Mary E. Fredrickson, PharmD, BCPS
- Clinical Pharmacy Specialist, St. Joseph Warren Hospital, Warren, Ohio
https://www.neomed.edu/directory-profile/fredrickson-liz-132020/
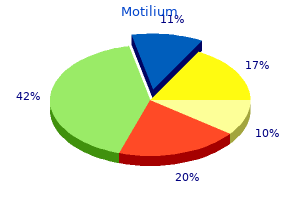
This surgery combines correction of atrial venous return with the arterial switch procedure gastritis zungenbelag order motilium with paypal. However helicobacter gastritis diet purchase motilium 10mg line, systolic dysfunction of the left ventricle seems to be common after the double switch procedure gastritis diet for cats motilium 10 mg. Although shortterm to midterm results are promising nodular gastritis definition discount motilium generic, longterm followup is unavailable gastritis diet 60 best 10mg motilium. The morphologic right ventricle becomes the systemic ventricle, making tricuspid valve dysplasia and systolic right ventricle dysfunction the most important prognostic factors. The postnatal survival rate of greater than 90% declines progressively through the years to a 20-year survival rate of 65% to 75%. Longterm outcome of surgi cally treated patients with corrected transposition of the great arteries. Chromosomal abnormalities are found in 10% to 20% of cases; trisomies 18 and 13 are the most frequently associated. The defect is usually perimembranous and is considered noncommitted because it opens in to the right ventricle beneath the septal leaflet of the tricuspid valve or because the tension apparatus of the atrioventricular valves is interposed between the margins of the defect and the subarterial outflow tracts. As previously described, the pulmonary artery bifurcates early in to pulmonary branches, and the aorta gives origin to supraaortic vessels far from the semilunar valve. The fetus should be evaluated periodically (every 4 to 6 weeks) to rule out progressive outflow tract obstruction and other associated cardiac and extracardiac anomalies that could manifest later in pregnancy. Prognosis generally varies depending on other anomalies, which also influence the pregnancy termination rate. If postnatal series are considered, the overall surgical mortality rate for biventricular repair is low; a 10-year survival rate greater than 80% is reported. Pulmonary arteries originate separately from common trunk Absence of pulmonary trunk. Both pulmonary arteries originate from the arterial trunk separate from each other Two pulmonary branches arise from the descending aorta. Other cardiac anomalies are present in 35% to 50% of cases, particularly arch abnormali ties and absence of the ductus arteriosus. Van Praagh and Van Praagh Classification for Common Arterial Trunk Type A1 Anatomic Features Origin of partially separate main pulmonary trunk from common trunk. Corresponds to Collett and Edwards type I Pulmonary arteries originate separately from common trunk Absence of one pulmonary artery. The truncal valve anulus is usually dysplastic and is formed by two, three, or four cusps. The common truncal artery supplies the pulmonary, aortic, and coronary circulations. Coronary artery patterns are abnormal in many patients; the most frequent variations are an intramural course and a single coronary artery. Postnatal manifestations appear during the first days of life and are a consequence of saturated and desaturated blood flow mixing and a nonre strictive lefttoright shunt, resulting in a variable degree of cyanosis and pulmonary vascular disease. The truncal valve anulus is formed by two, three, four, or more leaflets and is usually dysplastic, leading to valve regurgitation, which can be evaluated with color Doppler. The appearance of pulmonary vascular disease and systemic valve failure worsens the prognosis, leading to a 15year survival rate between 65% and 80%. The four-chamber view can be normal, but routine outflow tract examination shows a typicalappearance. The fetus should be evaluated periodically (every 4 weeks) to rule out progressive valve dysfunction and other associ ated cardiac and extracardiac anomalies that could manifest later in pregnancy. Delivery should be planned in a tertiary referral center with cardiac surgery capabilities. There is a trend to make the cor rection in the neonatal period, preferably after pulmonary vascular resistance decreases, usually during the 2nd or 3rd week of life. If congestive heart failure or aortic arch inter ruption is present, surgery should be undertaken regardless of the age of the patient. Prognosis depends on the presence of extracardiac and chromosomal anomalies and of unfavorable cardiac anatomy. If surgical series are considered, the overall surgical mortality rate ranges from 5% to 20% depending on the presence of associated anomalies. Truncus arte riosus: diagnostic accuracy, outcomes, and impact of prenatal diagno sis. Common arterial trunk in the fetus: characteristics, associations, and outcome in a multicentre series of 23 cases. The anatomy of common aorticopulmo nary trunk (truncus arteriosus communis) and its embryologic impli cations: a study of 57 necropsy cases. Accuracy of prenatal echocardio graphic diagnosis and prognosis of fetuses with conotruncal anoma lies. Longterm followup after primary complete repair of common arterial trunk with homo graft: a 40year experience. Double-inlet single ventricle comprises a heterogeneous group of cardiac anomalies characterized by the presence of two atria with a single ventricle. Other cardiac (valvular atresia or stenosis or coarctation of aorta) or noncardiac (heterotaxia, cystic hygroma, congenital diaphragmatic hernia) anomalies are frequently associated. Chromosomal anomalies may be also associated (trisomy 18, Klinefelter syndrome, DiGeorge syndrome, or Goldenhar syndrome). The connection between both atria and one ventricle may be through one or two atrioventricular valves. Although a rudimentary accessory ventricle may also exist, only one ventricle is functional receiving the flow from both atria. This entity does not include cases with a single functional ventricle secondary to mitral or tricuspid atresia. Etiology and Pathophysiology the morphologic spectrum of double-inlet single ventricle is broad, with a variety of segmental patterns and anatomic variables, including differences in anatomic pattern of the single ventricle (left, right, or indeterminate); the sizes of the atrioventricular valves or atresia of one atrioventricular valve; variable ventricular looping and ventriculoarterial relationship; and obstruction to systemic or pulmonary outflow (or both systemic and pulmonary outflow). The most common form is a single left ventricle with a rudimentary right ventricle, two atrioventricular valves, and aorta disposed anteriorly and to the left of the pulmonary artery. Outflows from the great arteries are usually anomalous with typically an anterior and left aortic disposition. Anatomic, imaging, and clinical characteristics of double-inlet, double-outlet right ventricle. Mid-term results for double inlet left ventricle and similar morphologies: timing of Damus-KayeStansel. The terms heterotaxy syndrome, cardiosplenic syndrome, right and left isomerism, and situs ambiguus are often used to describe these defects. It is associated with a very poor prognosis owing to high in utero and neonatal mortality. Heart block, atrioventricular septal defect, double-outlet right ventricle, right or left ventricular outflow tract obstruction, total anomalous pulmonary vein drainage, persistence of left superior vena cava, and aorta and inferior vena cava located on the same abdominal side may also be present. However, associations with chromosome 22q11 deletion (DiGeorge syndrome), trisomy 18, trisomy 13, and other chromosomal deletions or inversions have been described. Complete heart block, complex cardiac abnormalities, and fetal hydrops are poor prognostic features. Right isomerism is associated with a worse prognosis with a very high mortality rate (>90%) in the 1st year after birth. Atrial isomerism also can be diagnosed in the first trimester as increased nuchal translucency, cardiac rhythm disturbance, or hydrops. A proper situs abdominal exploration is essential to detect typical anomalies such as stomach dextroposition, intestinal obstruction, and inferior vena cava malposition (Video 92-2). Other typical anomalies, such as asplenia or pulmonary lobulation, may require postnatal imaging or necropsy. Etiology and Pathophysiology Atrial isomerism manifests with a varied spectrum of cardiac malformations with viscerocardiac heterotaxy occurring in most cases. Typical features include asplenia, bilateral trilobed lungs, intestinal malrotation, abnormal drainage of the pulmonary veins, persistence of the left superior vena cava, aorta and inferior vena cava located on the same abdominal side, atrioventricular septal defect, and ductus-dependent pulmonary flow. Fetal anomalies include bilateral morphologic left atrial appendages, bilobed lungs, multiple splenuli, and malrotation of the intestines. The nomenclature, definition and classification of cardiac structures in the setting of heterotaxy. Clinical features, management and outcome of children with fetal and postnatal diagnoses of isomerism syndromes. The syndrome of left isomerism: sonographic findings and outcome in prenatally diagnosed cases. Spectrum of cardiovascular disease: accuracy of diagnosis and outcome in fetal heterotaxy syndrome. With the improvement in long-term outlook for these patients as a result of modern cardiac surgery, intraabdominal anomalies have become increasingly relevant because they may affect longterm outcome. Immediate and increasing hypoxemia and acidosis are the rule, which can be reversed only by emer gency postnatal cardiac surgery. The four pulmonary veins drain in to a venous collector located behind the left atrium, from which a vertical vein runs up to reach the innominate vein, and this terminates in the right superior vena cava and right atrium. It has been reported that the vertical vein may be obstructed, but this is rarely severe in the perinatal period. The pulmonary veins drain through the coronary sinus or directly in to the right atrium. The pulmonary veins converge in to a descending vertical vein that reaches the abdomen through the diaphragm. It usually drains in to the portal vein or, more rarely, in to the ductus venosus or the inferior vena cava. These diagnostic features are mainly indirect indicators and may not all be present. For instance, coexistence of heterotaxia may make diagnosis very difficult because of the variable number of pulmonary veins. Other Applicable Modality Bflow imaging using spatiotemporal image correlation may be helpful in refining the diagnosis of pulmonary anomalous return. Color Doppler shows the connection of right and left pulmonaryveinstothecollector. If severe obstruction is suspected, it may be necessary to intervene in the first few hours of life. Partial and total anomalous pulmonary venous connection in the fetus: twodimensional and Doppler echocardiographic findings. Prenatal diagnosis and antenatal history of total anomalous pulmonary venous return. The echocardiographic diagnosis of totally anomalous pulmonary venous connection in the fetus. Fetal echocardiography in detecting anomalous pulmonary venous connection: four false positive cases. Two and fourdimensional echocardiography with Bflow imaging and spatiotemporal image cor relation in prenatal diagnosis of isolated total anomalous pulmonary venous connection. Prenatal diagnosis in fetal life can be reliably excluded only by direct examination of pulmonary venous blood flow entering the left atrium on color or pulsed flow mapping. Prevalence and Epidemiology Anomalous systemic venous return is rarely seen prenatally. Etiology and Pathophysiology Although knowledge of the normal anatomy of the fetal venous system has increased enormously, little information is available on the mechanisms leading to abnormal in utero development. Anomalies of systemic venous drainage rep resent a heterogeneous group of malformations including abnormalities in cardinal, umbilical, and vitelline veins. Consequently, the venous blood from the caudal part of the body reaches the heart via the azygos or hemiazygos vein through the superior vena cava. Outcome is related to the associated anomalies and may be affected by agenesis or underdevelopment of the fetal portal system. Manifestations of Disease Clinical Presentation the prenatal course is mostly uneventful1,3 except for very rare cases of absent ductus venosus leading to right heart overload and failure, which might evolve to hydrops. Other Applicable Modality Bflow by spatiotemporal image correlation may be helpful to understand complex venous return anomalies better. There is a high association with heterotaxia or other structural or chromosomal anomalies. The fetal venous system, part I: normal embryology, anatomy, hemodynamics, ultrasound evaluation and Doppler investigation. Left superior vena cava persistence in patients undergoing pacemaker or cardioverter defibrillator implantation: a 10year experience. Shunt diameter in agenesis of ductus venosus with extrahepatic portosystemic shunt impacts prognosis. Pathogenesis of persistent left superior vena cava with a coronary sinus connection. In the presence of dilatation of the coronary sinus or azygos vein, an anomalous systemic venous return may be suspected. In series including neonates and infants, cardiomyopathies represent about 2% to 7% of all cardiac defects. The prevalence is thought to be higher during fetal life, probably around 6% to 11%. The difference is explained by intrauterine loss, which may occur in one-third of affected fetuses. There may be great variability in the presentation of dilated cardiomyopathy in the fetus. Prevalence and Epidemiology Cardiomyopathy is a very rare disease during intrauterine life.
Smoking and smoking cessation during early pregnancy and its effect on adverse pregnancy outcomes and fetal growth gastritis rare symptoms buy discount motilium 10 mg. Prenatal smoking cessation and the risk of delivering preterm and small-for-gestational-age newborns diet of gastritis patient buy motilium on line. Acetylsalicylic acid for the prevention of preeclampsia and intra-uterine growth restriction in women with abnormal uterine artery Doppler: a systematic review and meta-analysis gastritis diet journal printable discount motilium 10 mg amex. Changes of pulsatility index from fetal vessels preceding the onset of late decelerations in growthretarded fetuses gastritis questionnaire order motilium 10mg amex. Qualitative venous Doppler waveform analysis improves prediction of critical perinatal outcomes in premature growth-restricted fetuses gastritis diet ðñò buy generic motilium 10mg on line. Before amniocentesis, the patient should be counseled regarding the purpose, risks, and alternatives to the procedure, and informed consent should be obtained. If the location of the amnionchorion separation cannot be avoided during amniocentesis, one may consider postponing the procedure to a gestational age when the amnion and chorion should be fused. The maternal bowel and bladder should be identified and avoided because traversing the maternal bowel can introduce bowel flora in to the amniotic cavity leading to chorioamnionitis and subsequent pregnancy loss. Although some studies suggested complications were increased after transplacental amniocentesis,3 other studies refuted this suggestion. If it cannot be avoided, the needle is usually directed through the thinnest portion of the placenta. Color Doppler may be useful in avoiding the umbilical cord insertion site and large chorionic vessels. A large area should be prepared because the fetus may move, changing the optimal fluid pocket site. Local anesthesia can be administered before inserting the spinal needle; however, most patients tolerate the procedure with minimal discomfort. Local anesthesia does not alleviate the discomfort or cramping that usually occurs when the needle is inserted in to the uterine muscle. The "freehand technique" allows adjustment of the needle direction and is the method that most experienced operators prefer. A needle-guiding device that is attached to the transducer is also available, which may assist in reaching the designated fluid pocket. When the needle tip is in the targeted fluid pocket, the assistant holds the transducer and maintains visualization of the needle tip while the operator withdraws the amniotic fluid. This window generally ensures enough time to obtain the results if the patient should choose to terminate the pregnancy based on an abnormal karyotype. Genetic amniocentesis can also be performed later in pregnancy to assist in deciding mode or timing of delivery and plans for extent of fetal or neonatal intervention if a lethal karyotype is discovered. Interphase fluorescence in situ hybridization, which detects aneuploidy only of chromosomes 13, 18, 21, X, and Y, yields results within 24 to 48 hours. Although fluorescence in situ hybridization results are accurate, rare cases of false-positive and falsenegative results have been reported. The amniotic fluid is most commonly evaluated for a lecithin-to-sphingomyelin (L/S) ratio and the presence or absence of phosphatidylglycerol. The risk of respiratory distress is exceedingly low when the L/S ratio is greater than 2 and phosphatidylglycerol is present. Some laboratories use other cutoffs, and physicians should be familiar with local standards. Less frequently performed studies include assessment of the lamellar body count, fluorescence polarization, and the foam stability index. If amniotic fluid cannot be easily withdrawn, the fetal membranes are likely tented over the needle tip. If this thrust does not pierce the membranes, the operator may need to reposition the needle. The initial drop of amniotic fluid may contain maternal cells collected as the needle passed through the maternal tissues. Most operators discard this initial drop because it may introduce low-level mosaicism with maternal cells in cytogenetic studies. The amount of amniotic fluid withdrawn should be based on the gestational age and the type of test being performed on the fluid. Karyotype analysis usually requires 20 to 30 mL; a fetal lung maturity test requires 5 to 10 mL of fluid. After the appropriate amount of amniotic fluid is withdrawn, the operator detaches the syringe, replaces the stylet, and quickly removes the spinal needle. Amniotic fluid is transferred from the syringes to the specimen tubes for laboratory testing. The patient should be counseled that mild intermittent cramping is common but that she should call her physician or midwife if she has regular, painful contractions; leakage of fluid from the vagina; vaginal bleeding; or a fever. Patients should be advised to maintain pelvic rest and decreased activity for 24 hours after the procedure. Unsensitized Rh0(D)-negative women should be given Rh0(D) immune globulin after an amniocentesis to prevent Rh sensitization. Until substantial evidence exists regarding the safety of amniocentesis in women with the aforementioned infections, women should be counseled regarding the plausible risk of vertical transmission and alternative options, including first-trimester and second-trimester screening for aneuploidy. Indications Amniocentesis is most commonly indicated for prenatal diagnosis and for fetal lung maturity. Other indications include amnioreduction, diagnosis of an intraamniotic infection, confirmation of preterm premature rupture of membranes with an amnio dye test, evaluation of hemolytic anemia in the fetus, diagnosis of hemoglobinopathy, and diagnosis of neural tube defects. The guidance is similar to that used during cordocentesis to evaluate for fetal platelet count, anemia, and blood type. Outcomes and Complications Many large studies have confirmed the safety of genetic amniocentesis and the cytogenetic diagnostic accuracy of the procedure. In more recent studies, the procedure-related loss rate was reported to be 1: 300 to 1: 500, and the rate may be even lower depending on the experience of the operator. Other infrequent complications include amniotic fluid leakage (which occurs in about 1% to 2% of all cases), vaginal bleeding, chorioamnionitis (which occurs in <1%), needle injuries to the fetus, and amniotic fluid cell culture failure. Randomised trial to assess safety and fetal outcome of early and midtrimester amniocentesis. Spontaneous abortion following mid-trimester amniocentesis: clinical significance of placental perforation and blood-stained amniotic fluid. Incidence of spontaneous abortion after amniocentesis: influence of placental localization and past obstetric and gynecologic history. Procedure-related fetal losses in transplacental versus nontransplacental genetic amniocentesis. Genetic amniocentesis: impact of placental position upon the risk of pregnancy loss. Transplacental needle passage and other risk-factors associated with second trimester amniocentesis. Fetal loss rate after second trimester amniocentesis at different gestational age. Risk factors for procedurerelated fetal losses after mid-trimester genetic amniocentesis. Risk factors for perinatal human immunodeficiency virus transmission in patients receiving zidovudine prophylaxis. Procedure-related complications of amniocentesis and chorionic villous sampling: a systematic review. Amniocentesis as a possible risk factor for mother-to-infant transmission of hepatitis C virus. Amniocentesis in mothers who are hepatitis B virus carriers does not expose the infant to an increased risk of hepatitis B virus infection. Risk of hepatitis B transmission after amniocentesis in chronic hepatitis B carriers. The presence of hepatitis B surface antigen and deoxyribonucleic acid in amniotic fluid and cord blood. Age-specific risk of fetal loss post second trimester amniocentesis: analysis of 5,043 cases. Fetal blood transfusions were initially performed via the intraperitoneal route,1 but that approach is rarely used since the advent of intravascular transfusions. Intracardiac access has also been described, but that is reserved for extraordinary circumstances. These procedures should usually be done in a setting where an urgent cesarean delivery can take place, such as in an operating room or in close proximity to the labor and delivery floor. In some cases, it may be useful to have the patient evaluated by the anesthesia team and prepared for a possible emergent delivery. In these situations, consideration should be given to administering prenatal steroids before the procedure. Counseling All cordocentesis procedures should be preceded by an extensive counseling session in which the indication, risks, benefits, and alternatives to the procedure are discussed. Other, less common locations include a free-floating loop of cord and the insertion site of the cord in to the fetal abdomen. Both of these locations are associated with higher complication rates secondary to fetal movement. Intraperitoneal or intracardiac transfusions are reserved for cases in which the usual intravascular approach is essentially deemed to be impossible. If the placenta is anterior, it should be traversed to reach the cord insertion site; in such cases, paralysis of the fetal skeletal muscles is usually not indicated. However, in many cases in which the placenta is posterior, the cord insertion site can be reached only by traversing the amniotic cavity, where fetal activity could disrupt the needle during the procedure. In these cases, medical paralysis of fetal skeletal muscle should be considered, especially if a transfusion is to be performed. Although antibiotics have not been proven to decrease the complication rate, we administer antibiotic prophylaxis before the procedure. After covering the transducer face with a sterile sheath, the vascular target should be identified again. In most diagnostic cases, a 22-gauge needle can be used; however, we perform blood transfusions through a 20-gauge needle. The needle length is determined by the measured distance from the skin to the targeted vessel and ranges from 9 to 16 cm in most cases. When the needle tip is seated within the vessel, the stylus is removed, a syringe that was previously flushed with heparin is attached to the needle, and a fetal blood sample is aspirated. The mean corpuscular volume obtained from the aspirated sample is generally used as an indicator that the blood is fetal. In cases where a transfusion is indicated, T-connector tubing is attached to the needle so that transfusion and further sampling does not cause inadvertent movement of the needle tip. If paralysis of fetal skeletal muscle is needed, we recommend using vecuronium bromide at a dose of 0. The blood transfused should be cytomegalovirus-negative, irradiated, filtered, O negative packed red blood cells. The blood volume to be transfused depends on several factors, including the estimated fetal weight, initial fetal hematocrit, and final target hematocrit. After adequate transfusion, a repeat sample is taken to ensure having obtained the desired final hemoglobin level, and the needle is withdrawn at the same angle of its insertion. The puncture site is visually assessed for streaming, which is observed until its cessation. Throughout the procedure and after it, fetal well-being is assessed by intermittent visualization of cardiac activity. Fetal heart rate and uterine activity in viable pregnancies should be monitored for at least 2 hours after the procedure. In a single center in Italy, the reported use of cordocentesis for prenatal diagnosis of karyotype analysis decreased from 26. We rarely perform cordocentesis for diagnostic purposes or for other therapeutic indications, such as fetal drug administration (antithyroid drugs for fetal thyrotoxicosis or digoxin for fetal arrhythmia unresponsive for maternal therapy). Fetal Anemia Alloimmunization results in the production of antibodies to red blood cell surface antigens, which traverse the placenta and can lead to fetal anemia. Parvovirus infection has also been described as a cause of fetal anemia, particularly during the first half of pregnancy. To identify these fetuses, it is the standard of care to screen all pregnant women for red blood cell alloimmune sensitization during each pregnancy. IgG antibodies produced in response to this sensitization cross the placenta and may cause thrombocytopenia that is severe enough to cause intracranial hemorrhages in 20% to 30% of affected cases. The procedure was repeated at regular intervals throughout the remainder of their pregnancies. This protocol established a baseline fetal platelet count to document subsequent improvements and to monitor the effectiveness of treatment administered to permit the addition of supplemental therapy, if the response was suboptimal. It was further recommended that the procedure be performed with immediate access to a rapid platelet count during the sampling before the needle is withdrawn from the fetal vessel. If a platelet count of less than 50,000/mL3 is found, a unit of packed maternal platelets should be transfused before withdrawing the needle. As the number of indications for performing cordocentesis in general decreased, there was a concomitant reduction in the number of individuals with substantial experience performing the procedure safely. Current treatment regimens divide patients in to three different risk categories for developing severe fetal thrombocytopenia and its consequences, based on the occurrence and timing of having had a fetus with an intracranial hemorrhage in a prior pregnancy. Patients in the intermediate group had fetuses with an intracranial hemorrhage detected in the third trimester or shortly after delivery. If the fetal platelet count is found to be greater than 50,000/mL3, no change in therapy is indicated, but if the platelet count is less than 100,000/ mL3, there can be no assurance that a vaginal delivery would be safe several weeks later. If the platelet count is less than 50,000/mL3, therapy should be increased, or the patient should be offered a cesarean delivery in the near future.
Buy motilium australia. How Grapefruit Can Kill You.

Chromosome markers gastritis natural supplements generic motilium 10mg line, such as cystic hygroma healthy liquid diet gastritis buy motilium with a visa, increased nuchal skin fold gastritis juice diet buy 10mg motilium otc, absence of the nasal bone gastritis diet íàï order motilium on line amex, and brain and cardiac anomalies gastritis and back pain discount motilium 10 mg with amex, aid in determining if the fetus is at risk for aneuploidy. When fetal hydrops is encountered, systematic evaluation of the fetus often points to an etiology, which allows for appropriate counseling and treatment options. Peak Systolic Velocity Values of the Middle Cerebral Artery as a Function of Gestational Age Week of Gestation 18 20 22 24 26 28 30 32 34 36 38 40 23. In the absence of red blood cell antigenrelated causes, cases of hydrops should be considered nonimmune. The causes of nonimmune hydrops are copious and often multifactorial, and there is an inherent possibility for differential diagnosis as to the definite etiology of nonimmune hydrops. In the setting of anemia, providers may move to more invasive treatment options-cordocentesis and intrauterine fetal transfusion. In some cases, additional specific gene probes or microarray testing is available to make an early diagnosis of many metabolic and other disorders. Early delivery can be considered after fetal lung maturity is proven, especially considering the possible surgical course after delivery. Infants who did not survive this course were more immature, presented with lower Apgar scores, and more commonly experienced heart failure. Mortality rates remain extremely high, and early detection, investigation, diagnosis, and treatment lead to increased rates of survival. Hydrops fetalis-has there been a change in the diagnostic spectrum and mortality Hydrops fetalis: a retrospective review of cases reported to a large national database and identification of risk factors associated with death. Incidence of chromosomal abnormalities in the presence of fetal subcutaneous oedema, such as nuchal oedema, cystic hygroma, and non-immune hydrops. Middle cerebral artery peak systolic velocity and ductus venosus velocity in the investigation of nonimmune hydrops. Frequency of parvovirus B19 infection in nonimmune hydrops fetalis and utility of three diagnostic methods. Transient hydrops fetalis of the donor fetus in twin-twin transfusion syndrome after therapeutic amnioreduction. Increased concentrations of antiangiogenic factors in mirror syndrome complicating twin-to-twin transfusion syndrome. Cystic adenomatoid malformation of the lung causing hydrops fetalis: case report and review of the literature. Fetomaternal hemorrhage can also occur at spontaneous or induced abortion, owing to maternal trauma, with any maternal vaginal bleeding, at the time of invasive procedures such as chorionic villus sampling or amniocentesis, or spontaneously. In very rare cases, sensitization occurs despite appropriate use of immune globulin, and there are other causative antibodies. When a fetus inherits a paternal antigen that is foreign to the mother and for which the mother has IgG antibodies, these may cross the placenta and sensitize the fetal cells for destruction in the fetal spleen. Severe fetal anemia typically does not develop in first affected pregnancies because of low maternal antibody titers and initial IgM responses that do not cross the placenta, but subsequent pregnancies become progressively more vulnerable. Until the past decade, serial amniocentesis was the only reliable technique to assess severity of fetal anemia. Peak Systolic Velocity Values of the Middle Cerebral Artery as a Function of Gestational Age Week of Gestation 18 Cereb Multiple of Median 1. This noninvasive technique is superior to serial amniocentesis for detection of severe anemia2 and does not lead to the anamnestic response that may result from serial amniocentesis. The measurement should be done manually; if the gain is set too high, the automeasure feature may overestimate the velocity. Other possible markers of severity of fetal anemia have been explored, with limited success. Degree of polyhydramnios, umbilical vein diameter, placental thickness, presence of pericardial effusion, and right-to-left ventricular size have not proved reliable. Summary Protocol for Prenatal Management of Rh and Kell Sensitization Patients at Historical High Risk Includespatientswhose fetusesorinfantsrequired transfusionsinprevious pregnancies 1. Women who have antibodies should be referred to a center with expertise in immune fetal hydrops for discussion of pregnancy risks and management options. If paternity is certain and the father does not possess the antigen in question, the fetus is not at risk. In fetuses that are known to be at risk (because they possess the antigen in question) or cases of unknown paternal antigen status, maternal antibody titers should be followed throughout pregnancy (monthly until 24 weeks and twice monthly thereafter, especially for high-risk antigens such as Rh D or Kell). Worse outcomes are associated with greater prematurity, greater severity of fetal hydrops, lower 5-minute Apgar scores, lower platelet counts, and need for ventilation. In pregnancies that are known or suspected to be at risk, maternal antibody titers should be followed until a critical titer is reached; commonly, the titer never reaches a level that puts the fetus at risk. Hydrops fetalis caused by homozygous -thalassemia and Rh antigen alloimmunization. Anti-Rh D is the most common antibody, although the frequency of Rh D disease has been markedly reduced since the widespread use of Rh0(D) immune globulin. Kell alloimmunization is associated with the least predictable and most severe fetal anemia. Intravascular fetal blood transfusions in cases of severe anemia and hydrops have dramatically improved the outcome of these pregnancies. The Institute of Medicine1 estimated the average cost for each newborn admission is $51,000, resulting in annual health care costs of $26 billion. Preterm birth is complex and incompletely understood, but an important clinical observation supports the claim that a dysfunctional cervix is a significant contributor; a short cervix in midpregnancy more accurately predicts preterm birth than any other clinical test. It has a dual role: (1) Before term, it should remain closed to allow fetal growth and development; (2) close to term, it should soften and dilate to allow fetal passage during labor. The biochemi cal mechanisms responsible for pregnancyassociated cer vical softening and ripening are incompletely elucidated and an active area of research. For singletons, a common definition of a short cervix is less than 25 mm, but the significance varies with gestational age; it corresponds to the 1st percentile at 18 weeks, the 3rd percentile at 22 weeks, the 5th percentile at 24 weeks, and the 10th percentile at 28 weeks. Fetal Number the risk of preterm birth increases when cervical length is less than 25 mm in twins (similar to <15 mm in singletons). The relative risk increased steadily as cervical length shortened to a maximum of 14. In a systematic review of 17 pooled studies of asymptomatic singletons, the likelihood ratio for preterm birth was increased if the gestational age at testing was less than 20 weeks compared with 20 to 24 weeks. The most common pathophysiology linked to a short cervix is infection and inflammation. Other possible causes of a short cervix include hemorrhage, preterm contractions, weakened extracellular matrix of the cervical stroma, and aggressive cone biopsy. A study examining the connection between a short cervix and inflammation and infection defined cervical insuffi ciency as dilatation 1. Using this definition, positive amniotic fluid cultures are present in half of cases of cervical insufficiency. Similarly, studies of women with a short cervix (<25 mm) revealed increased prevalence of intrauterine infection and inflammation. In the setting of a short cervix, the risk of cultureproven microbial invasion of the amniotic cavity is 4. In one study, the risk of microbial invasion was higher when the cervix was less than 15 mm (26. Uterine Contractility and a Short Cervix Although it is intuitive that uterine contractility would cause a short cervix, this association is weak at best. Uterine Overdistention and Short Cervix Uterine overdistention from multiple gestation or polyhy dramnios is a known cause of preterm birth and cervical shortening. Although the risk of preterm birth increases rapidly when cervical length is less than 15 mm in a single ton gestation, in a twin gestation, a similar increase in risk is seen at a higher threshold, with a cervical length of less than 25 mm. The patho physiology of preterm birth is different for multiple versus singleton gestations. Cervical Insufficiency Cervical insufficiency is a recognized cause of cervical shortening and preterm birth. Cervical tissue gets its "strength" from its collagenrich connective tissue, and abnormalities of cervical tissue have been associated with adverse outcomes. Future research aimed at clarifying the role of a short cervix in preterm birth will aid efforts to tailor suitable therapies to prevent preterm birth. Manifestations of Disease Clinical Presentation Most patients are asymptomatic when a short cervix is dis covered, regardless of whether the discovery occurs during screening of a highrisk patient or routine fetal anatomic survey in a lowrisk patient. If a patient presents with both a short cervix and symptoms of preterm labor, the likeli hood of delivery within 2 weeks is significantly greater than when no symptoms are present. The transducer is introduced in to the vagina and gently applied to the cervix in the ante rior fornix. Pressure is applied until a satisfactory image is seen and then withdrawn slightly until the image starts to degrade. Excessive pressure from the transducer may falsely lengthen the cervix because of tissue compression. As a guide line, if the widths of the anterior and posterior cervix are equal, tissue compression is not likely significant. When the cervix is curved, a linear distance may underestimate the cervical length. In these cases, it is acceptable to esti mate the curved length using two linear segments. These landmarks are (1) the cervical/vaginal interface (marked by a border of increased echogenicity), (2) internal cervical os, (3) external cervical os, (4) full length of the cervical canal, and (5) outline of the cervix corpus. Imaging is considered adequate if at least three components are visualized, and an optimal image is one in which four or more components are visualized. In women at high risk for preterm birth, serial measurements significantly improve predictive accu racy. In this study, highrisk women with cervical length longer than 30 mm were seen every 2 weeks, but weekly measurements were performed if cervical length was less than 30 mm. As the cervix shortens, the fetal membranes increas ingly protrude in to the cervical canal, forming an enlarging funnel ("Y V"). Because funneling is a prominent feature of a short cervix, investigators asked whether the presence of a funnel has prognostic significance. The most common definition of a funnel is a minimum of 5 mm of dilated internal os. Several studies reported that the presence of a funnel confers increased risk of preterm birth independent of a short cervix. Dynamic changes can occur spontaneously or can be elicited by a provocative maneuver such as fundal pressure. When studied as an indepen dent risk factor for preterm birth, a poorly developed lower uterine segment appeared to be protective. Amniotic fluid sludge is found in 20% to 30% of women at high risk for preterm birth. In addition, among women at high risk for preterm birth, amniotic fluid sludge is an independent risk factor for intrauterine infection and preterm birth. Other Applicable Modality Cervilenz (Chagrin Falls, Ohio) is a disposable measuring probe with a movable flange to measure the distance from the lateral fornix to the distal end of the cervix. Two alternatives are available when a short cervix is seen in the second trimester: progesterone supplementation and cer clage. Bed rest is commonly recommended, although ran domized controlled trials do not support its effectiveness for singleton or twin gestations. Progesterone Supplementation for a Short Cervix Success with progesterone supplementation in women with a prior history of preterm birth prompted trials of progesterone supplementation in women with a short cervix because a short cervix is a more common anteced ent of preterm birth than a history of preterm birth. One capsule was placed in the vagina every night and continued until 33 weeks, 6 days. Progesterone supplementation was also associated with decreased incidence of treatment for neonatal sepsis (rela tive risk 0. In a sec ondary analysis of progesterone supplementation for a history of preterm birth, vaginal progesterone gel (8%, 90 mg of natural progesterone) was associated with decreased incidence of preterm birth at less than or equal to 32 weeks when the cervix was less than 28 mm com pared with greater than or equal to 28 mm. There are several unanswered ques tions, however, because mechanisms are not yet elucidated. The optimal progesterone formulation, route of administra tion, and progesterone dose all remain to be determined. In addition, longterm followup of newborns exposed to in utero progesterone is needed. Cerclage for a Short Cervix the recognition that cervical length is inversely associated with risk of preterm birth4 prompted investigators to ask whether a cerclage could change the natural history of cer vical shortening and delay preterm birth. The primary outcome variable was preterm birth before 35 weeks, which was seen in 32% of the cerclage arm and 42% of the expectant management arm (odds ratio 0. When the analysis was stratified by cervical length, cerclage benefit was significant when cervical length at randomization was less than 15 mm (P =. Secondary perinatal outcomes revealed cerclage was associated with decreased previable birth (P =. Supplemental progesterone appears to be ineffective,34 and cerclage may cause harm. More work is needed to improve clinical out comes for this highrisk patient population, and experts differ in their approach to this problem-along a spectrum from not evaluating cervical length, to a single evaluation in the second trimester, to serial assessment of cervical length. Although progesterone and cerclage seem harmful or ineffective, as opposed to these interventions for single tons, evaluation may lead to subsequent risk assessment, such as fetal fibronectin testing, and possibly improve neonatal outcomes by transferring the patient to an appro priate tertiary center or timely administration of steroids for accelerated fetal lung development. Interventions for a short cervix (<25 mm and definitely <15 mm) in singletons include cerclage or progesterone supplementation, or both, and referral to a center experienced in counseling about these therapies should be considered. There is evidence that cerclage for cervical shortening in twins is harmful and little evidence to suggest progesterone supplementation is helpful, and the benefit of cervical length monitoring in multiple gestation is unclear. Transabdominal cervical length measurement, albeit more technically difficult and less accurate, may be a reasonable initial examination. The optimal timing of cervical evaluation has not been determined; one reasonable approach is measurement every 2 weeks from 16 to 22 6 weeks; another is to increase screening to weekly screening if the cervix shortens to less than 30 mm. Treatments for a short cervix include vaginal micronized progesterone or cerclage. The role of cervical length screening in twin gestations is unclear because neither progesterone nor cerclage has been shown to prevent preterm birth in clinical trials.
A year later gastritis symptoms in spanish motilium 10 mg otc, he reported brief episodes of word finding difficulties on a daily basis gastritis ibs diet purchase motilium 10 mg line. Cerebral cavernous malformation gastritis symptoms acute cheap motilium 10 mg with amex, also known as cavernous angioma or cavernoma digestive gastritis through diet motilium 10 mg visa, is characterized by an abnormal cluster of blood vessels embedded in normal brain tissue and enclosed in a capsule gastritis diet èç buy motilium toronto. Cavernous malformations account for approximately 5% to 13% of all vascular malformations. They lack the high flow arterial feeders and draining veins of typical arteriovenous malformations. There is no neural tissue in these walls but the periphery is surrounded by a pseudocapsule of gliotic brain. Cavernous malformations are often small, but may enlarge due to recurrent bleeding and clot organization. The lesion has a "popcorn" or "honeycomb"appearance, which is characteristic of a cavernous malformation. It is speculated that the breakdown products caused by repeated microhemorrhages deposit ferric iron in to the surrounding cortex, which is epileptogenic. The mixed signal intensity within the center represents small hemorrhages of different ages, and the surrounding rim represents hemosiderin in the surrounding cortex. Angiography is rarely necessary because the lesions do not have high flow arterial feeders or anomalous drainage, and are usually not shown. The reported incidence of hemorrhage varies from 8% to 37% in adults in different series. However, the risk of hemorrhage overall is believed to be relatively small, varying from 0. The risk of hemorrhage is cumulative over the life expectancy of the patient, and is therefore of more concern in younger patients. The location of the lesion in the vicinity of an eloquent cortical region such as the language areas of the brain and its association with another venous anomaly are associated with increased surgical risks including residual neurological injury and venous infarction. He successfully underwent surgical excision of the lesion without persistent complications. Patent foramen ovale and cavernous angiomas are often incidental findings unrelated to the clinical syndrome. Cavernomas are abnormal clusters of sinusoidal capillaries embedded in normal brain tissue. Hemorrhage can be recurrent, but blood is usually contained within the capsule of the lesion. Because of increasing angina he had coronary angiography that showed severe 3-vessel coronary artery disease. After surgery he was slow to awaken and when he did stir he became hyperactive and has been given increasing doses of haloperidol. Atorvastatin (given in 80 mg/evening dose preoperatively) had not been restarted after surgery. He moves his right arm and both legs more than his left arm and deep tendon 151 reflexes are exaggerated on the left. A slightly larger infarct involves the parasylvian right cerebral convexity surface. When patients develop rebound hyperactivity on withdrawing from haloperidol, physicians unfortunately often prescribe an even higher dose. In my opinion haloperidol should never be used in older patients, especially in those with neurological abnormalities. The one indication is hemiballism when other measures do not control the violent motions. Cessation of statins can lead to a rebound increase in the likelihood of cardiac and brain ischemic events. I prescribed beginning again atorvastatin 80 mg/day given through his nasogastric tube. Decreased ventricular and atrial contractility and postoperative atrial fibrillation are important causes of stroke. The most important risk factor for stroke after cardiopulmonary bypass surgery is aortic atheromas. Low mean arterial blood pressure and prolonged bypass time increase the likelihood of the patient developing strokes and encephalopathy postoperatively. Preoperative transesophageal echocardiography can detect atrial and ventricular dysfunction and can localize and quantify the presence of aortic plaques and protruding atheromas. At times the numbers of microemboli are so numerous that a "white out" of emboli occurs. When severe aortic atherosclerosis is detected preoperatively or even at surgery using a hand-held Doppler, a number of alternatives arise: using "off-pump" surgery, pump-assisted bypass without cross-clamping the aorta, clamping at a location relatively free of disease, or instituting a filter placed in the aorta to catch embolic debris. Cessation of haloperidol resulted in the patient awakening rather completely and rapidly. Examination after awakening revealed a very slight left hemiparesis and poor memory and visual-spatial functions. A transesophageal echocardiogram showed regions of decreased ventricular mobility, an ejection fraction of 35%, and a very atherosclerotic aorta with protruding plaques. Antiplatelet therapy was also reinstituted, but there seemed not to be an indication for prophylactic anticoagulation. Economic concerns have led payors to dictate that patients having elective coronary artery bypass surgery be admitted to the hospital on the day of surgery. Although most have had coronary artery angiography, many have not had an adequate assessment of atrial and ventricular function, or echocardiographic study of their hearts and their aortas for the presence of thrombi and aortic atheromas. The most common cause of strokes and encephalopathy after coronary artery bypass surgery is embolization from atherosclerotic aortic atheromas. Thorough evaluation including a history of transient ischemic attacks and strokes, and studies of cardiac function and aortic atherosclerosis should precede elective coronary artery bypass surgery Strategies for surgery-on-pump vs. Comparison of transcranial Doppler ultrasonography and transesophageal echocardiography during coronary artery bypass surgery. He was unable to provide a cogent history but was recognized by staff from prior evaluations. Previous medical history was notable for hypertension, cirrhosis due to chronic alcohol use, alcohol intoxication with withdrawal seizures, tobacco use, and medication noncompliance. He had superficial abrasions and ecchymoses on his left forehead, volar surfaces of his hands, and right elbow. Abdomen was slightly tender in the left upper quadrant but without rebound tenderness. Spontaneous speech was sparse, as the patient indicated that he was "feeling sick. Sensation was intact and he did not extinguish to double simultaneous stimulation. Serum chemistries were suggestive of acute kidney injury with a serum creatinine of 1. After initiation of vancomycin, the patient defervesced and began to improve clinically. As epidemiology and culprit organisms evolve, atypical presentations, often subtle in early stages, make diagnosis a challenge. As stroke or other systemic embolization are the feared complications, the importance of an early diagnosis cannot be overstated. The Duke criteria, among others used, incorporate historical factors, clinical examination findings, and diagnostic tests, chiefly echocardiography. The sine qua non of endocarditis is the presence of cardiac valvular vegetations on echocardiography. Often, the transesophageal approach, particularly for adequate view of posterior leaflets and small vegetations, proves more sensitive than transthoracic approach. Epidemiologically the mitral valve, followed by aortic, tricuspid and pulmonic valves are most often affected. The microbiology of endocarditis has implications not only in choosing appropriate antimicrobial therapy but also in predicting the likelihood of systemic complications as well as to identify organisms associated with atypical presentations. A subset of patients with endocarditis will harbor difficultto-culture organisms, usually gram negative bacilli Haemophilus species. Endocarditis is a relatively uncommon cause of stroke, but stroke in patients with endocarditis is fairly common, clinically apparent in over 1/3 of patients but asymptomatically present in another 50%. Larger vegetations, ones on the mitral and to less extent aortic valve, and ones from Staphylococcus aureus carry higher risks. Smaller or streptococcal vegetations still can cause emboli, as can vegetations in the right heart. However, in embolic stroke from endocarditis, anticoagulation is not routinely given, because of the increased risk of hemorrhage. Likewise, antiplatelet agents are unlikely to confer additional benefit but will increase hemorrhagic risk (albeit less than anticoagulation). Risk with anticoagulation is further increased by the possibility of the rare complication of a mycotic aneurysm-arterial wall erosion and dilatations from invasion of infective agent. Additionally, in patients with embolization (whether cranial or systemic), screening for occult embolization after initiation of antimicrobial therapy can be useful. Recurrent infarction several days after the initiation of appropriate antimicrobial therapy is an indication for valvular surgery as it suggests medical failure. Cerebral hemorrhage or vascular imaging that suggest aneurysm formation requires a formal angiogram for diagnosis and possible treatment of a mycotic aneurysm. Recurrent embolization after initiation of appropriate antimicrobial therapy is an indication for consideration of valvular surgery. Infective endocarditis due to Staphylococcus aureus: deleterious effect of anticoagulant therapy. She had coronary angiography that revealed severe 3-vessel coronary artery disease. Before the procedure the surgeon noted a left carotid bruit and ordered an ultrasound examination of the neck arteries. The Doppler examination was consistent with 60% stenosis of the left internal carotid artery and less than 30% stenosis of the right. Patients who have stroke after surgery have longer hospitalizations and a higher risk of long-term disability. The mechanism of the majority of perioperative strokes is embolism from the heart or aorta. Risk factors for perioperative stroke include advanced age, history of hypertension, congestive heart failure, diabetes, and peripheral vascular disease. Aortic atherosclerosis is a major risk for perioperative stroke and encephalopathy. It is important to identify patients with symptomatic disease and those in whom carotid artery disease has caused strokes shown by brain imaging. Patients with asymptomatic carotid artery stenosis are often identified preoperatively by auscultation of a carotid bruit. The presence of a carotid bruit does not correlate with the degree of underlying stenosis nor does it correlate with the risk of perioperative stroke. Carotid bruits are associated with long-term risk of stroke during the following years. Often the stroke is in a territory incongruent with the affected vessel, suggesting that the presence of a bruit is a marker for atherosclerosis and stroke risk in general. In contrast to patients with symptomatic carotid artery stenosis, the reported risk of stroke in patients with asymptomatic carotid disease has varied widely, with some studies showing an increased risk while others have not. This discrepancy is largely due to the varying nature of the studies that have addressed this issue, and so uncertainty as to the significance of asymptomatic carotid stenosis remains. Contralateral carotid artery occlusion may be a risk factor for perioperative stroke but is not amenable to revascularization. Most perioperative strokes are not preventable by revascularization as they are attributable to causes other than carotid stenosis. Time is better directed toward evaluating patients for aortic atherosclerostic and poor cardiac function, as these are more common sources of embolism. Based on these findings, the panel concluded that there is no evidence to declare a superior approach. The most common mechanism of perioperative stroke in patients with carotid stenosis is embolism from the heart or aorta. Perioperative stroke is most often recognized after a delay from anesthesia recovery. Continuing controversy in the management of concomitant coronary and carotid disease: an overview. A systematic review of outcomes in patients with staged carotid artery stenting and coronary artery bypass graft surgery. Determination of etiologic mechanisms of strokes secondary to coronary artery bypass graft surgery. Type 1B (idiopathic) diabetes mellitus results from non-autoimmune destruction of beta cells, and evidence of autoimmunity cannot be demonstrated. Type 1A diabetes typically presents with acute symptomatic hyperglycemia and diabetic ketoacidosis. According to the 2009 American Diabetes Association Standards of Care,1 a random blood glucose level 200 mg/dL with signs and symptoms of diabetes, a fasting blood glucose of 126 mg/dL, or a glucose of 200 mg/dL after an oral glucose tolerance test all make the diagnosis of diabetes mellitus (Table 1. Hemoglobin A1c has been discussed as a method to diagnose diabetes in nonpregnant individuals. An expert panel of the American Diabetes Association recommends that an A1c value of 6. The panel specifically mentions that type 1 diabetes, with its usual classic clinical onset in children and adolescents, should continue to be diagnosed clinically, and that A1c testing can be used in the absence of specific clinical conditions. As typical type 1A diabetes usually presents with an acute onset of hyperglycemia, the A1c may not reflect the current acute hyperglycemia. Caution must be used in interpreting the A1c level, which may have limitations in certain settings, such as the presence of blood loss, transfusion, hemoglobinopathies, and age-related increases.
References
- Azua Blanco J, Azua Romeo J, Ortego J, Perez Cacho MJ. Cytologic features of pulmonary hamartoma. Report of a case diagnosed by fine needle aspiration cytology. Acta Cytol 2001;45(2):267-70.
- Yeung JY, Eschenbacher MA, Pauls RN: Pain and embarrassment associated with urodynamic testing in women, Int Urogynecol J 25:645n650, 2014.
- Graves JA, Wakefield MJ, Toder R: The origin and evolution of the pseudoautosomal regions of human sex chromosomes, Hum Mol Genet 7:1991n1996, 1998.
- Wu HY, Snyder HM 3rd: Pediatric urologic oncology: bladder, prostate, testis, Urol Clin North Am 31(3):619n627, xi, 2004.
- Chilian WM, Harrison DG, Haws CW, et al: Adrenergic coronary tone during submaximal exercise in the dog is produced by circulating catecholamines. Evidence for adrenergic denervation supersensitivity in the myocardium but not in coronary vessels, Circ Res 58:68, 1986.