Kathleen Borge, RN, MS
- Faculty Chair
- Samaritan Hospital School of Nursing
- Troy, New York
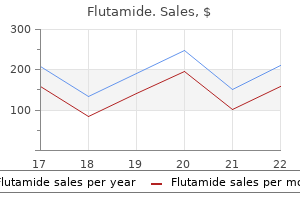
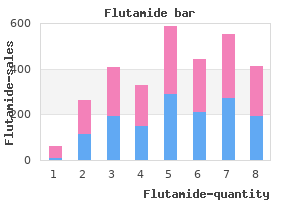
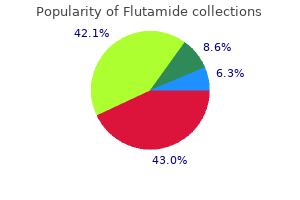
Many children born with tracheoesophageal fistula have recurrent cough and lower respiratory tract infection for many years symptoms flu proven 250 mg flutamide, even after successful surgical correction medicine nelly 250 mg flutamide otc. The cough is characteristically the harsh cough of tracheomalacia medications 73 cheap 250 mg flutamide overnight delivery, which is present at the site of the fistula. Treatment involves regular chest physiotherapy and early and aggressive use of antibiotics whenever there is evidence of increased pulmonary symptoms. Hemangiomas may be present within the airway and can cause cough, rarely with hemoptysis. Stridor (if the hemangioma is high in the airway) and respiratory distress (if the hemangioma is large) may also occur. In rare cases, with very large airway hemangiomas, there may even be dysphagia from extrinsic compression. Children with cutaneous hemangiomas in the mandibular or neck region ("beard" distribution) are at risk for an airway hemangioma. However, if they cause symptoms, it may not be advisable or possible to wait for them to resolve. Many airway hemangiomas regress with steroid treatment; however, due to the side effect profile, propranolol is considered the treatment of choice. Asthma is a contraindication for propranolol treatment due to its beta-blocking effect and potential to worsen asthma. Laser ablation may be indicated in some refractory cases that do not respond to first-line treatment. In the case of a large subglottic hemangioma, a tracheostomy is performed and maintained until the mass regresses. Enlarged mediastinal lymph nodes, such as those resulting from tuberculosis, leukemia, other hematologic malignancies, or other infections, are occasionally a cause of cough in children (Table 2. The diagnosis is made with bronchoscopy, after suspicion has been raised by the child having recurrent infiltrates in the same lobe, especially with localized wheeze. In some cases, endoscopic balloon dilatation or airway stent placement is successful; in others, surgical resection of stenotic areas may be necessary. Bronchogenic cysts are uncommon, but they can cause cough, wheeze, stridor, or any combination of these. They may also cause recurrent or persistent pneumonia if they block a bronchus sufficiently to interfere with normal drainage of the segment or lobe. Habit (Psychogenic) Cough On occasion, a school-aged child may develop a cough that lasts for weeks, often after a fairly typical cold. The child is otherwise well and may seem rather unbothered by the spectacle created. It seems that this type of cough, previously termed "psychogenic," or "psychogenic cough tic," but now called habit cough, has given the child valuable attention. This attention then serves as the sustaining force, and the cough persists beyond the original airway inflammation. In the small minority of cases, there may be deep-seated emotional problems of which the cough is the physical expression. During the history or physical examination, the child appears completely well and may cough when attention is drawn to the child or when the word "cough" is uttered. The physical examination findings are otherwise completely normal, as are laboratory values. Because this may occur in any child, evidence of mild reactive airways disease (history or pulmonary function testing) does not rule out the diagnosis. Once a physician has seen a child with this problem, it is usually possible to make the diagnosis with certainty on entering the examining room or, indeed, from the hallway outside the room. Suggestion therapy empowers and encourages the patient to suppress the cough for short increments of time. Cough occurs because of bronchial blockage, either extrinsic or endobronchial (see Table 2. Treatment depends on the cell type, but it usually involves at least some surgical removal. Isolated tracheomalacia or bronchomalacia is uncommon but can cause cough in some children. Some children, usually preschoolers, may episodically awaken at night with stridor and a harsh, barking cough indistinguishable from that of viral croup. In other instances, it may arise after adenovirus, measles, or influenza pneumonia; after exposure to certain toxins; or in other rare circumstances. The diagnosis is suggested by the pulmonary function test or radiographic evidence of small airways obstruction; however, these findings are not always present. Not all chest radiographs show overinflated lungs, and not all pulmonary function tests show decreased small airways function. Most children with obliterative bronchiolitis recover, but many progress to chronic disability or death. Bronchiectasis is defined as an abnormal dilation of the subsegmental bronchi and is usually associated with chronic cough and purulent sputum production. Treatment of bronchiectasis consists of airway clearance with chest physiotherapy with postural drainage or highfrequency chest wall oscillation, occasionally bronchodilators and mucolytic agents, and antibiotic therapy during exacerbations. Surgical resection may be indicated in cases that are progressive and localized when medical therapy has failed. Conditions in which the cilia do not function properly (immotile cilia or ciliary dyskinesia) lead to cough, usually because infection (and bronchiectasis) occurs in the absence of normal mucociliary transport. Interstitial lung diseases are now classified based on those that occur during the neonatal period and those that are not as prevalent in infancy. Pulmonary hemosiderosis is a rare, and often fatal, condition of bleeding into the lung that can manifest with cough. Some cases are associated with milk hypersensitivity (Heiner syndrome), and affected children may have upper airway obstruction. Radiographs usually show diffuse fluffy Hemoptysis the child who coughs out blood or bloody mucus presents special diagnostic and therapeutic challenges. It is important (and not always easy) to distinguish cases in which blood has originated in the tracheobronchial tree (true hemoptysis), the nose (epistaxis), and the gastrointestinal tract (hematemesis). None of these guidelines is foolproof, partly because blood that has originated in one of these sites might well end up in another before being expelled from the body; for instance, blood from the nose can be swallowed and vomited or aspirated and expectorated. Bronchiectasis can readily cause erosion into bronchial vessels, often made tortuous by years of local inflammation, and produce hemoptysis. Other infectious causes are less common and include necrotizing pneumonias and fungal and parasitic lung invasion. Foreign bodies in the airway can cause hemoptysis by direct irritation, by erosion of airway mucosa, or by secondary infection. Pulmonary embolus is uncommon in children and adolescents, but it needs to be considered in the differential diagnosis of an adolescent with hemoptysis of unclear origin. For example, hemoptysis that occurs immediately after a surgical or invasive diagnostic procedure in the chest should suggest an iatrogenic problem. The chest radiograph can help suggest lung abscess, pulmonary sequestration, bronchogenic cyst, or tumor. In many instances, bronchoscopy does not help except by excluding some possibilities, because either no blood or blood throughout the tracheobronchial tree is found. It can be a terrifying symptom to children and their parents, and a calm, reassuring approach is essential. Furthermore, hemoptysis most often resolves, and treatment of the bleeding itself is not often needed. What is required is treatment of the underlying cause of the hemoptysis, such as therapy for infection, removal of a foreign body, or control of collagen vascular disease. When death occurs from hemoptysis, it is more likely to be from suffocation than from exsanguination. In cases of massive bleeding, the rigid open-tube bronchoscope may help suction large amounts of blood while ventilating and keeping unaffected portions of lung clear of blood. Interventional radiologists treat as well as localize a bleeding site by injecting the offending vessel with occlusive substances (embolization). Disadvantages include narcotic addiction and loss of the protective cough reflex with subsequent mucous retention and possible superinfection. Demulcent preparations (sugar-containing, bland soothing agents or honey) temporarily suppress the cough response from pharyngeal sources, and decongestant-antihistamine combinations may reduce postnasal drip. Most complications are uncommon, and most accompany only very severe cough, but some are serious enough to justify treatment of the cough itself. Cough suppressants include codeine and hydrocodone (two narcotics) and dextromethorphan (a nonnarcotic D-isomer of the codeine analog of levorphanol). In the acute setting, severe disease, including massive hemoptysis or profound dyspnea or hypoxemia, warrants immediate attention, rapid diagnosis, and rapid management. Finally, a child whose cough fails to respond to what should have been reasonable treatment should be referred to a pulmonary specialist (Table 2. Wheezing in infants with cystic fibrosis: Clinical course, pulmonary function, and survival analysis. The management of communityacquired pneumonia in infants and children older than 3 months of age: Clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Infant pneumonitis associated with cytomegalovirus, Chlamydia, Pneumocystis, and Ureaplasma: Follow-up. British Thoracic Society guidelines for the management of community acquired pneumonia in children: Update 2011. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis.
Twelve percent of infants with bronchopulmonary dysplasia develop hypertension treatment alternatives boca raton purchase flutamide overnight, which is probably multifactorial in origin but may involve effects of umbilical artery catheterization and the administration of corticosteroids and bronchodilators nioxin scalp treatment discount flutamide 250 mg free shipping. Clinical Presentation the clinical presentation of hypertension in the neonate is quite variable medications on a plane purchase flutamide 250mg without a prescription. Although elevated blood pressures are typically noted on routine monitoring, nonspecific symptoms such as poor feeding, irritability, and lethargy may be present. Determinants of blood pressure in infants admitted to neonatal intensive care units: a prospective multicenter study, Philadelphia Neonatal Blood Pressure Study Group. Neurologic symptoms such as tremors, hypertonicity, hypotonicity, opisthotonos, asymmetric reflexes, hemiparesis, seizures, apnea, or coma may also occur. Ultrasonography of the kidneys with a Doppler flow study of the aorta and renal arteries should be performed to exclude a renal arterial or aortic thrombus or structural anomalies of the urinary tract. Absence of a defined thrombus does not, however, rule out renovascular hypertension as the majority of thrombi are very small and not detectable by ultrasonography. Computed tomography, magnetic resonance angiography, and angiography may be considered in more difficult cases, although their use may be limited in the very small infant. Echocardiography should be performed to exclude aortic coarctation and evaluate the left ventricular mass. Treatment the first approach to the treatment of neonatal hypertension is to correct all iatrogenic causes of blood pressure elevation, including inotrope administration, volume overload, withdrawal from narcotics, or inadequately controlled pain. If blood pressures remain elevated, the clinician has a wide variety of intravenous and oral antihypertensives that may be considered (Table 101-6 and Table 101-7). The chief advantage of a continuous infusion is the ability to quickly increase or decrease the rate of infusion to achieve the desired blood pressure. The goal of therapy is a gradual decrease in blood pressure to minimize injury to the brain, heart, and kidneys. Blood pressure should not be lowered below the 95th percentile for at least 24 to 48 hours to avoid the possibility of cerebral and optic disc ischemia. Oral antihypertensive agents are best used in infants with less severe hypertension or in those whose acute hypertension has been controlled with intravenous infusions and who are ready to switch to chronic oral therapy. Calcium channel blockers, such as isradipine and amlodipine, are first-choice agents. A standardized protocol for accurate blood pressure measurement in neonates is shown in Box 101-5. A complete physical examination is imperative, including blood pressure measurements of all four extremities to diagnose or rule out aortic coarctation. The infant should be examined carefully for signs of volume overload including peripheral edema, cardiac gallop, or rales. The abdomen should be carefully inspected for presence of abdominal or flank masses or renal bruits. Ambiguous genitalia in a hypertensive infant should raise the suspicion of congenital adrenal hyperplasia. Initial laboratory studies should include a urinalysis and determinations of serum electrolytes, blood urea nitrogen, serum creatinine, and serum calcium. Other diagnostic studies, including renin, aldosterone, cortisol, thyroid function tests, and catecholamines, can be considered based on the clinical scenario and results of screening studies. Intermittent administration of intravenous agents, such as hydralazine or labetalol, may be considered in hypertensive infants with mild to moderate hypertension in whom oral agents cannot be used because of gastrointestinal dysfunction. In infants with suspected renovascular hypertension, the umbilical artery catheter should be removed as soon as possible. If a large thrombus is identified, systemic heparinization may be considered to prevent extension of the clot. If the hypertension cannot be controlled medically or massive aortic thrombosis results in major complications, thrombolysis with urokinase, streptokinase, or tissue plasminogen activator may be considered. If severe hypertension persists, surgical thrombectomy or nephrectomy may be contemplated. In addition, infants with nephrocalcinosis may present with microscopic or gross hematuria, granular material in the diaper, or urinary tract infection. Nephrocalcinosis, defined as calcium deposition in the renal interstitium, develops as the consequence of an imbalance between stone-promoting and stone-inhibiting factors. The primary risk factor in neonates is hypercalciuria (excessive urinary calcium excretion), which is commonly caused by chronic treatment with loop diuretics. Other risk factors include prematurity, low birth weight, severe respiratory disease, low urine volume, the hypercalciuric effect of glucocorticoids or xanthine derivatives, hypocitraturia, hyperoxaluria, parenteral nutrition, metabolic acidosis, and a familial history of nephrolithiasis. In those with documented nephrocalcinosis, loop diuretics should be Prognosis Infants with elevated blood pressures related to polycystic kidney disease, renal venous thrombosis, or congenital kidney disease will most likely have hypertension that persists into childhood. However, most neonatal hypertension presumed to be caused by umbilical artery catheters or bronchopulmonary dysplasia resolves with time and infants do not typically require antihypertensive medications beyond 12 months of age. Other agents that increase urinary calcium excretion, including glucocorticoids, xanthine derivatives, and any sodium-containing supplements should be minimized or discontinued if possible. A high urinary flow rate should be maintained to reduce the probability of urinary crystallization. Metabolic acidosis, if present, should be treated with potassium (not sodium) citrate because chronic acidosis enhances urinary calcium excretion. Thiazide diuretics, such as chlorothiazide, may be effective in reducing urinary calcium excretion, although serum calcium should be monitored closely to avoid hypercalcemia. The goal of therapy should be the maintenance of the spot urinary calcium to creatinine ratio less than 0. In one study, nephrocalcinosis persisted in 34% of preterm infants at 15 months of age, and in only 15% at 30 months of age. However, the prognosis for the affected kidney is poor, with progressive atrophy in up to 70% of kidneys. Congenital and Inherited Disorders of the Kidney and Urinary Tract Many of the disorders of the kidney and urinary tract that present in utero or in the neonatal period are the result of congenital malformations or inherited disorders (Box 101-6; see also Table 101-2). Most of the congenital abnormalities of the kidney and urinary tract disorders occur sporadically, and the pathogenesis is not well defined. However, recent studies have begun to elucidate the genetic basis for some of these disorders, such as Eagle-Barrett ("prune belly") syndrome, renal hypoplasia and renal dysplasia. The following section will review some of the more common renal disorders that present in neonates and infants. Thrombosis begins in the small renal veins and propagates toward the main renal vein, ultimately reaching the inferior vena cava. Thrombosis is usually unilateral (70%) but may be bilateral or extend into the inferior vena cava, and is associated with adrenal infarction in a minority of patients. Ultrasonography in the acute phase reveals typical findings of kidney enlargement, loss of corticomedullary differentiation, increased renal echogenicity, and perivascular echogenic streaking. Ultrasonography following the acute phase may show gradual decrease in kidney size with renal atrophy. Renal Dysplasia Renal dysplasia is characterized by abnormal renal development in the fetus, leading to replacement of the renal parenchyma by cartilage and disorganized epithelial structures. The pathogenesis of renal dysplasia may involve mutations in developmental genes, urinary tract obstruction or in utero toxin/medication exposure. Most forms of "polycystic kidneys" that are reported in association with syndromes, in fact, represent bilateral cystic dysplasia. The function of dysplastic kidneys is quite variable, and infants with bilateral dysplasia may exhibit signs of renal insufficiency as early as the first few days of life. Concentration and acidification defects may also be present, but hematuria, proteinuria, and hypertension are unusual findings. Children with bilateral renal dysplasia generally develop progressive renal insufficiency during childhood and adolescence. Although older data suggested that the rate of contralateral urinary tract abnormalities, including vesicoureteral reflux, ureteropelvic junction obstruction, renal dysplasia, and ureterocele was as high as 90% in patients with unilateral renal agenesis,9 a newer meta-analysis suggests the rate is only 30%. Unilateral renal agenesis is also associated with developmental defects of the Mrian ducts, such as Mayer-Rokitansky or Herlyn-Werner-Wunderlich syndromes. The pathogenesis is poorly understood but may involve failure of the ureteric bud to integrate and branch appropriately into the metanephros. The contralateral kidney, if unaffected by other urologic malformations, generally shows compensatory hypertrophy,76 allowing the child to maintain normal renal function. With mild unilateral disease, diagnostic testing may be limited and the patient can be managed by the pediatrician or neonatologist in consultation with a pediatric nephrologist or urologist. In contrast, management of fetuses with severe bilateral disease requires a multidisciplinary team approach involving neonatology, nephrology, urology, and social services and/or palliative care starting in the prenatal period and continuing after birth to optimize care. The grading and reporting of hydronephrosis on prenatal and postnatal ultrasounds remains somewhat subjective and dependent on the preferences, practices, and expertise of the physician performing the study. Despite these limitations, important prognostic information has emerged from various studies, and certain findings on prenatal ultrasonography appear to have a role in predicting longterm outcome. Measurement of the anteroposterior diameter is the most commonly performed assessment of fetal hydronephrosis. Most practitioners accept the threshold of less than 4 mm as normal and the presence of an anteroposterior diameter of greater than 15 mm as indicative of severe prenatal hydronephrosis that is likely to be associated with poorer outcome. With less severe and unilateral disease, less frequent prenatal imaging is required. Prenatal interventions, such as percutaneous vesicoamniotic shunt placement, have been attempted in an effort to improve amniotic fluid volume and relieve in utero obstruction. Studies of such interventions are small, and their contribution to improving overall renal outcome may be modest. In addition, antenatal shunt placement is associated with significant risks, including fetal loss, preterm labor, and chorioamnionitis (see Chapter 14). Postnatal management begins with a detailed obstetrical and family history, physical exam and renal/bladder ultrasonography.
Buy genuine flutamide line. Parkinson's Disease and Depression: Symptoms and Treatments.
Jaundice manifesting in the first 24 hours of life is emphasized as an important risk factor medications that cause tinnitus buy 250mg flutamide mastercard, and recommendations for infants with early jaundice are included in the therapeutic guidelines treatment zinc toxicity buy cheap flutamide on-line. It is commonly accompanied by a rise in serum levels of other constituents of bile symptoms just before giving birth flutamide 250mg visa, such as bile salts and phospholipids. The designation cholestasis, meaning reduction in bile flow, is used to describe this group of disorders. The rise of conjugated serum bilirubin may be the result of primary defects in the hepatocellular transport or excretion of bile, or secondary to abnormalities in bile duct function or structure. The hepatocellular phase of bile secretion involves the transport of conjugated bilirubin across the hepatic cell membrane at the biliary pole. The lateral cell membrane at this site is folded to form microvilli and becomes part of the canalicular space, surrounded by two or more adjacent hepatocytes. Microvilli and the underlying cytoplasm contain microfilaments visible by electron microscopy. These structures consist of the contractile protein actin, which is necessary for normal canalicular contraction and microvillous motility, important elements in the generation of intrahepatic bile flow. It follows that any hepatocellular injury may result in impairment of the cellular phase of bile excretion and breakdown of the tight junctions, leading to the clinical and laboratory findings of cholestasis. Hyperbilirubinemia resulting from hepatocellular injury may be associated with other abnormalities that reflect impairment of other hepatocellular functions. A liver biopsy taken in the early stages of one of the diseases caused by a hepatocellular defect in bile secretion would characteristically show bile pigment granules in hepatocytes and canaliculi, referred to as intracellular and intracanalicular cholestasis. Bile pigment granules are not seen in either hepatocytes or canaliculi of normal liver parenchyma. In fact, the canalicular lumen is not visualized in routine sections of normal liver parenchyma because it is partially obliterated by microvilli identifiable only by electron microscopy. In cholestasis, there is usually blistering, blunting, or destruction of these microvilli, transforming the bile canaliculus into a widened, round space containing bile (the bile plug). On rare occasions, liver biopsies from patients with conjugated hyperbilirubinemia fail to show any abnormalities when examined with the light microscope. The intrahepatic biliary system comprises the bile ductules (the initial portion of which is frequently referred to as the canals of Hering); the interlobular (portal) bile ducts, recognized by their constant association with a vein and an arteriole; and the right and left hepatic ducts, which in some individuals may partially extend beyond the liver capsule at the liver hilum. The extrahepatic component includes the common hepatic duct, the cystic duct, the gallbladder, and the common bile duct (choledochus). The extrahepatic biliary system and the major right and left hepatic ducts contain intramural and periductal glandular structures. Although the role of these structures in humans is not clearly understood, information derived from animal experiments suggests they may play an important role in bile duct regeneration or failure to regenerate. Anatomic structures are identified to the left of the illustration, and the corresponding physiologic events are listed on the right. Most diseases affecting the extrahepatic bile ducts, and occasionally the left and right hepatic ducts, are associated with segmental or diffuse luminal obliteration and are primarily expressions of mechanical disturbance in bile flow. Diseases involving the intrahepatic ducts, in the absence of concomitant extrahepatic disease, are complex and probably result from a combination of mechanical obstruction to the flow of bile, abnormalities of the biochemical pathways involved in the process of bile secretion, and, in some cases, persistence of infectious agents or viral antigens. This change may not be present when luminal obliteration is incomplete or when it develops slowly because these cases are frequently complicated by reduction in intrahepatic bile secretion and flow. A constant and characteristic tissue response to complete mechanical obstruction of a major bile duct is dilation and proliferation of proximal portions of the intrahepatic biliary system, including the ductules and canals of Hering, structures that are outside the confines of the portal tracts. A constant accompaniment to bile duct proliferation is an increase in surrounding connective tissue, which eventually leads to fibrous bridging between adjacent portal tracts, causing biliary cirrhosis. Although bile secretory defects may initially be purely hepatocellular or ductal, any long-standing abnormality in the flow of bile leads to some degree of hepatocellular damage. Box 100-5 lists diseases that may manifest as conjugated hyperbilirubinemia in the neonatal period. This list is divided into those disorders caused by a primary defect in the hepatocellular phase of bile secretion and those caused by ductal disturbances. A small amount of indirect-reacting bilirubin is always present, reflecting mild hemolysis, defective uptake and excretion, or hydrolysis of conjugated bilirubin. As hepatic conjugation and uptake of bilirubin mature, the indirect-reacting portion decreases, whereas the direct portion increases. Idiopathic neonatal hepatitis and biliary atresia together account for about 60% to 80% of all cases of conjugated hyperbilirubinemia. It is possible that similar pathogenetic mechanisms produce a spectrum of disease, with biliary atresia being the final possible, but not the inevitable, outcome. Idiopathic neonatal hepatitis is defined as prolonged conjugated hyperbilirubinemia without the apparent stigmata of a generalized viral illness, the evidence of identifiable infectious agents, or an etiologically specific metabolic abnormality. On liver biopsy, this group is characterized by extensive transformation of hepatocytes into multinucleated giant cells, and it is, therefore, sometimes referred to as neonatal giant cell hepatitis. It is caused by rupture of lateral cell membranes of adjacent hepatocytes, with consequent reduction in the number of bile canaliculi and retention of conjugated bilirubin. Necrosis of hepatocytes and inflammation are usually present, although special stains. Necrosis and inflammation may be transient, with giant hepatocytes persisting for many months or even years. Extrahepatic biliary atresia is defined as a condition in which there is luminal obliteration or apparent absence of all or segments of the extrahepatic biliary system. Differentiation between these two groups of diseases may be difficult in the early stages; however, an early accurate diagnosis is essential for the choice of proper clinical management. Unrelieved by surgery, the defect inevitably leads to death from biliary cirrhosis in the first 3 years of life. The prognosis in idiopathic neonatal hepatitis is uncertain and cannot be predicted on the basis of clinical or laboratory findings. The causes of idiopathic neonatal hepatitis and biliary atresia remain undetermined. The long-held view that biliary atresia represents a simple congenital developmental anomaly with failure of canalization is now thought untenable. In most cases, biliary atresia and neonatal hepatitis occur as isolated abnormalities, and both are considered to represent acquired conditions that may be initiated by the same or similar noxious factors. In support of the acquired nature of most cases of biliary atresia is the absence of reported cases in stillborn fetuses and the relatively rare association with other malformations. Similarly, clinical evidence of total obstruction to the flow of bile (such as acholic stools or colorless meconium) is not detected in the early stages of jaundice. The onset of acholic stools and conjugated hyperbilirubinemia is frequently delayed until 2 weeks of life or later. Injury to the structures involved in bile secretion (hepatocytes and biliary epithelium) may occur either in utero or in the perinatal period, but the consequences of such injury and, therefore, clinically manifested disease, are delayed until sometime after birth. Clinical manifestations and eventual outcome may depend on the severity and persistence of lesions in a specific location. Thus, primary injury to hepatocytes may result in clinical manifestations of neonatal hepatitis, whereas injury to major bile ducts and gallbladder may result in biliary atresia. Reovirus type 3 has been implicated as an etiologic factor in extrahepatic biliary atresia as well as in neonatal hepatitis. These studies include an experimental model in which a hepatobiliary disease bearing a strong resemblance to human biliary atresia can be induced in very young mice by infection with reovirus type 3. No studies, however, have definitively proved a role for any of the known hepatotrophic viruses including reovirus type 3 in the etiology of biliary atresia in humans. Other viruses such as cytomegalovirus and rubella virus have been implicated in intrahepatic bile duct destruction and paucity. Patients currently classified as having idiopathic neonatal hepatitis constitute a heterogeneous group that undoubtedly includes various, as yet undefined, metabolic disorders. A metabolic disorder may explain the recurrent incidence of this disease in some families. Most patients with idiopathic neonatal hepatitis or biliary atresia represent isolated cases without familial incidence or associated anomalies. Neonatal hepatitis has a familial incidence of 10% to 15%, whereas no familial cases of histologically proven extrahepatic biliary atresia have been observed. Both neonatal hepatitis and biliary atresia occur more frequently in patients with trisomy 18 than in the general population. Biliary atresia has been observed in association with the polysplenia-heterotaxia syndrome in 10% to 15% of cases. This syndrome is characterized by situs inversus of abdominal organs, intestinal malrotation, multiple spleens, centrally placed liver, and a variety of cardiac, pulmonary, and vascular malformations. Early clinical manifestations of both idiopathic neonatal hepatitis and biliary atresia may be limited to jaundice. In a small proportion of patients, especially among those who later develop neonatal hepatitis, jaundice may be apparent at birth, documented by increased concentrations of conjugated bilirubin in cord blood. No case of extrahepatic biliary atresia has ever been described in which elevation of direct-reacting bilirubin was found in the cord blood. The dark yellow staining of diapers from the presence of bilirubin in the urine often prompts the parents to seek medical advice. Splenomegaly is more frequently present in neonatal hepatitis, but this is not a constant finding. Obstruction to the flow of bile is reflected by acholic stools and may be observed in both neonatal hepatitis and biliary atresia. It is always transient and incomplete in neonatal hepatitis, but its duration is variable and may extend beyond the crucial period during which an accurate diagnosis must be established if surgical correction is needed. Routine clinical and laboratory findings usually do not distinguish between extrahepatic biliary atresia and neonatal hepatitis. A routine series of diagnostic laboratory tests is suggested, however, to establish the severity of hepatic involvement and to screen for possible causes (Box 100-6).
Daily weights and careful intake and output measurements are essential to follow volume status schedule 8 medicines purchase generic flutamide from india. In continuous venovenous hemodialysis medicine versed order 250 mg flutamide with amex, countercurrent dialysate is used rather than replacement fluid to achieve solute removal symptoms 7 days after conception buy flutamide 250mg. The main disadvantages are the need to achieve and maintain central vascular access and the need for continuous anticoagulation. Intermittent hemodialysis is a less commonly used but technically feasible mode of renal replacement therapy in the neonatal population. Hemodialysis involves intermittent 3- to 4-hour treatment periods in which fluid and solutes are rapidly removed from the infant using an extracorporeal dialyzer, with clearance achieved by the use of countercurrent dialysate. The chief advantage of hemodialysis is the ability to rapidly remove solutes and fluid, a characteristic that makes this modality the therapy of choice in neonatal hyperammonemia. Providing adequate renal replacement therapy may be limited by the challenges in placing and/or maintaining intravascular or peritoneal dialysis access in the very small premature neonate. Determination of the true incidence of neonatal hypertension is problematic, however, because of inconsistencies in the definition of hypertension, variations in blood pressure measurement techniques, and normal changes in blood pressure with gestational age and weight. Many other factors affect blood pressure readings, including the level of wakefulness, abdominal palpation, crying, and pain. Renovascular hypertension is the most frequent cause of neonatal hypertension and accounts for up to 80% to 90% of all cases. The most common cause of renovascular hypertension is renal arterial thromboembolism related to umbilical artery catheterization. Risk factors for complications from umbilical artery catheters include maternal diabetes, sepsis, dehydration, birth trauma, perinatal asphyxia, patent ductus arteriosus, and cocaine exposure. Less common causes of neonatal renovascular hypertension include congenital renal artery stenosis, fibromuscular dysplasia, midaortic coarctation, and renovascular compression by tumors. Medications such as corticosteroids, bronchodilators, phenylephrine, and bronchodilators have been associated with neonatal hypertension. Neurologic causes of hypertension include intracranial hypertension, seizures, pain, and drug withdrawal. However, because renal ultrasound in the first 72 hours of life may under- or overestimate the severity of hydronephrosis because of variations in urine output, a follow-up study is recommended. In cases of mild, unilateral disease identified on prenatal ultrasound, the postnatal study may be deferred until 2 to 4 weeks of life, assuming the infant is voiding and clinically stable. The role of prophylactic antibiotics in patients with mild or moderate disease is controversial. Voiding cystourethrography is an important adjunct to the evaluation of neonates with a history of prenatal hydronephrosis. Some have estimated that over 80% of mild cases will resolve spontaneously in the first year of life. Physiologic hydronephrosis may be caused by a delay in the maturation of the ureter, which leads to transient urinary flow obstruction. The hydronephrosis in these patients generally resolves within the first two years of life. Many clinicians advocate antibiotic prophylaxis to prevent urinary tract infection, which was shown to be effective in preventing infection in a metaanalysis of patients with high-grade hydronephrosis. Temporary relief of obstruction may be necessary and is often achieved by placement of a percutaneous nephrostomy drain. This disorder may be related to the deficient development of the distal ureter or the presence of a ureterocele. It is defined as the retrograde propulsion of urine into the upper urinary tract during bladder contraction. Vesicoureteral reflux is graded from I to V, with grade I indicating the lowest and grade V the highest. A posterior urethral valve is composed of a congenital membrane that obstructs or partially obstructs the posterior urethra. Findings on prenatal ultrasound may include hydronephrosis; dilated ureters; a thickened, trabeculated bladder; dilated proximal urethra; and oligohydramnios. The antenatal presentation may include a palpable, distended bladder, poor urinary stream, and signs and symptoms of renal and pulmonary insufficiency. Treatment is centered on securing adequate drainage of the urinary tract, initially by placement of a urinary catheter and later by primary ablation of the valves. Vesicostomy may be required in infants who show persistent obstruction and impaired urinary drainage despite ablation. Upper tract diversion is less commonly required but may be attempted in patients with markedly dilated, tortuous ureters and worsening renal function despite placement of a bladder catheter. Bladder Exstrophy-Epispadias Complex the bladder exstrophy-epispadias complex includes a spectrum of malformations that ranges from the mildest form, epispadias, through classic bladder exstrophy, to the most severe form, cloacal exstrophy, which may encompass omphalocele, bladder exstrophy, imperforate anus, and spinal defects. The nature of the specific abnormality is dependent, in large part, on the timing of the rupture of the cloacal membrane. If rupture occurs before the fourth week of gestation, cloacal exstrophy develops, whereas if rupture occurs after 6 weeks of gestation, epispadias or classic bladder exstrophy occurs. As with other congenital structural urogenital anomalies, many cases of bladder exstrophy-epispadias complex are sporadic. However, there are some reports of occurrence within families, suggesting a genetic component for this multifactorial disorder. Not all patients display all three components, and the severity of findings may be variable. The estimated incidence is 1 in 35,000 to 50,000 live births, with more than 95% of the cases occurring in boys. Although most cases occur sporadically, several reports of familial inheritance led to the identification of at least two potential causative genes (see Table 101-2), each involved in the formation or function of the bladder. Treatment in the neonatal period involves optimization of urinary tract drainage, management of renal insufficiency, and antibiotic prophylaxis. Management later in childhood may include the surgical repair of reflux, orchiopexy, reconstruction of the abdominal wall, and dialysis and/or renal transplantation. The penis appears shorter and the epispadic urethra covers the dorsum of the penis. A renal sonogram is mandatory for every infant with bladder exstrophy-epispadias complex to obtain a baseline examination of both kidneys before repair. Hip radiographs and possibly magnetic resonance imaging of the pelvis help estimate the symphysis gap and hip localization. Monogenic diseases (those with single gene defects) that may present in the newborn period include congenital nephrotic syndrome, polycystic kidney diseases, and several disorders of tubular transport. Alterations in nephrin cause disruption of the filtration barrier, leading to massive urinary protein loss and the clinical characteristics of nephrotic syndrome. Current treatment includes intravenous albumin infusions, aggressive nutritional support, correction of associated hypothyroidism and prompt treatment of infectious and thromboembolic complications. Bilateral nephrectomy is typically required for the management of massive protein loss, followed by peritoneal dialysis support and early renal transplantation. The ultrasonographic detection of placental edema, ascites, or fetal hydrops should also raise the suspicion of this disorder. Although the amniotic fluid volume is initially normal, oligohydramnios is often noted in the late second trimester. With improved care of pediatric chronic kidney disease, long-term survival has improved as well. With the long-term survival afforded by dialysis and renal transplantation, the hepatic complications have emerged as an important cause of morbidity and mortality, particularly as patients enter adulthood. However, disease cannot be definitively ruled out until at least age 30, which can be an issue because of the younger age of many parents of neonates. Newer data, however, suggest that over 90% of these patients maintain intact renal function during childhood. Thecortexisthickandspongy,andthemedullarypyramids contain grossly apparent cysts; the latter are sometimes visible radiographically. Ventilatory support is critical in neonates with pulmonary hypoplasia or respiratory embarrassment. Hypertension is often a primary concern and may require the administration of continuous intravenous infusions of several antihypertensive agents. Optimizing nutrition may be challenging owing to massively enlarged kidneys causing feeding difficulties. Unilateral nephrectomies have not been shown to improve the respiratory status but may improve feeding issues. Hepatic complications, such as portal hypertension, are typically absent in the newborn period, and synthetic function is intact. In the era of modern neonatal care, survival in the neonatal period is estimated to be about 70%. Bartter syndrome is inherited as an autosomal recessive trait; the incidence of neonatal Bartter syndrome is 1 in 50,000 to 100,000 live births. Newborn infants with neonatal Bartter syndrome typically present with profound salt wasting, polyuria, hypokalemia, and hypercalciuria. Definitive therapy for a localized renal mass begins with surgical exploration, and in most cases the primary treatment is nephrectomy. Infants with multilocular cystic nephromas or congenital mesoblastic nephromas require no postoperative therapy. Infants with malignant tumors such as Wilms tumor are treated according to well-established oncologic protocols.
References
- Vijayalakshmi IB. 'Role of Echocardiography in Rarest Congenital Heart Disease' in Journal of Indian Academy of Echocardiography. 2003;7:509-12.
- ACOG. Committee opinion: number 278, November 2002.
- Warnock DG. Renal genetic disorders related to K+ and Mg2+. Annu Rev Physiol. 2002;64:845-876.
- Baskin LS, Erol A, Li YW, et al: Anatomical studies of the human clitoris, J Urol 162(3 Pt 2):1015-1020, 1999.
- Choussat, Fontan A, Besse P: Selection criteria for Fontan's procedure. In Anderson RH, Shinebourne EA, editors: Pediatric cardiology, Edinburgh, 1978, Churchill Livingstone. 131.
- Hochman JS, McCabe CH, Stone PH, et al. Outcome and profile of women and men presenting with acute coronary syndromes: a report from TIMI IIIB. TIMI Investigators. Thrombolysis in Myocardial Infarction. J Am Coll Cardiol 1997;30:141-148.
- Makris D, Moschandreas J, Damianaki A, et al. Exacerbations and lung function decline in COPD: new insights in current and ex-smokers. Respir Med 2007; 101: 1305-1312.
- Cappuzzo F, Janne PA, Skokan M, et al. MET increased gene copy number and primary resistance to gefitinib therapy in non-small-cell lung cancer patients. Ann Oncol 2009;20:298-304.