Glenn M. Weinraub, DPM, FACFAS
- The Permanente Medical Group
- Department of Orthopaedic Surgery
- Fremont/Hayward, California
- Clinical Associate Professor
- Midwestern University, School of Podiatric Medicine
- Glendale, Arizona
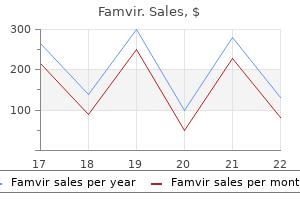
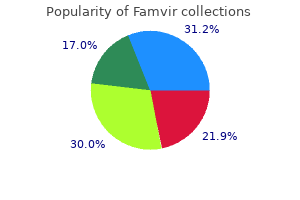
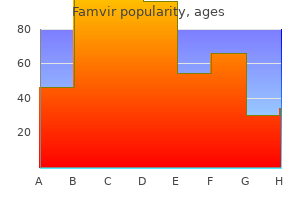
Without dissent antiviral young living oils discount 250mg famvir amex, on October 10 joint infection hiv buy discount famvir 250 mg on-line, 1962 hiv infection symptoms in hindi purchase famvir 250 mg without prescription, the KefauverHartis Drug Amendments to the Food hiv infection rates south africa purchase genuine famvir, Drug antiviral used for cold sores cheap 250mg famvir free shipping, and Cosmetic Act of 1938 were passed by both houses of Congress. The Comprehensive Drug Abuse Prevention and Control Act of 1970 established five "schedulesn for the classification and control of drug substances that are subject to abuse. These schedules provide for decreasing levels of control, from schedule I to schedule V. In this category are morphine, cocaine, methamphetamine, amobarbital, and other such drugs. In this category are specified quantities of codeine, hydrocodone, and similar agents. In this category are specified quantities of difenoxin, diazepam, oxazepam, and similar agents. Included in this category are specified quantities of dihydrocodeine, diphenoxylate, and similar agents. The pregnancy categories A, B, C, D, and X are removed from all human prescription drug and biological product labeling. The requirement now is that the labeling includes a summary of the risks of using a drug during pregnancy and lactation, a discussion of the data supporting that summary, and relevant information to help health care providers make prescribing decisions and counsel women about the use of drugs during pregnancy and lactation. The labeling also includes relevant information about pregnancy testing, contraception, and infertility for health care providers prescribing for females and males of reproductive potential. It creates a consistent format for providing information about the risks and benefits of prescription drug and/or biological product use during pregnancy and lactation and by females and males of reproductive potential. Medication Exposures During Pregnancy and Lactation Every woman in the general population has a 3% to 5% risk of having a child with a birth defect or mental retardation. Two important factors to consider when assessing the teratogenic potential of a medication are the stage of pregnancy at which the exposure occurred and the amount of medication taken. It is critical to evaluate each exposure on a case-by-case basis in order to give an accurate risk assessment. In a pregnant or breast-feeding patient who is currently taking, or considering taking, a medication, the patient needs to be counseled about potential adverse effects the medication could have on her fetus or infant (11). All foreign drug manufacturing and distributing firms whose products are imported into the United States are also included in this regulation. Exempt from the registration and listing requirements are hospitals, clinics, and the various health practitioners who compound pharmaceutical preparations for use in their respective institutions and practices. Also exempt are research and teaching institutions in which drug products are prepared for purposes other than sale. Under this system, the first four numbers, the labeler code of the 10-character code, identify the manufacturer or distributor. The last six numbers identify the drug formulation and the trade package size and type. The segment that identifies the drug formulation is the product code, and the segment that identifies the trade package size and type is the package code. The manufacturer or distributor determines the ratio of use of the last six digits for the two codes, as a 3:3 digit product code to package code configuration. Only one such type of configuration may be selected for use by a manufacturer or distributor, who then assigns a code number to each product to be included in the drug listing. Even when a drug manufacturer discontinues the manufacture and distribution of a product, the number may not be used again. It also prohibits resale by health care institutions of Orphan Drug Ad of 1983 Drugs intended for the treannent of "rare diseases and conditions" may be designated orphan drugs to help promote research on rare diseases. The law provides tax credits and designated years of marketing exclusivity as incentives. This reduces considerably the time and expense of bringing a generic version of the drug to market. In 2014, the unbranded generics dispensed in the United States were about 82% and the branded generics 5. The act is intended to reduce the risks of adulterated, misbranded, repackaged, or mislabeled drugs entering the legitimate marketplace through "secondary sources. Reimportation: Prohibits the reimportation of drug pharmaceuticals purchased explicitly for the use of the institution. Charitable institutions that receive drugs at reduced prices or no cost cannot resell the drugs. Distribution of samples: Samples may be distributed only to (a) practitioners licensed to prescribe such drugs and, (b) at the written request of the practitioner, to pharmacies of hospitals or other health care institutions. Wholesale distributors: Manufacturers are required to maintain a list of their authorized distributors. The Act is credited with a more rapid application review process and the speedier approval of new drug products. The third enacnnent, passed as part of the "Public Health Security and Bioterrorism Preparedness and Response Act of 2002," included designated resources for postmarketing studies to monitor the continuing safety and efficacy of new drug products. The act forbids manufacturers or distributors of these products to make any advertising or labeling claims that indicate that the use of the product can prevent or cure a specific disease. In fact, a disclaimer must appear on the product: "This product is not intended to diagnose, treat, cure, or prevent any disease. Sales restrictions: Prohibits selling, trading, purchasing, or the offer to sell, trade, or purchase a drug sample. Presidential Conunission on Dietary Supplement Labels called for more research in this country on the health benefits ofdietary supplements. Also, the statute further prohibits any product from being granted more than one period of data exclusivity unless a manufacturer modifies an approved product to produce a change in safety, purity, or potency. In this case, the modified product would be considered a new product and would be entitled to new data exclusivity of 12 years. The outbreak of fungal meningitis occurred in 2012 and was traced to fungal contamination in three lots of compounded methylprednisolone suspension for epidural steroid injections. It establishes requirements for 503a traditional compounding pharmacies and for 503b outsourcing facilities. Data indicate that 80% of the active pharmaceutical ingredients used in the manufacture of pharmaceutical products and 40% of the finished dosage forms used in the United States are imported (16). It should be noted that the activities of the United States Pharmacopeia are also worldwide in scope nowadays, with physical operations in key international manufacturing and distribution sites. A practitioner also has a responsibility to report a problem with any drug product or medical device using the MedWatch program. Reported problems may include product defects, product adulteration, container leakage, improper labeling, unexpected adverse reactions, and others. Drug Products Removed or Withdrawn the following drug products were withdrawn or removed from the market because such drug products or components of such drug products were found to be unsafe or not effective. Thus, the products, as listed may not be compounded under the provisions of section 503A(a) of the Federal Food, Drug, and Cosmetic Act. It is important to note that not all dosage forms of the drugs listed have been removed or cannot be compounded because in some situations, it is select dosage forms. The PharmD degree includes the internship experiences within the curriculum during the final year of the program and is still a total of 6 years education/training. Under this format, all pharmacists in the states where this has been implemented can be called doctors as are those who have earned the PharmD degree; one is a professional degree designation and the other a licensure designation. Most pharmacists practice within an ambulatory care or community pharmacy setting. As members of the health care team, pharmacists serve as an expert source of drug information and participate in the selection, monitoring, and assessment of drug therapy. For most of its history as a profession, pharmacy was relatively undifferentiated. The emergence of some practice differentiation occurred in the late 1960s and early 1970s with the professional literature describing hospital pharmacists who had developed unique roles that were distinctive from the traditional dispensing roles of the pharmacist. The "clinical pharmacists" associated with physicians in therapeutic decision-making, and it was suggested that their level of knowledge and practice skills required special preparation. Further, hospital pharmacists were encouraged to organize their departments to recognize and utilize these emerging "specialties" and proposed that the medical model of service organization might be applicable to pharmacy. Its 1975 report acknowledged that differentiation in pharmacy practice was occurring and that this differentiation was, in general, expected and desirable. While not specifying specialty practice areas, the commission suggested that a structure be established to oversee all pharmacist credentialing. Currently, there are eight specialty areas as follows: ambulatory care, critical care, nuclear, nutrition support, oncology, pediatric, pharmacotherapy, and psychiatric pharmacy. In recent years, managed health care programs have grown extraordinarily and managed health care organizations have enrolled a large and growing base of patients and thus have assumed major responsibilities in the delivery of health care, including the delivery of pharmaceutical services. In these functions, managed care pharmacists apply administrative, epidemiological, clinical, financial, research, information technology, and communication skills in their practice. A number of pharmacy graduates, particularly those having an interest in institutional practice, participate in postgraduate residency and/or fellowship programs to enhance their practice and/or research skills. A pharmacy residency is an organized, directed postgraduate training program in a defined area of practice. The chief purpose is to train pharmacists in professional practice and management skills. A fellowship to develop skill in research is a directed, highly individualized postgraduate program designed to prepare the participant to become an independent researcher. Both pharmacy residencies and fellowships last 12 months or longer and require the close direction of a qualified preceptor. In government service, pharmacists perform professional and administrative functions in the development and implementation of pharmaceutical care delivery programs and in the design and enforcement of regulations involving drug distribution and drug quality standards. Career opportunities for pharmacists in government service at the federal level include positions in the military service, in the U. Some pharmacists work full-time in the academic setting, whereas many others provide parttime professional instruction in community or hospital pharmacies, teaching hospitals and clinics, drug information centers, nursing homes and extended care facilities, health departments, home health care, managed care, and other areas in which pharmaceutical services are delivered. A number ofpharmacists serve their profession in volunteer or professional positions with local, state, and national pharmaceutical associations. Pharmacists exercise a vital service health education role in their communities through participation in drug and health education community forums, by conducting "brown bag" sessions, by speaking on drug issues in schools, by conducting in-service education programs in patient care settings, and by providing input on drug and health issues to state and federal legislators and community leaders and officials. Together with applicable federal laws, they constitute the basis for the legal practice of pharmacy. Over the years, various professional associations in pharmacy have developed documents termed standards of practice. In general, establishes and administers pharmacy management, personnel, and fiscal policy. Implicit in all of these statements is the requirement of pharmacists to participate fully in all aspects of medication distribution (manufactured and compounded drugs) and their appropriate clinical use to achieve optimal therapeutic outcomes. The developed classification is intended to provide the common language to be used and understood within and outside of the profession in describing the practice activities of pharmacists. The statute was designed to ensure that prescriptions are appropriate, medically necessary, and not likely to result in adverse medical effects. Pharmacists are to maintain patient medication profiles and therapeutic counseling records. However, it should be mentioned that no reimbursement was defined in these new responsibilities. Many states used the model regulations for the practice of pharmaceutical care developed by the National Association of Boards of Pharmacy. This Code, prepared and supported by pharmacists, is intended to state publicly the principles that form the fundamental basis of the roles and responsibilities of pharmacists. These principles, based on moral obligations and virtues, are established to guide pharmacists in relationships with patients, health professionals, and society. A pharmacist respects the covenantal relation- ship between the patient and pharmacist. Considering the patient-pharmacist relationship as a covenant means that a pharmacist has moral obligations in response to the gift of trust received from society. In return for this gift, a pharmacist promises to help individuals achieve optimum benefit from their medications, to be committed to their welfare, and to maintain their trust. A pharmacist promotes the good of every patient in a caring, compassionate, and confidential manner. A pharmacist places concern for the well-being of the patient at the center of professional practice. In doing so, a pharmacist considers needs stated by the patient as well as those defined by health science. A pharmacist is dedicated to protecting the dignity of the patient With a caring attitude and a compassionate spirit, a pharmacist focuses on serving the patient in a private and confidential manner. A pharmacist promotes the right of self-determination and recognizes individual self-worth by encouraging patients to participate in decisions about their health. In all cases, a pharmacist respects personal and cultural differences among patients. A pharmacist has a duty to tell the truth and to act with conviction of conscience. A pharmacist avoids discriminatory practices, behavior or work conditions that impair professional judgment, and actions that compromise dedication to the best interests of patients. Among its many provisions are expanded prescription drug coverage for Medicare and Medicaid patients, programs for innovative methods of health care delivery, and a pathway for the approval of biosimilars (generic biological products) (42). A pharmacist has a duty to maintain knowledge and abilities as new medications, devices, and technologies become available and as health information advances. A pharmacist respects the values and abilities of colleagues and other health professionals.
In a patient with a prior history of pancreatitis hiv infection rates by population buy famvir 250 mg overnight delivery, this finding is consistent with a pseudocyst anti viral apps order 250 mg famvir with amex. A hiv infection rates manchester generic 250 mg famvir with visa, Axial contrast-enhanced computed tomography scan shows a large pancreatic body mass (arrowhead) with distal ductal dilation (open arrow) antiviral infection definition famvir 250mg with amex. Because the pain of acute herpes zoster may precede the rash by 3 to 7 days hiv infection and aids symptoms discount famvir online mastercard, it may erroneously be attributed to chronic pancreatitis in patients who have had previous bouts of the disease. In addition, the clinician should always consider the possibility of malignant pancreatic disease. TreaTmenT the initial management of chronic pancreatitis focuses on alleviating pain and treating malabsorption. As with acute pancreatitis, the pancreas is allowed to rest by giving the patient nothing by mouth to decrease serum gastrin secretion and, if ileus is present, instituting nasogastric suction. If ileus is present, a parenteral opioid such as meperidine is a good alternative. The use of opioid analgesics must be monitored carefully, because the potential for misuse and dependence is high. Alternatively, continuous thoracic epidural block with local anesthetic, opioid, or both may provide adequate pain control and allow the patient to avoid the respiratory depression associated with systemic opioid analgesics. Hypovolemia should be treated aggressively with crystalloid and colloid infusions. For prolonged cases of chronic pancreatitis, parenteral nutrition is indicated to avoid malnutrition. If opioids are used, the clinician must constantly watch for overuse and dependence, especially if the underlying cause of the chronic pancreatitis is alcohol abuse. Correct diagnosis is necessary to treat this painful condition properly and to avoid overlooking serious extrapancreatic complications. The judicious use of opioid analgesics is usually adequate to control the pain of acute exacerbations. Ilioinguinal neuralgia is caused by compression of the ilioinguinal nerve, and the most common causes of compression are traumatic injury to the nerve, including direct blunt trauma and damage during inguinal herniorrhaphy and pelvic surgery. The ilioinguinal nerve is a branch of the L1 nerve root, with a contribution from T12 in some patients. The nerve follows a curvilinear course that takes it from its origin at the L1 (or occasionally T12) somatic nerves to inside the concavity of the ileum. The ilioinguinal nerve continues anteriorly to perforate the transverse abdominal muscle at the level of the anterior superior iliac spine. The nerve may interconnect with the iliohypogastric nerve as it continues to pass along its course medially and inferiorly, where it accompanies the spermatic cord through the inguinal ring and into the inguinal canal. The distribution of the sensory innervation of the ilioinguinal nerves varies from patient to patient, and overlap with the iliohypogastric nerve may be considerable. In general, the ilioinguinal nerve provides sensory innervation to the skin of the upper inner thigh and the root of the penis and upper scrotum in men or the mons pubis and lateral labia in women. Plain radiographs of the hip and pelvis are indicated in all patients who present with ilioinguinal neuralgia, to rule out occult bony disease. Further, significant variability exists in the anatomy of SignS and SympTomS Ilioinguinal neuralgia manifests as paresthesias, burning pain, and occasionally numbness over the lower abdomen that radiates into the scrotum or labia and occasionally into the upper inner thigh; pain does not radiate below the knee. If the condition remains untreated, progressive motor deficit, consisting of bulging of the anterior abdominal wall muscles, may occur. Physical findings include sensory deficit in the inner thigh, scrotum, or labia in the distribution of the ilioinguinal nerve. Therefore, the ice ball produces a white (hyperechoic) surface reflex and a shadow behind it. TreaTmenT Initial treatment of ilioinguinal neuralgia consists of simple analgesics, nonsteroidal antiinflammatory drugs, or cyclooxygenase-2 inhibitors. Pharmacologic treatment is usually disappointing, however, in which case ilioinguinal nerve block with local anesthetic and steroid is required. The anterior superior iliac spine is identified by palpation, and a point 2 inches medial and 2 inches inferior to it is identified and prepared with antiseptic solution. A total of 5 to 7 mL of 1% preservative-free lidocaine in solution with 40 mg methylprednisolone is injected in a fanlike manner as the needle pierces the fascia of the external oblique muscle. Care must be taken not to insert the needle too deeply, which risks entering the peritoneal cavity and perforating the abdominal viscera. Because of the overlapping innervation of the ilioinguinal and iliohypogastric nerves, it is usually not necessary to block branches of each nerve. After injection of the solution, pressure is applied to the injection site to decrease the incidence of ecchymosis and hematoma formation, which can be quite dramatic, especially in anticoagulated patients. Because of the anatomy of the ilioinguinal nerve, damage to or entrapment of the nerve anywhere along its course can produce a similar clinical syndrome. Therefore, a careful search for pathologic processes at the T12-L1 spinal segments and along the path of the nerve in the pelvis is mandatory in all patients who present with ilioinguinal neuralgia without a history of inguinal surgery or trauma to the region. The major complications of ilioinguinal nerve block are ecchymosis and hematoma formation. If the needle is too deep and enters the peritoneal cavity, perforation of the colon may result in the formation of an intraabdominal abscess and fistula. Clinical Pearls Ilioinguinal neuralgia is a common cause of lower abdominal and pelvic pain, and ilioinguinal nerve block is a simple technique that can produce dramatic pain relief. If a patient presents with pain suggestive of ilioinguinal neuralgia and does not respond to ilioinguinal nerve block, a lesion more proximal in the lumbar plexus or an L1 radiculopathy should be considered. It may be caused by compression of or damage to the genitofemoral nerve anywhere along its path. The most common causes of genitofemoral neuralgia involve traumatic injury to the nerve, including direct blunt trauma and damage during inguinal herniorrhaphy and pelvic surgery. The genitofemoral nerve arises from fibers of the L1 and L2 nerve roots and passes through the substance of the psoas muscle, where it divides into a genital and a femoral branch. The femoral branch passes beneath the inguinal ligament, along with the femoral artery, and provides sensory innervation to a small area of skin on the inner thigh. The genital branch passes through the inguinal canal to provide innervation to the round ligament of the uterus and labia majora in women. In men, the genital branch passes with the spermatic cord to innervate the cremasteric muscles and provide sensory innervation to the bottom of the scrotum. The pain of genitofemoral neuralgia is made worse by extension of the lumbar spine, which puts traction on the nerve. Plain radiographs of the hip and pelvis are indicated in all patients who present with genitofemoral neuralgia, to rule out occult bony disease. Further, significant variability exists in the anatomy of the genitofemoral nerve and can result in significant variation in the clinical presentation. Pubic tubercle figure 75-2 Correct needle placement for genitofemoral nerve block. Pharmacologic treatment is usually disappointing, however, in which case genitofemoral nerve block with local anesthetic and steroid is required. The genital branch of the genitofemoral nerve is blocked as follows: the pubic tubercle is identified by palpation, and a point just lateral to it is identified and prepared with antiseptic solution. A total of 3 to 5 mL of 1% preservative-free lidocaine in solution with 80 mg methylprednisolone is injected in a fanlike manner as the needle pierces the inguinal ligament. Care must be taken not to insert the needle deeply enough to enter the peritoneal cavity and perforate the abdominal viscera. The femoral branch of the genitofemoral nerve is blocked by identifying the middle third of the inguinal ligament. Care must be taken not to enter the femoral artery or vein or to block the femoral nerve inadvertently. The needle must be kept in a subcutaneous position to avoid entering the peritoneal cavity and perforating the abdominal viscera. If the patient has an inflammatory component to the pain, the local anesthetic is combined with 80 mg methylprednisolone and injected in incremental doses. Subsequent daily nerve blocks are carried out in a similar manner, by substituting 40 mg methylprednisolone for the initial 80-mg dose. Because of overlapping innervation of the ilioinguinal and iliohypogastric nerves, it is usually not necessary to block branches of each nerve during genitofemoral nerve block. For patients who do not rapidly respond to genitofemoral nerve block, consideration should be given to epidural steroid injection of the L1-2 segments. CompliCaTionS and piTfallS Because of the anatomy of the genitofemoral nerve, damage to or entrapment of the nerve anywhere along its course can produce a similar clinical syndrome. Therefore, a careful search for pathologic processes at the L1-2 spinal segments and along the path of the nerve in the pelvis is mandatory in all patients who present with genitofemoral neuralgia without a history of inguinal surgery or trauma to the region. The major complications of genitofemoral nerve block are ecchymosis and hematoma formation. If a patient presents with pain suggestive of genitofemoral neuralgia and does not respond to genitofemoral nerve block, lesions more proximal in the lumbar plexus or an L1 radiculopathy should be considered. In addition to pain, patients may experience numbness, weakness, and loss of reflexes. The causes of lumbar radiculopathy include herniated disk, foraminal stenosis, tumor, osteophyte formation, and, rarely, infection. This condition represents a neurosurgical emergency and should be treated as such. Radionuclide bone scanning and plain radiography are indicated if fracture or a bony abnormality, such as metastatic disease, is being considered. If the diagnosis of lumbar radiculopathy is in question, laboratory testing consisting of a complete blood count, erythrocyte sedimentation rate, antinuclear antibody testing, human leukocyte SignS and SympTomS Patients suffering from lumbar radiculopathy complain of pain, numbness, tingling, and paresthesias in the distribution of the affected nerve root or roots (Table 76-1). Patients may also note weakness and lack of coordination in the affected extremity. Muscle spasms and back pain, as well as pain referred into the buttocks, are common. Pain syndromes that may mimic lumbar radiculopa- TreaTmenT Lumbar radiculopathy is best treated with a multimodality approach. Physical therapy, including heat modalities and deep sedative massage, combined with nonsteroidal antiinflammatory drugs and Lumbar n. A, With the patient in the supine position, the unaffected leg is flexed 45 degrees at the knee, and the affected leg is placed flat against the table. B, With the ankle of the affected leg placed at 90 degrees of flexion, the affected leg is slowly raised toward the ceiling while the knee is kept fully extended. If necessary, caudal or lumbar epidural nerve blocks can be added; nerve blocks with local anesthetic and steroid are extremely effective in the treatment of lumbar radiculopathy. CompliCaTionS and piTfallS Failure to diagnosis lumbar radiculopathy accurately may put the patient at risk for the development of lumbar myelopathy, which, if untreated, may progress to paraparesis or paraplegia. Further, lumbar radiculopathy and tibial nerve entrapment may coexist in the double-crush syndrome. The latissimus dorsi muscle originates on the spine of T7; the spinous processes and supraspinous ligaments of all lower thoracic, lumbar, and sacral vertebrae; the lumbar fascia; the posterior third iliac crest; the last four ribs; and the inferior angle of the scapula. The muscle inserts on the bicipital groove of the humerus and is innervated by the thoracodorsal nerve. Blunt trauma to the muscle may also incite latissimus dorsi myofascial pain syndrome. In addition, involuntary withdrawal of the stimulated muscle, called a jump sign, often occurs and is also characteristic of myofascial pain syndrome. In spite of this consistent physical finding, the pathophysiology of the myofascial trigger point remains elusive, although trigger points are believed to be the result of microtrauma to the affected muscle. This trauma may result from a single injury, repetitive microtrauma, or chronic deconditioning of the agonist and antagonist muscle unit. In addition to muscle trauma, various other factors seem to predispose patients to develop myofascial pain syndrome. For instance, a weekend athlete who subjects his or her body to unaccustomed physical activity may develop myofascial pain syndrome. The latissimus dorsi muscle seems to be particularly susceptible to stress-induced myofascial pain syndrome. The clinician must rule out other coexisting disease processes that may mimic latissimus dorsi syndrome, including primary inflammatory muscle disease, multiple sclerosis, and collagen vascular disease. The use of electrodiagnostic and radiographic testing can identify coexisting pathologic processes such as subscapular bursitis, cervical radiculopathy, herniated nucleus pulposus, and rotator cuff tear. The clinician must also identify coexisting psychological and behavioral abnormalities that may mask or exacerbate the symptoms of latissimus dorsi syndrome. It is hoped that interrupting the pain cycle in this way will allow the patient to obtain prolonged pain relief. Because of the lack of objective diagnostic testing, the clinician must rule out other coexisting disease processes that may mimic latissimus dorsi syndrome (see "Differential Diagnosis"). For patients who do not respond to these traditional measures, consideration should be given to the use of botulinum toxin type A; although not currently approved by the Food and Drug Administration for this indication, the injection of minute quantities of botulinum toxin type A directly into trigger points has been successful in the treatment of persistent latissimus dorsi syndrome. Special care must be taken to avoid pneumothorax during injection of trigger points in proximity to the underlying pleural space.
Endocervical adenocarcinoma with morphologic features of both usual and gastric types: Clinicopathologic and immunohistochemical analyses and high-risk detection by in situ hybridization hiv infection gas station buy cheap famvir 250 mg. Absence of human papillomavirus infection in minimal deviation adenocarcinoma and lobular endocervical glandular hyperplasia anti viral cleanse and regimen reviews buy famvir 250mg line. Endocervical adenocarcinomas with prominent endometrial or endomyometrial involvement simulating primary endometrial carcinomas antiviral zovirax purchase famvir paypal. Mucinous tumors of the ovary associated with mucinous adenocarcinomas of the cervix: A clinicopathologic analysis of 16 cases hiv gi infection purchase cheap famvir. Well-differentiated villoglandular adenocarcinoma of the uterine cervix: Oncogene/tumor suppressor gene alterations and human papillomavirus genotyping hiv symptoms of infection discount 250 mg famvir with mastercard. Well differentiated villoglandular adenocarcinoma of uterine cervix: A clinicopathological study of 24 cases. Adenocarcinoma of the uterine cervix with predominantly villoglandular papillary growth pattern. Villoglandular adenocarcinoma of the cervix: Clarity is needed on the histological definition for this difficult diagnosis. Villoglandular papillary adenocarcinoma of the uterine cervix: A clinicopathological analysis of 13 cases. Clinicopathologic features of villoglandular papillary adenocarcinoma of the uterine cervix. Primary signet-ring cell carcinoma of the cervix: Case report and review of the literature. Colloid carcinoma of the uterine cervix: A case report with respect to immunohistochemical analyses. Signet-ring cells in squamous cell carcinoma of the cervix and in non-neoplastic ectocervical epithelium. Adenocarcinoma of the uterine cervix of intestinal type containing numerous Paneth cells. Pseudomyxoma-type invasion in gastrointestinal adenocarcinomas of endometrium and cervix: A report of 2 cases. Histopathologic subtyping of cervical adenocarcinoma reveals increasing incidence rates of endometrioid tumors in all age groups. Minimal-deviation endometrioid adenocarcinoma of the cervix: A case report with ultrastructural analysis demonstrating abnormal ciliation of the tumor cells. Endometrial endometrioid adenocarcinoma of the uterine corpus involving the cervix: Some cases probably represent independent primaries. Minimal deviation endometrioid adenocarcinoma of cervix: A clinicopathological and immunohistochemical study of two cases. Minimal-deviation endometrioid adenocarcinoma of the uterine cervix: A report of five cases of a distinctive neoplasm that may be misinterpreted as benign. Malignant mesonephric tumors of the female genital tract: A clinicopathologic study of 9 cases. Mixed mesonephric adenocarcinoma and high-grade neuroendocrine carcinoma of the uterine cervix: Case description of a previously unreported entity with insights into its molecular pathogenesis. Mesonephric neoplasms of the uterine cervix: A report of eight cases, including four with a malignant spindle cell component. Mesonephric adenocarcinomas of the uterine cervix: A study of 11 cases with immunohistochemical findings. Clear cell carcinoma of the uterine cervix presented (sic) as submucosal tumor arising from a background of cervical endometriosis. Clear cell carcinoma of the cervix with choriocarcinomatous differentiation: Report of an extremely rare phenomenon associated with mismatch repair protein abnormality. Clear cell carcinoma of the uterine cervix: A clinical and pathological analysis of 47 patients without intrauterine diethylstilbestrol exposure. Adenosquamous carcinoma versus adenocarcinoma in early-stage cervical cancer patients undergoing radical hysterectomy: An outcomes analysis. Clear cell adenosquamous carcinoma of the cervix: An aggressive tumor associated with human papillomavirus-18. Adenosquamous carcinoma of the cervix: Prognosis in early stage disease treated by radical hysterectomy. Prevalence, distribution, and viral burden of all 15 high-risk human papillomavirus types in adenosquamous carcinoma of the uterine cervix: A multiplex real-time polymerase chain reaction-based study. Familial papillary serous carcinoma of the cervix, peritoneum, and ovary: A report of the first case. Invasive micropapillary carcinoma of the uterine cervix: Case report of a rare entity. Papillary serous carcinomas of the uterine cervix and paraneoplastic cerebellar degeneration: a report of two cases. Papillary serous carcinoma of the uterine cervix: A clinicopathologic study of 17 cases. Is there really a difference in survival of women with squamous cell carcinoma, adenocarcinoma, and adenosquamous carcinoma Cervical carcinomas with a micropapillary component: A clinicopathologic study of 8 cases. Adenoid basal carcinoma of the uterine cervix: Report of two cases with reference to adenosquamous carcinoma. Adenoid cystic carcinoma of the uterine cervix: A tumor with myoepithelial and neuroendocrine differentiation. A reappraisal of "basaloid carcinoma" of the cervix, and the differential diagnosis of basaloid cervical neoplasms. Incidence, histology, and response to radiation of mixed carcinomas (adenoacanthomas) of the uterine cervix. Glassy cell carcinoma of the uterine cervix: Histochemical, immunohistochemical, and molecular genetic characteristics. Glassy cell carcinoma predominantly commits to a squamous lineage and is strongly associated with high-risk type human papillomavirus infection. Adenoid basal carcinoma of the cervix: A unique morphological evolution with cell cycle correlates. The origin and molecular characterization of adenoid basal carcinoma of the uterine cervix. Terminology of endocrine tumors of the uterine cervix: Results of a workshop sponsored by the College of American pathologists and the National Cancer Institute. Small cell neuroendocrine carcinoma of the uterine cervix: A review of 226 cases with emphasis on patterns of growth and immunohistochemical features. Prognostic factors in neuroendocrine small cell cervical carcinoma: A multivariate analysis. Small cell carcinoma of the cervix: A clinicopathologic and immunohistochemical study of 23 cases. Cervical carcinomas with neuroendocrine differentiation: A report of 28 cases with immunohistochemical analysis and molecular genetic evidence of 157. Neuroendocrine carcinoma of the cervix: Review of a series of cases and correlation with outcome. Small-cell undifferentiated carcinoma of the cervix: A clinicopathologic, ultrastructural, and immunocytochemical study of 15 cases. Mixed small cell carcinoma of the uterine cervix: Prognostic impact of focal neuroendocrine differentiation but not of Ki-67 labeling index. Small cell neuroendocrine carcinomas of the uterine cervix: A histological, immunohistochemical, and molecular genetic study. Neuroendocrine carcinoma of the uterine cervix: the role of multimodality therapy in early-stage disease. Large cell neuroendocrine carcinoma of the cervix: Prognostic factors and survival advantage with platinum chemotherapy. Large cell neuroendocrine carcinoma of the uterine cervix: A clinicopathologic study of 12 cases. Detection of human papillomavirus in large cell neuroendocrine carcinoma of the uterine cervix: a study of 12 cases. Large cell neuroendocrine carcinoma of the cervix associated with intestinal variant (of) invasive mucinous adenocarcinoma. Large cell neuroendocrine carcinoma of the uterine cervix with cytogenetic analysis by comparative genomic hybridization: A case study. Spectrum of neuroendocrine carcinomas of the uterine cervix, including histopathologic features, terminology, immunohistochemical profile, and clinical outcomes in a series of 50 cases from a single institution in India. Large cell neuroendocrine carcinoma of the uterine cervix: A clinicopathologic study of six cases. Cervical carcinoma with divergent neuroendocrine and gastrointestinal differentiation. Monoclonality of composite large-cell neuroendocrine carcinoma and invasive intestinal-type mucinous adenocarcinoma of the cervix: A case study. Large cell neuroendocrine carcinoma Albores-Saavedra J, Martinez-Benitez B, Luevano E. Compact, densely cellular nests of degenerating endometrial stromal cells with scanty cytoplasm and small, sometimes spindled, hyperchromatic nuclei are characteristic of menstrual endometrium, and have been mistaken for small cell carcinoma. Other typical findings include neutrophils, nuclear debris, syncytial papillary change (see corresponding heading below), and fibrin thrombi. Features distinguishing menstrual changes from abnormalities include the fragmented and degenerative appearance of the epithelium and stroma, common residual secretory changes, and the absence of nuclear atypicality and mitotic activity other than that acceptable for a reactive process. Menstrual endometrium can rarely be found within myometrial vessels, potentially mimicking intravascular carcinoma. Left and center: Note fragmented glands, compacted aggregates of degenerating stromal cells, neutrophils, and blood. Cytotrophoblast and syncytiotrophoblaste a Endometrioid Endometrioid Endometrioid Endometrioid Endometrioid Endometrioid Endometrioid Endometrioid or squamous cell Endometrioid Endometrioid Villoglandular endometrioid or serous Mucinous Mucinous Serous Serous or clear cell Serous or clear cell Clear cell Small cell Undifferentiated Undifferentiated Undifferentiated or signet-ring cell Undifferentiated Undifferentiated Squamous cell carcinoma or undifferentiated Undifferentiated or giant cell Telescoping is more likely to be confused with hyperplasia than carcinoma. Similar changes may be found within fragments of endocervical polyps procured during an endometrial sampling. Cervical microglandular hyperplasia or even crowded aggregates of endocervical glands with or without squamous metaplasia can also be associated with diagnostic problems if the fragments are not recognized as endocervical in origin. This finding in biopsy or curettage fragments can suggest an endometrial stromal neoplasm or a small cell carcinoma. The scant tissue, atrophic appearance, and mitotic inactivity facilitate the diagnosis. The surface epithelium in an atrophic endometrium may show nuclear atypia and/or enlargement that may cause concern for intraepithelial serous carcinoma but in the former severe nuclear atypia and mitotic activity are absent. There is often eosinophilic cytoplasm, a subtle distinction from most cases of minimal volume (intraepithelial) serous carcinoma. Furthermore, atypia in the setting of atrophy would demonstrate a wild-type p53 staining pattern and low proliferative index by Ki-67, whereas serous carcinoma would show an abnormal p53 pattern (diffuse overexpression or complete loss) with increased proliferation. A sampling from an atrophic endometrium often yields only scanty strips of endometrial surface epithelium. Left: Focal nuclear enlargement and hyperchromasia are seen in the epithelial fragment at the top of the figure. Wild-type p53 expression (center panel) and very focal ki-67 staining (right panel) indicate a non-neoplastic process. This appearance can be misinterpreted as a complex hyperplasia or carcinoma, especially if the glands are proliferative with mitotic activity. Strips of endometrial surface epithelium can become coiled and compacted, producing a pseudopapillary pattern. This finding is often associated with an atrophic endometrium, but its appearance can be misconstrued as papillary hyperplasia or carcinoma. Postcurettage epithelial atypia, which may be striking, is typically confined to the surface epithelium and superficial glands. The reactive cells may have enlarged hyperchromatic nuclei with occasionally prominent nucleoli and sometimes a hobnail appearance (Table 7. The characteristic eosinophilic cytoplasm and focal stromal breakdown are also seen. Small tufts of cells with abundant eosinophilic cytoplasm are intermixed with aggregates of stroma showing breakdown. Glandular and surface epithelia, including those of polyps (especially those with papillary proliferations, see corresponding heading), may be involved. As metaplasias often reflect unopposed estrogen stimulation, metaplastic glands may be synchronously hyperplastic or associated with a synchronous typical endometrial hyperplasia or adenocarcinoma. Other etiologic factors are considered under the specific types of metaplasia (including syncytial papillary change) in the following sections. It is typically associated with postovulatory or anovulatory menstrual bleeding but may occur within or on the surface of an infarcted polyp. The appearance varies with its extent, the degree of its syncytial and papillary features, and the prominence of the associated stromal breakdown. The endometrial surface epithelium and less commonly the superficial glands are involved. This example shows a predominantly plaque-like proliferation with only limited papillarity. Center: Stroma free papillae are composed of syncytial eosinophilic cells with bland nuclear features; nuclear debris is also present. The cells usually have bland nuclear features but occasionally show reactive atypia, a hobnail appearance, and rare mitoses. Other menses-related changes (see separate heading) are often present, including neutrophils, nuclear debris, small nests of degenerating endometrial stromal cells, and thrombosed sinusoids. The papillarity, occasional cytologic atypia, mitoses, and p16 positivity may suggest a papillary carcinoma, especially serous carcinoma.

The needle is then carefully advanced at that point through the skin antiviral medication for warts cheap famvir express, subcutaneous tissues antiviral coconut oil purchase 250 mg famvir otc, muscle antiviral skin ointment purchase discount famvir, and tendon until it impinges on the bone of the ischial tuberosity hiv infection long term effects cheap famvir 250 mg without prescription. Care must be taken to keep the needle in the midline and not to advance it laterally over the counter antiviral cream buy famvir 250mg line, to avoid contacting the sciatic nerve. After careful aspiration, and if no paresthesia is present, the contents of the syringe are gently injected into the bursa. Because of the proximity to the sciatic nerve, injection for ischiogluteal bursitis should be performed only by those familiar with the regional anatomy and experienced in the technique. Many patients complain of a transient increase in pain after injection of the affected bursa and tendons, and patients should be warned of this possibility. If patients continue to engage in the repetitive activities responsible for ischiogluteal bursitis, improvement will be limited. Tumors of the hip and pelvis should also be considered in the differential diagnosis of ischiogluteal bursitis. Clinical Pearls To distinguish ischiogluteal bursitis from hamstring tendinitis, the clinician should remember that ischiogluteal bursitis manifests with point tenderness over the ischial bursa, whereas the tenderness of hamstring tendinitis is more diffuse over the upper muscle and tendons. Injection is extremely effective in relieving the pain of both ischiogluteal bursitis and hamstring tendinitis. For patients who do not respond to these treatment modalities, injection with local anesthetic and steroid is a reasonable next step. Patients with levator ani syndrome have a trigger point along the rectum or perineum. Trigger point Referred pain In addition to muscle trauma, various other factors seem to predispose patients to develop myofascial pain syndrome. Poor posture while sitting at a computer or while watching television has also been implicated as a predisposing factor. All these predisposing factors may be intensified if the patient also suffers from poor nutritional status or coexisting psychological or behavioral abnormalities, including chronic stress and depression. The levator ani muscle seems to be particularly susceptible to stress-induced myofascial pain syndrome. Axial (A) and coronal (B) gadoliniumenhanced spoiled gradient-echo magnetic resonance images show heterogeneously enhancing peritoneal and omental metastases (arrows) from recurrent rectal cancer. C, Three-dimensional color model generated from the coronal gadoliniumenhanced images shows the distribution of the peritoneal and omental tumor in purple. Because of the lack of objective diagnostic testing, the clinician must rule out other coexisting disease processes that may mimic levator ani syndrome (see "Differential Diagnosis"). The use of electrodiagnostic and radiographic testing can identify coexisting disorders such as rectal and pelvic tumors and lumbosacral nerve lesions. The clinician must also identify coexisting psychological and behavioral abnormalities that may mask or exacerbate the symptoms of levator ani syndrome. TreaTmenT Treatment is focused on eliminating the myofascial trigger and achieving relaxation of the affected muscle. Conservative therapy consisting of trigger point injection with local anesthetic or saline solution is the initial treatment of levator ani syndrome. For patients who do not respond to these traditional measures, consideration should be given to the use of botulinum differenTial diagnoSiS the diagnosis of levator ani syndrome is based on clinical findings rather than specific laboratory, electrodiagnostic, or radiographic testing. Clinical Pearls Although levator ani syndrome is a common disorder, it is often misdiagnosed. Therefore, in patients suspected of suffering from levator ani syndrome, a careful evaluation to identify underlying disease processes is mandatory. Levator ani syndrome often coexists with various somatic and psychological disorders. CompliCaTionS and piTfallS Trigger point injections are extremely safe if careful attention is paid to the clinically relevant anatomy. The avoidance of overly long needles can decrease the incidence of trauma to underlying structures. It occurs most commonly after direct trauma from a kick or a fall directly onto the coccyx. The pain of coccydynia is thought to be the result of strain of the sacrococcygeal ligament or, occasionally, fracture of the coccyx. SignS and SympTomS on physical examination, patients exhibit point tenderness over the coccyx; the pain increases with movement of the coccyx. Movement of the coccyx may also cause sharp paresthesias into the rectum, which patients find quite distressing. Magnetic resonance imaging of the pelvis is indicated if occult mass or tumor is suspected. Radionuclide bone scanning may be useful to exclude stress fractures not visible on plain radiographs. Insufficiency fractures of the pelvis or sacrum and disorders of the sacroiliac joints may on occasion mimic coccydynia. If the patient does not experience rapid improvement, injection is a reasonable next step. The legs and heels are abducted to prevent tightening of the gluteal muscles, which can make identification of the sacrococcygeal joint difficult. A wide area of skin is prepared with antiseptic solution so that all the landmarks can be palpated aseptically. A fenestrated sterile drape is placed to avoid 275 differenTial diagnoSiS Primary disease of the rectum and anus is occasionally confused with the pain of coccydynia. Proctalgia fugax can be distinguished from coccydynia because movement of the coccyx does not reproduce the pain. Histologic analysis confirmed a myxopapillary ependymoma that did not communicate with the dural sac. After locating the sacrococcygeal joint, a 11/2-inch, 25-gauge needle is inserted through the skin at a 45-degree angle into the region of the sacrococcygeal joint and ligament. If the ligament is penetrated, a "pop" will be felt, and the needle should be withdrawn through the ligament. If contact with the bony wall of the sacrum occurs, the needle should be withdrawn slightly to disengage the needle tip from the periosteum. When the needle is satisfactorily positioned, a syringe containing 5 mL of 1% preservative-free lidocaine and 40 mg methylprednisolone is attached to the needle. Ganglion impar represents the termination of the paravertebral sympathetic chains, converging at the sacrococcygeal level. B, Sagittal, T2-weighted magnetic resonance imaging showing the ganglion impar as a small, isointense signal structure anterior to the sacrococcygeal level (white arrow). C, Contrast medium outlining the ganglion impar, seen as filling defect (black arrow) in the pool of contrast. Any significant pain or sudden increase in resistance during injection suggests incorrect needle placement, and the clinician should stop injecting immediately and reassess the needle position. Physical modalities, including local heat, gentle range-ofmotion exercises, and rectal massage of the affected muscles, should be introduced several days after the patient undergoes injection for coccygeal pain. CompliCaTionS and piTfallS Coccydynia should be considered a diagnosis of exclusion in the absence of trauma to the coccyx and its ligaments, because failure to diagnose underlying tumor can have disastrous consequences. The injection technique is safe if careful attention is paid to clinically relevant anatomy. The major complication of injection is infection, given the proximity to the rectum. This complication should be exceedingly rare if strict aseptic technique is followed, as well as universal precautions to minimize any risk to the operator. Clinical Pearls the use of a foam donut when sitting, along with the other treatment modalities discussed, may provide symptomatic relief and allow the sacrococcygeal ligament to heal. The injection technique described is extremely effective in the treatment of coccydynia. Coexistent sacroiliitis may contribute to coccygeal pain, thus necessitating additional treatment with more localized injection of local anesthetic and methylprednisolone. The hip joint is susceptible to the development of arthritis from various conditions that have the ability to damage the joint cartilage. Less frequent causes of arthritis-induced hip pain include the collagen vascular diseases, infection, villonodular synovitis, and Lyme disease. Collagen vascular disease generally manifests as polyarthropathy rather than as monarthropathy limited to the hip joint, although hip pain secondary to collagen vascular disease responds exceedingly well to the treatment modalities described here. Patients may initially present with ill-defined pain in the groin; occasionally, the pain is localized to the buttocks. Some patients complain of a grating or popping sensation with use of the joint, and crepitus may be noted on physical examination. In addition to pain, patients often experience a gradual decrease in functional ability caused by reduced hip range of motion that makes simple everyday tasks such as walking, climbing stairs, figure 88-1 the pain of arthritis of the hip is localized to the hip, groin, and upper leg; it is made worse by weight-bearing exercise. With continued disuse, muscle wasting may occur, and a frozen hip secondary to adhesive capsulitis may develop. Lumbar radiculopathy may mimic the pain and disability associated with arthritis of the hip; however, in such patients, hip examination results should be negative. Primary and metastatic tumors of the hip and spine may also manifest similarly to arthritis of the hip. TreaTmenT Initial treatment of the pain and functional disability of arthritis of the hip includes a combination of nonsteroidal antiinflammatory drugs or cyclooxygenase-2 inhibitors and physical therapy. Intraarticular injection of the hip is performed by placing the patient in the supine position. The skin overlying the hip, subacromial region, and joint space is prepared with antiseptic solution. The femoral artery is identified; then, at a point approximately 2 inches lateral to the femoral artery, just below the inguinal ligament, the hip joint space is identified. The needle is carefully advanced through the skin and subcutaneous tissues through the joint capsule into the joint. Physical modalities, including local heat and gentle rangeof-motion exercises, should be introduced several days after the patient undergoes injection for hip pain. The major complication of intraarticular injection of the hip is infection; however, it should be exceedingly rare if strict aseptic technique is followed, along with universal precautions to minimize any risk to the operator. Approximately 25% of patients complain of a transient increase in pain after intraarticular injection of the hip joint, and patients should be warned of this possibility. A, Radiograph of the pelvis shows mild axial narrowing of the hip without erosions (large arrow). B, Coronal T1-weighted magnetic resonance image shows soft tissue thickening (synovitis) of intermediate density about the hip (small arrowhead) and acetabular erosion (large arrowheads). Clinical Pearls Coexistent bursitis and tendinitis may contribute to hip pain, thus necessitating additional treatment with more localized injection of local anesthetic and methylprednisolone. The injection technique described is extremely effective in the treatment of pain secondary to arthritis of the hip joint. The gluteus medius muscle originates from the outer surface of the ilium, and its fibers pass downward and laterally to attach on the lateral surface of the greater trochanter. The gluteus medius muscle locks the pelvis in place during walking and running; this muscle is innervated by the superior gluteal nerve. The iliopectineal eminence is the point at which the ilium and the pubis bone merge. The psoas and iliacus muscles join at the lateral side of the psoas, and the combined fibers are referred to as the iliopsoas muscle. Like the psoas muscle, the iliacus flexes the thigh on the trunk or, if the thigh is fixed, flexes the trunk on the thigh, such as when moving from a supine to a sitting position. SignS and SympTomS Physical examination reveals that patients can recreate the snapping and pain by moving from a sitting to a standing position and adducting the hip. Point tenderness over the trochanteric bursa, indicative of trochanteric bursitis, is often present. In Atlas of pain management injection techniques, ed 2, Philadelphia, 2007, Saunders, p 368. The needle is slowly advanced through the previously identified point at a right angle to the skin, directly toward the center of the greater trochanter, until the needle hits bone; the needle is then withdrawn out of the periosteum. After careful aspiration for blood, and if no paresthesia is present, the contents of the syringe are gently injected. CompliCaTionS and piTfallS the injection technique is safe if careful attention is paid to the clinically relevant anatomy, particularly the sciatic nerve. The proximity to the sciatic nerve makes it imperative that this procedure be performed only by those familiar with the regional anatomy and experienced in the technique. Although infection is rare, sterile technique must be used, along with universal precautions to minimize any risk to the operator. Most complications of the injection technique are related to needle-induced trauma at the injection site and in the underlying tissues. Many patients complain of a transient increase in pain after injection, and patients should be warned of this possibility.
Acute injuries are often caused by direct trauma to the bursa from falls onto the buttocks or by overuse hiv infections and zoonoses generic famvir 250mg with mastercard, such as prolonged riding of horses or bicycles hiv infection medications order 250 mg famvir with mastercard. SignS and SympTomS Patients suffering from ischiogluteal bursitis frequently complain of pain at the base of the buttock with resisted extension of the lower extremity hiv infection duration cheap famvir american express. The pain is localized to the area over the ischial tuberosity; referred pain is noted in the hamstring muscle hiv infection dose 250mg famvir with visa, which may develop coexistent tendinitis hiv infection through urine buy famvir online pills. Patients are often unable to sleep on the affected hip and may complain of a sharp, catching sensation when they extend and flex the hip, especially on first awakening. Magnetic resonance imaging is indicated if disruption of the hamstring musculotendinous unit is suspected. The injection technique described later serves as both a diagnostic and a therapeutic maneuver and is also used to treat hamstring tendinitis. Laboratory tests, including a complete blood count, erythrocyte sedimentation rate, and antinuclear antibody testing, are indicated if collagen vascular disease is suspected. Plain radiography and radionuclide bone scanning are indicated in the presence of trauma or if tumor is a possibility. To inject the ischiogluteal bursa, the patient is placed in the lateral position with the affected side upward and the affected leg flexed at the knee. Should paresthesia occur, the needle is immediately withdrawn and is repositioned more medially. The clinician must rule out other coexisting disease processes that may mimic snapping hip syndrome, including primary inflammatory muscle disease, primary hip disorders, and rectal and pelvic tumors. Clinical Pearls Snapping hip syndrome is a common disorder that often coexists with trochanteric bursitis. Because snapping hip syndrome is often misdiagnosed, a careful evaluation to identify underlying disease processes is mandatory. The injection technique described is extremely effective in the treatment of snapping hip syndrome. TreaTmenT Initial treatment of the pain and functional disability associated with snapping hip syndrome includes a combination of nonsteroidal antiinflammatory drugs or cyclooxygenase-2 inhibitors and physical therapy. To perform the injection, the patient is placed in the lateral decubitus position with the affected side upward. The midpoint of the greater trochanter is identified, and the skin overlying this point is prepared with antiseptic solution. Although significant interpatient variability exists in the number, size, and location of bursae, the iliopectineal bursa generally lies between the psoas and iliacus muscles and the iliopectineal eminence. If inflammation of the iliopectineal bursa becomes chronic, calcification may occur. SignS and SympTomS Patients with iliopectineal bursitis frequently complain of pain in the anterior hip and groin. The pain is localized to the area just below the crease of the groin anteriorly, with referred pain noted in the hip joint and anterior pelvis. A, Pelvic radiograph shows changes in the symphysis on the left with sclerosis that suggest a chondroidor osteoid-producing lesion (arrows). B, Computed tomography reveals a linear fracture plane and surrounding callus (arrowheads) resulting from a healing fracture; no evidence of a soft tissue mass is present. Passive flexion, adduction, and abduction, as well as active resisted flexion and adduction of the affected lower extremity, can reproduce the pain. Magnetic resonance imaging of the hip and pelvis is indicated if tendinitis, partial disruption of the ligaments, stress fracture, internal derangement of the hip, or pelvic mass is suspected. Radionuclide bone scanning is indicated if occult fracture, metastatic disease, or primary tumor involving the hip or pelvis is being considered. Less common causes of arthritisinduced pain include the collagen vascular diseases, infection, villonodular synovitis, and Lyme disease. Collagen vascular disease generally manifests as polyarthropathy rather than as monarthropathy limited to the hip joint, although pain secondary to collagen vascular disease responds exceedingly well to the injection technique described here. For patients who do not respond to these treatment modalities, injection of local anesthetic and steroid into the iliopectineal bursa is a reasonable next step. Injection into the iliopectineal bursa is performed with the patient in the supine position. The pulsation of the femoral artery at the midpoint of the inguinal ligament is identified. The major complication of injection of the iliopectineal bursa is infection, although it should be exceedingly rare if strict aseptic technique is followed, along with universal precautions to minimize any risk to the operator. Should a paresthesia occur, the needle is immediately withdrawn and is repositioned more laterally. The needle is then carefully advanced through the previously identified point at a 45-degree angle cephalad, to allow the needle to pass safely beneath the femoral artery, vein, and nerve. After careful aspiration for blood, and if no paresthesia is present, the contents of the syringe are gently injected into the bursa. Clinical Pearls the injection technique described is extremely effective in the treatment of iliopectineal bursitis. Iliopectineal bursitis frequently coexists with arthritis of the hip, which may require specific treatment to achieve pain relief and return of function. Lining these synovial sacs is a synovial membrane invested with a network of blood vessels that secrete synovial fluid. With overuse or misuse, the bursa may become inflamed or, rarely, infected; inflammation of the bursa results in an increase in the production of synovial fluid that causes swelling of the bursal sac. Although significant interpatient variability exists in the number, size, and location of bursae, the ischial bursa generally lies between the gluteus maximus muscle and the bone of the ischial tuberosity. The ischial bursa is vulnerable to injury from both acute trauma and repeated microtrauma. SignS and SympTomS Patients suffering from ischial bursitis frequently complain of pain at the base of the buttock with resisted extension of the lower extremity. Acute injuries are caused by direct trauma to the bursa from falls onto the buttocks and from overuse, such as prolonged riding of horses or bicycles. Less common causes of arthritis-induced pain include the collagen vascular diseases, infection, villonodular synovitis, and Lyme disease. For patients who do not respond to these treatment modalities, injection of local anesthetic and steroid into the ischial bursa is a reasonable next step. To inject the ischial bursa, the patient is placed in the lateral position with the affected side upward and the affected leg flexed at the knee. Should a paresthesia occur, the needle is immediately withdrawn and is repositioned more medially. Coronal T1-weighted magnetic resonance imaging shows asymmetrical decreased marrow signal intensity involving the left ischium. Clinical Pearls the injection technique described is extremely effective in the treatment of ischial bursitis. Ischial bursitis frequently coexists with arthritis of the hip, which may require specific treatment to achieve pain relief and return of function. The major complication of injection of the ischial bursa is infection, although it should be exceedingly rare if strict aseptic technique is followed, along with universal precautions to minimize any risk to the operator. This entrapment neuropathy manifests as pain, numbness, and dysesthesias in the distribution of the lateral femoral cutaneous nerve. The symptoms often begin as a burning pain in the lateral thigh, with associated cutaneous sensitivity. Although traumatic lesions to the lateral femoral cutaneous nerve have been implicated in meralgia paresthetica, in most patients, no obvious antecedent trauma can be identified. SignS and SympTomS Physical findings include tenderness over the lateral femoral cutaneous nerve at the origin of the inguinal ligament at the anterior superior iliac spine. A positive Tinel sign over the lateral femoral cutaneous nerve as it passes beneath the inguinal ligament may be present. Careful sensory examination of the lateral thigh reveals a sensory deficit in the distribution of the lateral femoral cutaneous nerve; no motor deficit should be present. Sitting or the wearing of tight waistbands or wide belts can compress the nerve and exacerbate the symptoms of meralgia paresthetica. A short course of conservative therapy consisting of simple analgesics, nonsteroidal antiinflammatory drugs, or cyclooxygenase-2 inhibitors is a reasonable first step in the treatment of meralgia paresthetica. To treat the pain of meralgia paresthetica, the patient is placed in the supine position with a pillow under the knees if lying with the legs extended increases the pain because of traction on the nerve. A point 1 inch medial to the anterior superior iliac spine and just inferior to the inguinal ligament is identified and is prepared with antiseptic solution. A 11/2-inch, 25-gauge needle is slowly advanced perpendicular to the skin until the needle is felt to pop through the fascia. After careful aspiration, a solution of 5 to 7 mL of 1% preservative-free lidocaine and 40 mg methylprednisolone is injected in a fanlike pattern as the needle pierces the fascia of the external oblique muscle. In addition, most patients suffering from lumbar radiculopathy have back pain associated with reflex, motor, and sensory changes, whereas patients with meralgia paresthetica have no back pain and no motor or reflex changes; the sensory changes of meralgia paresthetica are limited to the distribution of the lateral femoral cutaneous nerve and should not extend below the knee. Lumbar radiculopathy and lateral femoral cutaneous nerve entrapment may coexist as the double-crush syndrome. CompliCaTionS and piTfallS Care must be taken to rule out other conditions that may mimic the pain of meralgia paresthetica. If the needle is placed too deep and it enters the peritoneal cavity, perforation of the colon may result in the formation of an intraabdominal abscess and fistula. If the needle is placed too medially, blockade of the femoral nerve may occur, thus making ambulation difficult. If a patient presents with pain suggestive of meralgia paresthetica but does not respond to lateral femoral cutaneous nerve block, however, a lesion more proximal in the lumbar plexus or an L2-3 radiculopathy should be considered. Some investigators reported that severe limb pain before amputation increases the incidence of phantom limb pain, but other investigators failed to find this correlation. The cause of this phenomenon is not fully understood, but it is thought to be mediated in large part at the spinal cord level. Patients may be able to describe the limb in vivid detail, although it is often distorted or in an abnormal position. In many patients, the sensation of the phantom limb fades with time, but in some patients, phantom pain remains a distressing part of daily life. Phantom limb pain is often described as a constant, unpleasant, dysesthetic pain that may be exacerbated by movement or stimulation of the affected cutaneous regions; a sharp, shooting neuritic pain may be superimposed on SignS and SympTomS Phantom limb pain can take multiple forms, but it usually consists of dysesthetic pain. Investigators have reported that many patients with phantom limb pain experience a telescoping phenomenon; for example, a patient may report that the phantom foot feels like it is attached directly to the proximal thigh. Phantom limb pain may fade over time, and younger patients are more likely to experience this diminution in symptoms. Because of the unusual nature of phantom limb pain, a behavioral component is invariably present. Testing is generally used to identify other treatable coexisting diseases, such as radiculopathy. Such testing includes the following: basic laboratory tests; examination of the stump for neuroma, tumor, or occult infection; and plain radiographs and radionuclide bone scanning if fracture or osteomyelitis is suspected. After several weeks of treatment, antidepressants may exert a mood-elevating effect, which may be desirable in some patients. Care must be taken to observe closely for central nervous system side effects in this patient population, and these drugs may cause urinary retention and constipation. Nerve Block Neural blockade with local anesthetic and steroid by either epidural nerve block or blockade of the sympathetic nerves subserving the painful area is a reasonable next step if the aforementioned pharmacologic modalities fail to control phantom limb pain. The exact mechanism by which neural blockade relieves phantom limb pain is unknown, but it may be related to the modulation of pain transmission at the spinal cord level. Opioid Analgesics opioid analgesics have a limited role in the management of phantom limb pain, and they frequently do more harm than good. Because many patients suffering from phantom limb pain are older or have severe multisystem disease, close monitoring for the potential side effects of opioid analgesics. Daily dietary fiber supplementation and Milk of Magnesia should be started along with opioid analgesics to prevent constipation. Adjunctive Treatments the application of ice packs to the stump may provide relief in some patients with phantom limb pain. The application of heat increases pain in most patients, presumably because of increased conduction of small fibers, but it may be worth trying if the application of cold is ineffective. Transcutaneous electrical nerve stimulation and vibration may also be effective in a limited number of patients. The favorable risk-to-benefit ratio of these modalities makes them reasonable alternatives for patients who cannot or will not undergo sympathetic neural blockade or who cannot tolerate pharmacologic treatment. The topical application of capsaicin may be beneficial in some patients suffering from phantom limb pain; however, the burning associated with application of this drug often limits its usefulness. If the amputation was necessitated by malignant disease, occult tumor must be excluded. Many pain specialists agree that preemptive analgesia early in the natural course of a disease that may lead to amputation, such as peripheral vascular insufficiency, can reduce the likelihood that patients will develop phantom limb pain. Analgesics the anticonvulsant gabapentin is a first-line treatment in the palliation of phantom limb pain. It should be administered early in the course of the pain syndrome and can be used concurrently with neural blockade, opioid analgesics, and other adjuvant analgesics, including antidepressants, if care is taken to avoid central nervous system side effects. Gabapentin is started at a bedtime dose of 300 mg and is titrated upward in 300-mg increments to a maximum of 3600 mg/day given in divided doses, as side effects allow. Carbamazepine should be considered in patients with severe neuritic pain who do not respond to nerve block and gabapentin.
Order famvir 250 mg amex. HIV-AIDS and Condom Use -- Dr. Willie Ong Health Blog #10.
References
- Schoenberg SO, Rieger J, et al. High - spatial - resolution MR angiography of renal arteries with integrated parallel acquisitions: comparison with digital subtraction angiography and US. Radiology 2005; 235:687.
- Figlewicz DP, Benoit SC. Insulin, leptin, and food reward: Update 2008.
- Pego-Fernandes PM, Costa PL, Fernandes F, Benvenuti LA, Oliveira SA. Right atrial lipoma. Arq Bras Cardiol 2003;80:97-99, 94-96.
- Nickel JC, Gilling P, Tammela TL, et al: Comparison of dutasteride and finasteride for treating benign prostatic hyperplasia: the Enlarged Prostate International Comparator Study (EPICS), BJU Int 108(3):388n394, 2011.