Steven J. Kronowitz, MD, FACS
- Professor
- Department of Plastic Surgery
- University of Texas
- MD Anderson Cancer Center
- Houston, Texas
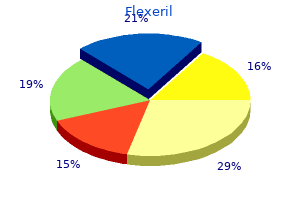
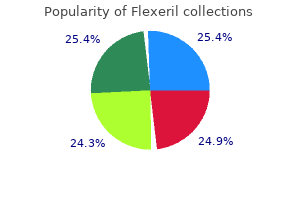
Civil Capacities in Clinical Neuropsychology Research Findings and Practical Applications treatment tinnitus buy flexeril with visa. Validation of the modified telephone interview for cognitive status in amnestic mild cognitive impairment and intact elders treatment molluscum contagiosum generic 15 mg flexeril with visa. Progression of mild cognitive impairment to dementia in clinic- vs community-based cohorts treatment type 2 diabetes order flexeril 15mg with visa. Mini-Mental State: A practical method for grading the cognitive state of patients for the clinician medicinenetcom order flexeril with a visa. The vegetative and minimally conscious states: current knowledge and remaining questions medications 24 buy flexeril 15mg amex. Cognitive impairment in newly diagnosed multiple sclerosis patients: a 4-year follow-up study. Differential aberrant sprouting in temporal lobe epilepsy with psychiatric co-morbidities. The effects of small vessel disease and amyloid burden on neuropsychiatric symptoms: a study among patients with subcortical vascular cognitive impairments. Influence of negative stereotypes and beliefs on neuropsychological test performance in a traumatic brain injury population. Minimum requirements for the diagnosis of psychogenic nonepileptic seizures: a staged approach: a report from the International League against Epilepsy Nonepileptic Seizures Task Force. Factors influencing postconcussion and posttraumatic stress symptom reporting following military-related concurrent polytrauma and traumatic brain injury. Assessment of cognitive fluctuation in dementia: a systematic review of the literature. Classification of seizure disorder and syndromes, and neuropsychological impairment in adults with epilepsy. Identification of pure subcortical vascular dementia using 11C-Pittsburgh compound B. The diagnostic utility of cerebrospinal fluid alpha-synuclein analysis in dementia with Lewy bodies-a systematic review and meta-analysis. Structural model for estimating the influence of cognitive reserve on cognitive performance in adults with subjective memory complaints. Executive functioning in children with intractable frontal lobe or temporal lobe epilepsy. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport, Zurich, November 2012. From frontotemporal lobar degeneration pathology to frontotemporal lobar degeneration biomarkers. Language, executive function and social cognition in the diagnosis of frontotemporal dementia syndromes. Disentangling the relationship between epilepsy and its behavioral comorbidities-the need for prospective studies in new-onset epilepsies. Multifactorial etiology of interictal behavior in frontal and temporal lobe epilepsy. The longer-term cognitive effects of adjunctive antiepileptic treatment with lacosamide in comparison with lamotrigine and topiramate in a naturalistic outpatient setting. Comparison of subjective cognitive complaints with neuropsychological tests in individuals with mild vs more severe traumatic brain injuries. A meta-analysis of the accuracy of the minimental state examination in the detection of dementia and mild cognitive impairment. Cognitive and psychiatric aspects of Huntington disease contribute to functional capacity. Detecting dementia with the mini-mental state examination in highly educated individuals. Beyond and below the cortex: the contribution of striatal dysfunction to cognition and behaviour in neurodegeneration. The Trail Making Test in prodromal Huntington disease: contributions of disease progression to test performance. Investigating higherorder cognitive functions in temporal lobe epilepsy: cognitive estimation. Effects of cerebrovascular disease and amyloid beta burden on cognition in subjects with subcortical vascular cognitive impairment. Cognitive decline in prodromal Huntington Disease: implications for clinical trials. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. The elusive biomarker for personalized medicine in multiple sclerosis: the search continues. Responsiveness of magnetic resonance imaging and neuropsychological assessment in memory clinic patients. Assessment techniques: tests, test batteries, norms, and methodological approaches. A follow-up study of cognitive function in young adults who had resective epilepsy surgery in childhood. Consolidation deficits in traumatic brain injury: the core and residual verbal memory defect. The prevalence and incidence of dementia with Lewy bodies: a systematic review of population and clinical studies. Predictors of memory and processing speed dysfunctions after traumatic brain injury. Neuropsychological and physiological correlates of fatigue following traumatic brain injury. Neuropathological profile of mild cognitive impairment from a population perspective. The vascular depression hypothesis: mechanisms linking vascular disease with depression. Recognition memory and verbal fluency differentiate probable Alzheimer disease from subcortical ischemic vascular dementia. An adaptation of the Modified Mini-Mental State Examination: analysis of demographic influences and normative data: the Cache County study. Lavin I do not know of any kind of work better fitted for correcting loose habits of observation and careless thinking than a study of the ocular motor nerves. Despite sophisticated advances in technology, competence in neuro-ophthalmological diagnosis still requires basic clinical skills that include attentive listening, empathetic and timely probing questions, extensive knowledge of neuroanatomy and disorders that affect the afferent and efferent visual pathways, skill in examination of the visual and nervous systems, and experience and expertise in evaluating supplementary investigations including perimetry, fluorescein angiography, optical coherence tomography, and neuroimaging. The enormous amount of medical information available to patients on the internet, some of which is useful, but most of which is misleading, often complicates their care; thus a thorough clinical examination, up to date knowledge, and careful thought frequently preempt uncomfortable, invasive, expensive, and potentially harmful procedures. The human fovea is a highly sensitive part of the retina capable of resolving angles of less than 20 arc seconds. The ocular motor system places images of objects of regard on the fovea and maintains fixation (foveation) if the object or head moves. The actions of the medial and lateral recti are essentially confined to the horizontal plane. The actions of the superior and inferior recti are solely vertical when the eye is abducted 23 degrees. For practical purposes, the vertical actions may be tested at 30 degrees of adduction and abduction. According to the Hering law of dual innervation, yoked muscles receive equal and simultaneous innervation while their antagonists are inhibited (the Sherrington law of reciprocal inhibition), thereby allowing the eyes to move conjugately and with great precision. The pulling actions of the extraocular muscles evolved to move the eyes in the planes of the semicircular canals, which are not strictly horizontal or vertical. When it varies with gaze direction, the patient has a noncomitant (paralytic or restrictive) strabismus. In general, comitant strabismus is ophthalmological in origin, whereas noncomitant strabismus is neurological. Some form of ocular misalignment is present in 2% to 3% of preschool children and some form of amblyopia in 3% to 4%. Most people have a latent tendency for ocular misalignment, heterophoria, which may become manifest (heterotropia) under conditions of stress such as fatigue, exposure to bright sunlight, or ingestion of alcohol, anticonvulsants, or sedatives. In nonparalytic (comitant) strabismus, the image is projected in the direction opposite the deviation. When such a latent tendency for the visual axes to deviate is unmasked, the diplopia usually is present in most directions of gaze (relatively comitant). Vertical misalignment of the visual axes is less common: When the nonfixating eye is higher, the patient is said to have a hypertropia, and when it is lower, a hypotonia (Donahue, 2007), irrespective of which eye is abnormal; for example, with a right hypertropia, the right eye is higher. In patients with paralytic strabismus, the image from the nonfixating paretic eye is the false image and is displaced in the direction of action of the weak muscle. After a variable period, the patient learns to ignore or suppress the false image. If suppression occurs before visual maturity (approximately 6 years of age) and persists, central connections in the afferent visual system fail to develop fully, leading to permanent visual impairment in that eye (developmental amblyopia). Amblyopia is more likely to develop with esotropia than with exotropia, because exotropia is commonly intermittent. After visual maturity, suppression and amblyopia do not occur; instead, the patient learns to avoid diplopia by ignoring the false image. Comitant strabismus occurs early in life; the magnitude of misalignment (deviation) is similar in all directions of gaze, and each eye has a full range of movement. Probably, it occurs because of failure of central mechanisms in the brain that keep the eyes aligned. Infantile (congenital) esotropia may be associated with maldevelopment of the afferent visual system, including the visual cortex, and presents within the first 6 months of life; those with comitant esotropia of more than 40 prism diopters (20 degrees) do not "grow out of it" and require surgical correction (Donahue, 2007). Evidence using cortical motion visual evoked potentials indicates that early correction of strabismus (before 11 months of age) improves visual cortical development (Gerth et al. Comitant esotropia that manifest between the ages of 6 months and 6 years (average 2 1 2 years) usually is caused by hyperopia (farsightedness) resulting in accommodative esotropia: such children with excessive farsightedness must accommodate to have clear vision; the constant accommodation causes excessive convergence and leads to persistent esotropia. Evidence indicates that high-level stereopsis is restored in these children (unlike those with uncorrected infantile esotropia) if treatment is initiated within 3 months of the onset of constant esotropia (Fawcett et al. Occasionally, children with Chiari malformations or posterior fossa tumors present with isolated esotropia before the appearance of other symptoms or signs. Features that suggest a structural cause for the esotropia include presentation after age 6, complaints such as diplopia or headache, incomitance in horizontal gaze, esotropia greater at distance than near, and neurological findings such as abduction deficits, ataxia, optic disc edema, pathological nystagmus, and saccadic pursuit. Adults in whom isolated esotropia develops, particularly when they become presbyopic in their early 40s, should have a cycloplegic refraction to detect latent hyperopia. Other causes of adult-onset esotropia include Chiari malformations and acute thalamic hemorrhage (Box 44. Esotropia after the age of 3 months is abnormal and, if constant, usually is associated with development delay, cranial facial syndromes, or structural abnormalities of the eye. It should be corrected early unless contraindicated by one of the above underlying conditions. Intermittent exotropia is common and can be treated with exercises, minus-lens spectacles to stimulate accommodation, or surgery. Noncomitant(Incomitant)Strabismus Noncomitant strabismus occurs when the degree of misalignment of the visual axes varies with the direction of gaze as a result of weakness or restriction of one or more extraocular muscles. When a patient with a noncomitant strabismus fixates on an object with the nonparetic eye, the angle of misalignment is referred to as the primary deviation. When the patient fixates with the paretic eye, the angle of misalignment is referred to as the secondary deviation. Thefoveaofthelefteye(f1)viewsthe"A"sideofthetarget;thefovea of the right eye (f2) views the "B" side of the target. The normal left medial rectus muscle also is overdriven (the Hering law of dual innervation), resulting in a large esotropia(secondarydeviation). For various reasons the patient may interpret subtle diplopia as blurring unless one eye is covered, or the onset may be uncertain because the diplopia is intermittent initially, of small amplitude, or compensated for by head position, as may be the case in disorders such as congenital superior oblique palsy, ocular myasthenia, and thyroid eye disease. Most adult patients with acquired heterotropia complain of frank double vision, but if the images are close together, the patient may not be aware of frank diplopia but merely perceive blurring, overlapping images (ghosting), or eyestrain. Anxious or histrionic patients may misinterpret physiological diplopia, a normal phenomenon, as a pathological symptom. Physiological diplopia occurs when a subject fixates an object in the foreground and then becomes aware of another object farther away but in the direction of gaze. Conversely, when the subject fixates a distant object, a near object may appear double. If the palsy is acquired, one image is virtually always tilted-an infrequent finding when the palsy is congenital. Images are most widely separated when an attempt is made to look in the direction of the paretic muscle. If one image is tilted, the weak muscle is more likely an oblique rather than a predominantly vertically acting rectus. Spread of comitance-that is, the tendency for the ocular deviation to "spread" to all fields of gaze-occurs in longstanding cases; then the diplopia no longer obeys the usual rules. If double vision persists when one eye is covered, the patient has monocular diplopia, which may be bilateral. The most common cause of monocular diplopia is an optical aberration (refractive error) and warrants appropriate correction (Box 44. Less commonly, monocular diplopia is psychogenic, but occasionally it can be attributed to dysfunction of the retina or cerebral cortex. The patient is asked to look through a pinhole; if the cause is refractive, the diplopia abates because optical distortion is eliminated as the light rays entering the eye through the pinhole are aligned along the visual axis and thus not deflected. Occasionally, disorders that displace the fovea, such as a subretinal neovascular membrane, can cause binocular diplopia by disrupting the alignment of the photoreceptors (the dragged-fovea diplopia syndrome or the foveal displacement syndrome). The diplopia probably results from rivalry between central and peripheral fusional mechanisms. Central disruption of fusion (see later) and horror fusionis (in patients with asymmetrical retinal disease) cause intractible diplopia.
Lower stimulation frequency can enhance tolerability and efficacy of pallidal deep brain stimulation for dystonia medicine for nausea discount flexeril 15mg with visa. Hypothalamic deep brain stimulation for cluster headache: experience from a new multicase series medicine hat buy 15mg flexeril mastercard. Chronic electrical stimulation of the ventralis intermedius nucleus of the thalamus as a treatment of movement disorders symptoms ibs order flexeril online. Mechanisms of deep brain stimulation in movement disorders as revealed by changes in stimulus frequency medications mitral valve prolapse buy online flexeril. Thalamic deep brain stimulation in the treatment of essential tremor: a longterm follow-up medications enlarged prostate cost of flexeril. Are complications less common in deep brain stimulation than in ablative procedures for movement disorders Update on neurosurgical treatment of chronic trigeminal autonomic cephalalgias and atypical facial pain with deep brain stimulation of posterior hypothalamus: results and comments. Lack of benefit of accumbens/capsular deep brain stimulation in a patient with both tics and obsessive-compulsive disorder. Microthalamotomy effect during deep brain stimulation: potential involvement of adenosine and glutamate efflux. Electrical stimulation of the globus pallidus internus in patients with primary generalized dystonia: long-term results. Worsening essential tremor following deep brain stimulation: disease progression versus tolerance. Deep brain stimulation of the anterior internal capsule for the treatment of Tourette syndrome: technical case report. Safety and efficacy of deep brain stimulation in refractory cluster headache: a randomized placebo-controlled double-blind trial followed by a 1-year open extension. Ventralis intermedius plus ventralis oralis anterior and posterior deep brain stimulation for posttraumatic Holmes tremor: two leads may be better than one: technical note. Dual electrode thalamic deep brain stimulation for the treatment of posttraumatic and multiple sclerosis tremor. Granular insular cortex inactivation as a novel therapeutic strategy for nicotine addiction. Clinical study for alleviating opiate drug psychological dependence by a method of ablating the nucleus accumbens with stereotactic surgery. Deep brain stimulation for intractable obsessive compulsive disorder: pilot study using a blinded, staggered-onset design. Deep brain stimulation of the ventral internal capsule/ventral striatum for obsessive-compulsive disorder: worldwide experience. Neurosurgery for intractable obsessive-compulsive disorder and depression: critical issues. Deep brain stimulation for chronic neuropathic pain: long-term outcome and the incidence of insertional effect. Multicentre European study of thalamic stimulation for parkinsonian tremor: a 6 year follow-up. Identification and management of deep brain stimulation intra- and postoperative urgencies and emergencies. Long-term treatment with vagus nerve stimulation in patients with refractory epilepsy. Long-term electrical capsular stimulation in patients with obsessive-compulsive disorder. Development and initial validation of a screening tool for Parkinson disease surgical candidates. A trial of scheduled deep brain stimulation for Tourette syndrome: moving away from continuous deep brain stimulation paradigms. A case-based review of troubleshooting deep brain stimulator issues in movement and neuropsychiatric disorders. Thalamic deep brain stimulation: comparison between unilateral and bilateral placement. The North American survey of placement and adjustment strategies for deep brain stimulation. Effect of an external responsive neurostimulator on seizures and electrographic discharges during subdural electrode monitoring. Remission of alcohol dependency following deep brain stimulation of the nucleus accumbens: valuable therapeutic implications Neurotransmitter release from high-frequency stimulation of the subthalamic nucleus. Treatment of chronic pain by deep brain stimulation: long term follow-up and review of the literature. Surgical and hardware complications of subthalamic stimulation: a series of 160 procedures. Prospective randomized double-blind trial of bilateral thalamic deep brain stimulation in adults with Tourette syndrome. Cellular effects of deep brain stimulation: model-based analysis of activation and inhibition. Uncovering the mechanism(s) of action of deep brain stimulation: activation, inhibition, or both. Patient selection and assessment recommendations for deep brain stimulation in Tourette syndrome. Thalamic deep brain stimulation for essential tremor: relation of lead location to outcome. Thalamic deep brain stimulation for treatment-refractory Tourette syndrome: twoyear outcome. Vagus nerve stimulation for intractable epilepsy: outcome in two series combining 90 patients. Hypothalamic stimulation in chronic cluster headache: a pilot study of efficacy and mode of action. A comparison of continuous thalamic stimulation and thalamotomy for suppression of severe tremor. Neuromodulation of the posterolateral hypothalamus for the treatment of chronic refractory cluster headache: Experience in five patients with a modified anatomical target. Deep brain stimulation in 18 patients with severe Gilles de la Tourette syndrome refractory to treatment: the surgery and stimulation. Microelectrodeguided deep brain stimulation for Tourette syndrome: withinsubject comparison of different stimulation sites. Comonitoring of adenosine and dopamine using the Wireless Instantaneous Neurotransmitter Concentration System: proof of principle. Lessons learned in deep brain stimulation for movement and neuropsychiatric disorders. Vagus nerve stimulation therapy: 5-year or greater outcome at a universitybased epilepsy center. Chronic stimulation of the posterior hypothalamic region for cluster headache: technique and 1-year results in four patients. Multicentre European study of thalamic stimulation in essential tremor: a six year follow up. Disrupting disordered neurocircuitry: treating refractory psychiatric illness with neuromodulation. Effectiveness of vagus nerve stimulation in epilepsy patients: a 12-year observation. Deep brain stimulation of the nucleus accumbens shell attenuates cocaine priming-induced reinstatement of drug seeking in rats. Bilateral deepbrain stimulation of the globus pallidus in primary generalized dystonia. Bilateral, pallidal, deep-brain stimulation in primary generalised dystonia: a prospective 3 year follow-up study. Chronic bilateral thalamic stimulation: a new therapeutic approach in intractable Tourette syndrome. Pallidal deep brain stimulation in patients with primary generalised or segmental dystonia: 5-year follow-up of a randomised trial. Bilateral deep brain stimulation vs best medical therapy for patients with advanced Parkinson disease: a randomized controlled trial. Randomized trial of deep brain stimulation for Parkinson disease: thirty-six-month outcomes. Influence of the frequency parameter on extracellular glutamate and gammaaminobutyric acid in substantia nigra and globus pallidus during electrical stimulation of subthalamic nucleus in rats. Long-term seizure outcome in patients initially seizure-free after resective epilepsy surgery. A variety of techniques are applied for monitoring and testing, and in a wide variety of clinical circumstances. The monitoring must take account of confounding effects such as from anesthesia, temperature, and technical problems. Surgeons have a variety of ways to respond to monitoring alarms that reduce neurologic deficit risks when monitoring raises an alarm. Cost analysis shows substantial savings to hospital systems from use of monitoring. When problems begin, these techniques warn the surgeon in time to intervene and correct the problem before it becomes worse or permanent. A surgeon can rely on monitoring for reassurance about nervous system integrity, allowing the surgery to be more extensive than would have been safe without monitoring. Some patients are eligible for surgery with monitoring who may have been denied surgery without monitoring because of a high risk of nervous system complications. Patients and families can be reassured that certain feared complications are screened for during surgery. Effective collaboration and communication is needed among surgeon, anesthesiologist, and neurophysiologist, who typically maintain communication throughout a specific procedure. An experienced electrodiagnostic technologist applies electrodes and ensures technically accurate studies. The interpreting neurophysiologist either is in the operating room or monitoring continuously online in real time. This guides the surgeon to resect physiologically dysfunctional or epileptogenic areas while sparing relatively normal cortex. Direct cortical stimulation applies very localized electrical pulses to cortex through a handheld wand. The electricity disrupts cortical function such as language, which can be tested in patients awake during portions of a craniotomy. These techniques identify language or motor regions so they can be spared during resections. Similar direct nerve stimulation is used for cranial and peripheral nerves to locate them amid pathological tissue and to check whether they still are intact. One version is stimulation at the floor of the fourth ventricle or during brainstem resection to identify tracts and nuclei of interest. For spinal procedures using pedicle screws, risk is incurred to the nerve roots or spinal cord during screw placement. The reader is referred elsewhere for extensive coverage of intraoperative neurophysiological techniques (Nuwer, 2008). Averaged recordings are made at standardized surface locations over the spine and scalp. Small electrical potentials are recorded during 50 milliseconds after stimulation, recording the transit and arrival of the axonal volley or synaptic events at the peripheral, spinal, brainstem, and primary sensory cortical levels. Electrical pulses are delivered at a level strong enough to discharge the axon hillock of motor cortex pyramidal cells. The resulting action potentials travel down corticospinal tracts and discharge spinal anterior horn cells. Which peaks are preserved and which are changed can localize the side and level of impairment. Often the ulnar nerve rather than the median nerve is used during cervical surgery for better coverage of the lower cervical cord. The peroneal nerve at the knee may substitute for the posterior tibial nerve at the ankle for elderly patients, diabetics, or others in whom a peripheral neuropathy may interfere with adequate distal peripheral conduction. Sometimes other incidental clinical problems are detected beyond the primary purpose of spinal cord, brainstem, or cortical region monitoring. For example, a developing plexopathy or peripheral nerve compression can be spotted by loss of the peripheral peak, which may be easily treated by repositioning an arm. Each pair of tracings is the current tracing (black) compared to the baseline (gray) at the beginning of the case. Other monitoring pages available to the neurophysiologist (not shown) display a variety of other views, and can be interrogated to interpret better the signals online in real time. One is monitoring, in which baseline findings are established and subsequent findings are compared to baseline. Alarm criteria are set in advance based on knowledge of how much change is acceptable without risk. One is to identify a structure, such as finding the facial nerve within pathological tissue where it may be difficult to identify. A third example is identifying which cauda equina root is L5, or S1, or S2, or which is the sensory or the motor portion of a root. Occasional transient significant changes occur without significant risk for postoperative neurological problems.
Order cheap flexeril on line. Withdrawal Symptoms.
Storkbill (Herb Robert). Flexeril.
- Are there safety concerns?
- What is Herb Robert?
- Diarrhea, liver and kidney conditions, bladder and gallbladder conditions, and the prevention of stones forming in the kidney, bladder, or gallbladder.
- Dosing considerations for Herb Robert.
- How does Herb Robert work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96074
F treatment yellow fever safe flexeril 15mg, Axial T2-weighted image demonstrates the hypointense hemosiderin deposition even better (arrow) treatment centers for alcoholism buy cheap flexeril 15mg line. This 48-year-old patient presented with a new-onset seizure and right visual field deficit that resolved later treatment kennel cough discount flexeril 15mg without a prescription. B medications on airline flights discount flexeril 15mg, Noncontrast T1-weighted image also reveals abnormal hyperintense signal in the involved venous sinuses medications zovirax purchase 15 mg flexeril with mastercard. C, Postcontrast T1-weighted image reveals normal filling in the sinus on the right, but there is no filling along the visualized segment of the left transverse sinus (arrowheads). Gadolinium-enhanced images help in these cases, demonstrating contrast filling/ enhancement in the sinuses and confirming the absence of thrombosis. T1- and T2-weighted images, however, are usually able to demonstrate the absence of thrombus in the sinus. Hemorrhagic Cerebrovascular Disease Structural neuroimaging is crucial in the evaluation of hemorrhagic cerebrovascular disease. Besides detection of the hematoma itself, its location can provide useful information regarding its etiology. Lobar hematomas, especially along with small, scattered, parenchymal microbleeds, raise the possibility of cerebral amyloid angiopathy, whereas putaminal, thalamic, or cerebellar hemorrhages are more likely to be of hypertensive origin. Other underlying lesions such as brain tumors causing hemorrhages can be detected by structural imaging. This section discusses hemorrhagic cerebrovascular disease and cerebral intraparenchymal hematoma, whereas other causes of hemorrhage such as trauma or malignancy are discussed in other sections. Please also refer to Chapters 66 and 67 for a clinical neurological review of intracerebral hemorrhages. With a normal hematocrit, both retracted and unretracted clots exhibit hyperdensity that contrasts sufficiently with the isodense background of brain parenchyma to be easily detectable. Various degrees of midline shift or subtypes of herniation (transtentorial, subfalcine, etc. The surrounding edema is seen as hypodensity and tends to appear irregular with varying thickness depending on the degree of involvement of adjacent white matter tracts, which are preferentially affected. The initially distinct border of the hematoma changes within days to a few weeks after onset and becomes irregular and "moth-eaten" due to the phagocytic activity of macrophages. Signal characteristics of hemorrhage vary widely across different pulse sequences (T1, T2, T2* gradient echo) depending on the age of the hemorrhage; presence of oxyhemoglobin, deoxyhemoglobin, methemoglobin, and hemosiderin; changing water content within the clot; and integrity of erythrocyte membranes. In the early (hyperacute) phase of intraparenchymal hemorrhage (<24 hours) the red blood cells are intact, and a mixture of oxy- and deoxyhemoglobin is present (Bakshi et al. In this stage, the signal on T1-weighted images is isointense to the brain, so even larger hematomas may be missed on this pulse sequence. On T2-weighted images, the oxyhemoglobin portion is hyperintense and deoxyhemoglobin is hypointense, resulting in the gradual appearance of a hypointense rim and gradually increasing hypointense foci within the hematoma as the amount of deoxyhemoglobin increases from the periphery. Between the clot and the deoxyhemoglobin-containing rim, thin intervening clefts of fluid-like T2 hyperintensity may be seen as an initial manifestation of clot retraction. On gradient echo images, hyperacute hemorrhage will exhibit heterogeneously isointense to markedly hypointense signal, the latter corresponding to deoxyhemoglobin content in more peripheral portions of the clot. During this stage, hemoglobin is transformed to deoxyhemoglobin, but the membranes of the erythrocytes are still intact (Bakshi et al. The surrounding edema, which is more extensive during this stage, is hypointense on T1 and hyperintense on T2. At this stage, the blood degradation products are still intracellular (Bakshi et al. Intracellular methemoglobin is hyperintense on T1 and hypointense on T2-weighted images. T1 shortening is primarily the result of dipole-dipole interactions between heme iron and adjacent water protons, facilitated by a conformational change that occurs when deoxyhemoglobin is converted to methemoglobin. Sequestration of methemoglobin within the intact red blood cell membrane results in a locally paramagnetic environment adjacent to the diamagnetic, methemoglobin-free extracellular compartment. Therefore, on T2-weighted images the presence of intracellular methemoglobin results in hypointensity of the hemorrhage. These signal changes start from the periphery of the hematoma where the deoxyhemoglobin-to-methemoglobin transformation first occurs. In the late subacute phase, the membranes of the red blood cells disintegrate, and methemoglobin becomes extracellular (Bakshi et al. During this stage (usually 2 weeks after the hemorrhage) hemosiderin deposition begins, typically at the periphery of the hematoma where macrophages reside. If the hemorrhage is small, eventually its entire area will be occupied by hemosiderin deposition. Susceptibility-weighted images are even more sensitive to magnetic filed distortion due to blood products and can reveal microbleeds that are missed even by conventional gradient echo images. Structural Imaging using Magnetic Resonance Imaging and Computed Tomography A 436. Susceptibility-weighted image demonstrates multiple hypointense foci (arrows), scattered in the hemispheres. These are felt to represent chronic blood degradation products, due to microbleeds from suspected amyloid angiopathy. Axial T2-weighted image demonstrates linear areas of hypointensity along the surface of multiple frontal lobe gyri bilaterally (arrowheads). Superficial Siderosis the phenomenon of superficial siderosis has been described as a late consequence of subarachnoid hemorrhage. It typically follows chronic or repeated episodic bleeding into the subarachnoid space. The recurrent hemorrhage can be due to certain tumors, trauma, or vascular malformations. As a result of the bleeding, there is deposition of hemosiderin into the subpial layer of the brain parenchyma. Although the phenomenon may be idiopathic, an extensive search for the earlierdescribed possible sources of hemorrhage is warranted. In the typical uncomplicated form of bacterial meningitis, no abnormalities are seen in the brain parenchyma, and without contrast administration, the meninges may also appear unremarkable. With gadolinium, however, intense meningeal enhancement is seen, usually over the convexities and along the basal cisterns; this is due to vascular engorgement and increased vascular permeability secondary to the inflammatory process. At times, as a complication, ventriculitis may develop, and then the ependymal lining of the ventricles also exhibits enhancement. Cerebritis and abscess can arise as complications of bacterial meningitis, but they may also spread to the brain hematogenously from another source such as endocarditis or pulmonary abscess. With gadolinium, a heterogeneous irregular enhancement pattern may or may not be present. If the process continues to cerebral abscess formation, after an average of 2 weeks, the core appears more demarcated, and fibrotic capsule formation is noted. This is usually hypointense on T1 (but may appear more hyperintense, depending on the protein content) and hyperintense on T2. Often the T2 hypointense rim is well seen, separating the hyperintense core from the usually less hyperintense surrounding edema. With gadolinium, the capsule exhibits ring enhancement, which is typically a smooth, thin, complete ring. Sometimes the deeper segment of the enhancing ring is thinner than the superficial. A characteristic feature that supports the diagnosis of abscess is the so-called daughter abscess, which is seen as a smaller ring-enhancing lesion connected to the parent abscess. Cerebral abscesses are part of the differential diagnosis when ring-enhancing cerebral lesions are encountered. Cerebral Amyloid Angiopathy this condition results from deposition of -amyloid into the media and adventitia of small and medium-sized arteries. The damaging effect of amyloid causes narrowing of the lumen of these vessels, but fibrinoid necrosis and microaneurysm formation is also noted. Microvascular damage causes white matter ischemic lesions, hyperintense on T2 and hypointense on T1-weighted images. Rupture of the vessel wall or microaneurysm results in cerebral hemorrhage, which can be large. A lobar pattern of hemorrhage in a normotensive elderly patient, especially when multiple lobes are affected, should raise the possibility of underlying amyloid angiopathy. The hemorrhagic lesions may be much smaller too, often appearing as multiple microbleeds. Amyloid angiopathy may be seen in the setting of Alzheimer disease, and in these cases the characteristic mesial temporal atrophy or generalized cerebral atrophy may also be noted. Hyperintense edema in adjacent parenchyma extends to various white matter regions. B, Axial T1-weighted postcontrast image shows complete ring enhancement in the capsule of the abscess (arrowheads). Diffuse parenchymal enhancement is noted in the brain medial to the abscess, likely due to cerebritis (arrow). C, Abscess cavity is characteristically hyperintense on diffusion-weighted images (arrow). Tuberculomas exhibit solid or ring enhancement and, similar to tuberculosis related abscesses, enhance intensely; in cases of ring enhancement, it is usually thicker and more irregular than seen with pyogenic abscesses. Tuberculous meningitis is another frequent occurrence in this disease, diffusely abnormal meningeal enhancement being most intense along the basal meninges; distinct nodules may also be noted. Tuberculosis-related vasculitis may complicate the disease, causing infarctions of various sizes. In the brain parenchyma, Lyme encephalitis may cause multiple lesions that are slightly hypointense on T1 and hyperintense on T2-weighted images. The most common locations are the subcortical and periventricular white matter, but the thalamus, corpus callosum, and pons may be involved as well. The lesions appear nonspecific, their size ranging from a few millimeters to a centimeter. Vasculitis, demyelinating disease, and microvascular ischemia are frequent differential diagnostic considerations. If present, abnormal enhancement along the meninges and cranial nerve segments may indicate involvement of these structures by Lyme disease. The infection may involve the parenchyma, but meningeal, subarachnoid, and intraventricular locations are also common. The lesions are usually cystic, and the cysts often exhibit a T1 hyperintense central scolex. Intraparenchymal cysts are common at the gray/white junction, their size ranging from millimeters to a few centimeters. The cyst itself is of variable signal intensity, hypo- to hyperintense on T1 and iso- to hyperintense on T2. The cyst and its leaking Structural Imaging using Magnetic Resonance Imaging and Computed Tomography 436. A, Axial T2-weighted image reveals prominent, mass-like lesion is seen in the pontine tegmentum. B,C, Axial and coronal T1 postcontrast images demonstrate intense, ring-pattern enhance of the pontine lesion, with surrounding T1 hypointense edema. A,B, Axial T1-weighted images reveal cystic, ring-enhancing lesions (arrows) in periventricular and subcortical locations. Professor of Neuroradiology, University Hospital Bellvitge, Department Manager Diagnostic Neuroradiology, and Interventional Neuroradiology of Spine. With gadolinium, the amount of enhancement depends on the degree of inflammatory reaction. As the larva dies, the cystic lesion usually retracts, and at the chronic stage there is calcification without contrast enhancement. C,D, In a different patient, even more prominent temporal lobe involvement is seen. On a noncontrast T1-weighted image (C) the left temporal lobe is swollen, and parts of the cortex show faint hyperintensity, indicating potential hemorrhage (arrows). The encephalitis is frequently hemorrhagic, causing additional signal changes depending on the age of the hemorrhage. Typically, a few days after onset, variable patterns of enhancement may be seen (gyriform, nodular, leptomeningeal, or intravascular). In the chronic stage, varying degrees of encephalomalacia, atrophy, calcification, and gliosis are seen in the affected lobes. Eventually, basal ganglionic and thalamic involvement is also Structural Imaging using Magnetic Resonance Imaging and Computed Tomography 436. The disease initially involves the white matter, most commonly in the frontal, parietal, and occipital lobes. They tend to involve the subcortical white matter, including the U-fibers, with later involvement of the deep gray matter, corpus callosum, and posterior fossa. With gadolinium administration, faint enhancement may be present, but usually no enhancement is seen. Meningitis and ependymal involvement are also possible, seen as enhancement of these structures after gadolinium administration. A significant amount of edema surrounds the lesions, appearing as T1 hypointensity and T2 hyperintensity. With gadolinium, the smaller lesions enhance homogeneously, and the larger ones exhibit ring or nodular enhancement. After antibiotic treatment, chronic lesions frequently show calcification and hemosiderin deposits. Progressive multifocal leukoencephalopathy is an infectious demyelinat- Creutzfeldt-Jakob Disease. Creutzfeldt-Jakob disease is a rapidly progressing, fatal dementing illness caused by prions- self-replicating, infectious protein particles.
A congenital inability to fuse is associated with amblyopia or congenital esotropia treatment irritable bowel syndrome buy flexeril 15 mg with amex. The hemislide (hemifield slip) phenomenon causes diplopia in patients with large visual field defects symptoms sleep apnea generic flexeril 15 mg with visa, particularly dense bitemporal hemianopias or medications help dog sleep night effective flexeril 15mg, occasionally medications routes order flexeril 15mg with amex, heteronymous altitudinal defects medicine 018 purchase flexeril 15mg amex. Because of loss of overlapping areas of visual field, patients have difficulty maintaining fusion and can no longer suppress any latent ocular deviation. Cyclical esotropia, also called circadian, alternate-day, or clock-mechanism esotropia, usually begins in childhood, although it can occur at any age and can also follow surgery for intermittent esotropia. The cycles of orthotropia and esotropia may run 24 to 96 hours, similar to many other cyclical or periodic biological phenomena of obscure mechanisms. Patients with cyclical esotropia can decompensate into a constant esotropia that can be corrected surgically. Ocular neuromyotonia is a brief episodic myotonic contraction of one or more muscles supplied by the ocular motor nerves, most commonly the oculomotor nerve. It may occur spontaneously or be provoked by prolonged gaze in a particular direction. Usually it results in esotropia of the affected eye accompanied by failure of elevation and depression of the globe. When the oculomotor nerve is affected, there may be associated signs of aberrant reinnervation (see Chapter 104). Ocular neuromyotonia occurs most often after radiation therapy for sellar region tumors. Less often it is associated with compressive lesions such as pituitary adenomas, cavernous sinus meningiomas or aneurysms, thyroid orbitopathy, radiation of a frontal lobe lesion (Whitted et al. Demyelinating lesions in the region of the third cranial nerve fascicle also can cause "paroxysmal spasm" of the muscles innervated by the oculomotor nerve but usually are accompaned by other findings such as eyelid retraction or paroxysmal limb dystonia. It should be distinguished from superior oblique myokymia and the spasms of cyclical oculomotor palsy. Cyclical oculomotor palsy is characterized by paresis alternating with "cyclic" spasms of both the extra- and intraocular muscles supplied by the oculomotor nerve. It is a rare condition usually noted in the first 2 years of life, although the majority of cases are believed to be congenital and are often associated with other features of birth trauma. During the spasms, which last 10 to 30 seconds, the upper eyelid elevates, the globe adducts, and the pupil and ciliary muscle constrict, causing miosis and increased accommodation (Loewenfeld, 1999); the paretic phase usually lasts longer. Spasms, often heralded by twitching of the upper lid, may be precipitated by intentional accommodation or adduction. The cycles usually persist throughout life, but the spasms of the extraocular muscles may abate, leaving only intermittent miosis. Symptomatic cyclical oculomotor palsy may occur in later life in patients with underlying lesions involving the third cranial nerve, but the features and cycles are atypical. The mechanism of cyclical spasms is unclear but is discussed elsewhere (Loewenfeld, 1999). Gaze-evoked phenomena such as end-point nystagmus, the oculoauricular phenomenon, and orbicularis oculi myokymia are physiological or benign. Electro-oculography, also known as electronystagmography (Chapter 46), is a popular method of quantitative oculography but has a limited range and is unreliable for vertical eye movements because of eyelid artifact. Damping of monocular pendular nystagmus with vibraton in a patient with multiple sclerosis. Therapy for paraneoplastic syndromes in six patients with protein A column immunoadsorption. Bowtie and upbeat nystagmus evolving into hemi-seesaw nystagmus in medial medullary infarction: Possible anatomic mechanisms. Ataxia with oculomotor apraxia type I in southern Italy: late onset and variable phenotype. Timing of surgery for infantile esotropia in humans: effects on cortical motion visual evoked responses. Familial horizontal gaze palsy with progressive scoliosis maps to chromosome 11q23-25. Congenital ocular motor apraxia with wheel-rolling ocular torsion-a neurodiagnostic phenotype of Joubert Syndrome. Opsoclonus-myoclonus syndrome in patients with locked-in syndrome: a therapeutic porthole with gabapentin. A randomized trial of 4-aminopyridine in ea2 and related familial episodic ataxias. Effects of acetazolamide on infantile nystagmus syndrome waveforms: comparisons to contact lenses and convergence in a well-studied subject. For the best possible vision, the image of the object of regard must fall onto the fovea, which is the most sensitive part of the macula. The cone photoreceptors, which mediate central and color vision, are greatest in density at the fovea. Visual acuity and cone density fall off rapidly as eccentricity from the fovea increases. For example, the retina 20 degrees eccentric to the fovea can only resolve objects equivalent to Snellen 20/200 (6/60 metric) optotypes or larger. Rod photoreceptors are present in highest numbers approximately 20 degrees from the fovea and are more abundant than cones in the more peripheral retina; rods function best in dim illumination. Each eye sends visual information, transduced by the retina, to both hemispheres of the brain by the optic nerves, each of which contains over 1 million axons. Axons that arise from the ganglion cells of the nasal retina of each eye decussate in the optic chiasm to the contralateral optic tract. The percentages of crossed and uncrossed axons in the human optic chiasm are approximately 53% and 47%, respectively. Similarly, the superior retina receives information from the inferior visual field, and vice versa. Axons from ipsilateral retinal ganglion cells synapse in layers 2, 3, and 5; contralateral axons synapse in layers 1, 4, and 6. The magnocellular pathway is concerned mainly with movement detection, detection of low contrast, and dynamic form perception. After projecting to the primary visual cortex (visual area 1, V1, or Brodmann area 17), information from the M pathway is distributed to V2 (part of area 18) and V5 (junction of areas 19 and 37). Information from the P pathway is distributed to V2 and V4 (fusiform gyrus) (Trobe, 2001). Since these fibers pass close to the tip of the temporal lobe, temporal lobectomy sometimes damages these fibers causing a "pie in the sky" homonymous visual field defect. The primary visual cortex (striate cortex, V1, or Brodmann area 17) is in the occipital lobe. Fibers from the macula project to the portion of the visual cortex closest to the occipital poles, while fibers from the peripheral retina project to the visual cortex lying more anteriorly. The nonoverlapping part of the most peripheral temporal visual field (monocular temporal crescent) arises from unpaired crossed axons from the nasal retina that project to the most anteromedial portion of the visual cortex. The primary visual cortex has interconnections with visual association areas concerned with color, motion, and object recognition (Trobe, 2001). Since many neurologists are not familiar with ophthalmic examination techniques, and ophthalmologists are often not experienced with neurological localization, the neuro-ophthalmological subspecialty provides a bridge between the two disciplines. Visual acuity should always be measured in each eye individually and with the best possible optical correction. The resulting measure, called bestcorrected visual acuity, is the only universally interpretable measurement of central visual function. Light-StressTest In some disorders of the macula, abnormalities are not apparent with the direct ophthalmoscope. The light-stress (or photo-stress) test is a useful method for determining whether reduced central vision is a consequence of macular dysfunction (Wall and Johnson, 2005). Then, with the eye with decreased vision occluded, the other eye is exposed to a bright light for 10 seconds. Immediately thereafter, the patient is instructed to read the next largest line on the eye chart, and the recovery period is timed. The same procedure is followed for the eye with decreased vision, and the results are compared. Fifty seconds is the upper limit of normal for visual recovery, although most normal subjects recover within several seconds. In patients with macular disease, the recovery period often takes several minutes. ColorVisionTesting Dyschromatopsia, especially if asymmetrical between the eyes, is an indication of optic nerve dysfunction, but can also occur with retinal disease (Almog and Nemet, 2010). A gross color vision defect is identifiable at the bedside by assessing for red desaturation. Asking for a comparison of red saturation on each side of fixation sometimes detects a subtle hemianopia. Formal measurements of color vision can be obtained with pseudoisochromatic color plates. The notation 20/20 (6/6 metric) indicates that the patient (numerator) is able to see the optotypes seen by a normal person at 20 feet (denominator). A visual acuity of 20/60 (6/18 metric) indicates that the patient sees an optotype at 20 feet that a normal person would see at 60 feet. A disparity between the distance and near visual acuities is often indicative of a specific problem. For example, the most common cause of better distance than near acuity is uncorrected presbyopia. Common causes of better near than distance acuity include myopia and congenital nystagmus. When measuring near vision, the reading card should be held at the specified distance of 14 inches (or 0. Both are useful, but in neurological practice, a near card with text measures visual acuity as well as reading ability to some degree. A disparity between the measurements from the two types of near card might suggest a disturbance of some other cortical function, such as language function (see Chapter 12). ExaminationofthePupils Examination of the pupils involves assessing pupil size and shape, the direct and consensual reactions to light, and the near response. If a difference in pupil size (anisocoria) is noted, look for ptosis and ocular motility deficits, keeping in mind the possibility of Horner syndrome or third cranial nerve palsy. Measurements of pupil size and light reaction are made in dim illumination with the patient fixating on an immobile distant target. If there is anisocoria, it is useful to measure pupil size in both darkness and bright light. Anisocoria due to oculosympathetic paresis (Horner syndrome) is often greater in the dark, because the affected pupil does not dilate well. With this method, a near reaction can be elicited even in a completely blind patient, owing to proprioceptive influences. The pupil shows light-near dissociation when the direct light reaction is less prominent than the near reaction. Light-near dissociation can be seen with parasympathetic denervation of the pupil. The swinging flashlight test compares the direct and consensual light reactions in the same eye. However, in patients with a unilateral or asymmetric optic neuropathy, because of reduction in the direct reaction as compared with the consensual reaction, the pupil of the eye with decreased vision dilates when re-illuminated. The patient should fixate on an immobile distant target to minimize fluctuations in pupillary size and accommodative miosis. Each pupil should be checked individually for its direct light response, which can be graded on a scale of 1 to 4 (see Table 45. The light should be moved quickly to illuminate each eye alternately every 1 second (the swinging flashlight test). Only 3 or 4 swings of the light should be made, to minimize bleaching of the retina, and subsequent slowing of the pupillary reactions. VisualFieldTesting Evaluation of the visual fields is vital in patients with visual loss. Several techniques can be used for visual field examination, ranging from simple confrontation testing to sophisticated threshold static perimetry. Confrontation testing should be part of the routine neurological examination, although it is insensitive for detection of mild visual field loss (Kerr et al. For the purposes of this discussion, the emphasis is on simple and practical techniques, while complicated methods are briefly summarized. For example, a patient with a central scotoma may report that the eyes and nose are missing, a patient with an inferior altitudinal visual field defect may report that the lower half of the face is missing, while a patient with homonymous hemianopia may report that one side of the face is missing. Although many methods are available, a simple, thorough examination can be done by finger counting in all four quadrants, coupled with hand comparison. Finger counting in the quadrants: the clinician holds up fingers sequentially in each of the four quadrants of the visual field and asks the patient to count the number seen. Then the patient is asked to add the total number of fingers shown with both hands. Visual inattention is often identifiable during this step of confrontation testing.
References
- Kole H. Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg Oral Med Oral Pathol 1959; 12:277.
- Chiesa Estomba CM, Reinoso FA, Velasquez AO, et al. Complications in CO2 laser transoral microsurgery for larynx carcinomas. Int Arch Otorhinolaryngol 2016;20(2):151-155.
- Hay JM, Peyrard P, Lautard M, et al. Closed peritoneal lavage in the diagnosis of non traumatic acute abdomen. Ital J Surg Sci. 1988;18(2):115-120.
- Exarhos DN, Malagari K, Tsatalou EG, et al. Acute mediastinitis: spectrum of computed tomography findings. Eur Radiol 2005; 15: 1569-1574.
- Bax JJ, Bleeker GB, Marwick TH, et al: Left ventricular dyssynchrony predicts response and prognosis after cardiac resynchronization therapy, J Am Coll Cardiol 44:1834-1840, 2004.
- Gelas T, Margain Deslandes L, Mestrallet G, et al: Spontaneous regression of suspected cystic dysplasia of the rete testis in three neonates, J Pediatr Urol 12(6):387.e1n387.e4, 2016.
- Davidson D, Barefield ES, Kaltwinkel J, Dudell G, Damask M, Straube R, et al. Safety of withdrawing inhaled nitric oxide therapy in persistent pulmonary hypertension. Pediatrics 1999;104:231-6.
- Bass JL, Gruenstein D. Transcatheter closure of the perimembranous ventricular septal defect-preclinical trial of a new Amplatzer device. Catheter Cardiovasc Interv. 2012; 79:1153-60.