limitations are open toward the pelvis, and the perirenal fat is in close contact with the pelvic fat tissue. Blood cultures are positive in 10% to 40% of cases, and urinary cultures are positive in 50% to 80%. It is mainly seen in men in the fourth to seventh decades but also occurs in women or newborns. Causes are operations or trauma in the genital or perineal region, including microlesions, or infectious processes from the rectal or urethral areas.
16 mg duetact with amex. डायबिटीज (Diabetes) को जड़ से खत्म करें | Swami Ramdev.
Several -lactam antibiotics diabetes in toddlers purchase duetact 17 mg on line, fluoroquinolones diabetes type 2 urine test buy generic duetact 16mg line, clindamycin, and tigecycline possess activity against anaerobic organisms. A few investigational agents have the potential for use in anaerobic infections, but clinical data are needed. Bacteremia due to Bacteroides fragilis group: distribution of species, beta-lactamase production, and antimicrobial susceptibility patterns. Metronidazole, -lactam/-lactamase combinations, and carbapenems were consistently the most active agents. This review presents a comprehensive overview of the pharmacokinetics, pharmacodynamics, and use of metronidazole and nitroimidazole antimicrobials. Reassessment of Clostridium difficile susceptibility to metronidazole and vancomycin. This report affirms the findings of Aldridge and colleagues and documents the first report of metronidazole resistance among Bacteroides spp. Trends in susceptibility testing showed increasing resistance to clindamycin, moxifloxacin, and ampicillin/sulbactam, with relatively stable resistance rates to carbapenems, and piperacillin/tazobactam. A comprehensive review of Bacteroides with emphasis on virulence, infections in humans, resistance, antianaerobic agents, and susceptibilities. Performance standards for antimicrobial susceptibility testing; twenty-second informational supplement. Bacteriology of moderate-to-severe diabetic foot infections and in vitro activity of antimicrobial agents. Update on resistance of Bacteroides fragilis group and related species with special attention to carbapenems 2006-2009. Susceptibility of respiratory tract anaerobes to orally administered penicillins and cephalosporins. In vitro efficacy of beta-lactam/beta-lactamase inhibitor combinations against bacteria involved in mixed infections. Diagnosis and management of complicated intraabdominal infections in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Practice Guidelines for the Diagnosis and Management of Skin and Soft-Tissue Infections. Pharmacological properties of parenteral cephalosporins: rationale for ambulatory use. Prevalence of antibiotic resistance in anaerobic bacteria: worrisome developments. Cefoxitin in the treatment of aerobic/anaerobic infections: prospective correlation of in vitro susceptibility methods with clinical outcome. Infections after elective colorectal surgery: bacteriological analysis of failures in a randomized trial of cefotetan vs. Moxifloxacin is non-inferior to combination therapy with ceftriaxone plus metronidazole in patients with community-origin complicated intra-abdominal infections. Multicenter survey of the changing in vitro antimicrobial susceptibilities of clinical isolates of Bacteroides fragilis group, Prevotella, Fusobacterium, Porphyromonas, and Peptostreptococcus species. Carbapenem stewardship: does ertapenem affect Pseudomonas susceptibility to other carbapenems Activity of meropenem against antibiotic-resistant or infrequently encountered gram-negative bacilli. Increasing trends in antimicrobial resistance among clinically important anaerobes and Bacteroides fragilis isolates causing nosocomial infections: emerging resistance to carbapenems. Lessons learned from the anaerobe survey: historical perspective and review of the most recent data (2005-2007). Multicenter study of in vitro susceptibility of the Bacteroides fragilis group, 1995 to 1996, with comparison of resistance trends from 1990 to 1996. National survey on the susceptibility of Bacteroides fragilis Group: report and analysis of trends for 1997-2000. Variation in the susceptibility of Bacteroides fragilis group isolates from six Chicago hospitals. Linezolid activity compared to those of selected macrolides and other agents against aerobic and anaerobic pathogens isolated from soft tissue bite infections in humans. Presence and antibiotic resistance of Porphyromonas gingivalis, Prevotella intermedia, and Prevotella nigrescens in children. Antibiotic resistance in Propionibacterium acnes, microbiological and clinical aspects. Susceptibility of anaerobic bacteria to metronidazole: relative resistance of non-spore forming gram-positive bacilli. Carcinogenicity of 5-nitrofurans, 5-nitroimidazoles, 4-nitrobenzenes, and related compounds. Safety of metronidazole during pregnancy: a cohort study of risk of congenital abnormalities, preterm delivery and low birth weight in 124 women. Two cases of infections due to multidrug-resistant Bacteroides fragilis group strains. Comparative in vitro susceptibilities of 396 unusual anaerobic strains to tigecycline and eight other antimicrobial agents. In vitro activities of moxifloxacin against 900 aerobic and anaerobic surgical isolates from patients with intra-abdominal and diabetic foot infections. In vitro activity of moxifloxacin against 923 anaerobes isolated from human intra-abdominal infections. Clinical efficacy and correlation of clinical outcomes with the in vitro susceptibility for anaerobic bacteria in patients with complicated intra-abdominal infections treated with moxifloxacin. Emergence of beta-lactamase-producing aerobic and anaerobic bacteria in the oropharynx of children following penicillin chemotherapy. Intact anaerobic flora is considered an important defense mechanism against intestinal colonization by potentially pathogenic microorganisms. Anaerobic bacteria grow well on the mucosa of the gut and actively line the epithelium. Combinations of nonabsorbable antibiotics have been used to selectively decontaminate the digestive tract and reduce the load of pathogenic aerobic microorganisms while maintaining the anaerobic flora. Because inclusion was based on several criteria, this created the possibility of selection bias. To minimize the occurrence of selection bias, patient eligibility and inclusion rates were monitored frequently and immediately followed by feedback to the participating investigators. Yet despite the use of these measures next to the objective inclusion criteria, there were baseline differences between the control and the two intervention groups. Suppression of the anaerobic flora increases the risk of overgrowth by gram-negative bacteria. The overall risk of acquisition of colistin-resistant gram-negative bacteria and conversion rates to colistin resistance were low. These findings do not support the concern that the use of topical antibiotics, with or without systemic prophylaxis with thirdgeneration cephalosporins, increases the prevalence levels of antibiotic resistance in gram-negative bacteria. This conclusion is supported by two 5-year prospective studies and a recent meta-analysis. Both were superior to chlorhexidine, with a remark that chlorhexidine might be associated with increased mortality. If a sputum surveillance culture (>48 h after Nebulize 5 mL (80 mg) polymyxin E 4 times daily until 2 Decolonization admission culture) yields gram-negative bacteria* sputum cultures are negative. An increasing incidence of resistance in the participating hospitals might have influenced these results. This difference was primarily attributed to the decrease in the use of antibiotics such as ciprofloxacin, ceftazidime, imipenem, and antifungal treatment. No evidence supports the concern that the use of topical antibiotics with or without systemic prophylaxis increases the prevalence of antibiotic resistance to gram-negative bacteria. The effect of selective decontamination of the digestive tract on colonization and infection rate in multiple trauma patients. Antibiotic prophylaxis to reduce respiratory tract infections and mortality in adults receiving intensive care. Effects of selective decontamination of the digestive tract on mortality and acquisition of resistant bacteria in intensive care: a randomised controlled trial. Both interventions significantly improved survival (absolute mortality reduction of 3.
New-onset multiple organ dysfunction syndrome diabetes test how to prepare 17mg duetact with mastercard, incisional hernias diabetes in dogs pain discount duetact 16 mg overnight delivery, and new-onset diabetes mellitus occurred less frequently in patients randomized to this less invasive study arm. This Cochrane review compares 40 studies of 16 different antibiotic regimens for peritonitis in 5094 patients. Other factors such as local guidelines and preferences, ease of administration, costs, and availability must therefore be used for antibiotic selection. Complications associated with inadequate source control include abscess formation, anastomotic dehiscence, surgical site infection, recurrent or persistent (secondary or tertiary) peritonitis, fistula formation, abdominal compartment syndrome, sepsis, and multiple organ dysfunction syndrome. Neither planned re-laparotomy nor open abdomen techniques offer survival benefits when compared with on-demand relaparotomy in achieving adequate source control. Multiple organ dysfunction syndrome is present in virtually every patient who dies from intraabdominal infection. Longitudinal outcomes of intraabdominal infection complicated by critical illness. Noradrenergic neurons regulate monocyte trafficking and mortality during gram-negative peritonitis in mice. Low doses of celecoxib attenuate gut barrier failure during experimental peritonitis. Role of hypoxia inducible factors 1alpha and 2alpha in basal adhesion formation and in carbon dioxide pneumoperitoneum-enhanced adhesion formation after laparoscopic surgery in transgenic mice. Na+H+ exchange and the regulation of intracellular pH in polymorphonuclear leukocytes. Influence of the critically ill state on host-pathogen interactions within the intestine: gut-derived sepsis redefined. Immune reactions to Bacteroides fragilis populations with three different types of capsule in a model of infection. Fivefold reduction in peritonitis using a multifaceted continuous quality initiative program. Vancomycin-resistant peritonitis associated with peritoneal dialysis: a cause for concern. Laparoscopic peritoneal lavage for perforated colonic diverticulitis: a systematic review. Tertiary peritonitis (recurrent diffuse or localized disease) is not an independent predictor of mortality in surgical patients with intraabdominal infection. Methicillin-resistant Staphylococcus aureus as a causative agent of post-operative intra-abdominal infection: relation to nasal colonization. Diagnosis and management of complicated intraabdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Enhancement of intraperitoneal staphylococcal virulence for mice with different bile salts. Antibiotic regimens for secondary peritonitis of gastrointestinal origin in adults. Postoperative enterococcal infection after treatment of complicated intraabdominal sepsis. Emergence of antibiotic-resistant bacteria in cases of peritonitis after intraabdominal surgery affects the efficacy of empirical antibiotic therapy. An increasing prominent disease of Klebsiella pneumoniae liver abscess: etiology, diagnosis, and treatment. Image-guided percutaneous procedure plus metronidazole versus metronidazole alone for uncomplicated amoebic liver abscess. Endoscopic ultrasound-guided hepatic and perihepatic abscess drainage: an evolving technique. Use of morphine cholescintigraphy in the diagnosis of acute cholecystitis in critically ill patients. Temporary closure of the open abdomen: a systematic review on delayed primary fascial closure in patients with an open abdomen. Negative-pressure wound therapy for critically ill adults with open abdominal wounds: a systematic review. The open abdomen and temporary abdominal closure systems- historical evolution and systematic review. The Spanish Group for the Study of Septic Complications in Severe Acute Pancreatitis. Early antibiotic treatment (prophylaxis) of septic complications in severe acute necrotizing pancreatitis: a prospective, randomized, multicenter study comparing two regimens with imipenem-cilastatin. Current status of minimally invasive necrosectomy for post-inflammatory pancreatic necrosis. Three hundred consecutive emergent celiotomies in general surgery patients: influence of advanced diagnostic imaging techniques and procedures on diagnosis. Abdominal computed tomography for the diagnosis of intraabdominal sepsis in critically injured patients. High-risk intrahospital transport of critically ill patients: safety and outcome of the necessary "road trip. Critical issues in the clinical management of complicated intra-abdominal infections. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2012. Meta-analysis of the effect of peritoneal lavage on survival in experimental peritonitis. Radical surgical debridement in the treatment for established peritonitis: the results of a prospective randomized clinical trial. Fecal peritonitis: microbial adherence to serosal mesothelium and resistance to peritoneal lavage. Staged lavage versus single high-volume lavage in the treatment of feculent/purulent peritonitis: a matched pair analysis. Mechanically assisted intra-operative peritoneal lavage for generalized peritonitis as a result of perforation of the upper part of the gastrointestinal tract. Irrigation versus suction alone during laparoscopic appendectomy for perforated appendicitis: a prospective randomized trial. Mortality and morbidity of planned relaparotomy versus relaparotomy on demand for secondary peritonitis. Empiric treatment options in the management of complicated intra-abdominal infections. Evaluating empiric treatment options for secondary peritonitis using pharmacodynamic profiling. A multicenter trial of the efficacy and safety of tigecycline versus imipenem/cilastatin in patients with complicated intra-abdominal infections. A multicentre, open-label, randomised comparative study of tigecycline versus ceftriaxone sodium plus metronidazole for the treatment of hospitalised subjects with complicated intra-abdominal infections. Randomized controlled trial of moxifloxacin compared with piperacillin-tazobactam and amoxicillin-clavulanate for the treatment of complicated intraabdominal infections. Predictive factors of mortality due to polymicrobial peritonitis with Candida isolation in peritoneal fluid in critically ill patients. Pharmacokinetics of sequential intravenous and enteral fluconazole in critically ill surgical patients with invasive mycoses and compromised gastrointestinal function. Can yeast isolation in peritoneal fluid be predicted in intensive care unit patients with peritonitis De-escalation after empirical meropenem treatment in the intensive care unit: fiction or reality Management of postoperative enterocutaneous fistulas: the role of parenteral nutrition and surgery. One hundred and fourteen fistulas of the gastrointestinal tract treated with total parenteral nutrition. Somatostatin versus octreotide in the treatment of patients with gastrointestinal and pancreatic fistulas. Daily organ-system failure for diagnosis of persistent intra-abdominal sepsis after postoperative peritonitis. Intensive versus conventional insulin therapy: a randomized controlled trial in medical and surgical critically ill patients. Immunomodulation in sepsis: the role of endotoxin removal by polymixin B-immobilized cartridge. Mechanical obstruction is the inability for contents to move forward due to luminal obstruction. Further classification is based on the presence of vascular compromise and ischemia.
References
- Thompson KW, Suchomelova LM. Transplants of cells engineered to produce GABA suppress spontaneous seizures. Epilepsia 45: 4-12, 2004.
- Pessin MS, Panis W, Prager RJ, et al. Auscultation of cervical and ocular bruits in extracranial carotid occlusive disease: A clinical and angiographic study. Stroke 1983;14:246-9.
- Eilber FC, Eilber FR, Eckardt J, et al. The impact of chemotherapy on the survival of patients with high-grade primary extremity liposarcoma. Ann Surg 2004;240(4):686-695.
- Foley KM. How well is cancer pain treated? Palliat Med 2011;25(5):398-401.
- Sasaki M, Satoh K, Fukunaga K, et al. Rounded atelectasis formation following decrease of pleural effusion: a case report. Radiat Med 1996;14(6): 331-3.
- Oldfors A, Holme E, Tulinius M, Larsson N-G. Tissue distribution and disease manifestations of the tRNALys A?G(8344) mitochondrial DNA mutation in a case of myoclonus epilepsy and ragged red fibers. Acta Neuropathol 1995;90:328.
- Kasemsiri P, Prevedello DM, Otto BA, et al. Endoscopic endonasal technique: treatment of paranasal and anterior skull base malignancies. Braz J Otorhinolaryngol 2013;79(6):760-779.
- Venkatraghavan L, Manninen P. Anaesthesia for deep brain stimulation. Curr Opin Anesthesiol. 2011;24: 495-9.