Dean R. Cerio, MD
- Instructor, Division of Plastic Surgery
- Department of Surgery
- University of Alabama at Birmingham School of Medicine
- Birmingham, Alabama
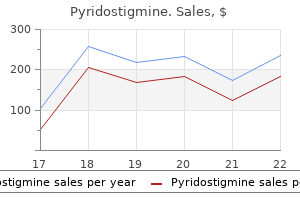
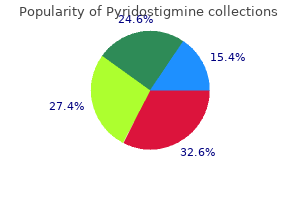
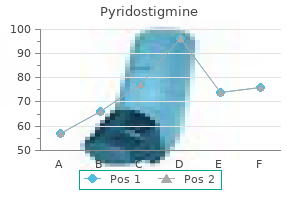
Peripherally acting -receptor antagonists Naloxone is a centrally acting opioid antagonist muscle relaxant for back pain purchase pyridostigmine american express. Naloxone crosses the blood brain barrier and it may precipitate opioid withdrawal symptoms infantile spasms 2012 buy cheap pyridostigmine line. Agents, which specifically block the peripheral actions of opioids and do not lead to opioid withdrawal and antagonize the centrally mediated analgesic effects, will be advantageous. All the following agents increase spontaneous bowel movements and reduce other bowel symptoms compared to placebo in patients who are on chronic opioids for non-cancer pain. None of these drugs are associated with serious adverse effects and have no cardiovascular events associated with their use. Methylnaltrexone (Relistor, Salix) Methylnaltrexone is a quaternary N-methyl derivative of the -opioid receptor antagonist naltrexone. The addition of a methyl group decreases its lipid solubility and increases polarity, preventing it from crossing into the brain [26]. Therefore, it does not reverse centrally mediated opioid analgesia or precipitate withdrawal. The study included a 1-week open-label phase followed by a three-week open-label extension phase to explore the persistence of any benefit. This study compared subcutaneous methylnaltrexone 12 mg once daily, 12 mg every other day or subcutaneous placebo for 4 weeks. Change from baseline in mean weekly bowel movement, bowel movement straining scale score, Bristol stool scale score and complete evacuation from base line improved (all P < 0. All events occurred in patients with underlying cardiovascular disease or cardiovascular risk factors. The investigators concluded that there was no clear pattern and evidence to suggest causal relationship between these cardiac events and methylnaltrexone. The reduced dose of 150 mg orally and 6 mg subcutaneous injection daily is recommended for patients with renal and hepatic impairment. Naloxone is a potent -receptor antagonist however, blood brain barrier penetration and extensive first pass metabolism limits it use. Naloxegol acts peripherally without affecting the central actions of opioids because the polyethylene glycol moiety limits naloxegol capacity to cross the blood brain barrier. Adverse event leading to discontinuation of treatment were abdominal pain and diarrhea. Most adverse events in the naloxegol group were mild to moderate in severity, occurred early and resolved during or after discontinuation, 11 patient discontinued use due to diarrhea and nine patients due to abdominal pain. No treatment related death, cardiovascular event or bowel perforation occurred during this study. Naloxegol did not cause opioid withdrawal symptoms and no change in the dose of opioid was required to treat pain during the study [33]. The peripheral action of naloxegol was evident by not causing opioid withdrawal or worsening of pain. The recommended dosage of naloxegol is 25 mg once daily in the morning, on an empty stomach. The proportion of responders in both trials was significantly higher in the naldemedine treated group. There was no difference in the reported adverse events between the treatment and placebo groups in both trials. Naldemedine was not associated with signs or symptoms of opioid withdrawal and no impact on opioid mediated analgesia. The improvement in bowel movement frequency, overall constipation-related symptoms and quality of life were observed with naldemedine more often than placebo (all P 0. Naldemedine was well tolerated for 52 weeks and did not interfere with opioid-mediated analgesia or precipitated opioid withdrawal. Lubiprostone (Amitiza, Takeda) Lubiprostone is a bicyclic fatty acid derived from prostaglandin E1. It increases fluid secretion in the gastrointestinal tract by stimulating the cystic fibrosis transmembrane regulator and type 2 chloride channels in the apical membrane to secrete chloride and water in the lumen. There is evidence that lubiprostone may reverse morphine induced anti-secretory effect through its direct action on mucosal chloride channels [37]. It has been suggested that increase in peristalsis and acceleration of small bowel and colon transit by lubiprostone is due to increase in water secretion in the lumen. However, in mice, lubiprostone caused an increase in contractility of circular but not longitudinal small intestinal smooth muscles. A prospective, multicenter, double-blind placebo-controlled trial enrolled 418 patients to lubiprostone 24 g or placebo twice daily for 12 weeks [40]. Similarly, improvement in constipation symptoms and severity showed greater improvement in the lubiprostone than placebo group. In this study 431 patients were randomized to lubiprostone 24 g or placebo twice daily for 12 weeks. Prucalopride is approved for the treatment of chronic idiopathic constipation in the United States. Prucalopride is also approved in Europe for the treatment of idiopathic constipation in women. The patients were randomized to prucalopride 2 mg, or 4 mg, or placebo for 4-weeks. Over the 4 weeks of treatment, improvement were seen in other efficacy parameter with 2 and 4 mg dose compared to placebo, although not always reaching statistical significance. When naloxone is used orally, it acts locally on -opioid receptors in the gastrointestinal tract [44]. Naloxone displaces oxycodone from the mu receptors due to high affinity of naloxone to opioid receptors. When the combination of oxycodone and naloxone was 2:1, the efficacy to relive constipation was greater and side effects fewer compared to other ratios [46]. Guidelines for the management of opioid-induced constipation Treatment of opioid induced constipation is challenging; most patients are not satisfied with their commonly used laxatives [47]. Prior to initiating opioids, a careful history should be obtained to assess comorbid illnesses including hypothyroidism or hypercalcemia and medication use. Many patients with opioid-induced constipation have underlying risk factors for constipation. Opioids also have a sedating effect resulting in decreased physical activity and poor response to the urge to defecate. It is imperative to determine if patients already experience constipation and are taking laxatives. It may also be of benefit to switch to less constipating opioids, such as the transdermal fentanyl patch. Lifestyle changes are an important first step in management of constipation due to any cause. This includes adequate fiber and fluid intake, regular moderate exercise as tolerated, bowel conditioning and responding to urge as soon as possible. Caution should be exercised as excessive fiber causes bloating/gas and should be avoided. Stimulant laxatives may be preferred to osmotic laxatives; a combination of stimulant and osmotic laxatives usually performs better than either class alone. Second-line therapies, after laxatives fail, include naldemedine, naloxegol, methylnaltrexone, or lubiprostone. The differences in response rate among these drugs may be due to differences in endpoints used in clinical trials. Characteristically, these patients will have significant improvement of their abdominal pain when opioids are withdrawn. Eating can aggravate the symptoms, so weight loss can occur due to anorexia or avoiding food to aggravate pain. Since than there have been other case reports with a more detailed description of this disorder [52]. Pathophysiology Opioid-induced bowel disorders are predominantly due to the actions of opioids on the peripheral -receptors. It is thought that hyperalgesia is due to glial cell activation in the dorsal horn of the spinal cord resulting in release of pain neurotransmitters from sensory nerves.
However muscle relaxant effects pyridostigmine 60mg for sale, it is unique in that it provides a conduit for both the passage of air and the transport of liquids and food boluses muscle relaxant non-prescription buy discount pyridostigmine 60 mg on line. The pharyngeal phase of deglutition refers to transport of the food bolus through the pharynx to the esophagus whilst the respiratory function of the pharynx stops. As the bolus enters the oropharynx it crosses the anterior facial pillars, a contact which initiates the involuntary trigger of the pharyngeal phase. Unlike other reflexes, this pharyngeal swallow response can be modulated by how the bolus is transported before it reaches the oropharynx, a phenomenon which is termed the leading complex. Bolus properties such texture, taste and volume can delay or initiate an earlier response. Once the pharyngeal phase is triggered, respiration ceases, which is achieved by adduction of the true vocal cords by contracture of the laryngeal muscles. This pharyngeal peristaltic wave squeezes the bolus through the pharynx into the upper esophagus. The pharynx elevates and the suprahyoid muscles contract, causing the hyoid bone to move anteriorly and superiorly. The thyrohyoid muscle simultaneously contracts which moves the larynx superiorly towards the hyoid bone. These movements direct the larynx under the tongue base and invert the epiglottis, moving the bolus away from the laryngeal inlet. The laryngeal and hypopharyngeal elevation cause a negative pressure below the bolus which helps to suck it down into the esophagus. After the food bolus enters the esophagus, the cricopharyngeal muscle returns to its contracted state and seals off the esophagus, thereby preventing any retrograde reflux of the bolus into the hypopharynx. Esophageal peristalsis is activated and the bolus is propelled towards the stomach. Oropharyngeal dysphagia Swallowing is defined by the World Health Organization as the function of clearing food and drink through the oral cavity, pharynx and esophagus into the stomach at the appropriate rate and speed [2]. Dysphagia refers to a difficulty in swallowing, and can be either esophageal or oropharyngeal in origin. Oropharyngeal dysphagia is a condition where there is perceived or actual difficulty in forming or moving a food bolus safely from the oral cavity to the esophagus [3]. The main symptoms include coughing, repetitive throat clearing, hoarse voice, residual food in the oropharynx, choking (mechanical obstruction causing impaired pulmonary air flow) and aspiration (the entry of food, liquid or secretions into the trachea and lungs). Clinically, oropharyngeal dysphagia may give rise to several groups of clinically relevant complications [4]: (1) Protein-calorie malnutrition and dehydration due to decreased oral intake secondary to a decrease in deglutition efficacy (2) Tracheobronchial aspiration, which can manifest as a pneumonia in up to 50% of patients with significant mortality and morbidity [5]. Oropharyngeal dysphagia should be differentiated from functional disorders such as globus pharyngeus, a disorder where patient feels a continuous sensation of having a lump in the throat, an obstruction or phlegm [2]. Although oropharyngeal dysphagia is associated with greater morbidity and mortality than esophageal dysphagia, it is less often diagnosed and treated. Deglutition and oropharyngeal dysphagia Chapter 11 169 Elderly the natural aging process causes changes in head and neck anatomy as well as changes in muscular and neural mechanisms, resulting in a loss of functional swallowing reserve which may affect the swallowing process. In healthy older patients, these changes are termed presbyphagia and are not necessarily considered pathological if the safety of the swallow is not compromised [7]. Anatomical differences in elderly patients include a smaller cross-sectional area of the masseter and medial pterygoid muscles used in mastication, lingual atrophy and decreased muscle fiber diameter. There is age-related decline in the mobility, strength and endurance of the lips and tongue. In addition, there is decreased sensory perception of oral spatial tactile recognition, diminished perception of viscosity and taste perception [7]. The distinction between what is considered a normal deglutition in the elderly and oropharyngeal dysphagia can be difficult to establish. When these changes coincide with elderly, frail, overmedicated patients with multiple comorbidities, the risk or oropharyngeal dysphagia and its sequelae increase significantly. In addition, the prevalence of oropharyngeal dysphagia differs whether patients are hospitalized, institutionalized or live independently. Hence, one study reported a 27% prevalence of oropharyngeal dysphagia in a cohort of 254 elderly patients >70 years old living in the community [8]. Another study evaluating 1662 patients >70 years old admitted to an acute geriatric unit showed a prevalence of 47. Patients institutionalized in long term facilities had a higher prevalence, with one study showing a prevalence of 51% in nursing home residents [10], increasing up to 90% in elderly patients acutely hospitalized with pneumonia [11]. Neurological and degenerative diseases According to the American Stroke Association, stroke is the leading neurological cause of dysphagia or difficulty in swallowing. Oropharyngeal dysphagia is more prevalent in brainstem stroke, followed by bilateral hemispheric stroke. Although the pathophysiology is poorly understood, both dopaminergic and non-dopaminergic mechanisms are implicated. Head and neck cancer Neoplasms of the head and neck can cause dysphagia secondary to mass effect, altered anatomy and treatments such as surgery, chemotherapy and radiation. The majority of patients are treated with chemoradiation, and over 40% develop oropharyngeal dysphagia. Chemoradiation in head and neck cancers has been found to cause reduced range of lingual motion and strength, impaired bolus formation and transport, prolonged transit times and increased oral residue, as well as a variety of pharyngeal phase deficits such as delayed triggering of the pharyngeal swallow, reduced hyoid and laryngeal motion, and reduced opening of the upper esophageal sphincter [19]. Chemoradiation in head and neck cancers impact lymphatic function, putting patients at risk for developing lymphedema. Efforts at organ preserving surgeries do not always translate into preserved swallowing function due to late stage fibrosis [21]. The highest rates of dysphagia are in patients who have had both surgery and chemoradiation [22]. Other structural causes Oropharyngeal dysphagia may be caused by structural alterations that impair or prevent oropharyngeal reconfiguration during deglutition, or impair bolus transit to the esophagus. Cervical osteophytes are a common incidental finding occurring between 6% and 30% of elderly patients, although only 0. However, if prominent enough, cervical osteophytes can cause dysphagia by compressing the posterior pharyngeal wall, but para-esophageal inflammation from continued motion over the vertebrae can contribute as well. There are also a variety of medications that can contribute to dysphagia and are frequently used by older patients. Anticholinergics work by blocking the neurotransmitter acetylcholine and are used to treat a variety of conditions of the gastrointestinal tract and urinary tract, motion sickness, and more. This effect can cause decreased mucous and saliva production in the nose, mouth and throat, causing a dry mouth that can cause oropharyngeal dysphagia. Pathophysiology As outlined above, deglutition occurs in three sequential phases, and impairment of any phase can cause oropharyngeal dysphagia. Dehydration, malnutrition, respiratory infections and aspiration pneumonia are the most common complications in patients with oropharyngeal dysphagia and lead to frailty and an increase in readmissions and mortality. In addition, there is a weak bolus propulsion force and impaired supra-hyoid traction thought mainly to be secondary to loss of muscle tissue (sarcopenia), ultimately resulting in a fractional swallow and oropharyngeal food residue [28]. In oropharyngeal dysphagia after stroke, symptoms are a result of damage to somatic motor nuclei in the brainstem, damage to the central pattern generator, or damage to the dominant pharyngeal cortex [29]. The goal is to accurately identify patients with dysphagia, identify specific etiologies that may be amenable to medical or surgical therapies, characterize biomechanical changes causing in oropharyngeal dysphagia and design a set of therapeutic strategies to facilitate safe and effective deglutition. The diagnosis is best achieved with a thorough knowledge of the etiology and clinical manifestations of dysphagia, and ability to perform clinical screening. Odynophagia suggests a pharyngeal or esophageal inflammatory condition or an esophageal motor disorder. Dysphagia for liquids, need for multiple swallows of a small bolus, and repeated respiratory infections suggests neurogenic dysphagia, while dysphagia to solids suggests more of an obstructive difficulty. The presence of coughing or choking suggest aspiration although up to 40% of patients may have silent aspiration. Screening the aim of screening is to identify patients who are at risk of oropharyngeal dysphagia. These patients should be referred for swallowing assessment and therapeutic interventions to prevent complications such as aspiration. Clinical assessment There are a variety of clinical tools that can be used to evaluate the safety and efficacy of swallowing, as well as to detect aspiration at the bedside. The general principle behind all of them involves asking patients to swallow various amounts and consistencies of liquids, in an attempt to identify an abnormal swallow reflex by the presence of coughing, a slow swallow or the presence of a wet or hoarse voice. Traditional bedside tests involve the swallowing of various amounts of water and assessment for abnormal swallowing, such as coughing, presence of a slow swallow or a change in voice quality.
However spasms left side under rib cage purchase pyridostigmine with mastercard, all implement pH-impedance monitoring and correlate symptoms with reflux events muscle relaxant for headache purchase pyridostigmine toronto. The defined population of patients affected by functional heartburn will continue to change as novel diagnostic techniques are developed. This has already begun to occur with the coordination of pH-impedance monitoring, high resolution esophageal manometry and better statistical tools for quantifying the relationship between reflux events and symptoms. Pathophysiology Functional heartburn patients experience symptoms unrelated to esophageal acid exposure. Current evidence suggests that there is an interplay of several different mechanisms leading to symptom generation including esophageal hypersensitivity, abnormal central processing of esophageal stimuli and psychiatric comorbidities. Esophageal hypersensitivity Although symptoms of functional heartburn are not temporally associated with reflux events, a growing body of literature suggests that symptoms arise from visceral hypersensitivity of esophageal nociceptors [44]. Numerous studies utilizing electrical stimulation and balloon distension have consistently demonstrated lower thresholds for pain perception in functional heartburn patients [44]. However, perceptual responses to esophageal perfusion of acid has yielded mixed results. They found that 89% of patients perceived acid perfusion as painful while only 52% perceived intra-esophageal balloon distension as painful [45]. Of note, the study did not differentiate functional heartburn from reflux hypersensitivity as at the time of the study they were not considered separate entities. They hypothesized that the etiology of increased sensitization is likely multifactorial, resulting from increased sensitization of acid chemoreceptors and altered mucosal permeability allowing esophageal contents to penetrate the deeper layers of esophageal mucosa [47]. Whether or not functional heartburn patients are sensitive to esophageal acid exposure remains controversial. Further evidence that acid exposure does not play a role in symptom generation is supported by two key studies. Lower esophageal sphincter pressure, esophageal acid exposure, and prevalence of hiatal hernia did not differ between the two groups, suggesting that a mechanism other than acid reflux must be driving symptoms [50]. In summary, esophageal hypersensitivity is thought to have an important role in functional heartburn symptoms. However, while most studies have demonstrated mechanoreceptor sensitivity to balloon distension, chemoreceptor sensitivity to acid perfusion has remained controversial with conflicting results among several studies. It may be that the current definition of functional heartburn includes a heterogeneous group of patients, some with chemoreceptor sensitivity and others without. Visceral neuron dysfunction Visceral neuron dysfunction and altered central processing of pain may contribute to the pathophysiology of functional heartburn. Functional heartburn patients demonstrated shorter cortical evoked potential latencies for esophageal distension and both shorter latencies and greater amplitudes for acid perfusion when compared to the healthy controls [51]. In functional heartburn patients, the diameter of intercellular spaces appears to be the same as normal controls. This is supported by measurements of baseline impedance (a measure of mucosal permeability), which appear to be the same between functional heartburn patients and healthy controls [52]. Another interesting study utilizing 24-h pH-impedance testing assessed the role of different types of refluxate on symptom perception. Disordered esophageal motility A study of 40 functional heartburn patients demonstrated that 66% of participants had non-specific abnormal esophageal manometry testing manifested as weak or failed peristalsis. For now, in the assessment of functional heartburn, manometry is used to rule-out major esophageal motility disorders that can lead to refractory heartburn symptoms. Psychiatric comorbidities Psychiatric comorbidities are a common finding in patients with functional esophageal disorders. Whether these comorbidities are a cause of functional heartburn, a consequence of or merely epiphenomena remains to be elucidated. Functional heartburn patients were noted to have higher levels of anxiety and hysteria, and social support structures were also noted to be significantly lower [56]. Patients with functional heartburn were also noted to have traits similar to other functional bowel disorders such as increased somatization, chest pain and altered autonomic function [48]. Psychological factors are unlikely to be the primary etiology of functional heartburn symptoms. However, they undoubtedly exacerbate symptoms, drive patients to seek medical attention and are an important target of therapy for improving symptoms and quality of life. Up to 66% of functional heartburn patients complain of other symptoms, including belching, bloating and dyspepsia, and patients tend to be younger and female [44]. As previously described, patients may also possess features similar to other functional bowel disorders, such as increased somatization, chest pain and altered autonomic function [48]. Psychiatric comorbidities are common in functional heartburn including anxiety, stress and depression [48]. Quality of life scores in functional heartburn patients are low, and patients may complain of difficulty eating and sleeping, fatigue and anxiety [44]. The role of biopsies during upper endoscopy is primarily to rule out eosinophilic esophagitis [44]. For example, the absence of dilated intercellular spaces may suggest functional heartburn [57]. Another method relies on a histologic sum score based on features suggestive of esophageal acid exposure such as dilated intercellular spaces, inflammation and basal cell hyperplasia [58]. The next step in diagnosis is ambulatory reflux monitoring which serves two purposes. First, to identify if the patient has abnormal esophageal acid exposure; and second, to identify a temporal relationship between reflux events and symptoms. Patients with normal acid exposure have either functional heartburn or reflux hypersensitivity based on the correlation between reflux events and symptom onset. This is accomplished by dividing the number of reflux-associated symptoms events by the total number of symptom events multiplied by 100%. If symptoms are not correlated with reflux symptoms, this suggests functional heartburn. Of note, the study did not address pH-impedance monitoring which has the added benefit of observing reflux events as liquid movement and not just pH changes [59]. The final step in diagnosis is esophageal manometry to exclude a major motility disorder presenting as refractory reflux. It can be performed during upper endoscopy and reflects the integrity of the esophageal mucosa. In functional heartburn, the diameter of intercellular spaces appears to be the same as normal controls [61]. Other endoscopic tools under investigation include high-magnification endoscopy, narrow-band imaging and autofluorescence imaging endoscopy, however their applicability remains uncertain and requires further research. Treatment Functional heartburn is treated similarly to functional chest pain using neuromodulators, complementary behavioral treatments and alternative therapies [1]. There is some evidence for acid suppression therapy, however it remains controversial [38]. Functional esophageal chest pain Chapter 17 255 Promotility agents Most studies evaluating the efficacy of prokinetics exclude functional heartburn patients as there is no clear mechanistic association between functional heartburn and dysmotility [44]. However, tegaserod was withdrawn from the United States market due to an increased rate of adverse cardiovascular events, but has just become available once again. Neuromodulators the role of neuromodulators in treating functional heartburn has not been extensively evaluated. A small randomized placebo-controlled trial evaluating the use of fixed dose imipramine in functional heartburn and reflux hypersensitivity patients, failed to demonstrate an improvement in heartburn symptoms. However, it did show a benefit in quality of life scores which suggests a potential role for patients with psychiatric comorbidities [64]. Histamine 2 receptor antagonists, typically used for acid suppression, have been shown to improve symptoms in functional heartburn patients potentially via an alternative pathway. A small randomized placebo-controlled, double-blind crossover study of 18 functional heartburn patients demonstrated increased esophageal pain threshold with ranitidine treatment when compared to placebo [65]. The mechanism of action is thought to be related to neuromodulation of esophageal visceral sensation. Use of these newer neuromodulators remains experimental with studies demonstrating their clinical applicability currently underway. Complementary and alternative medicines Functional heartburn patients often pursue complementary and alternative therapies as pharmacologic options are limited [44]. An open-label, controlled trial of nine functional heartburn patients evaluated the efficacy of esophageal-directed hypnotherapy on heartburn symptoms [67]. After completing seven sessions of weekly hypnotherapy, patients had a demonstrable improvement in visceral anxiety (P=0.
Demographic and clinical characteristics associated with glomerular filtration rates in living kidney donors spasms left abdomen cheap pyridostigmine american express. Glomerular filtration rate in healthy living potential kidney donors: a meta-analysis supporting the construction of the full age spectrum equation muscle relaxant for alcoholism purchase pyridostigmine 60 mg with visa. Age-dependent reference intervals for estimated and measured glomerular filtration rate. The reference change value: a proposal to interpret laboratory reports in serial testing based on biological variation. The effect of exercise on the renal plasma flow and filtration rate of normal and cardiac subjects. Selection of routine method for determination of glomerular filtration rate in adult patients. Contrast media as markers for glomerular filtration: a pharmacokinetic comparison of four agents. The clinician and estimation of glomerular filtration rate by creatininebased formulas: current limitations and quo vadis. A simple technique for estimating glomerular filtration rate with subcutaneous injection of (125I)lothalamate. Plasma clearance of nonradioactive iohexol as a measure of glomerular filtration rate. Iohexol plasma clearance in determining glomerular filtration rate in diabetic patients. Iohexol plasma clearance for measuring glomerular filtration rate in clinical practice and research: a review. Luis-Lima S, Gaspari F, Negrin-Mena N, Carrara F, Diaz-Martin L, Jimenez-Sosa A, Gonzalez-Rinne F, Torres A, Porrini E. Glomerular filtration rate estimated by cystatin C among different clinical presentations. Evaluation of sample bias for measuring plasma iohexol clearance in kidney transplantation. Definition of chronic kidney disease after uninephrectomy in living donors: what are the implications Specificity characteristics of 7 commercial creatinine measurement procedures by enzymatic and Jaffe method principles. Measurement of muscle mass in humans: validity of the 24-hour urinary creatinine method. For estimating creatinine clearance measuring muscle mass gives better results than those based on demographics. A proposed mechanism for reduced creatinine excretion in severe chronic renal failure. The influence of a cooked meat meal on creatinine plasma concentration and creatinine clearance. Creatinine clearance during cimetidine administration for measurement of glomerular filtration rate. Isolation, physiological importance, inhibitory mechanism, gene structure and relation to hereditary cerebral hemorrhage. Relationships among serum cystatin C, serum creatinine, lean tissue mass and glomerular filtration rate in healthy adults. Potential contribution of adipose tissue to elevated serum cystatin C in human obesity. Factors influencing serum cystatin C levels other than renal function and the impact on renal function measurement. Effect of clinical variables and immunosuppression on serum cystatin C and beta-trace protein in kidney transplant recipients. The impact of interlaboratory differences in cystatin C assay measurement on glomerular filtration rate estimation. Filtration markers may have prognostic value independent of glomerular filtration rate. Molecular characterization of beta-trace protein in human serum and urine: a potential diagnostic marker for renal diseases. Beta-trace protein is an alternative marker for glomerular filtration rate in renal transplantation patients. Method of glomerular filtration rate estimation affects prediction of mortality risk. Beta-trace protein in serum: a new marker of glomerular filtration rate in the creatinine-blind range. Factors other than the glomerular filtration rate that determine the serum beta-2-microglobulin level. Inter-laboratory discordance of beta-2 microglobulin results: impact on the validity of the international staging system for multiple myeloma. Beta2-microglobulin for risk stratification of total mortality in the elderly population: comparison with cystatin C and C-reactive protein. A metabolome-wide association study of kidney function and disease in the general population. Metabolomic profiling to improve glomerular filtration rate estimation: a proof-of-concept study. Optimally predicting mortality with kidney function markers is not the same as optimally determining how kidney function predicts mortality. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Predictive performance of the modification of diet in renal disease and Cockcroft-Gault equations for estimating renal function. A systematic comparison of cockcroft-gault and modification of diet in renal disease equations for classification of kidney dysfunction and dosage adjustment. Serum cystatin C predicts vancomycin trough levels better than serum creatinine in hospitalized patients: a cohort study. Cystatin C-guided vancomycin dosing in critically ill patients: a quality improvement project. Estimating glomerular filtration rate for the full age spectrum from serum creatinine and cystatin C. Generation of a new cystatin C-based estimating equation for glomerular filtration rate by use of 7 assays standardized to the international calibrator. Cathepsins (S and B) and their inhibitor Cystatin C in immune cells: modulation by interferon-beta and role played in cell migration. Estimating the glomerular filtration rate from serum creatinine is better than from cystatin C for evaluating risk factors associated with chronic kidney disease. Performance of glomerular filtration rate estimation equations in Congolese healthy adults: the inopportunity of the ethnic correction. Evaluation of the Chronic Kidney Disease Epidemiology Collaboration equation for estimating the glomerular filtration rate in multiple ethnicities. Estimation of renal function in subjects with normal serum creatinine levels: influence of age and body mass index. Cystatin C or creatinine for detection of stage 3 chronic kidney disease in anorexia nervosa. Assessment of changes in kidney allograft function using creatinine-based estimates of glomerular filtration rate. Comparison of methods for determining renal function decline in early autosomal dominant polycystic kidney disease: the consortium of radiologic imaging studies of polycystic kidney disease cohort. A comparison of change in measured and estimated glomerular filtration rate in patients with nondiabetic kidney disease. Assessment of glomerular filtration rate in the neonate: is creatinine the best tool Beta-trace protein is not better than cystatin C as an indicator of reduced glomerular filtration rate. Beta trace protein does not outperform creatinine and cystatin C in estimating glomerular filtration rate in older adults. Combining cystatin C and creatinine yields a reliable glomerular filtration rate estimation in older adults in contrast to beta-trace protein and beta2-microglobulin.
Effective 60mg pyridostigmine. Top 3 Ways to Treat Trigger Finger or a Snapping Finger or Thumb..
References
- Wen JG, Yang L, Xing L, et al: A study on voiding pattern of newborns with hypoxic ischemic encephalopathy, Urology 80(1):196n199, 2012.
- Bazarbachi A, Plumelle Y, Carlos Ramos J, et al. Meta-analysis on the use of zidovudine and interferon-alfa in adult T-cell leukemia/lymphoma showing improved survival in the leukemic subtypes. J Clin Oncol 2010;28(27):4177-4183.
- Sea J, Jonat LM, Chew BH, et al: Optimal power settings for Holmium:YAG lithotripsy, J Urol 187(3):914-919, 2012.
- Piros L, Fehervari I, Gorog D, et al. Examinations of factors influencing survival of liver transplantation for hepatocellular carcinoma: a single-center experience from Budapest. Transplant Proc 2015;47(7):2201-2206.