Adrian S. Woolf, MD
- Professor of Nephrology and Head of Nephro-Urology Unit,
- Institute of Child Health, University College London,
- Great Ormond Street Hospital for Children, London, United Kingdom
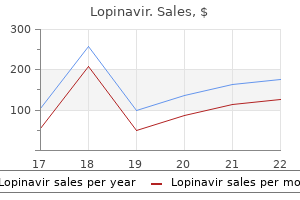
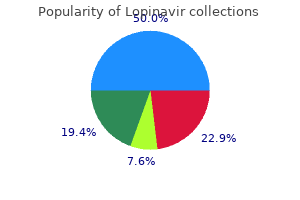
This information reveals issues directly or indirectly related to feeding and growth treatment yeast diaper rash order 250mg lopinavir overnight delivery. The other members of the team perform focused examinations related to their specialty treatment for uti purchase lopinavir without prescription. The physical examination of the child with feeding difficulties focuses on factors that might inhibit or contribute to the ability of the patient to adequately receive nutrition 25 medications to know for nclex 250 mg lopinavir otc. Examination of the head medicine 6469 discount lopinavir 250mg with visa, eyes medicine zithromax purchase 250mg lopinavir fast delivery, ears, nose, and throat includes assessment of overall facial tone, craniofacial anomalies, cleft lip or palate, dentition, asymmetry, tonsillar hypertrophy, and ankyloglossia (tongue tie). Anterior and posterior ankyloglossia have been controversial regarding the impact on feeding, and more specifically, breastfeeding. There are varying degrees of ankyloglossia and care should be taken to assess the function of the tongue as well as the appearance. The anterior lingual frenulum can be released rather easily if the membrane is thin and elastic. Also important to note, although ankyloglossia is often temporally related to feeding issues, it may not be causally related. The chest is assessed by auscultation of breath sounds, congestion, noisy breathing, and work of breathing. Aspiration of fluid into the lungs can contribute to increased rates of upper respiratory infections and pneumonia. The abdomen should be inspected for pain, tenderness, distention, and palpable stool on examination. Gastrostomy tubes are inspected for appropriate fit, leaking, skin irritation, erythema, and granulation tissue around the stoma. A rectal examination is beneficial for assessment of rectal tone, skin tags, fissures, hematochezia (passage of fresh blood through the anus, usually in or with stools), and stool in the rectal vault. Many children with feeding disorders have difficulty with constipation due to low tone, poor colonic motility, and lack of adequate hydration and poor diet. Vomiting and poor feeding tolerance can often be attributed to unmanaged constipation. Examination of the musculoskeletal system includes inspection of the spine for scoliosis, which in severe cases can cause compression of the stomach and decrease tolerance to volume. Muscle weakness and low tone can contribute to difficult positioning for feedings. Neurologic assessment includes level of alertness, hypotonia or hypertonia, ability to communicate, ability to interact and respond, and degree of neurologic impairment. Some patients have neuromuscular or neurologic disorders that progressively impair the ability to chew and swallow over time. These patients require frequent evaluation of their swallowing function through observation and swallowing studies. As such, behavior issues often need to be managed before feeding therapy can be effective. The nurse practitioner frequently requests input from the social worker to assess the needs of both the patient and the family to manage feeding concerns. The social worker often assists the nurse practitioner by working with families to locate resources such as 246 Pediatric dysPhagia: etiologies, diagnosis, and ManageMent early intervention, psychological or counseling services, mental health services, and feeding therapy. The social worker also assists the nurse practitioner by providing further explanation, education, and support to patients and caregivers regarding the feeding. Considerations for evaluation could start with medication trial or diagnostic testing. Cyproheptadine is often used for appetite stimulation, vomiting, and gastric accommodation. A gastric emptying scan can be done to evaluate emptying time at 1 and 2 hours after drinking/eating. Delayed gastric emptying can be treated with low dose erythromycin or cyproheptadine. The dietitian can recommend dietary adjustments to aid in comfort and feeding tolerance in the context of gastroparesis and delayed gastric emptying. The differential diagnosis would include erosive esophagitis, gastritis, eosin- ophilic esophagitis, Helicobacter pylori, or celiac disease. An impedance probe or pH probe is considered for a patient with reflux to assess acid versus non-acid events and to provide additional clinical data to determine if a fundoplication is warranted. Treatment typically begins with daily medication, including a stool softener (polyethylene glycol 3350) or a stimulant laxative. An abdominal X-ray can be ordered to assess stool load on patients who are difficult to physically assess. Retentive constipation that does not respond to daily treatment may require treatment with a bowel cleanout with a high dose of polyethylene glycol, suppositories, or enemas over 1 to 2 days. Specific directions for bowel cleanout are provided to the caregiver, taking age, weight, and volume tolerance into account. Patients with chronic constipation that is difficult to manage are generally referred to a gastroenterologist who specializes in motility. Our institution employs psychologists who specifically work with children who have feedingrelated anxiety. This patient population is often quite challenging, as some infants may refuse bottles, formula, and food, thus creating stress and anxiety among family members. Issues associated with maternal anxiety can include low milk supply, milk expression through pumping, refusing to feed while Mom is at work, difficulty finding caregivers, and night feeding. These certified health professionals come from various professional backgrounds and undergo specialized training in human lactation and breastfeeding. Although most feeding teams do not include a lactation consultant, this specialist can be a valuable resource for providing breastfeeding mothers with guidance and support. Facilitating cultural differences Having an understanding of cultural differences is often a key element in developing feeding strategies and achieving the desired outcomes. Many patients have extended family members who assist with the daily care of the child with feeding issues. Family dynamics can either strengthen or deter feeding strategies that are necessary to provide continuity and consistency with feeding management skills. Depending on the population being served, language barriers can also impact treatment. In this circumstance, the presence of a certified medical interpreter at all appointments is vital to successful treatment. The information gathered during this part of the visit includes a detailed diet and feeding history, a growth history, and documenta- tion of tolerance to foods, feeding schedule, and bowel habits. Anthropomorphic measurements are also obtained, including weight, height/length, and head circumference (for children younger than age 2). These measurements are then plotted on the appropriate growth 249 250 Pediatric dysPhagia: etiologies, diagnosis, and ManageMent chart for the child. The measurements should be compared with previous ones documented in records to determine if a child is achieving desired growth or is deviating from the growth curve. In addition to these two growth charts, there are disease-specific growth charts for children with specific conditions, including cerebral palsy, Down syndrome, and Noonan syndrome. However, given the small sample size used in establishing these charts, they are not considered optimal tools to measure growth. Measurement Equipment To obtain accurate anthropometric measurements, the following equipment must be available: n Infant scale that records within the nearest 0. Standardized scales have been developed for weight-for-age scores, height-for-age scores, and weight-for-height scores. A score of 0 to 1 is considered to be a child who is well nourished (1 standard deviation from the reference). Lastly, a score of more than 3 (above 3 standard deviations from the reference) is considered severely malnourished. The overall evaluation process includes the use of standardized clinical assessment protocols, informal clinical assessment measures, and instrumental evaluations. Knowledge of the underlying disease and whether it is developmental or degenerative is essential. This information is helpful in guiding assessment questions and the format of the clinical assessment. For example, if the patient has an underlying degenerative muscle disease, the evaluation may focus on current nutrition intake method, respiratory status, and the need for compensatory strategies as opposed to rehabilitation of the feeding or swallowing disorder. Discussion focuses on past medical history, developmental history, and the current issues and concerns with feeding and swallowing. Questions that are often posed to caregivers during n n (how many words, types of words, use of phrases or sentences) Slow feedings or mealtimes lasting longer than 30 minutes can be associated with oral motor or oral sensory issues with feeding. Does the child demonstrate any coughing, choking, gagging, color changes, increased congestion while eating and drinking These signs and symptoms may indicate possible airway compromise or swallowing dysfunction. Frequent snacking or "grazing" can interfere with establishing a strong hunger drive (appetite) and decrease hunger at mealtime. Frequent and large volume intake of liquids (juice or milk) may interfere with the hunger and appetite drives. Responses to these questions provide insight regarding typical behavioral responses and triggers for these responses. The protocols for oral motor/feeding assessment of infants and children are discussed in Chapter 29. The components of this evaluation are summarized as follows: n Review of gestational age, birth should be carefully observed in order to identify possible signs of fatigue or disorganization of feeding as feeding progresses. The overall volume of intake and the length of the feeding are considered; generally, feeding should not exceed 20 to 30 minutes. This examination encompasses (1) an assessment of the face, jaw, tongue, palate, oropharynx, and mucosa; (2) a functional assessment of the range and strength of the oral motor movements of the jaw, tongue, and lips; and (3) an assessment of secretion management ability. Direct observation of the child while feeding should occur during the evaluation, preferably while being fed by the parent or caregiver. This ensures that the assessment that is made is based on a representative feeding in terms of positioning, food and liquid types, and manner of presentation. Oral motor skills during feeding are assessed in relation to the expectations for chronologic age (see Chapter 6). A number of assessment measures are available for the evaluation of clinical oral motor feeding of children 6 months and older. The entire feeding 262 Pediatric dysPhagia: etiologies, diagnosis, and ManageMent condition. The clinical team may recommend that the physician consider an instrumental examination of swallowing to rule out swallowing abnormalities or airway protection issues during swallowing. Obtaining this information in a team format minimizes the need for the family to repeat their answers to multiple providers who must have the same information. Medical interventions should be reviewed as well as an assessment of the efficacy of the treatment. For example, a child with gastroesophageal reflux disease may be receiving treatment for this condition, yet the clinical signs of the condition may persist. Similarly, underlying neurologic conditions (cerebral palsy, seizure disorders) as well as developmental disabilities result-ing from prematurity, neuromuscular diseases, or genetic disorders may significantly impact oral sensorimotor skills for feeding. The presence of maladaptive feeding behaviors exhibited by the child may lead caregivers to initiate inappropriate interventions in their attempt to ensure adequate nutritional intake by the child. Underlying sensory processing issues may be exacerbated by attempts to force feed a child. For example, the practice of sitting on the floor during mealtimes may lead to problems with upright positioning in a child who has decreased motor control. Some families often cook with their traditional fragrant spices, which can negatively influence an interest in foods in a child with sensory issues. For a child with poor oral motor skills, handling foods such as rice may be difficult. It is also important to determine (1) if meals are limited to specific times with scheduled snacks or if the child is permitted to graze throughout the day, (2) if the child has free access to feedings at night, (3) if the child is expected to eat what is prepared for the family or if the family prepares separate meals for the child. Children with a limited preferred list of foods often cause increased stress with mealtimes in family members. During the interdisciplinary feeding team assessment, the child is fed by a parent to allow the team to observe interactions between the parent and the child during nutritive presentations. These children may move out of their seat and wipe their face or hands, which disrupts the presentation of another bite or drink. They may have specific dislikes and exhibit resistance to the parent offering a specific consistency of food (smooth or hard texture) and may accept only specific brands of food items or eat only selective foods and drinks. Some children refuse items that are not whole or foods that are not cut in a specific way. Others may require the removal of the crusts on bread or may insist that foods be a specific color or have no marks or blemishes. In children with olfactory overresponsiveness issues, the environment may contain sensory inputs that negatively impact feeding. Smells of cooking food may be overwhelming, affecting the ability of the child to sit at a table or remain in a lunch room. Some children may have decreased awareness to foods or liquids on their hands or face (the messy eater).
This confounder is more likely to occur in patients who are known to have a weakness in muscle function treatment centers for drug addiction buy discount lopinavir line, such as those with a history of muscular dystrophy everlast my medicine buy generic lopinavir 250 mg line, spinal muscular atrophy treatment that works order cheap lopinavir online, or metabolic disorders acute treatment cheap 250mg lopinavir mastercard. The size of the adenoids and tonsils and any impingement of these structures on the oropharyngeal airway are noted medications given during dialysis buy lopinavir 250mg. The lingual tonsils should be evaluated for the degree of effacement of the vallecular space. Additional structures to be identified include the epiglottis (posterior to the hyoid), the vallecular region (anterior to the upper portion of the epiglottis), the pyriform sinuses, the vestibule, and the tracheal air column. Performing the study Maximizing Information and Minimizing Radiation When infants are first offered a bottle, they rapidly ingest formula during the initial sucking burst. Ingestion then typically slows to a more sustained pattern of shorter sucking bursts and pauses during swallowing. After the initial assessment of several consecutive swallowing sequences, the fluoroscopy equipment is turned off. The beam is then turned back on at intervals while the infant continues to feed; this allows for the assessment of any possible fatigue effect and the deterioration of airway protection ability that may occur with ongoing swallowing effort. As the pharyngeal phase of the swallow is initiated, the fluid is transferred to the hypopharynx and consistent maintenance of airway protection as well as hypopharyngeal clearance must be demonstrated. Given that the pharynx is a shared pathway for breathing and swallowing, it is essential that airway closure and swallowing occur in a coordinated fashion. To prevent aspiration, the laryngeal airway closes and respiration ceases (swallowing apnea). If timely airway protection does not occur, penetration and/or aspiration will ensue. Laryngeal penetration occurs when fluid enters the airway but either remains above the vocal folds or is ejected from the larynx. In term infants, swallowing typically occurs at the end of inspiration, with an estimated duration of 0. In these infants, although the respiratory swallowing pattern remains coordinated, it may be inefficient due to the frequent respiratory pauses. They may also engage in continuous swallows during the apneic interval for prolonged periods of time, thereby increasing the risk for oxygen desaturation. Respiratory effort associated with feeding manifests differently depending on the developmental maturity of the infant. In some preterm infants, feeding overrides the normal chemoreceptor control of ventilation. Reduction of ventilation results in declining oxygenation and accumulation of carbon dioxide. For example, introducing pacing intervals during feeding (eg, imposing a pause by moving the nipple anteriorly to slow sucking) will interrupt sequential swallows, allowing adequate ventilation time and maintaining airway protection. Alternatively, decreasing the rate of liquid flow from the nipple will decrease the frequency of swallowing and swallowing-related apnea, thereby facilitating respiration and blood oxygen saturation. Oxygen desaturation can occur in the presence of normal swallowing patterns in infants with a variety of medical conditions. For example, despite having undergone cardiac repair, infants with a congenital cardiac anomaly may have poor cardiac output that affects oxygenation. Assessing the Swallow in Older Infants, Toddlers, and Children In older infants, toddlers, and children, sequential swallows are viewed during bottle feeding of liquids or purees or during fluid intake from a sipper cup or straw cup, as developmentally appropriate. In children who are able to spoon-feed, observations are made regarding oral transit, the adequacy of velopharyngeal closure during swallowing, the timeliness of swallowing initiation, the adequacy of airway protection, and the degree of hypopharyngeal clearance following the swallow. Difficulties with various textures can be observed; however, viewing all of the textures children may or may not accept in their usual diets is not essential. An upper gastrointestinal series may therefore be required for a subgroup of infants and children who present with feeding refusal, frequent emesis episodes, or other indications of gastrointestinal structural or functional issues. This study provides an image of the esophagus, stomach, and duodenum (small intestine) and identifies conditions such as esophageal strictures, webs, vascular rings, achalasia, tracheoesophageal fistula, and intestinal malrotation. This twisting between the first and second parts of the small intestine causes a mechanical obstruction. Alterations in positioning facilitate respiration and swallowing coordination and help to relieve upper airway obstruction that may occur in association with feeding. For example, infants with mandibular retrognathia may benefit from being in a side-lying position; this promotes anterior tongue positioning and decreases the likelihood of posterior displacement of the tongue and upper airway obstruction during feeding. The rationale for this strategy is that the imposed pause intervals allow the infant to optimize the coordination of respiration with sucking and swallowing. Modification of Flow Rate Modulating the flow of liquid is a commonly used strategy to facilitate the safety and efficiency of swallowing during bottle-feeding in both preterm and term infants. Decreasing the flow rate and thereby decreasing overall swallowing frequency provides more ventilation time; this increased time facilitates the coordination of swallowing and respiration. Nipples vary in terms of the type of hole they have, the type of material they are made of, and their shape. There is wide variability in flow rates, particularly for disposable nipples, Alterations in Positioning Establishing optimal positioning is basic to facilitating coordinated oral motor movements and swallowing safety. To facilitate swallowing safety, infants and children with underlying abnormalities in muscle tone require 30. Changes in Liquid Viscosity the rationale for altering the viscosity of liquid is that the reduced flow rate may facilitate oral control and provide increased time for the patient to achieve airway closure and thus airway protection during the swallow. Although thickening liquids is frequently used in the care of pediatric patients, there are significant implications for its use and a lack of evidence regarding its effect on long-term outcomes. Multiple methods for thickening liquids exist, including the use of rice cereal, pureed fruit, xanthan gum, and a wide variety of commercial thickening products. The viscosity of liquids varies based on the product used to thicken these liquids, and there is no universal protocol for the use of thickened liquids or for transitioning patients away from thickened liquids (see Chapter 38 for a more detailed discussion of viscosity). These ratings were developed and tested by Martin-Harris and colleagues28 over a 5-year period for content, reliability, and both construct validity and external validity. The quantification of physiologic swallowing impairment is intended to track the trajectory of swallowing impairment throughout development in young children. Altering Bolus Sensorimotor Properties There is considerably less available evidence in children than in adults regarding the effects of altering bolus sensorimotor properties on oropharyngeal muscle activity during swallowing. Although limited, available research has shown that significant differences in the duration and magnitude of muscle activity result as a function of bolus consistency. The professional team provides an explanation of key findings such as aspiration or significant residue following swallows. Recommendations to improve the safety and efficiency of the swallow may include altering the manner of feeding or the types of liquid and food offered to the child. Dysphagia treatment may be necessary to direct the patient and family in learning strategies to improve swallowing function. Referrals may also be made to other medical or surgical specialists to evaluate possible structural or functional abnormalities associated with swallowing dysfunction. A coordinated, interdisciplinary approach to assessment leads to appropriate management. Ideally, a single collaborative report summarizing examination findings is generated. The editors would like to thank Christopher Young, Radiology Assistant, for his efforts in collecting many of the radiographs for this chapter. Pediatric Videofluoroscopic Swallow Studies: A Professional Manual with Caregiver Guidelines. Guidelines for Speech-Language Pathologists Performing Videofluoroscopic Swallowing studies. Balance between radiation risks and obtaining a complete videofluoroscopic swallow study in pediatric patients. Management of pediatric radiation dose using Philips fluoroscopy systems DoseWise: perfect image, perfect sense. Image gently, step lightly: increasing radiation dose awareness in pediatric interventions through an international social marketing campaign. Use of medical imaging procedures with ionizing radiation in children: a population-based study. Nutritive and non-nutritive swallowing apnea duration in term infants: implications for neural control mechanisms. Maturational changes in the rhythms, patterning, and coordination of respiration and swallow during feeding in preterm and term infants. Development of co-ordination of sucking, swallowing and breathing: ultrasound study of term and preterm infants. Improving bottle feeding in preterm infants: investigating the elevated side-lying position. Effects of nonnutritive sucking on behavioral organization and feeding perfor- 24. Coregulated approach to feeding preterm infants with lung disease: effects during feeding. It allows the radiologist and the speech-language pathologist to take a careful look at the process of swallowing. To ensure the best possible study, please provide your child with an explanation of what will occur during the study. The speech-language pathologist will be present during the test and may ask the child to change position or try different textured foods or liquids in order to help find the safest and best way for the child to eat. Although the videofluoroscopic swallowing study does not hurt, children may not like the taste of the food or liquid mixed with barium. Because they are often more cooperative and less apprehensive when a loved one is with them, we encourage you to stay with your child during the test. For children who receive tube feedings, these feedings should also be stopped 4 hours before the study. This is not cause for concern, and encouraging your child to drink fluids will allow the stool to return to normal within a short time. It is necessary to drink the barium, or in some cases, to mix the barium with the food or liquid so that it will highlight the throat on the X-rays. To make children more comfortable during the test, a parent may be asked to feed the barium-prepared items to the child. The children tolerated advancement of the scope without difficulty, allowing clinicians to ensure that the pres- 31. Findings revealed good validity and reliability between the two procedures with regard to the judgment of bolus transfer control, laryngeal penetration and depth, and aspiration. The overall clinical results were similar and the resultant clinical recommendations derived from all three studies performed on these children were virtually identical. Both professionals must have expertise in the diagnosis and management of infants and children with swallowing disorders. Although the scheduler at our institution provides an overview of the procedure, often a nurse or a nurse practitioner has a further explanatory conversation. Although a videoendoscope provides the best image quality, its larger size may limit its applicability. To ensure that the endoscope is not dislodged, the nurse also monitors arm and hand position. Infants and children are positioned in a sitting, semi-reclined, side- lying, or cradle position, depending on what simulates their feeding experience at home. Breastfeeding infants are positioned upright for scope insertion and are repositioned for the exam. Doing this atraumatically and comfortably requires the proceduralist to maintain the endoscope within the lumen of the aerodigestive tract, thereby minimizing contact of the endoscope with the medial or lateral walls of the nose. Ideally, the endoscope is held between the thumb and the index finger of the nondominant hand. The third, fourth, and fifth fingers should rest on the nasal bridge and forehead of the patient to minimize relative motion of the endoscope should children move their head. The scope should be passed through the nasal vestibule, with the proceduralist visualizing the nasal septum medially and the head of the inferior turbinate laterally. The nasopharynx is reached when the scope is passed through the posterior choanae. The adenoid pad is seen superiorly in the nasopharynx, and the soft palate is seen inferiorly. The scope should be kept in the midline and passed posteriorly over the free edge of the soft palate. Soft palate closure can be assessed as it closes against the posterior pharyngeal wall. As the scope passes over the posterior soft palate, the hypopharynx can be visualized ahead. Ideally, it is placed below the velopharyngeal valve, just above the tip of the epiglottis. This allows visualization of the valleculae, pyriform sinuses, and the endolarynx. Touching the posterior wall of the pharynx or any of the laryngeal structures will induce a gag response. Given that the larynx will elevate during the swallow, the proceduralist must anticipate this motion and position the endoscope appropriately to prevent contact with the rising larynx. At times, the floor of the nose will be narrowed by a septal deviation or a prominent spur of the maxillary crest (bone upon which the septum rests). In this scenario, the endoscope may not pass easily beyond the obstruction without causing pain or discomfort.
Proven lopinavir 250mg. Hypotonic isotonic and hypertonic solutions (tonicity) | Khan Academy.
Children with chronic aspiration may have recurrent lower respiratory tract infections affecting multiple lobes of the lung 9 treatment issues specific to prisons purchase 250mg lopinavir otc. The latter clinical scenario may be more likely to occur when a child spends considerable time in one position medical treatment 80ddb generic lopinavir 250 mg otc, such as an infant who remains supine after feeds or a neurologically impaired child who preferentially is positioned on one side symptoms to pregnancy purchase lopinavir with visa. Chronic aspiration should be strongly considered for any child with recurrent pneumonia and an underly- may be obtained to evaluate the cause of chronic or recurrent respiratory symptoms or to screen for sequelae of chronic aspiration symptoms tonsillitis buy lopinavir 250mg fast delivery. The chest radiograph should be ordered to provide both a frontal view and a lateral view treatment brachioradial pruritus generic 250mg lopinavir visa. The central airways should be assessed for evidence of obstruction or compression. Mediastinal masses may be obvious on a chest radiograph and may displace the trachea. Vascular compression of the distal trachea from a right-sided aortic arch may be suspected based on findings on a frontal chest radiograph. The size of the heart should be noted, as cardiomegaly may be associated with pulmonary edema. Peribronchial cuffing, a haziness or thickening surrounding the bronchial walls when viewed "on end," can be seen in 218 Pediatric dysPhagia: etiologies, diagnosis, and ManageMent patients with asthma. Severe bronchiectasis can be identified on chest radiographs and can be seen in patients with cystic fibrosis, primary ciliary dyskinesia, retained foreign body, and immunodeficiency, as well as in children with chronic aspiration. Finally, the lung fields should be closely examined to evaluate for signs of airspace disease, interstitial disease, atelectasis (collapse), pulmonary nodules, or evidence of pleural fluid. If there has been a recent significant aspiration event, there may be evidence of airspace disease; however, this finding is non-specific and is often not visible immediately following an aspiration event. In children with chronic aspiration and subsequent lung disease, there may be evidence of subsegmental atelectasis, infiltrates, hyperinflation, or peribronchial cuffing. Enlarged distal bronchi on a chest radiograph may be noted by the presence of the "tram track" sign (bronchial walls running parallel to each other), which reflects dilated, non-tapering bronchi. The right upper lobe is more commonly affected in infants who are often supine during episodes of aspiration, whereas older children who are usually upright are more likely to have lower lobe involvement. There may also be evidence of mucus impaction of distal airways, which may be represented by tree-in-bud opacities in the central or peripheral lung fields. It is a non-specific finding that implies impaction of secretions within bronchioles, the smallest airway passages in the lung. When coupled with impaired secretion clearance, this may result in additional airway damage and inflammation, creating a "vicious circle" that leads to structural airway changes and bronchial dilation. Early bronchiectasis is cylindrical, which is visualized when a bronchus is noted to be larger than the accompanying branch pulmonary artery. The pulmonologist is responsible for both the evaluation and medical management of children with bronchiectasis. Although this disease is not uncommon in children with chronic aspiration, it is more frequently seen in children with neurologic impairment. Digital clubbing, which refers to the loss of the normal angle between the nail bed and the cuticle, is also seen in some children. There is a significant burden of disease and impact on the quality of life for children with bronchiectasis. These children experience increased anxiety, depression, and stress associated with symptom exacerbation. Serum tests for allergic bronchopulmonary aspergillosis can be considered for children with wheezing refractory to bronchodilator therapy. Bronchoscopic airway evaluation should be considered to rule out airway abnormalities and to evaluate for lower airway inflammation or infection. The majority of cases occur in people with underlying illnesses but with otherwise normal immune systems. Dilation of peripheral bronchi results in the loss of structural integrity of the lower airways and difficulty clearing secretions during coughing. Additionally, chronic inflammation of the lower airways damages the cilia that line the airway, impairing the "mucociliary elevator," which refers to the natural movement of lower airway secretions to the oropharynx where secretions can be swallowed or expectorated. Airway clearance modalities can assist in improving both cough clearance and mucociliary clearance. In younger children or children who are neurologically impaired, airway clearance is passive in the form of chest physiotherapy or vest therapy. Despite a lack of clear evidence, airway clearance is commonly used by pulmonologists as part of the treatment regimen for children with bronchiectasis. It does so by chemically changing the viscosity of the mucus, allowing it to be more easily expelled. Exacerbations of bronchiectasis are primarily treated with targeted antimicrobial therapy. During exacerbations, children may develop a worsening cough, chest congestion, or even chest pain or dyspnea. If they are able to expectorate sputum, the use of an antibiotic tailored to culture results is appropriate. If respiratory cultures cannot be obtained, empiric treatment can be initiated to address the most common infectious agents: Haemophilus influenzae, Streptococcus pneumoniae, Moraxella 20. Loss of cartilaginous airway support from bronchiectasis may result in chronic obstructive lung disease. Vascular proliferation along the bronchial mucosa may occur due to chronic hypoxia, and this may result in intermittent or life-threatening hemoptysis or lower airway hemorrhage. In some cases, disease may progress to the extent where lobectomy or pneumonectomy is recommended if the diseased lung is focal. Pulmonary Function Testing Spirometry is a simple and inexpensive test that can be performed in an office setting to evaluate how well a child inhales and exhales. By assessing airflow limitation during inhalation and exhalation, spirometry can be used as a screening tool for general respiratory health. Rates of acceptability increase with increasing age; however, even some adults are unable to perform acceptable spirometry. Asthma is characterized by obstruction of small airways due to chronic inflammation and bronchoconstriction. When a bronchodilator such as albuterol is administered in the pulmonary function laboratory, improvement in airflow may be noted during spirometry. Children with other diseases, including cystic fibrosis and primary ciliary dyskinesia, may also have demonstrable obstructive ventilatory limitation on spirometry, though these children are less likely to improve with the administration of a bronchodilator. Similarly, children with bronchiectasis may have obstructive ventilatory limitation on spirometry if the degree of bronchiectasis is so great that it causes bronchial collapse during forced expiration. Also, those with obstructive ventilatory limitation due to bronchiectasis are unlikely to show improvement with administration of a bronchodilator. If there is no improvement in lung function or an appreciable decrease in severity or frequency of respiratory symptoms, treatment with bronchodilators or inhaled corticosteroids may not provide any significant clinical benefit. Flexible Bronchoscopy Flexible bronchoscopy is an important adjunct to the evaluation of children with chronic pulmonary aspiration. It can assist in identifying anatomic abnormalities that would predispose a child to aspiration, rule out additional causes of chronic respiratory symptoms, and assess visual or cellular evidence of inflammation or infection of the lower airways. In cases of acute aspiration, flexible bronchoscopy may be therapeutic, as debris can be suctioned from the airway and the risk of developing an infection is reduced. Flexible bronchoscopy is best performed under light anesthesia without an artificial airway. This allows for a structural and dynamic assessment of both the upper and lower airways, which is critical when evaluating a child with chronic cough or other respiratory symptoms. Findings in the upper airway, including posterior pharyngeal cobblestoning or laryngeal edema, 20. Purulent nasal drainage may be present in children with chronic sinusitis or primary ciliary dyskinesia. Lower airway findings, including endobronchial lesions or airway foreign bodies, should be ruled out when evaluating a child with chronic cough or wheezing. If coughing is elicited during the procedure, dynamic collapse of the trachea or mainstem bronchi can be visualized, suggesting tracheomalacia or bronchomalacia as a possible etiology for the chronic cough. When evaluating a child with known or suspected aspiration, anatomic abnormalities including a laryngeal cleft or tracheoesophageal fistula should be considered. Rigid bronchoscopy allows better visualization of the posterior larynx and tracheal wall, enabling detection of a small tracheoesophageal fistula. Although laryngeal clefts can sometimes be detected by flexible bronchoscopy, rigid bronchoscopy is the preferred procedure due to the ability to manipulate tissue and more closely examine the posterior commissure. Flexible bronchoscopy also allows for a visual assessment of inflammation of the lower airways. The bronchial mucosa appears edematous, with poor vascular definition when chronically inflamed. Direct visualization of the bronchi also allows for an assessment of the secretion burden of the lower airways. Increased thin and frothy secretions may coat the lower airways with aspiration of saliva. Thick, purulent secretions may be present with acute or chronic infection due to aspiration. Children with bronchiectasis may have chronic purulent lung disease and may have significant difficulty clearing secretions from the lower airways. Collection of a small-volume lavage specimen of the distal airways can assist in the evaluation of the child with chronic aspiration. This is a phagocytic cell that is responsible for engulfing and disposing of foreign material and infectious agents in the lung. Since lipids are present in organic material, lipid may be seen in macrophages following aspiration of food. It generally affects children younger than 2 years of age and can lead to severe respiratory compromise that requires treatment in an intensive care unit. Gastric pepsin has been noted to be elevated in critically ill neonates and children when intubated. Currently, airway pepsin is not widely used as a marker for chronic pulmonary aspiration. She is dependent on a tracheostomy tube and ventilator at home when both awake and with sleep. A chest radiograph obtained prior to the clinic visit reveals subsegmental atelectasis in the right upper lobe. A formal airway evaluation under anesthesia using flexible bronchoscopy and rigid bronchoscopy was scheduled. The flexible bronchoscopy revealed diffuse lower airway inflammation and increased thin and frothy secretions throughout the lower airway. The patient, who refused thickened liquids, purees, or solids, was restricted from oral intake while working with a speech pathologist in the outpatient setting. The child was scheduled for Botox injections of the parotid and submandibular glands and subsequently had a marked decrease in the need for tracheal suctioning. The patient remained out of the hospital and was weaned from daytime ventilator support, requiring ventilation only during sleep. She remained well, requiring infrequent suctioning following treatment of her salivary glands. Advances in the diagnosis and management of chronic pulmonary aspiration in children. Aspiration and non-aspiration pneumonia in hospitalized children with neurologic impairment. Clinical signs and symptoms of oropharyngeal aspiration and dysphagia in children. Gastroesophageal reflux-associated recurrent pneumonia and chronic asthma in children. A clinical index to define risk of asthma in young children with recurrent wheezing. Pediatric vocal fold paralysis after cardiac surgery: rate of recovery and sequelae. Reversible bronchial dilatation in children: comparison of serial high-resolution computer tomography scans of the lungs. Bronchiectasis in chronic pulmonary aspiration: risk factors and clinical implications. Non-cystic fibrosis bronchiectasis in children: clinical profile, etiology and outcome. Bronchoscopy contributes to the clinical management of indigenous children newly diagnosed with bronchiectasis. A randomized crossover trial of chest physiotherapy in non-cystic fibrosis bronchiectasis. Withdrawal of inhaled steroids in children with non-cystic fibrosis bronchiectasis. Longterm azithromycin for Indigenous children with non-cystic-fibrosis bronchiectasis or chronic suppurative lung disease (Bronchiectasis Intervention Study): a multicentre, double-blind, randomised controlled trial. The lipid-laden alveolar macrophage as a marker of aspiration in parenchymal lung disease. Bronchoalveolar lavage and esophageal pH monitoring data in children with "difficult to treat" respiratory symptoms. Lipid-laden macrophage index and inflammation in bronchoalveolar lavage fluids in children. Gastric vs small-bowel feeding in critically ill children receiving mechanical ventilation: a randomized controlled trial. Pepsin, a marker of gastric contents, is increased in tracheal aspirates from preterm infants who develop bronchopulmonary dysplasia. Pepsin in bronchoalveolar lavage fluid: a specific and sensitive method of diagnosing gastro-oesophageal reflux-related pulmonary aspiration.
Typically medications safe while breastfeeding cheap 250 mg lopinavir mastercard, the abnormal cortex is still functional medicine runny nose purchase lopinavir paypal, and the surrounding normal-appearing cortex is epileptogenic medications not to take during pregnancy purchase lopinavir 250mg free shipping, probably because of an abnormal connectivity symptoms gluten intolerance buy lopinavir 250mg online. The medial cortex on the right side is thick and dark (diffuse microcalcification) treatment authorization request cheap lopinavir 250mg on line, while the underlying white matter is bright. In this patient with severe gelastic seizures, a small hypothalamic mass is seen attached to the ventricular side of the mammillary body; the T2 signal is slightly brighter than that of the hemispheric cortex. Classic appearance of the hippocampal sclerosis: bright T2 signal of the left hippocampal head, loss of the internal structure. Hippocampal Sclerosis While hippocampal sclerosis is the most common epileptogenic substrate seen in adult surgical epilepsy series, it is less common in children. Hippocampal volume reduction correlates with the severity of the neuronal cell loss. Surgical indications for schizencephaly-associated epilepsy are uncommon but there are reports of successful surgery of closed lip schizencephaly. A distinction is made between the more anterior parahypothalamic pedunculated hamartomas clinically associated with a central precocious puberty; and the more posterior intrahypothalamic (sessile) hamartomas connected to the mammillary bodies, clinically associated with an early onset severe, typically gelastic epilepsy (which over time results in cognitive deterioration and behavioral problems). There is no enhancement or calcification; a hypothalamic hamartoma may uncommonly be cystic. Uni- or bilateral, intra- or extraventricular, symmetric or not, the mass is of variable size, and grows in proportion to the brain only. It may extend anteriorly to the pituitary stalk, and posteriorly may splay the cerebral peduncles apart and displace the basilar artery. Epilepsy-associated hypothalamic hamartoma can be treated with surgical disconnection or radiosurgery. Clinically, the seizures begin abruptly in a previously normal child and include partial seizures and epilepsia partialis continua. With disease progression, the patients in months develop hemiparesis or hemiplegia and marked cognitive decline. Three years later (b), prominent parenchymal volume loss with extension of the cortical necrosis. The lateral ventricle is larger than before on the right side but also on the left side. Medical treatments are not really efficient, and surgical hemispherectomy may be the best option to stop the progression of the disease. If the medical treatment fails, hemispherectomy may be required on the condition that the other hemisphere is not involved. Using fat saturation, it may show associated abnormalities of the ocular choroid and in the calvarium as well. Acute ischemia with focal edema, bleed or diffuse hemispheric swelling from prolonged seizure activity may be demonstrated. Hemispheric atrophy may result from the seizure activity and/or from the perfusion defect. In infants, the white matter may present with the low T2 signal of a seizure-induced early myelination. Arteriovenous malformations are usually not epileptogenic in children, except for large ones. In severe cases, surgery for removal of the epileptogenic cortex may be an option. Yield of emergent neuroimaging among children presenting with a first complex febrile seizure. Neuro-imaging evaluation after the first afebrile seizure in children: a retrospective observational study. Metabolic and electrophysiological alterations in subtypes of temporal lobe epilepsy: a combined proton magnetic resonance spectroscopic imaging and depth electrodes study. Evaluation of subcortical white matter and deep white matter tracts in malformations of cortical development. Diffusion tensor tractography imaging in pediatric epilepsy - A systematic review. Intersubject variability in the anterior extent of the optic radiation assessed by tractography. Epilepsy surgery: recent advances in brain mapping, neuroimaging and surgical procedures. Disrupted global and regional structural network and subnetworks in children with localization-related epilepsy. The spectrum of longterm epilepsy-associated tumors: long-term seizure and tumor outcome and neurosurgical aspects. Evidence for developmental precursor lesions in epilepsy-associated glioneuronal tumors. Supratentorial gangliogliomas: histopathologic grading and tumor recurrence in 184 patients with a median follow-up of 8 years. Pleomorphic xanthoastrocytoma, a distinctive astroglial tumor: neuroradiologic and pathologic features. Pleomorphic xanthoastrocytoma: a developmental glioneuronal tumor with prominent glioproliferative changes. Association of pleomorphic xanthoastrocytoma with cortical dysplasia and neuronal tumors. Prenatal and early postnatal ontogenesis of the human motor cortex: a golgi study. Shaken infant syndrome: developmental neuropathology, progressive cortical dysplasia, and epilepsy. Cortical perivascular satellitosis in intractable epilepsy: a form of cortical dysplasia Mild malformation of cortical development with oligodendroglial hyperplasia in frontal lobe epilepsy: a new clinic-pathological entity. Hemispheric malformations of cortical development: surgical indications and approach. Surgical management of medically refractory epilepsy in patients with polymicrogyria. This is particularly true for presurgical investigations of cognitive and motor functions. The factors that have contributed to its success are chiefly its noninvasiveness, reproducibility, and wide availability. Finally, we will briefly mention developments in the mapping of blood flow changes associated with epileptic activity. Stimulation tasks are tailored to the cognitive domains under investigation, using visual or auditory stimulus presentation. The most commonly used task to assess hemispheric dominance for expressive language is silent word generation to letters (fluency) or words (verb or synonym generation). Other language tasks include story comprehension, semantic decision-making (based on an object description,9 or "gap filling" in heard stories). The main questions are whether surgery is planned in the language-dominant hemisphere and whether language cortex is located near the planned resection. More recent investigations, with the benefit of modern neuroimaging, have, nevertheless, shown that a considerable proportion of patients with early acquired or developmental left-sided perisylvian lesions showed evidence of intrahemispheric reorganization of language. This latter finding points to the possibility that epileptic activity drives functional reorganization. This study also indicated that structural brain asymmetries, such as a short planum temporale in the right hemisphere, can constrain the likelihood of language reorganization to the right, contralesional hemisphere. Although this has generally worked well with most patients, it has the disadvantage of being prone to ambiguous results if activation patterns are atypical or in loss of activation in less cooperative patients. More recent studies have used experimental protocols that require patients to respond using button presses to indicate a choice between different stimulus categories or presence of certain target items. The induced subtle movement artifacts can be reduced using modern motion- and artifact-suppression post-processing methods, such as motion fingerprint14 and functional image artefact correction heuristic. The expressive language task (verb generation) activates left inferior frontal and posterior temporal regions, while the receptive task (story comprehension) recruits mainly right temporal regions. Extreme discordance was rare (< 2%) and could be due to crossed language dominance between frontal and temporal regions, which was not assessed in this study. If replicated, these findings are promising for the evaluation of less cooperative patients. The study by Roux et al54 showed less encouraging results (maximal sensitivity 66% for combined verb generation and naming tasks) and highlighted the challenges in combining both modalities. It also appears that tasks that involve sentence comprehension are better suited to activate temporoparietal language areas than those that use single-word or item processing. By contrast, Rutten et al53 used an operator-independent, fixed threshold: perhaps favored by a good signal-to-noise ratio in their study. A recent series in 20 children showed excellent concordance with no case of discordant classification. Sensitivity ranged from 59 to 100% and specificity from 0 to 97% across studies with variable methodology. While the long-term outcome in children is more favorable than in adults, with most children recovering to preoperative memory performance,58 there is nevertheless a risk for significant memory deficits in the short term. Note: the crosshair indicates the local maximum activation using silent verb generation task. A priori allocation of a region of interest is crucial: topographically unrelated co-(de)activation may lack a clinical relevance. Pediatric Studies Encouraging findings have been obtained in a prospective cohort of 53 children with pharmacoresistant focal epilepsy. Assessing the feasibility of surgical resection and predicting its risk for cognition. However, the level of evidence to support the replacement of invasive techniques may vary between types of epileptogenic lesions. This includes improvements in image acquisition and task design as well as post-processing. Higher field strengths have resulted in better signal-to-noise ratio and reduced scanning times. Monitoring of task performance, including overt speech, during scanning can reduce ambiguity of atypical References 1. Organization of language networks in children: functional magnetic resonance imaging studies. Left hippocampal pathology is associated with atypical language lateralization in patients with focal epilepsy. Asymmetry of planum temporale constrains interhemispheric language plasticity in children with focal epilepsy. A reconsideration of bilateral language representation based on the intracarotid amobarbital procedure. Use of preoperative functional neuroimaging to predict language deficits from epilepsy surgery. An update on determination of language dominance in screening for epilepsy surgery: the Wada test and newer noninvasive alternatives. Discrepant findings for Wada test and functional magnetic resonance imaging with regard to language function: use of electrocortical stimulation mapping to confirm results. Intrahemispheric reorganization of language in children with medically intractable epilepsy of the left hemisphere. Language plasticity after hemispherotomy of the dominant hemisphere in 3 patients: Implication of non-linguistic networks. Language functional magnetic resonance imaging in preoperative assessment of language areas: correlation with direct cortical stimulation. Is preoperative functional magnetic resonance imaging reliable for language areas mapping in brain tumor surgery Review of language functional magnetic resonance imaging and direct cortical stimulation correlation studies. Presurgical language mapping in children with epilepsy: clinical usefulness of functional magnetic resonance imaging for the planning of cortical stimulation. Pre- and postoperative verbal memory in pediatric patients with temporal lobe epilepsy. Verbal memory after temporal lobe epilepsy surgery in children: do only mesial structures matter Reorganization of verbal and nonverbal memory in temporal lobe epilepsy due to unilateral hippocampal sclerosis. Lateralization of hippocampal activation differs between left and right temporal lobe epilepsy patients and correlates with postsurgical verbal learning decrement. Hippocampal adequacy versus functional reserve: predicting memory functions following temporal lobectomy. Combined electroencephalography-functional magnetic resonance imaging and electrical source imaging improves localization of pediatric focal epilepsy. The former images localization-specific cerebral perfusion, and the latter cerebral glucose utilization, as the guiding principles in identification of the seizure onset zone. These techniques aid not only in the identification of a surgical target, but also in visualizing secondary epileptic foci, dual diagnoses, cortical function, postsurgical targeting for second resections, and surgical outcome prognostication. Almost 25% of epileptic patients do not respond to multiple antiepileptic treatments and will have intractable. These patients can be helped by surgically removing the epileptogenic region of the cerebral cortex. However, to accomplish this, the epileptogenic region has to be precisely delineated before surgery.
References
- Kalish RJ, Clancy PE, Orringer MB, Appelman HD. Clinical, epidemiologic, and morphologic comparison between adenocarcinomas arising in Barrett's esophageal mucosa and in the gastric cardia. Gastroenterology 1984;86:461.
- Brin MF, Kirby RS, Slavotinek A, et al: Pregnancy outcomes following exposure to onabotulinumtoxinA, Pharmacoepidemiol Drug Saf 25(2):179-187, 2016.
- Lopez JA, Jarow JP: Penile vascular evaluation of men with Peyronieis disease, J Urol 149(1):53n55, 1993.
- RCOG Guideline No. 51 Management of Monochorionic Twin Pregnancy. London: RCOG, 2009.
- Gorton E, Whitfield HN: Renal calculi in pregnancy, Br J Urol 80(Suppl 1):4-9, 1997.