Carolyn Sears Avery, MD
- Assistant Professor of Pediatrics
- Assistant Professor in Medicine

https://medicine.duke.edu/faculty/carolyn-sears-avery-md
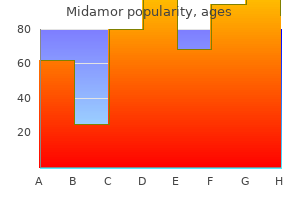
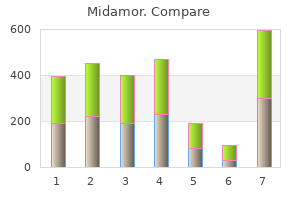
It can cause pharyngitis and skin and soft tissue infections such as cellulitis blood pressure chart app generic 45mg midamor with mastercard, impetigo arteria zigomatico orbital cheap midamor 45 mg online, myositis, necrotizing fasciitis, and streptococcal toxic shock syndrome. The Immune System and Infection M proteins, encoded by the emm gene, inhibit the binding of antibodies and opsonin and can protect the organism from phagocytosis by neutrophils. Group A streptococcus cytolysins include (1) streptolysin O, which creates cholesterol aggregates that facilitate cell lysis; (2) hyaluronidase, which hydrolyzes hyaluronic acid in deep tissues; (3) streptokinase, which converts plasminogen to plasmin and may contribute to the development of poststreptococcal glomerulonephritis; (4) nicotinamide-adenine dinucleotidase; and (5) deoxyribonucleases A, B, C, and D. Group A streptococcus exotoxins act as super antigens and can contribute to invasive disease and toxic shock syndrome. Acute pharyngitis can be treated with oral penicillin 2 to 4 times per day for 10 days; penicillin is the recommended first-line therapy, but other antibiotic options include a macrolide, such as azithromycin, or cephalosporin, such cefuroxime or cefpodoxime, for 5 days. Clinical presentation can range from hematuria to acute nephritic syndrome (edema, hypertension, acute kidney injury with red to brown urine, and proteinuria). Haemophilus influenzae this pleomorphic Gram-negative rod is a nonmotile facultative anaerobe that resides in the human respiratory tract. It has 6 serotypes (A through F) that are associated with an outer capsule and a nontypeable serotype that is not associated with a capsule. The currently available H influenza type B conjugate vaccine is active against the most common serotype B and induces bactericidal antibodies to capsular polysaccharides. The widespread use of the vaccine has reduced the incidence of invasive disease due to H influenza serotype B, but it has been suggested to have increased the incidence of infections due to nontypeable serotype. Amoxicillin or an oral second- or thirdgeneration cephalosporin can be used for pneumonia and less severe infections. N meningitides presents with meningitis, meningitis with accompanying meningococcemia, or meningococcemia without meningitis. Patients may have a petechial rash that evolves into a purpuric rash, predominantly on the trunk and lower extremities. Cerebrospinal fluid studies for meningococcal meningitis typically show a high white blood cell count, a high protein level, and a low glucose level. Third-generation cephalosporins such as ceftriaxone or cefotaxime should be used for treatment. Chemoprophylaxis should be given to close contacts, such as household contacts and healthcare workers exposed to oral secretions, within 24 hours of exposure. Because S aureus forms biofilms on medical devices, removal of infected devices such as central lines and cardiac devices is crucial for clearance of infection. It has virulence factors, including the formation of biofilm, which is in part secondary to a mucoid phenotype; exotoxins A, S, and U; endotoxin lipopolysaccharides; elastase; alkaline protease; and phenazines. Severe infections can be complicated by ecthyma gangrenosum, which are ulcerative lesions with violaceous margins, penetrating the dermis. Although combination therapy with double coverage has previously been recommended, this is now reserved as empiric therapy for patients with serious infections and suspicion of Pseudomonas infections with possible drug resistance. Once susceptibility data is available, antibiotic therapy should be tailored appropriately. Antibiotics with good antipseudomonal activity include antipseudomonal -lactams with -lactamases (such as piperacillin/tazobactam and ticarcillin/ clavulanate), antipseudomonal cephalosporins (ceftazidime and cefepime), aztreonam, fluoroquinolones, and carbapenems (with the exception of ertapenem, which does not cover Pseudomonas). Aminoglycosides have antipseudomonal activity but are not generally recommended for monotherapy. Listeria Listeria monocytogenes is an aerobic and facultatively anaerobic Gram-positive rod with "tumbling motility" that can cause febrile gastroenteritis, meningoencephalitis, cerebritis, rhombencephalitis, pneumonia, skin infections, eye infections, septic joints, biliary tract infections, and cholangitis. The bacteria are ingested and travel to the bloodstream and into the liver and spleen. Staphylococcus this genus of Gram-positive cocci colonize the skin and upper respiratory tract and include the group known as coagulasenegative Staphylococcus, including S epidermidis, and S aureus, which is coagulase positive. Although coagulase-negative Staphylococcus is often a blood culture contaminant, it can cause bloodstream infections, particularly in the setting of catheters, endocarditis, and prosthetic joint infections. Its virulence is related to its ability to inhibit phagosome-lysosome fusion via defective organelle trafficking (dot) genes and intracellular multiplication (icm) genes. The urine antigen test is only for Legionella serogroup 1, but this serogroup causes the majority of infections. Corynebacterium Corynebacterium is a genus of Gram-positive bacilli that are catalase positive, urease negative, cystinase positive, and pyrazinamidase negative. Symptoms of malaise, sore throat, lymphadenopathy, and low-grade fever usually starts 2 to 5 days after infection. Dissemination of the diphtheria toxin can lead to systemic disease with involvement of the heart, nervous system, and kidneys. Nocardia Nocardia is a genus of filamentous, branching Gram-positive rods that can partially stain acid fast. Antibiotics with activity against Nocardia include amikacin, imipenem, meropenem, ceftriaxone, cefotaxime, minocycline, moxifloxacin, levofloxacin, linezolid, and tigecycline, but resistance to these agents is variable. Complications of B henselae infection include neuroretinitis, peliosis hepatis, Parinaud oculoglandular syndrome, osteomyelitis, encephalitis, or endocarditis. B quintana is spread through lice and can cause trench fever with cyclical fevers that classically recur every 5 days, severe headache, bone pain, splenomegaly, and sometimes rash. For Bartonella endocarditis, treatment is doxycycline plus rifampin for 6 to 8 weeks. Rhodococcus most commonly causes cavitary pneumonia with or without pleural effusions in the immunocompromised, Brucella Brucella is a small, nonmotile, aerobic, intracellular Gramnegative coccobacilli that lacks a capsule, spores, and flagella. Brucella has a smooth lipopolysaccharide and proteins that are involved in cell entry and likely help evade the immune response. Symptoms include fevers, night sweats, anorexia, weight loss, malaise, and arthralgias; complicated infections can lead to neurobrucellosis, endocarditis, and hepatic abscess. Brucella is associated with complications in pregnancy, including spontaneous abortion, premature delivery, and fetal death. Because of the risk of laboratory infection, the microbiology lab must be notified in advance if there is suspicion of brucellosis. Treatment is with the combination of either doxycycline and rifampin or doxycycline and streptomycin. Symptoms of typhoid fever usually occur several days to weeks after ingestion of the bacteria and include high fevers, often with relative bradycardia, abdominal pain, and salmon-colored macules known as "rose spots. Diagnosis is by culture, with bone marrow cultures being the most sensitive; serologic tests such as the Widal test are of limited use in endemic areas as they may represent previous infection. Patients can be chronic carriers of S typhi, shedding the bacteria in the urine and stool for more than 12 months after acute infection. Capnocytophaga canimorsus Capnocytophaga is a facultative anaerobe and a long, slender Gram-negative rod found in the oral flora of dogs or cats. It can cause severe sepsis after a dog bite in immunocompromised patients, most often due to splenic abnormalities such as asplenia or splenectomy, cirrhosis, or alcohol abuse. Treatment is with -lactams such as a -lactam/-lactamase combination, a cephalosporin, or a carbapenem, and duration is determined by clinical response. They appear as Gram-positive cocci in pairs and chains and are facultative anaerobes. The most common species that cause infection are E faecalis and E faecium, both of which reside in the human intestine. Enterococcus faecalis is usually susceptible to ampicillin, which is the antibiotic of choice, but E faecium is usually resistant to ampicillin and is often resistant to vancomycin. Quinupristin-dalfopristin is the only active antibiotic against E faecium and is not active against E faecalis. Clinically, syphilis can be divided into early infection (less than 1 year), which includes primary syphilis, secondary syphilis, and latent syphilis, or late infection. Secondary syphilis occurs weeks to months after the primary lesions with a diffuse maculopapular rash involving the soles and palms, constitutional symptoms, and lymphadenopathy. Escherichia coli is a facultative anaerobe the Immune System and Infection or nephrotic syndrome, and ocular disease. Early latent syphilis is when serologic tests are newly positive within the past 12 months, while late latent syphilis has positive testing either after 12 months or of unknown timing. Late syphilis can present up to 30 years from initial inoculation and consists of tertiary syphilis with gummatous syphilis, general paresis, tabes dorsalis, and cardiovascular syphilis. Doxycycline or ceftriaxone can be used in patients who are allergic to penicillin, but there is limited data on efficacy and higher rates of failure in neurosyphilis. Mycobacterium tuberculosis is the most clinically significant species, as the cause of tuberculosis, which causes significant infectious mortality worldwide.
When involvement is diffuse young squage heart attack cheap midamor 45mg visa, fasciotomy incisions on the extremities are often a useful starting place arteria angularis midamor 45 mg otc. Lack of resistance to this probing is the hallmark of the diagnosis in early cases. Cultures and stat Gram stain for aerobic and anaerobic cultures should be obtained. If the patient is immunosuppressed, cultures for Mycobacterium and fungus should also be sent. A colostomy may be helpful in cases with extensive perianal involvement to prevent ongoing stool contamination. Surgical feeding tube placement should be considered in critically ill patients or in patients with large surface area wounds that are likely to remain open for some time. Plans should be made at the end of the case for return to the operating room for reevaluation of the wounds within 48 hours. Adequate evaluation of these deep and often painful wounds is not possible at the bedside. It prevents maceration of the surrounding tissue and keeps the patient and the bed linens dry. The skin surrounding the wound can be evaluated for advancing cellulitis or edema. It is imperative if this type of wound care is to be used that hemostasis is meticulous and coagulopathy corrected. Parameters must be given to the nursing staff regarding volume and character of the fluid loss that is acceptable. Although some of these materials may be cytotoxic, the antimicrobial properties may outweigh the negative effect of the cytotoxicity on normal tissues. Broad-spectrum antibiotic therapy is initiated to cover the most likely causative organisms (Table 14). Methicillin resistance is emerging in the community, and this must be considered in choosing antibiotics. Vancomycin or daptomycin should be considered when resistance is suspected or in cases in which the patient is severely compromised. Patients with penicillin allergies can be treated with fluoroquinolones in combination with gramnegative and anaerobic therapy or carbapenems. When available, given the relatively high mortality and morbidity rates, use of this modality as an adjunct makes sense. Note the area of discoloration and blistering at the elbow with tense edema and erythema. Most of the morbidity results from the tissue destruction brought about by the infection. Tissues may be distorted by the inflammation and necrosis or scarred by prior surgery, making the identification of vital structures a challenge. Amputation rates from 17% to 33% have been documented in patients with extremity severe soft tissue infections. Management of the output of the fistula and providing for adequate nutrition are the treatment goals in the early management of this problem. Mortality rates as high as 76% have been recorded, although contemporary studies report overall mortality rates in the range of 8% to 25%. Clinical presentation and speed to surgery appear to be the two most important determinants. Patients who suffer delays in obtaining surgical treatment had higher mortality rates. Patients who present with organ failure or increased serum lactate also have higher mortality rates. This demonstrates the necrosis of the superficial fascia and fat found extending from the elbow. It must be stressed that resuscitation is begun, but all abnormalities will not and need not be fully corrected before proceeding to surgery. Resuscitation must continue throughout the preoperative, operative, and postoperative phases. It should be considered in postsurgical, posttraumatic wounds as well as in wounds from insect or animal bites. Differentiation from superficial infection is mandatory to assure appropriate surgical therapy is performed. Patients who fail to respond to appropriate medical therapy or who present with evidence of shock or organ dysfunction often harbor deeper infections. Progression of physical findings, including worsening edema, blistering, and crepitans or skin necrosis, mandates surgical exploration. A recent Institute of Medicine report estimated that 44,000 to 98,000 deaths each year were caused by medical errors. Obviously, trauma care is a much more difficult setting to perform in an errorless fashion. In many instances, interventions must be initiated before a complete clinical and radiographic evaluation is performed. Frequently, the history of the mechanism of injury is obscure, or injured patients involved in socially unacceptable or criminal activities may mislead the trauma team. Moreover, injured patients are frequently unresponsive, have a decreased level of consciousness, or are uncooperative due to intoxication. Seriously injured patients frequently present with multiple injuries that require the involvement of multiple providers. Routinely, numerous surgeons, surgical subspecialists, emergency medicine physicians, and residents must accurately communicate and coordinate care for an optimal outcome. Residents as members of the trauma team add complexity to communication, organization, and supervision. Because of these many difficulties, the surgeon who cares for trauma patients must pay particular attention to factors that cause errors in management and should make every effort to prevent these errors. In this article, a number of common errors in the management of injured patients are discussed. E pressure generated during inspiration contributes to herniation of intraabdominal organs into the thoracic cavity. There is a strong association between thoracic aortic transection and diaphragmatic rupture in deceleration injuries with up to 10% of patients with aortic injuries also having a diaphragmatic injury. Other associated injuries include liver and splenic lacerations, long-bone fractures, and traumatic brain injury. Penetrating thoracoabdominal injuries also often result in diaphragmatic injuries. Because these injuries are typically much smaller than blunt ruptures, the diagnosis may be unrecognized even if appropriate diagnostic modalities are used. The signs and symptoms are often nonspecific and include pleuritic chest pain, abdominal and epigastric tenderness, auscultation of bowel sounds in the chest, and hemodynamic instability. Respiratory distress may be present with large injuries causing tension viscerothorax. Up to 50% of initial chest radiographs in patients with confirmed diaphragmatic injuries are reported as normal.
Higher than expected pleural pressure (and therefore a plateau pressure that overestimates transalveolar pressure or stress) is seen in the setting of stiff thoracoabdominal structures caused by obesity arteria meningea anterior buy generic midamor online, anasarca heart attack 30s buy midamor 45 mg visa, ascites, pleural effusion, and so on. Conversely, exaggerated spontaneous breathing efforts can lead to drops in pleural pressure and thus an underestimation of transalveolar pressure if plateau pressure is used alone as an estimate. This is also not the case in this scenario, so conditions confounding interpretation of plateau pressure as a surrogate for transalveolar pressure are absent. A 50-year-old man with a history of hypertension and diabetes was admitted for acute blood loss anemia from upper gastrointestinal bleeding. He has received 2 units packed red blood cells and was started on a pantoprazole drip, and his hemoglobin has been stable now for 24 hours. Furosemide Conservative fluid management for patients who are hemodynamically stable (mean arterial pressure > 65 mmHg and off pressors for at least 12 hours) have been shown to have better survival than liberal fluid management. The use of albumin and diuretic will achieve a greater negative balance but might dehydrate the patient (choice C). Unlike the scenario in question 1, in this situation, the plateau pressure is a poor surrogate for transalveolar pressure (stress) because high thoracoabdominal elastance due to ascites and anasarca has led to a markedly elevated pleural pressure. When its value as estimated from esophageal manometry (15 cm H2O) is subtracted from plateau pressure (38 cm H2O), the difference, which is transalveolar pressure, is 23 cm H2O, a magnitude well below the standard for excessive lung stress. Contrary to what interpretation of plateau pressure alone would suggest, calculation of transalveolar pressure actually indicates adherence to lung-protective ventilation in regard to barotrauma. He had a sudden decompensation with rapid development of obstructive shock caused by a clinically evident right tension pneumothorax. He is facing imminent cardiocirculatory arrest and therefore needs emergent anterior chest needle decompression. Waiting for radiographic confirmation (choice A) of pneumothorax would delay potentially life-saving management. If immediately available, bedside thoracic ultrasound can complement clinical judgment in establishing the presence of pneumothorax when circulatory compromise is less severe. Definitions, Acute Respiratory Distress Syndrome mechanisms, relevant outcomes, and clinical trial coordination. Sepsis pathophysiology, chronic critical illness, and persistent inflammationimmunosuppression and catabolism syndrome. Respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Morphological response to positive end expiratory pressure in acute respiratory failure. Perspective on lung injury and recruitment: a skeptical look at the opening and collapse story. Severe impairment in lung function induced by high peak airway pressure during mechanical ventilation. A positron emission tomographic comparison of pulmonary vascular permeability during the adult respiratory distress syndrome and pneumonia. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. Hypercapnia attenuates ventilatorinduced lung injury via a disintegrin and metalloprotease-17. A high positive end-expiratory pressure, low tidal volume ventilatory strategy improves outcome in persistent acute respiratory distress syndrome: a randomized, controlled trial. High tidal volume and positive fluid balance are associated with worse outcome in acute lung injury. Meta-analysis: ventilation strategies and outcomes of the acute respiratory distress syndrome and acute lung injury. Chest wall restriction limits high airway pressure-induced lung injury in young rabbits. Accuracy of plateau pressure and stress index to identify injurious ventilation in patients with acute respiratory distress syndrome. Lung stress and strain during mechanical ventilation for acute respiratory distress syndrome. Respective effects of end-expiratory and end-inspiratory pressures on alveolar recruitment in acute lung injury. Tidal hyperinflation during low tidal volume ventilation in acute respiratory distress syndrome. Comparative effects of volutrauma and atelectrauma on lung inflammation in experimental acute respiratory distress syndrome. Open lung approach for the acute respiratory distress syndrome: a pilot, randomized controlled trial. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. Oxygenation response to positive end-expiratory pressure predicts mortality in acute respiratory distress syndrome. Recruitment and derecruitment during acute respiratory failure: an experimental study. Airway pressuretime curve profile (stress index) detects tidal recruitment/ hyperinflation in experimental acute lung injury. Bedside selection of positive end-expiratory pressure in mild, moderate, and severe acute respiratory distress syndrome. Spontaneous breathing with airway pressure release ventilation favors ventilation in dependent lung regions and counters cyclic alveolar collapse in oleic-acid-induced lung injury: a randomized controlled computed tomography trial. Spontaneous breathing during ventilatory support improves ventilation-perfusion distributions in patients with acute respiratory distress syndrome. An Official American Thoracic Society/ European Society of Intensive Care Medicine/Society of Critical Care Medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Reversibility of lung collapse and hypoxemia in early acute respiratory distress syndrome. Effects of positive endexpiratory pressure on alveolar recruitment and gas exchange in patients with the adult respiratory distress syndrome. Characteristics and outcomes of patients treated with airway pressure release ventilation for acute respiratory distress syndrome: A retrospective observational study. Airway pressure release ventilation as a primary ventilatory mode in acute respiratory distress syndrome. Tidal volume variability during airway pressure release ventilation: case summary and theoretical analysis. Airway pressure release ventilation versus assist-control ventilation: a comparative propensity score and international cohort study. Spontaneous breathing during lung-protective ventilation in an experimental acute lung injury model: high transpulmonary pressure associated with strong spontaneous breathing effort may worsen lung injury. Comparison of lung protection strategies using conventional and high-frequency oscillatory ventilation. High-frequency oscillatory ventilation for acute respiratory distress syndrome in adults: a randomized, controlled trial. High frequency oscillatory ventilation compared with conventional mechanical ventilation in adult respiratory distress syndrome: a randomized 229 88. Airway pressure release ventilation and high-frequency oscillatory ventilation: potential strategies to treat severe hypoxemia and prevent ventilator-induced lung injury. Is high-frequency oscillatory ventilation more effective and safer than conventional protective ventilation in adult acute respiratory distress syndrome patients Highfrequency ventilation does not provide mortality benefit in comparison with conventional lung-protective ventilation in acute respiratory distress syndrome: a meta-analysis of the randomized controlled trials. High-frequency oscillatory ventilation versus conventional ventilation for acute respiratory distress syndrome. Lung recruitment maneuvers during acute respiratory distress syndrome: is it useful Impact of pressure profile and duration of recruitment maneuvers on morphofunctional and biochemical variables in experimental lung injury. Effects of recruiting maneuvers in patients with acute respiratory distress syndrome ventilated with protective ventilatory strategy. Effects of recruitment maneuvers in patients with acute lung injury and acute respiratory distress syndrome ventilated with high positive endexpiratory pressure. A study of the physiologic responses to a lung recruitment maneuver in acute lung injury and acute respiratory distress syndrome.
Ultimately arteria 90 entupida buy midamor online from canada, this leads to ventilation/ perfusion mismatch with resultant hypoxia and hypercarbia blood pressure of 10060 cheap 45mg midamor visa. Massive fluid resuscitation with crystalloid solutions plays a prominent and potentially preventable role in the development of this syndrome. Such conditions include abdominal trauma, ruptured abdominal aortic aneurysm, retroperitoneal hemorrhage, elective abdominal operations, complications of pregnancy, and hepatic transplantation. First described by Kron et al, the technique involves clamping the bladder catheter, followed by the injection of 50 to 100 mL of sterile saline into the bladder. To avoid hypotension upon decompression, it is important to ensure that adequate intravascular volume resuscitation has been accomplished. Complications of abdominal decompression include hyperkalemia, respiratory alkalosis, hemorrhage, and reperfusion injury. Additional concerns include infection, fluid loss, evisceration, enterocutaneous fistula formation, and exposure of the abdominal viscera. The large ventral hernia that results from temporary closure frequently requires delayed repair with nonabsorbable mesh. The colon is the second most commonly injured organ in penetrating abdominal trauma, and concomitant injuries and complications from such wounds are common (Table 1). When these patients present, the surgeon must decide whether to primarily repair the colon, resect and perform an anastomosis, or create a colostomy. There is continuing debate as to the optimal treatment for penetrating colon injuries. Ogilvie published a letter in 1943 that mandated the performance of colostomy for colon injuries: the treatment of colon injuries is based on the known insecurity of suture and the dangers of leakage. Simple closure of a wound of the colon, however small, is unwarranted; men have survived such an operation, but others have died who would still be alive had they fallen into the hands of a surgeon with less optimism and more sense. Injured segments must either be exteriorized, or functionally excluded by a proximal colostomy. This declaration was based on scant evidence but was issued in response to a mortality rate greater than 50%. As military surgeons returned home, they perpetuated the dogma of treating all colonic injuries with colostomy. Notably, as early as 1951, Woodhall and Ochsner reported decreased mortality rate with primary repair compared to colostomy in civilian practice (8. In recent decades, surgeons have become more comfortable with primary repair of colon injuries that previously would have been diverted. Many surgeons are comfortable with repair or resection with anastomosis of right colon injuries, but treatment of left colon injuries are increasingly treated without colostomy as well. In previous decades, surgeons were forced to justify primary repair of a colon injury, but more recent data have changed this position. Stone and Fabian published a landmark prospective series in 1979 suggesting that many injuries could be managed without colostomy in stable patients, and in 1991, Chappuis et al reported a prospective, randomized study of primary repair versus diversion in penetrating colon injuries. Patients were randomized irrespective of injury, contamination, transfusions, or shock. A 1996 prospective, randomized study by Gonzalez evaluated patients with penetrating colon injuries and was randomized to either primary repair with or without resection versus mandatory colostomy. Although these differences were not statistically significant, this experience demonstrated that primary repair was at least equal to mandatory colostomy and might be superior. Several randomized trials appear to support repair or anastomosis in these populations. Gonzalez et al reported their 6-year experience with 181 patients with penetrating colon injury. These patients were again randomized to primary repair or colostomy, regardless of other injuries, heavy fecal contamination, or hypotension. In hemodynamically unstable patients, the complication rate was also lower in the primary repair group (26% vs. Complications declined over time in both groups, which can likely be explained by improvement in the overall care of trauma victims. Sixty percent of patients were treated with primary repair or resection and anastomosis. There was a 19% complication rate (colon and noncolon related) in the primary repair group as compared with a 36% complication rate in the diversion group. The authors also reported a 7% complication rate at the time of colostomy reversal. Berne et al performed a retrospective review of 40 patients who underwent colostomy reversal after trauma. They found a morbidity rate of 55% in patients initially treated with colostomy for colon injury. A note of caution was introduced by Ott et al with a review of 174 patients that showed a sixfold increase in leak rates in anastomoses performed in the setting of an open abdomen after damage control celiotomy, suggesting that scenarios still exist in which either delayed reconstruction when abdominal closure is possible or diversion may have a role. The decision to perform a diverting colostomy may seem theoretically sound, but contemporary trauma care must be based on evidence and not intuition. In addition to not clearly showing a short-term benefit in most instances, diverting colostomy condemns patients to a subsequent operation for reanastomosis and exposes them to stoma-specific complications, including hernia, ostomy stenosis or retraction, necrosis and skin breakdown at the ostomy site, and the lifestyle limitations attached to ostomy management. Based on current evidence, mandatory colostomy for penetrating colon injury should be abandoned. Consideration of colostomy for any colon injury, regardless of the coexisting injuries or comorbid conditions, must be justified based on patient physiology in the operating room and the realization that repair or anastomosis presents an equivalently safe or even superior option in many instances. It describes a modified operative sequence in which the immediate repair of all injuries is abandoned in favor of a staged approach. This is done in recognition of the physiologic insult suffered by the critically injured patient, and the continued deterioration during the operation, which may render that insult irreversible. The concept of abbreviated laparotomy dates to 1908, when Pringle described the principles of compression and hepatic packing for control of portal venous hemorrhage. In 1983, Stone et al introduced the modern concept of the abbreviated laparotomy with subsequent resuscitation and interval completion laparotomy after physiologic restoration. In 1993, Rotondo and associates popularized the term "damage control," and it has rapidly become a standard in the treatment of critically injured patients with deteriorating physiologic parameters in many areas of trauma and emergency surgery. Three stages of damage-control laparotomy were originally described-control of hemorrhage and contamination, ongoing resuscitation, and subsequent definitive repair of injuries. The first step is the truncated laparotomy in the face of life-threatening physiologic circumstances. It involves the control of hemorrhage with intra-abdominal packing and control of enteric contamination with rapid sutures, stapling, or resection. Lengthy vascular repairs are not pursued, but temporary shunting is used liberally. Packing should provide pressure in vectors that recreate the disrupted tissue planes, but it must be remembered that it is difficult to obtain hemostasis of arterial injuries with packing alone. If rapid repair, ligation, or stenting cannot be accomplished, then other methods, such as angiographic embolization, should be employed. Biliary tract and pancreatic injuries can be managed with external tube drainage in nearly all acute settings. Once the abbreviated laparotomy is completed, the abdomen is closed by temporary methods. For this reason, either commercial or modified vacuum dressings have largely become the dressings of choice in these instances. Each of these devastating physiologic complications has a compounding effect on the others. Hypothermia exists in as many as half of injured patients following trauma laparotomy and increases the requirement for fluid resuscitation, vasopressors, inotropes, and transfusions. It is independently associated with increased morbidity, organ dysfunction, coagulopathy, and mortality rate. Acidosis results from inadequate oxygen delivery secondary to hemorrhage, which results in anaerobic metabolism and the release of lactic acid. Acidosis worsens coagulopathy, depresses myocardial contractility, diminishes inotropic response to catecholamines, and predisposes to dysrhythmias. Correction of acidosis is directed at improvement of oxygen delivery and optimizing cardiac output.
Order midamor paypal. Only a Glass of lemon lime water Control Blood Pressure!.
References
- Takagi M, Aihara N, Kuribayashi S, et al. Localized right ventricular morphological abnormalities detected by electronbeam computed tomography represent arrhythmogenic substrates in patients with the Brugada syndrome. Eur Heart J. 2001;22:1032-41.
- Summers PE, Ferraro D, Duzzi D, et al. A quantitative comparison of BOLD fMRI responses to noxious and innocuous stimuli in the human spinal cord. Neuroimage. 2010;50(4):1408-1415.
- Prasad D, Schiff D. Malignant spinal-cord compression. Lancet Oncol 2005;6(1):15-24.
- Khalil M: Management of impacted proximal ureteral stone: extracorporeal shock wave lithotripsy versus ureteroscopy with holmium:YAG laser lithotripsy, Urol Ann 5:88-92, 2013.
- Graham MV, Purdy JA, Emami B, et al. Clinical dosevolume histogram analysis for pneumonitis after 3D treatment for non-small cell lung cancer (NSCLC). Int J Radiat Oncol Biol Phys 1999;45(2):323-329.