Steven M. Smith, PharmD, MPH, BCPS
- Assistant Professor of Pharmacy and Medicine, Departments of Pharmacotherapy & Translational Research and Community Health & Family Medicine, Colleges of Pharmacy and Medicine, University of Florida, Gainesville, Florida

https://pharmacy.ufl.edu/profile/smith-steven-1/
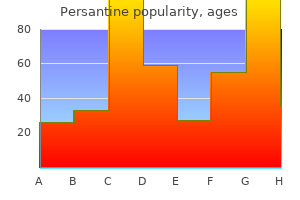
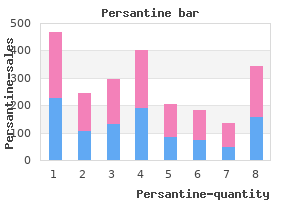
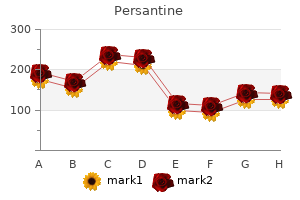
Thus section 8 medications order persantine 100 mg with mastercard, if signs or symptoms of these arc present medications knowledge buy 100 mg persantine otc, appropriate evaluation is indicated treatment for plantar fasciitis buy persantine online pills. Common to these conditions medications that raise blood sugar persantine 25mg low price, insulin resistance with compensatory hypcrinsulinemia is thought to promote the skin thickening of acanthosis nigricans medicine cat herbs buy persantine with a mastercard. Insulin binds to insulin-like growth factor receptors and leads to keratinocyte and dermal fibroblast proliferation (Hermanns-Le, 2004). However, weight loss can ameliorate insulin resistance, which may lead to plaque improvement. In those prescribed metformin for glucose control, improved acanthosis nigricans has been demonstrated (Romo, 2008). Last, topical vitamin D analogs such as calcipotrienc can promote plaque improvement (Bohm, 1998). Aphthous Uleers Nearly 25 percent of women in the second and third decade of life will experience these self-limited mucosal lesions. Classically found on nonkeratinized oral mucosa, aphthous ulcers may also develop on vulvovaginal surfaces. Histologically, aphthous ulcers show a mononuclear infiltrate with a fibrin coating. Although the etiology is unknown, immune-mediated epithelial cell damage is one theory (Rogers, 1997). Other described triggers include stress, trauma, infection, hormonal fluctuation, and nutritional deficiencies of vitamin B12, folate, iron, or zinc (Torgerson, 2006). Diffuse areas of increased pigmentation are usually encountered on the labia minora and fuurchette. However, this may also be seen with pigment variation of chronic inflammatory dermatoscs. These include benign mdanosis, lentigincs, cherry hemangiomas, angiokeratomas, and scborrheic keratosis (Heller, 2013). Knlfe<ut ulcers fn the labfocrural folds and perineum are commonly seen with vulvar Crohn disease. The four manfutation type& are vulvar edema (usually asymmetric), ulceration, hyperttophic lesiona, and chronic abscesses (Banet, 2014). Surgery often can be avoided or delayed with appropriate vulvar care, nutrition, and close collaboration with a ga. As a fast resort, excision of fistulous tracts and other refractory lesions or vulvectomy is an option. These warrant close surveillance as more than half of all melanomas arise from prcexisting nevi (Kaufinan, 2005). Common nevi are classified into three groups: junctional, compound, and dermal, depending on whether the melanotic nevus cells are located at the epidermis-dermis junction, extend into the dermis, or evolve over time to reside entirely within the dermis. Dermal nevi may appear bluish or have normal skin coloration depending on the depth of the nevu. The American College ofObstetricians and Gynccologists (2016a) recommends biopsy of all such lesions. Namdy, asymmetry, uneven pigmentation, irregular border, diameter >5 mm, or erosion or fissuring merits biopsy (F. Atypia or anatomically challenging biopsies, such as those near the clitoris, may prompt referral to clinicians with spc<:ialiu:d knowledge and experience with these lesions. Small, bland nevi that are not biopsied warrant a careful descriptive or photographic entry into die medical record and surveillance at least annually until the lesion is deemed stable. Beh~et disease is characterb:ed by mucocutaneous lesions (ocular, oral, and genital) and associated systemic vasculitis. Oral and genital ulcers appear similar to aphthous ulcers and generally heal within 7 to 10 days. The exact etiology of Beh41et disease remains unknown, although genetic and autoimmune etiologies are suspected. Accordingly, fur those suspected of Beh~t disease, referral to a rheumatologist fur additional testing and treatment is recommended. No race or ethnicity has greater risks fur vitiligo, but the disease may be more disfiguring and distressing fur darker. Although the etiology remains unknown, genetic factors are most likely (Zhang, 2005). Approximately 20 percent of patients have at least one affi:cted first-degree relative. The larger vulvar acrochordon shown here was exdsed due to mechanlcal symptoms fi"om Its size. Autoimmune diseases such as Hashimoto thyroiditls, Graves disease, diabetes mcllirus, rheumatoid anhritis, psoriasis, and vulvar lichen sderosus are associated with vitiligo (Boissy, 1997; Vrijman, 2012). Sometimes confused with the epithelial changes seen with lichen sc:lcrosus, vitiligo preserves normal skin texture and contour and is otherwise asymptomatic. No cure is presently available for vitiligo, and spontaneous rcpigmenution is rare. Less commonly, malignant lesions arise on the vulva and arc typically of squamous cdl epithelial origin. They are mistaken for vulvar condylomata, and therapeutic unresponsiveness by presumed genital warts should prompt removal fur histologic analysis. Acrochordons have been linked to diabc-tes mcllitus, and insulin-mediated fibroblast proliferation may explain this relationship Dcmir, 2002). Rarely developing on the vulva, lesions begin as 6nn, round papules that progress to a dome-shaped nodule with a central crater. Unucatcd, the lesion usually spontaneously regresses within 4 to 6 months and leaves only a slightly depressed scar. Nevertheless, its histofogic resemblance tD this cancer merits surgical c:xcision in most cases with a 4. The clinical appearance of vulvar syringoma is not pathognomonic, thus vulvar punch biopsy will establish the diagnosis and exclude malignancy. Film:nna is a benign tumor rarely arising from deep vulvar connective tissue by fibroblast proliferation. Larger lesions often become pedunculatcd with a long stalk and may cause pain or dysparcunia. Surgical excision is indicated for symptomatic lesions or if the diagnosis is unclear. This chronic vulvar mass grew slightly during pregnancy and then dramatically enlarged 3 days following an uncomplicated vaginal birth. Histologic evaluation following excision shows glands typical of breast tissue (arrow). Thus, complete dissection can require a larger incision and can be complicated by bleeding. Em>pic brtart tisnu may develop along the theoretical milk lines, which extend bilaterally from the axilla through the breast to the mons pubis. Importantly, these typically soft masses may also dcvdop breast pathologies including fibroadcnoma, phyllodcs rumor, Paget disease, and invasive adenocarcinoma. On physical examination, cysts typically are unilateral, round or ovoid, and Buctuant or tense. Small, asymptomatic Bartholin gland duct cysts require no intervention e:xcept exclusion of neoplasia in women older than 40 years. These include incision and drainage (I&: D), marsupialization, and Banholin gland excision, which are described and illustrated in Chapter 43 (p. These tend to dcvdop in populations with demographic profiles similar to those at high risk for sexually transmitted infections (Aghajanian, 1994). Esehtrichi4 coli is the most common isolate, but other gram-positive and gram-negative acrobcs and anaerobes are found (Kcssous, 2013; Mattila 1994; Tanaka, 2005). Given the rarity of these cancers, Bartholin gland excision is typically not indicated. Although histologically similar and lined by squamous epithelium, it is unclear if they represent separate entities. However, epidcrmoid cysts can also follow traumatic implantation of epidermal cells into deeper tissues and are filled with keratin. Epidermal inclusion cysts are variably sized, are typically round or ovoid, and are skin colorcd, yellow, or white. Grossly, cysts are usually filled with viscous, gritty, or caseous foul-smelling material. In distinction, pmistmt vuJvar pain is attributable to a specific condition (see Table 4-6). From limited studies, the prevalence of vulvodynia in the general population i& 3 to 11 percent (Lavy, 2007; Reed, 2004, 2014). One study e&timated that each year I in 50 women will devdop vulvodynia (Reed, 2008). The underlying cause of vulvodynia is multifactorial and varies among individuals (Stockdale, 2014). Potential factors associated with vulvodynia include other pain syndromes, genetic in8uenccs, hormonal factors, in8ammation, musculoskdetal dygfunction, neurologi. Ultimately, identification of these aasociated factors will guide individualized treatment planning. Subsequently, the wooden stick is broken to form a sharp point to retest the same areas. Pain scale scores of mild, moderate, or severe are recorded and followed over time. Diagnosis and treatment ddays, often by multiple providers, are common (Harlow, 2003, 2014). An evidence-based approach to diagnose vulvodynia and its associated factors is essential (Haefner, 2005; Stockdale, 2014). As noted, vulvodynia is categorized as spontaneous (unprovoked), triggered by physical pressure (provoked), or mixed. Sensations may be constant, intermittent, or episodic with exacerbations noted premenstrually (Arnold, 2006). Vulvodynia is described variably as burning, rawness, itching, or cutting pain within affected areas (Bergeron, 2001). These may include irritable bowd syndrome, interstitial cystitis, painful bladder syndrome, fibromyalgia, and mood or posttraumatic stress disorders. A history of recurrent infectious diseases such as herpes simplex or roster is sought. A sexual history may reveal clues of past or current abuse, unfavorable coital patterns, female sexual dysfunction, rdationship disharmony, and contraceptive modalities that could provoke vulvodynia (Chap. Additionally, clinicians inquire about recurrent candidiasis; prior genital trauma, including childbinh-rdated injuries; and current hygiene practices. Specifically, questions regarding genital shaving, type of undergarment fabric worn, and use of products in Table 4-1 can be hdpful. Inspection of the external vulva for lesions or irritation is followed by examination of the vestibule looking for focal, usually mild, erythema at vestibular gland openings. Use of a magnifying lens is imponant, and directed biopsies of nonerythematous epithdial changes may be hdpful. However, due to the lack of well-designed randomized trials, no specific therapy for vulvodynia demonstrates superiority. Often, a combination of several therapeutic options is required to relieve symptoms (Haefner, 2005; Landry, 2008). Approaches are described funher by Stockdale (2014) and the American College of 0 bstetricians and Gynecologists (2016b). Also, provision of accurate medical information can hdp resolve some patient concerns and questions associated with vulvodynia. Compared with the general population, no differences in marital contentment or psychologic distress are found (Bornstein, 1999). That said, education regarding foreplay, sexual positions, lubrication, and alternatives to vaginal intercourse are offered if potentially hdpful. Female sexual dysfunction and its treatment are funher discussed in Chapter 14 (p. Back pain, pdvic floor muscle spasm, or vaginismus may be the underlying cause of vulvodynia. A physical therapist familiar with treating these concerns may provide internal and external massage, myofascial release techniques, acupressure, joint manipulation, electrical stimulation, therapeutic ultrasonography, and pdvic floor muscle retraining to improve symptoms (Bergeron, 2002). Dietary oxalates excreted into urine have been suggested to aggravate symptoms, but evidence is limited and shows contradictory results (Baggish, 1997; Harlow, 2008). Similarly, support for supplementing with calcium citrate to balance the urine oxalates is scarce (Solomons, 1991). Nonsurgical Vulvodynia Treatment Vulvar care Topical agents Anti depressant See Table 4-2 2% lidocaine jelly or 5% lidocaine ointment, apply precoitally Gabapentin 2% to 6% ointment or cream, apply two or three times daily Amitriptyline, initially 5-25 mg orally daily, then increase daily dose by 10-25 mg each week. May increase to 60 mg daily Gabapentin, 100 mg orally three times daily and gradually increase as needed over 6-8 weeks.
Patients with neuroglycopenia after gastric bypass surgery have exaggerated incretin and insulin secretory responses to a mixed meal medications ranitidine purchase generic persantine on line. Hyperinsulinemic hypoglycemia after gastric bypass surgery is not accompanied by islet hyperplasia or increased beta-cell turnover symptoms juvenile rheumatoid arthritis purchase persantine once a day. Incretin hypersecretion in post-gastric bypass hypoglycemia-primary problem or red herring Blockade of glucagon-like peptide 1 receptor corrects postprandial hypoglycemia after gastric bypass medications ranitidine 100 mg persantine fast delivery. Laparoscopic reversal of Roux-en-Y gastric bypass: technique and utility for treatment of endocrine complications medications similar to adderall buy persantine 25 mg mastercard. Hypoglycemia due to an insulin binding antibody in a patient with an IgA-kappa myeloma symptoms 2 days before period quality 25 mg persantine. Clinical course of the syndrome of autoantibodies to the insulin receptor (type B insulin resistance): a 28-year perspective. Pathogenesis of hypoglycemia in insulinoma patients: suppression of hepatic glucose production by insulin. Nuclear medicine in the detection and management of pancreatic islet-cell tumours. Endoscopic ultrasonography-a sensitive tool in the preoperative localization of insulinoma. Intraarterial calcium stimulation and intraoperative ultrasonography in the localization and resection of insulinomas. Selective arterial calcium stimulation and hepatic venous sampling in the evaluation of hyperinsulinemic hypoglycemia: potential and limitations. Everolimus in the treatment of patients with advanced pancreatic neuroendocrine tumors: latest findings and interpretations. Re-evaluating "transitional neonatal hypoglycemia": mechanism and implications for management. Aerobic glycolysis in the human brain is associated with development and neotenous gene expression. Recommendations from the Pediatric Endocrine Society for evaluation and management of persistent hypoglycemia in neonates, infants, and children. The fasting test in paediatrics: application to the diagnosis of pathological hypo- and hyperketotic states. New insights and new conundrums in neonatal hypoglycemia: enigmas wrapped in mystery. Clinical and molecular characterisation of hyperinsulinaemic hypoglycaemia in infants born small-for-gestational age. Clinical and molecular characterisation of 300 patients with congenital hyperinsulinism. Genotype and phenotype correlations in 417 children with congenital hyperinsulinism. Managing congenital hyperinsulinism: improving outcomes with a multidisciplinary approach. Characterization of hepatic and brain metabolism in young adults with glycogen storage disease type 1: a magnetic resonance spectroscopy study. Fasting hypoglycemia resulting from hepatic carnitine palmitoyl transferase deficiency. The study of monogenetic obesity syndromes in rodents and humans and the identification of human genetic variants that predispose to obesity have revealed key gene products and brain systems (such as the adipose-derived hormone, leptin, and the hypothalamic melanocortin system) that participate in the regulation of energy balance. Hypothalamic circuits mediate the long-term balance between energy intake and expenditure; hypothalamic nuclei that play important roles in energy homeostasis include the arcuate nucleus, the ventromedial nucleus, the dorsomedial nucleus, the paraventricular nucleus, and the lateral hypothalamic area. Brain regions such as the ventromedial nucleus, along with melanocortin circuits, also play a role in the central control of glucose homeostasis. Understanding the molecular and neural mechanisms that modulate rewarding aspects of feeding may reveal sites for therapeutic intervention in obesity. The brainstem has traditionally been considered to control short-term feeding by mediating the effects of gut-derived satiety signals, but the brainstem represents the likely site of action for several antiobesity medications that decrease food intake and body weight over the long term. Brainstem nuclei that contribute to the control of food intake include the area postrema, the nucleus of the solitary tract, the dorsal motor nucleus of the vagus, and the lateral parabrachial nucleus. Consuming more calories than one expends leads to the storage of excess energy (generally, in adipose tissue); chronically, such positive energy balance causes obesity. While often thought of as a cosmetic problem, obesity represents a major health concern that contributes to the development of diabetes, cardiovascular disease, and cancer (among other illnesses). It has long been understood that organic lesions within specific regions of the brain can cause obesity. Leptin Signals the Repletion of Adipose Stores Parabiosis (joining the circulatory systems of two animals to permit the exchange of hormones) between obese rats with medial basal hypothalamus lesions and nonlesioned rats led to starvation and weight loss in the latter, while parabiosis between two medial basal hypothalamus-lesioned rats did not alter energy balance in either animal. Coleman used mice homozygous for ob, a recessive allele that causes hyperphagia, decreased energy expenditure, endocrine dysfunction, and obesity, and for db, which lies at a different locus but produces a phenotype similar to that of ob. Parabiosis of lean (wild-type) mice with ob/ob mice suppressed weight gain in the ob/ ob mice, whereas parabiosis of wild-type and db/db mice caused profound hypophagia and weight loss in the wild-type mice. Cloning of the causative gene mutations in ob and db strains confirmed the predictions of these parabiosis studies: the gene mutated in ob encodes a hormone of the type 1 cytokine family (subsequently named leptin [from the Greek leptos, meaning "thin"]), while db affects the gene that encodes the leptin receptor (LepR), a member of the type 1 cytokine receptor family. Decreased leptin following caloric restriction initiates the neuroendocrine starvation response, increasing food-seeking and appetite and suppressing the expenditure of energy by neuroendocrine systems (resulting in infertility, decreased sympathetic nervous system tone, thyroid function, etc. Leptin also reverses the hyperphagia, obesity, and neuroendocrine dysfunction of rare human patients with congenital leptin deficiency. Indeed, leptin was recently approved for the treatment of lipodystrophy syndromes in humans. Hence the absence of leptin sends a more powerful physiologic signal than does its excess. Indeed, while low leptin clearly represents the crucial signal of energy deficit, leptin does not mediate the anorexia that follows forced overfeeding,35 suggesting the existence of a separate signal important for the suppression of food intake during nutritional surfeit. The Hypothalamic Melanocortin System In 1902, French geneticist Lucien Cuenot described the obese agouti mouse (Ay/a; also termed lethal yellow because homozygotes for the allele die prenatally) that had been bred for decades by European mouse fanciers. Thus the hypothalamic melanocortin system is crucial for the control of food intake and energy balance. Mice null for Pomc throughout the body or specifically in the arcuate nucleus are hyperphagic and weigh approximately twice as much as control animals in adulthood. In all extrapituitary tissues, posttranslational processing of the prohormone resembles that in the intermediate lobe. Hypothalamic processing is similar but not identical to that in the intermediate lobe. While some other sites play roles in the control of energy balance, Mc4r expression in the paraventricular nucleus is necessary and sufficient for the control of feeding. This obesity syndrome demonstrated that the central melanocortin circuitry subserves energy homeostasis in humans as it does in the mouse. Remarkably, the associated physical findings are virtually identical to those reported for the mouse,44 with increased adipose mass, increased linear growth and lean mass, hyperinsulinemia greater than that seen in matched obese control subjects, and severe hyperphagia. The products of many of the affected genes play important roles in peptide processing. The sites mediating melanocortin action on linear growth, lipid handling, and blood pressure are not defined. In addition, several hormones crucial for the regulation of food intake and metabolism. Several hypothalamic sites (including the arcuate nucleus, ventromedial nucleus, dorsomedial nucleus, paraventricular nucleus, and lateral hypothalamic area) play key roles in coordinating food intake and other parameters of energy homeostasis. The paraventricular nucleus mediates important outflow from the hypothalamus to brainstem centers that control food intake. In between, the dorsomedial nucleus integrates other signals and relays information to and from the arcuate and paraventricular nuclei. Chapter 39 Neuroendocrine Control of Energy Stores 1557 Orthologs of many of the genes that encode crucial mediators of energy balance and/or that underlie rodent obesity models also cause or contribute to obesity in humans. Furthermore, genome-wide association studies have identified over 100 single nucleotide polymorphisms significantly associated with body mass index, and these are predominantly located in or near genes thought to act primarily in the hypothalamus. Core "homeostatic" hypothalamic circuits are shown in red, brainstem circuits are in dark blue, peripheral signals are green, leptin receptor pathways are in orange, and melanocortin pathways are in light blue. Roles in leptin action have been examined for other circumscribed sets of hypothalamic LepRb neurons as well. Early embryonic ablation of LepRb in the ventromedial nucleus blunts energy expenditure and thereby increases adiposity,96 while deletion of LepRb in neurotensin-expressing lateral hypothalamic area neurons diminishes motor activity to blunt energy expenditure and increase adiposity. Ghrelin is unique in that it requires the addition of an eight-carbon fatty acid (octanoate) side chain to have agonist activity at the ghrelin receptor. A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Similarly, neither genetic deletion of ghrelin O-acyltransferase123 nor the ablation of ghrelin-producing cells124 results in major changes in food intake and body weight. Roles for the Paraventricular Nucleus in Energy Balance the metabolic consequences that result from abnormal paraventricular nucleus development or the interference with paraventricular nucleus function underscore the importance of the paraventricular nucleus in energy balance and autonomic function. Destruction of the paraventricular nucleus by electrolytic lesion causes hyperphagia and obesity. Melanocortin action in paraventricular nucleus neurons plays crucial roles in the control of food intake, energy balance, and glucose homeostasis. The paraventricular nucleus is composed of a heterogeneous group of glutamatergic neurons that have been classically described as parvocellular or magnocellular based on cell size and axonal projection patterns. Paraventricular nucleus parvocellular cells are neurochemically diverse and send projections within the central nervous system to three main areas: (1) the median eminence, where secreted factors. Paraventricular nucleus-mediated energy balance control is thought to be regulated predominantly by parvocellular paraventricular nucleus neurons. Thus oxytocin neurons (and their contents) are not required for anorectic melanocortin action, and other (nonoxytocin) paraventricular nucleus neurons play crucial roles in the control of feeding (including in response to melanocortin action). Deletion of paraventricular nucleus Mc4r results in hyperphagic obesity, whereas re-expression of Mc4r selectively in the paraventricular nucleus in an otherwise null Mc4r background normalizes feeding and dramatically attenuates the obesity phenotype of these mice. Role for the Ventromedial Nucleus in Energy Balance As noted earlier, medial basal hypothalamus lesion studies demonstrated that combined ablation of the arcuate nucleus and ventromedial nucleus produce obesity. Indeed, the ventromedial nucleus represents an important site for the modulation of sympathetic nervous system outflow. The Role of Insulin and Glucose in the Regulation of Energy Homeostasis In addition to the well-known role for insulin action on peripheral tissues to control glucose homeostasis, insulin acts in the central nervous system to contribute to the control of energy balance. Several distinct populations of neurons in the brain sense glucose164: some neurons are activated by rising concentrations of glucose (glucose-excited cells), while other classes of neurons are inhibited by rising glucose (glucose-inhibited cells). Estradiol replacement decreases food intake and increases energy expenditure in rodents, however,177 indicating that exogenous estrogens may influence both energy intake and energy expenditure. Energy expenditure is often grouped into three categories: energy required for basal metabolism, energy required for physical activity, and the thermic effect of food. The importance of sympathetic output in energy balance is revealed by the profound obesity of mice lacking all -adrenergic receptors when exposed to a high-fat diet. In humans the key tissue mediating energy expenditure in response to changing energy intake is likely skeletal muscle, although brown adipose tissue has been identified in humans and may play a role in energy balance control. Key mediators of central nervous system autonomic output are the parasympathetic and sympathetic preganglionic neurons in the brainstem and spinal cord. Different rostral-caudal levels of the intermediolateral column provide innervation to different target organs and thus mediate distinct autonomic responses. For example, sympathetic preganglionic neurons in the upper thoracic levels of the intermediolateral column are thought to be important for control of the heart and cardiovascular system. Additionally, sympathetic preganglionic neurons in thoracic levels T6 to T12 of the intermediolateral column provide innervation of the adrenal gland and endocrine pancreas. While the neuroanatomy and neural mechanism(s) by which this early brainstem lesion altered blood glucose remain somewhat obscure, several hypothalamic systems clearly play important roles in the control of glucose homeostasis. For instance, Lepob/ob mice exhibit hyperglycemia despite constitutively elevated insulin production. Similarly, lipodystrophic mice and humans exhibit severe insulin resistance that is corrected by leptin replacement. Ventromedial Nucleus Control of Glucose and Energy Homeostasis the ventromedial nucleus plays important roles in the regulation of the sympathetic nervous system and contributes to both hepatic glucose output and glucose disposal. Since the ventromedial nucleus contains both glucose-inhibited and glucose-excited neurons, pan-ventromedial nucleus manipulations reveal the aggregate function of all cell types within the ventromedial nucleus. Conversely, under fed conditions the neurons that promote glucose utilization play a dominant role in glycemic control; thus disrupting overall ventromedial nucleus function causes glucose intolerance and blunts energy expenditure to promote weight gain. Furthermore, low glucose activates orexin-producing neurons in the lateral hypothalamic area. Intersection of Energy Balance and Reward Circuits Behaviorally, two systems govern eating: the circuits that control the incentive and reward values (wanting and liking) of food and the satiety system, which promotes meal termination associated with the sensation of fullness. Overlapping central nervous systems mediate motivation for natural and artificial rewards. The mesolimbic dopamine system, composed of dopaminergic neurons in the ventral tegmental area that project to the nucleus accumbens and other places, play important roles in motivation and reward. Indeed, leptin suppresses the motivation of animals to perform rewarding brain self-stimulation,244 and subpopulations of ventral tegmental area neurons express LepRb or ghrelin receptor. Thus leptin action in the lateral hypothalamic area controls orexin cells and ventral tegmental area cells to modulate the mesolimbic dopamine system. Leptin likely controls melanin-concentrating hormone neurons via its action on the hypothalamic melanocortin system. Core components of the mesolimbic dopamine system are shown in light purple, brainstem circuits are in dark blue, leptin receptor pathways are in orange, and melanocortin pathways are in light gray.
A normal vasogram is documented when contrast agent is visualized throughout the length of the vas deferens treatment 02 binh 100mg persantine with visa, seminal vesicles medications via g tube best order persantine, ejaculatory duct and bladder atlas genius - symptoms discount 25mg persantine with mastercard. The important points in the history relate to his age abro oil treatment persantine 25mg low price, marital status medications not covered by medicare buy persantine without a prescription, number of previous children and the age of the youngest child, previous contraceptive history and previous surgery in the inguino-scrotal region. Also document whether both he and his partner have considered other contraceptive measures. As well as a general examination, the specific important points on examination will relate to the laxity of the scrotum, whether the vasa are easily palpable and whether there is any other scrotal pathology present (varicocele, tumour). This also helps to decide on whether to perform the procedure under a local or general anaesthetic. I would provide written information on the procedure and invite the partner to be involved in the decision-making process. I will explain why the procedure is being performed, what the alternatives are, what the success rate is and what complications may occur. Importantly, they must continue some form of contraception until the patient produces an azoospermic semen sample (see later discussion). I would explain that failure may occur early (1 in 300 due to surgical error) or late (1 in 2000 due to recanalisation). He fits one of the criteria where patients often change their mind or are dissatisfied. Other groups which require careful attention are young couples, couples with two or less children, patients from lower socio-economic classes and where there is the possibility that the operation is being requested for financial or emotional reasons or that the male may be ambivalent about it. I would provide a written patient information sheet and a copy of the written consent. I would ask for a period of time between the consent and the operation so that there is sufficient time for the patient to make a fully informed choice. What methods of vasal occlusion are you aware of and do they have different success rates Suture ligation is still the most common method employed worldwide but may result in necrosis and sloughing of the cut end. Recent evidence suggests the use of Vicryl is associated with a higher rate of failure as compared to catgut. Vasal occlusion using two medium haemoclips on each end results in failure rates of less than 1%. Intraluminal occlusion with needle electrocautery, or battery-driven thermal cautery set at a power sufficient to destroy mucosa but not high enough to cause transmural destruction of the vas, reduces recanalization rates to less than 0. Using this technique it is recommended that at least 1 cm of the lumen should be cauterized in each direction. Following informed consent and with the patient supine I would perform a vasectomy using a mixture of 1% plain Lidocaine and 0. I would perform the procedure in a warm room and with warm preparation solution to relax the scrotum. Each vas is isolated from the spermatic cord vessels and manipulated to a superficial position under the scrotal skin. The local anaesthetic is injected into the skin (in some patients a cord block at the start of the procedure can be performed) and then advanced into the peri-vasal sheath. Small bilateral transverse incisions through the dartos are performed until the vas sheath is seen and pulled though the incision. A longitudinal incision through the sheath is performed and the bare vas isolated using a vasectomy ring forcep. The vasal artery, veins and accompanying nerves are dissected free of the vas and spared. A 1 cm segment is removed between two haemostats from the straight part of the vas and sent for pathological confirmation. The ends are occluded by using intra-luminal cautery and the ends sutured in different fascial planes (fascial interposition). I use a bilateral incision technique as this reduces the chance of dividing the same vas twice and it is also easier to divide the vas on the straight segment with bilateral incisions. I use intra-luminal cautery and fascial interposition to reduce the incidence of vasectomy failure by re-canalisation. This reduces the number of false-positive samples and thus minimises both patient inconvenience and repeat laboratory assessment [3]. However, persistent non-motile spermatozoa in the initial ejaculates is not uncommon, with studies reporting up to 33% non-azoospermic samples at 3 months, and 10% of ejaculates containing non-motile sperm at 6 months. Discussion in the literature has suggested that the risk of pregnancy occurring from these non-motile sperm is small, and probably no more than the risk of pregnancy after two azoospermic semen samples, as a result of spontaneous recanalization. Using these criteria only 1 of 50 men examined at least 3 years after vasectomy had sperm in their analysis, the others being azoospermic. It is likely that he has had a late failure of vasectomy which is caused by re-canalisation. It is defined as the re-appearance of sperm after a documented semen analysis showing azoospermia. He needs to give a further semen analysis to make sure that this is the correct diagnosis. If late failure has occurred he should be offered a scrotal exploration, identification of the vasa and further occlusion bilaterally under a general anaesthetic. The patient should use alternate forms of contraception until he has had a further exploration and documented azoospermia. If the repeat sample shows azoospermia then they should be referred for a paternity test. However, there have been documented pregnancies despite the test showing azoospermia where the patient is the biological father. In the initial consultation, I would want to assess both the male and female partner with respect to their previous health and reproductive histories. I would examine the patient and assess the size and consistency of the testis and epididymis as well as whether the vasa and gap between the two cut ends are easily palpable. I would ask the patient to perform a semen analysis if it has not already been performed. Approximately 6% of men who have undergone a vasectomy will subsequently request a reversal. The reason most frequently given by men requesting a vasectomy reversal is divorce and remarriage with a desire to have children with their new spouse. This can be micro-surgical using an operating microscope, magnified vision using loupes or some will just use a macroscopic technique. There should be sufficient mobilization of both ends of the vas deferens to prevent any tension on the anastomosis. The perivasal adventitia must remain intact as stripping of the adventitia surrounding the cut ends of the vas risks excising an important blood supply to the vas and may lead to ischemia and ultimately stenosis of the anastomosis. Precise approximation of the cut lumens is mandatory to avoid sperm leakage with formation of a sperm granuloma that may disrupt the lumen and result in a failed procedure. With the patient supine, the cut ends of the vas deferens are brought through two bilateral scrotal incisions or a midline raphe incision. The vas is mobilised both proximally and distally allowing sufficient length for the freshly cut ends of the vas to slightly overlap one another once they are positioned for the anastomosis. When both vasa have been dissected free, the vasa are held in a vasectomy reversal clamp above skin level. The vas above and below the vasectomy site is then transected until a patent lumen is seen both proximally and distally. A few drops of fluid from the testicular end of the vas lumen are placed on a sterile glass slide and examined using a light microscope. If there are sperm or sperm parts (sperm heads, sperm with partial tails) with clear copious fluid then a vasovasostomy can be performed. A modified doublelayer technique is used with four to six interrupted 9-0/10-0 sutures passed through the lumen and mucosal layer followed by six interrupted 9-0 sutures through the muscularis and the adventitial layers. Unfortunately some patients will require a vasoepididymostomy rather than a vasovasostomy because of a secondary obstruction at the level of the epididymis. This appears to be a timerelated phenomenon; the longer the time interval is from the original vasectomy, the greater the chances of an epididymal obstruction. More recently a model to pre-operatively identify patients who may require vasoepididymostomy was created which is based on time since vasectomy and patient age. The predictive model provides 84% sensitivity for detecting patients who may require vasoepididymostomy during vasectomy reversal (58% specificity). This model more accurately predicts the need for vasoepididymostomy than using a specific duration from vasectomy cut-off alone. The decision to perform a vasoepididymostomy is based on the quality of fluid found in the proximal vas deferens at the time of surgery. When the material coming from the proximal vas lumen is thick and devoid of sperm 2. If a vasovasostomy is performed then the success rates (patency rate and pregnancy rate) varies depending on the interval from the vasectomy until its reversal (Table 13. This is based upon a large series of 1469 men who underwent microsurgical vasectomy reversal procedures who were studied at five institutions [4]. More recently, pre-operative factors have been associated with a successful outcome including the same female partner as well as a short obstructive interval. Intraoperative factors included the use of surgical clips rather than suture at vasectomy, the presence of sperm granuloma and the presence and quality of the vasal fluid. In a recent study using the microsurgical vasovasostomy technique it was reported that the pregnancy rate for couples with a female partner aged 40 or older was significantly lower than for those with the female partner aged 39 or younger (14% versus 56%). The age of the female partner is therefore important in the counselling process and it may not be costeffective to perform vasectomy reversals in couples with a female partner older than age 40. There is controversy as to whether the outcomes using microsurgery, loupes or macroscopic techniques are equally effective or not. However, most experts believe that the results of microsurgical vasectomy reversal are superior to results of non-microsurgical techniques in terms of patency and pregnancy. However, microsurgery requires more training and experience to obtain the best results. Patency and pregnancy rates do not appear to be significantly different if a multilayer anastomosis is performed as opposed to a modified single-layer technique but the success is physician dependent. He is upset that despite the post-operative tests showing sperm in the semen, his new partner has not been able to conceive. It is important to establish whether he does indeed have sperm in his semen or not and what the fertility potential of his partner is. A 36-year-old man is referred as an urgent 2-week wait referral with a 3-month history of haematospermia. He is now abstaining from sexual contact as his partner is suspicious that he may have a sexually transmitted infection. However, if it persists beyond several weeks patients should undergo further urologic evaluation as it can occasionally be a result of an underlying significant urological pathology. Other important features in the history include recent trauma, infection and a history of bleeding disorders. The penis needs to be examined to exclude any lesions that may bleed and contribute to the ejaculate and a thorough palpation along the course of the vas is required to ensure their presence and assess for dilatation (signifies distal obstruction). In younger men, urethritis should be considered in the differential diagnosis and urethral swabs should be obtained. Are there any features in the history which would suggest that the patient may require further evaluation If there is persisting haematospermia in a patient over the age of 40 especially if associated with haematuria, a cysto-urethroscopy is required. The most important goal in the management of these patients is reassurance if they have been fully investigated and no cause can be identified. In younger patients it is important to exclude infective causes and a referral to a genitourinary clinic is useful. In the history he says that he has a normal orgasm but complains that when he passes urine the first time after he ejaculates the urine is cloudy. A post-orgasm urine examination should be performed to look for the presence of sperm in the urine on light microscopy. Medical treatments can be used to try to close the bladder neck and prevent retrograde ejaculation. Sympathomimetics, such as pseudoephedrine and ephedrine, can help close 321 the bladder neck and enhance antegrade ejaculation. Imipramine, a tricyclic antidepressant that has mixed anticholinergic and sympathomimetic properties may also be used. How would you organise for the patient to provide an alkalinised post-ejaculate urine specimen Patients are instructed to alkalinise their urine by the ingestion of 1 g of sodium bicarbonate the night before and a further 1 g on the morning of the collection. They are then instructed to obtain the post-ejaculatory urine as quickly as possible after orgasm and deliver the sample immediately to the laboratory. Using this technique, the fertilization rate has been reported to be as high as 51% with 7 of 16 couples achieving clinical pregnancies and three live offspring delivered.

Comparison of coronary bypass surgery with angioplasty in patients with multivessel disease treatment quotes and sayings 25 mg persantine visa. Clinical diabetic cardiomyopathy: a twofaced disease with restrictive and dilated phenotypes medications emts can administer buy persantine 100mg otc. Mechanisms determining course and outcome of diabetic patients who have had acute myocardial infarction medications vs medicine buy persantine 100mg cheap. Quantitative comparison of extent of coronary narrowing and size of healed myocardial infarct in 33 necropsy patients with clinically recognized and in 28 with clinically unrecognized ("silent") previous acute myocardial infarction symptoms 6 weeks pregnant buy cheap persantine on line. A comparison of the pathological spectrum of hypertensive treatment xdr tb buy 100 mg persantine otc, diabetic, and hypertensive-diabetic heart disease. A comparison of ultrastructural changes on endomyocardial biopsy specimens obtained from patients with diabetes mellitus with and without hypertension. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. Maximal coronary flow reserve and metabolic coronary vasodilation in patients with diabetes mellitus. A systematic review of the effectiveness of revascularization of the ulcerated foot in patients with diabetes and peripheral arterial disease. The North-West Diabetes Foot Care Study: incidence of, and risk factors for, new diabetic foot ulceration in a community-based patient cohort. High levels of foot ulceration and amputation risk in a multiracial cohort of diabetic patients on dialysis therapy. Reduction in diabetes-related lower-extremity amputations in the Netherlands: 1991-2000. Causal pathways for incident lower-extremity ulcers in patients with diabetes from two settings. Clinical examination and non-invasive screening tests in the diagnosis of peripheral artery disease in those with diabetes related foot ulceration. Effectiveness of revascularization of the ulcerated foot in patients with diabetes and peripheral artery disease: a systematic review. Analysis of the elective treatment process for critical limb ischaemia with tissue loss: diabetic patients require rapid revascularisation. Comprehensive foot examination and risk assessment: a report of the task force of the foot care interest group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Semiquantitative analysis of the histopathological features of the neuropathic foot ulcer: effects of pressure relief. A randomized trial of two irremovable off-loading devices in the management of plantar neuropathic diabetic foot ulcers. Antibiotics versus conservative surgery for treating diabetic foot osteomyelitis: a randomized comparative trial. Systematic review of economic evaluations of human cell-derived wound care products for the treatment of venous leg and diabetic foot ulcers. Negative pressure wound therapy after partial diabetic foot amputation: a multicentre, randomised controlled trial. Comparison of negative pressure wound therapy using vacuum-assisted closure with advanced moist wound therapy in the treatment of diabetic foot ulcers: a multicenter randomized controlled trial. I atrogenic hypoglycemia is the limiting factor in glycemic management of diabetes mellitus with insulin provisional therapies: insulin, a sulfonylurea, or a glinide. Blood-to-brain glucose transport is a direct function of the arterial plasma glucose concentration and requires the plasma glucose concentration be maintained within, or above, the physiologic range. Hypoglycemia causes functional brain failure, which is typically corrected after the plasma glucose concentration is raised (Table 38. Rarely, it causes a fatal cardiac arrhythmia or, if it is profound and prolonged, brain damage and death. The definition of "low" is judgmental, but a plasma glucose concentration of less than 55 mg/dL (3. Documentation of Whipple triad is particularly important for the diagnosis of hypoglycemia in patients who do not have insulin-, sulfonylurea-, or glinide-treated diabetes because hypoglycemic disorders are uncommon in such individuals. Glucoregulatory failure resulting in hyperglycemia (diabetes mellitus) is discussed in Chapters 33 through 37; that resulting in hypoglycemia is discussed in the paragraphs that follow. Glucose may be stored as glycogen, or may undergo glycolysis to pyruvate, which can be reduced to lactate, transaminated to form alanine, or converted to acetyl coenzyme A (CoA). Acetyl CoA, in turn, may be oxidized to carbon dioxide and water through the tricarboxylic acid cycle, converted to fatty acids that can be incorporated into triglycerides, oxidized, or utilized for synthesis of ketone bodies (acetoacetate, -hydroxybutyrate) or cholesterol. Only liver and kidneys express glucose-6-phosphatase, the enzyme necessary for release of glucose into the circulation, at levels sufficient to permit substantial contributions to the systemic glucose pool. Many tissues express the enzymes required to synthesize and hydrolyze glycogen (glycogen synthase and phosphorylase, respectively). The liver and kidneys also express the enzymes necessary for gluconeogenesis, including the critical gluconeogenic enzymes pyruvate carboxylase, phosphoenolpyruvate carboxykinase, and fructose-1,6-bisphosphatase. The liver is the major source of net endogenous glucose production (through glycogenolysis and gluconeogenesis). Conversely, the liver can be an organ of net glucose uptake and glycogen synthesis. Muscle can take up and store glucose as glycogen, or metabolize glucose (through glycolysis) to pyruvate, which, among other fates, can be reduced to lactate or transaminated to form alanine. Lactate (and pyruvate) released from muscle can be transported to the liver and the kidneys, to serve as a gluconeogenic precursor (the Cori or glucose-lactate cycle). Alanine, glutamine, and other amino acids can also flow from muscle to liver and kidneys, where they also serve as gluconeogenic precursors. These constitute the glucose-alanine and glucose-glutamine cycles, in which new glucose formation is from precursors. Although quantitatively less important than muscle, fat can also take up and metabolize glucose. Glucose is essentially the sole metabolic fuel for the brain under physiologic conditions. The brain can utilize alternative fuels if their circulating levels rise high enough for them to enter the brain in quantity. For example, during extended fasting, markedly elevated circulating ketone levels can support the majority of the energy needs of the brain and reduce its utilization of glucose. Hypoglycemia occurs when rates of glucose appearance in the circulation (the sum of endogenous glucose production and exogenous glucose delivery from ingested carbohydrates) fail to keep pace with rates of glucose disappearance from the circulation (the sum of ongoing glucose metabolism largely by the brain and of variable glucose utilization by tissues including muscle, fat, liver, and kidneys). In healthy adults, the physiologic postabsorptive (fasting) plasma glucose concentration ranges from approximately 70 mg/ dL (3. These rates are as much as threefold higher in infants, at least in part because of their greater brain mass relative to body weight. The liver is the predominant source of endogenous glucose production in the postabsorptive state; the kidneys, which both utilize and produce glucose, contribute little to net glucose production. However, as in the liver, glucose production in the kidney is regulated; it is suppressed by insulin and stimulated by epinephrine but not by glucagon. As a result, net renal glucose production occurs under some conditions, including hypoglycemia. Gluconeogenesis and glycogenolysis are important for maintenance of the plasma glucose concentration. Therefore, in an adult of average size, preformed glucose can provide less than an 8-hour supply of energy, even at the diminished rate of glucose utilization that occurs in the postabsorptive state. If fasting is prolonged to 24 to 48 hours, the plasma glucose concentration declines and then stabilizes; hepatic glycogen content falls to less than 10 g (55 mmol), and gluconeogenesis becomes the sole source of glucose production. Because amino acids are the main gluconeogenic precursors that result in net glucose formation, muscle protein is degraded. As lipolysis and ketogenesis accelerate and circulating ketone levels rise, ketones become a major fuel for the brain. Glucose utilization by the brain declines by about half, which reduces the rate of gluconeogenesis required to maintain the plasma glucose concentration and hence decreases protein wasting. After a meal, glucose absorption into the circulation increases to more than twice the rate of postabsorptive endogenous glucose production, depending on the carbohydrate content of the meal, the rate of gastric transit, and the rate of digestion and absorption. As glucose is absorbed, endogenous glucose production is suppressed, and glucose utilization by muscle, fat, and liver accelerates. The exogenous glucose is assimilated and, after a small rise, the plasma glucose concentration returns to the postabsorptive level. Exercise increases glucose utilization (by muscle) to rates that can be several times greater than those of the postabsorptive state. Endogenous glucose production normally accelerates to match use so that the plasma glucose concentration is maintained. In summary, the plasma glucose concentration is normally maintained within a relatively narrow range despite wide variations in glucose flux and thus maintains the systemic glucose balance. This remarkable homeostatic feat is accomplished by an array of hormonal, neural, and substrate glucoregulatory factors. Increased secretion of glucose counterregulatory hormones, including glucagon and epinephrine, occurs as glucose levels fall just below the physiologic range. Lower plasma glucose concentrations cause a more intense sympathoadrenal (sympathetic neural as well as adrenomedullary) response and symptoms. Even lower glucose levels cause cognitive dysfunction and additional manifestations of functional brain failure including seizure or coma. Clinical Manifestations of Hypoglycemia the symptoms and signs of hypoglycemia are nonspecific. Ra, Rate of glucose appearance, glucose production by the liver and kidneys; Rc, rate of glucose clearance by insulin-sensitive tissues; Rd, rate of glucose disappearance, glucose utilization by insulinsensitive tissues such as skeletal muscle (no direct effect on central nervous system glucose utilization). They include cognitive impairments; behavioral changes; psychomotor abnormalities; and, at lower glucose levels, seizure and coma. They include adrenergic (catecholamine-mediated) symptoms such as palpitations and tremor, and anxiety/arousal and cholinergic (acetylcholinemediated) symptoms such as sweating, hunger, and paresthesias. Central mechanisms may also be involved in the generation of some of these symptoms. The mechanism(s) of the signaling of the glucose regulatory and counterregulatory hormone and sympathetic responses to hypoglycemia are not known. However, those responses are not mediated by a decrease in brain glucose metabolism because the glycemic threshold for a decrease in the cerebral metabolic role of glucose, measured with [11C]-glucose positron emission tomography, is at a lower plasma glucose concentration than the glycemic thresholds for the hormonal and sympathetic responses12 (see Table 38. Signs of hypoglycemia include pallor and diaphoresis, which result from adrenergic cutaneous vasoconstriction and cholinergic activation of sweat glands, respectively. Among the neurogenic symptoms, "sweaty," "hungry," and "tingling" are cholinergic, and "shaky/tremulous," "heart pounding," and "nervous/anxious" are adrenergic. Mechanism of awareness of hypoglycemia: perception of neurogenic [predominantly cholinergic] rather than neuroglycopenic symptoms. The first physiologic defense against hypoglycemia is a decrease in insulin secretion by the pancreatic islet beta cells. The second physiologic defense against hypoglycemia is an increase in glucagon secretion by pancreatic islet alpha cells. This increase occurs as plasma glucose concentrations fall just below the physiologic range (see Table 38. Indeed, the adrenergic actions on beta-cell insulin secretion normally play an important role in the glycemic actions of epinephrine. However, some increase in insulin secretion-due to the rising glucose level, 2-adrenergic stimulation, or both-limits the magnitude of the glycemic response to epinephrine. These physiologic interactions explain why glycemic sensitivity to epinephrine is increased in patients who cannot increase insulin secretion. If they do not, the lower plasma glucose concentration causes a more intense sympathoadrenal response, resulting in symptoms1,3 (see Table 38. Falling glucose levels within the Epinephrine Liver Pancreatic islets 2 Insulin Glucagon Muscle Fat 1, 2 ( Clinical Hypoglycemia Definition and Diagnosis Clinical hypoglycemia is, by definition, a plasma glucose concentration low enough to cause symptoms or signs, including impairment of brain function. Therefore, it is not possible to state a single plasma glucose concentration that categorically defines hypoglycemia. Furthermore, the symptoms and signs of hypoglycemia are nonspecific, and a low measured plasma glucose concentration can be artifactual. For all of these reasons, hypoglycemia is most convincingly documented by Whipple triad1,2 (see Table 38. Documentation of Whipple triad is particularly important when hypoglycemia is suspected in a person who does not have diabetes mellitus, because hypoglycemic disorders are rare. In the absence of diabetes, a thorough diagnostic evaluation is recommended only for patients in whom Whipple triad can be documented. It is also important to recognize that glucose concentrations measured in whole blood are approximately 15% lower than those in plasma and may be further reduced if the hematocrit is high. Clinical Classification of Hypoglycemia Causes of hypoglycemia2 are outlined in Table 38. Although persons with diabetes can suffer from the same hypoglycemic disorders as those without diabetes, their hypoglycemic episodes are usually the result of treatment of their diabetes. Furthermore, the pathophysiology of hypoglycemia in diabetes is unique, and the diagnostic and management approaches are different from those for individuals without diabetes. Therefore, hypoglycemia in persons with diabetes and hypoglycemia in those without diabetes are discussed separately in this chapter. The barrier of hypoglycemia generally precludes maintenance of euglycemia over a lifetime of diabetes and thus full realization of the vascular benefits of glycemic control. Furthermore, hypoglycemia compromises physiologic and behavioral defenses against subsequent falling plasma glucose concentrations, resulting in a vicious cycle of recurrent hypoglycemia. Hypoglycemia in diabetes is caused by pharmacokinetically imperfect treatment with insulin or an insulin secretagogue.
Buy genuine persantine on line. What are the symptoms of MS?.
References
- Weiss W, Levin R, Goodman L. Pleural plaques and cigarette smoking in asbestos workers. J Occup Med 1981;23:427-30.
- Hammond EC, Selikoff IJ, Seidman H. Asbestos exposure, cigarette smoking and death rates. Ann N Y Acad Sci 1979;330:473-90.
- Josefson D. Herbal stimulant causes U.S. deaths. BMJ 1996;312:1378.
- Riley B. Strategies for ventilatory support. British Medical Bulletin Trauma 1999;55(4):806-20.