Linda Shore-Lesserson, MD
- Professor of Anesthesiology
- Chief, Cardiothoracic Anesthesiology
- Montefiore Medical Center
- Bronx, New York
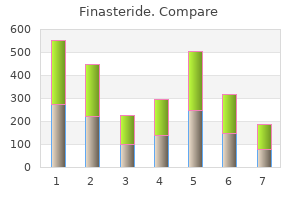
The ages at eruption are composite ages for the corresponding upper and lower teeth hair loss due to stress generic finasteride 5 mg mastercard. Generally hair loss cure year purchase genuine finasteride on-line, the lower (mandibular) teeth erupt somewhat earlier than their upper (maxillary) counterparts hair loss remedies 1mg finasteride sale. From the midline to the rear of each jaw hair loss cats safe finasteride 1 mg, there are two incisors hair loss in men finasteride 5mg with visa, a canine, two premolars, and up to three molars on each side (fig. The incisors are anterior, chisel-like cutting teeth used to bite off a piece of food. They serve as weapons in many mammals but became reduced in the course of human evolution until they now project barely beyond the other teeth. The premolars and molars have relatively broad, lumpy surfaces adapted for crushing, shredding, and grinding; they are often informally called the grinders. Each tooth is embedded in a socket called an alveolus, forming a joint called a gomphosis between the tooth and bone (fig. This anchors the tooth firmly in the alveolus but allows for slight movement under the stress of chewing. Regions of a tooth are defined by their relationship to the gingiva: the crown is the portion above the gum attachment; the root is the portion below the gum, embedded in alveolar bone; and the neck is the point where the crown, root, and gum meet. The hygiene of this sulcus is especially important to dental health (see Deeper Insight 25. With some variation, the incisors and canines have a single root; the premolars have one or two roots; the first and second molars have two to three roots; and in the third molar, the roots are usually fused into one. If plaque is not thoroughly removed by brushing and flossing, bacteria multiply, metabolize the sugars, and release lactic and other acids. These acids dissolve the minerals of enamel and dentin, and the bacteria enzymatically digest the collagen and other organic components. This requires either extraction of the tooth or root canal therapy, in which the pulp is removed and replaced with inert material. Calculus in the gingival sulcus wedges the tooth and gum apart and allows bacterial invasion of the sulcus. In some cases, bacteria spread from the sulcus into the alveolar bone and begin to dissolve it, producing periodontal disease. About 86% of people over age 70 have periodontal disease and many suffer tooth loss as a result. This grinds and tears food more effectively than if the occlusal surfaces were flat. Twenty deciduous teeth (milk teeth or baby teeth) erupt from the ages of 6 to 30 months, beginning with the incisors (fig. Over the course of human evolution, the face became flatter and the jaws shorter, leaving little room for the third molars. Thus, they often remain below the gum and become impacted-so crowded against neighboring teeth and bone that they cannot erupt. Mastication Mastication (chewing) breaks food into pieces small enough to be swallowed and exposes more surface to the action of digestive enzymes. Mastication requires little thought because food stimulates oral receptors that trigger an automatic chewing reflex. The tongue, buccinator, and orbicularis oris muscles manipulate food and push it between the teeth. The masseter and temporalis muscles Most of a tooth consists of hard yellowish tissue called dentin, covered with enamel in the crown and cementum (or cement) in the root. Dentin and cementum are living connective tissues with cells or cell processes embedded in a calcified matrix. Cells of the cementum (cementocytes) are scattered more or less randomly and occupy tiny cavities similar to the lacunae of bone. Cells of the dentin (odontoblasts) line the pulp cavity and have slender processes that travel through tiny parallel tunnels in the dentin. Enamel is not a tissue but a cell-free secretion produced before the tooth erupts above the gum. Damaged dentin and cementum can regenerate, but damaged enamel cannot-it must be artificially repaired. Internally, a tooth has a dilated pulp cavity in the crown and a narrow root canal in the lower root. These spaces are occupied by pulp-a mass of loose connective tissue, blood and lymphatic vessels, and nerves. These nerves and vessels enter the tooth through a pore, the apical foramen, at the basal end of each root canal. The occlusal surface of a premolar has two rounded bumps called cusps; thus, the premolars are also known as bicuspids. This dissection shows erupted deciduous teeth and, deep to them and marked with asterisks, the permanent teeth waiting to erupt. The Salivary Glands Parotid gland Parotid duct Tongue Sublingual ducts Masseter muscle Submandibular duct Submandibular gland Sublingual gland Mandible Lingual frenulum Opening of submandibular duct There are two kinds of salivary glands, intrinsic and extrinsic. The intrinsic (minor) salivary glands are an indefinite number of small glands dispersed amid the other oral tissues-lingual glands in the tongue, labial glands on the inside of the lips, palatine glands of the palate, and buccal glands on the inside of the cheeks. They secrete saliva at a fairly constant rate whether we are eating or not, but in relatively small amounts. This saliva contains lingual lipase and lysozyme and moistens the mouth when we are not eating. The extrinsic (major) salivary glands are three pairs of larger, more discrete organs located outside of the oral mucosa. The secretory acini at the twig ends of the tree are in some cases purely mucous, in others purely serous, and in mixed acini, composed of both mucous and serous cells (fig. The parotid duct passes superficially over the masseter muscle, pierces the buccinator muscle, and opens into the mouth opposite the second upper molar tooth. The submandibular glands, located halfway along the body of the mandible, medial to its margin, just deep to the mylohyoid muscle. The submandibular duct empties into the mouth at a papilla on the side of the lingual frenulum, near the lower central incisors. They have multiple ducts that empty into the mouth posterior to the papillae of the submandibular ducts. Salivation is controlled mainly by parasympathetic nerve fibers that originate in a group of salivatory nuclei, located in the brainstem near the junction of the pons and medulla oblongata. Preganglionic fibers travel from here by way of the facial and glossopharyngeal nerves to ganglia in and near the salivary glands; short postganglionic fibers then finish the path from there to the gland cells themselves (see fig. Sympathetic nerve fibers also innervate the salivary glands, originating in the superior cervical ganglion of the sympathetic chain and following blood vessels to the glands (see fig. Sympathetic stimulation, however, produces only slight increases in salivation, and may even inhibit it, as when fear or nervousness produces a dry mouth feeling. Salivary amylase begins to digest starch as the food is chewed; lingual lipase begins fat digestion to a slight extent; and the mucus binds the masticated food particles into an easily swallowed bolus. The Pharynx Salivary duct Serous acinus (a) Mixed acinus Serous demilune on mixed acinus Mucous cells the pharynx, described in section 22. It has a deep layer of longitudinally oriented skeletal muscle and a superficial layer of circular skeletal muscle. The circular muscle is divided into superior, middle, and inferior pharyngeal constrictors, which force food downward during swallowing. When food is not being swallowed, the inferior constrictor remains contracted to exclude air from the esophagus. This constriction is regarded as the upper esophageal sphincter, although it is not an anatomical feature of the esophagus. Thus, it is regarded as a physiological sphincter rather than a constant anatomical structure. Serous demilune Stroma Duct the Esophagus the esophagus is a straight muscular tube 25 to 30 cm long (see figs. It begins at a level between vertebra C6 and the cricoid cartilage, inferior to the larynx and posterior to the trachea. After passing downward through the mediastinum, it penetrates the diaphragm at an opening called the esophageal hiatus, continues another 3 to 4 cm, and meets the stomach at the level of vertebra T7. Its opening into the stomach is called the cardial orifice (named for its proximity to the heart). The wall of the esophagus is organized into the tissue layers described earlier, with some regional specializations. The submucosa contains esophageal glands that secrete lubricating mucus into the lumen. When the esophagus is empty, the mucosa and submucosa are deeply folded into longitudinal ridges, giving the lumen a starlike shape in cross section. The muscularis externa is composed of skeletal muscle in the upper one-third of the esophagus, a mixture of skeletal and smooth muscle in the middle one-third, and only smooth muscle in the lower one-third. Here, it is covered with a connective tissue adventitia that merges into the adventitias of the trachea and thoracic aorta. Serous cells often form crescent-shaped caps called serous demilunes over the ends of mucous acini. Irritants in the pharynx, esophagus, stomach, and upper duodenum-spicy foods, stomach acid, and toxins, for example-also stimulate salivation. Parasympathetic stimulation dilates the blood vessels to the salivary glands and increases blood flow. During chewing, the tongue collects food, presses it against the palate to form a bolus, and pushes it posteriorly. When the bolus reaches a critical size, the epiglottis tips posteriorly and the bolus slides around it, through a space on each side, into the laryngopharynx. The soft palate and root of the tongue block food and drink from entering the nasal cavity or reentering the mouth. To prevent choking, breathing is automatically suspended, the infrahyoid muscles pull the larynx up to meet the epiglottis and cover the laryngeal opening, and the vocal cords adduct to close the airway. The pharyngeal constrictors contract in order from superior to middle to inferior, driving the bolus downward into the esophagus. The esophageal phase is a wave of involuntary contractions called peristalsis, controlled jointly by the brainstem swallowing center and the myenteric plexus in the esophageal wall. The bolus stimulates stretch receptors that feed into the plexus, which transmits signals to the muscularis externa above and below the bolus. The circular muscle layer above the bolus constricts and pushes the food downward. Below the bolus, the circular muscle relaxes while the longitudinal muscle contracts. The latter action pulls the wall of the esophagus slightly upward, making it a little shorter and dilating it to receive the descending food. When one is standing or sitting upright, most food and liquid drop through the esophagus by gravity faster than the peristaltic wave can keep up with it. Liquid normally reaches the stomach in 1 to 2 seconds and a food bolus in 4 to 8 seconds. As a bolus reaches the lower end of the esophagus, the lower esophageal sphincter relaxes to let it pass into the stomach. The palate, tongue, vocal cords, and epiglottis block the oral and nasal cavities and airway while pharyngeal constrictors push the bolus into the esophagus. Peristalsis drives the bolus downward, and relaxation of the lower esophageal sphincter admits it into the stomach. What is the difference in function and location between intrinsic and extrinsic salivary glands Identify at least two histological features of the esophagus that are especially tied to its role in swallowing. Describe the mechanisms that prevent food from entering the nasal cavity and larynx during swallowing. It is divided into four regions: (1) the cardial part (cardia) is a small area within about 3 cm of the cardial orifice. The pylorus is surrounded by a thick ring of smooth muscle, the pyloric sphincter, which regulates the passage of chyme into the duodenum. Between the esophagus and duodenum, the stomach has two margins called the greater and lesser curvatures. The greater curvature is the long way around, about 40 cm, along the inferolateral surface. The greater omentum, overhanging the small intestine, is suspended from the greater curvature. The lesser curvature is the shorter distance from esophagus to duodenum, about 10 cm, along the superomedial margin facing the liver. The lesser omentum spans the space between the liver and lesser curvature (see fig. Innervation and Circulation the stomach receives parasympathetic nerve fibers from the vagus nerves and sympathetic fibers from the celiac ganglia (see table 15. All blood drained from the stomach and intestines enters the hepatic portal circulation and filters through the liver before returning to the heart. Microscopic Anatomy the stomach wall has tissue layers similar to those of the esophagus, with some variations. The apical regions of its cells are filled with mucin; after it is secreted, mucin swells with water and becomes mucus. The lamina propria is almost entirely occupied by tubular glands, to be described shortly. The muscularis externa has three layers, rather than two: outer longitudinal, middle circular, and inner oblique layers (fig.
Anemia and hypoxia reduce hepcidin synthesis hair loss wigs buy genuine finasteride online, removing its inhibitory effect and thus allowing increased absorption of dietary iron and mobilization of stored iron so it becomes available for hemoglobin synthesis hair loss cure update generic finasteride 5mg fast delivery. The nucleases (ribonuclease and deoxyribonuclease) of pancreatic juice hydrolyze these to their constituent nucleotides hair loss treatment australia buy 1mg finasteride amex. These products are transported across the intestinal epithelium by membrane carriers and enter the capillary blood of the villus hair loss 6 weeks pregnant purchase finasteride online now. By contrast german hair loss cure buy finasteride with a mastercard, it absorbs only about 40% of the dietary calcium, leaving the rest to pass in the feces. Hydrophilic region Hydrophobic region 979 Fat hydrolysis Pancreatic lipase Lecithin Bile acid Dietary lipid Triglyceride Free fatty acid Pancreatic lipase Free fatty acid Emulsification droplets are acted upon by pancreatic lipase, which hydrolyzes the first and third fatty acids from triglycerides, usually leaving the middle fatty acid. Monoglyceride Lipid uptake by micelles Bile acid Monoglycerides Cholesterol Lipid core Micelles in the bile pass to the small intestine and pick up several types of dietary and semidigested lipids. Fatty acids Fat-soluble vitamins Micelles Chylomicron formation Absorptive cell Brush border Fatty acids Triglycerides Chylomicron exocytosis and lymphatic uptake Chylomicrons in secretory vesicles Lacteal Monoglycerides Phospholipids Micelles Cholesterol Protein shell Chylomicron Chylomicrons in lymph Intestinal cells absorb lipids from micelles, resynthesize triglycerides, and package triglycerides, cholesterol, and phospholipids into protein-coated chylomicrons. Golgi complex packages chylomicrons into secretory vesicles; chylomicrons are released from basal cell membrane by exocytosis and enter the lacteal (lymphatic capillary) of the villus. As they leave the small intestine, sugars and amino acids arrive at the liver before any other organ, but lipids do not. This keeps the intracellular concentration of free calcium low, maintaining a gradient that favors uptake. It stimulates the kidneys to synthesize vitamin D from the precursors made by the epidermis and liver (see fig. Thus, it increases absorption of dietary calcium and raises the level of calcium in the blood. Because of their much greater length, the jejunum and ileum absorb much more calcium than the duodenum does, but here it is by the paracellular route (passing between cells) and is independent of hormones. Although green leafy vegetables are high in calcium, little of this is absorbed because they also contain an agent, oxalate, that binds calcium and makes it unavailable for absorption. Dietary fat retards calcium absorption by reacting with it to form poorly absorbed calcium soaps. Name as many enzymes of the intestinal brush border as you can, and identify the substrate or function of each. Explain the distinctions between an emulsification droplet, a micelle, and a chylomicron. What happens to dead epithelial cells that slough off the gastrointestinal mucosa This occurs when the intestine is irritated by bacteria and feces pass through too quickly for adequate reabsorption, or when the feces contain abnormally high concentrations of a solute such as lactose that opposes osmotic absorption of water. Constipation occurs when fecal movement is slow, too much water is reabsorbed, and the feces become hardened. This can result from lack of dietary fiber, lack of exercise, emotional upset, or long-term laxative abuse. The large intestine receives about 500 mL of indigestible food residue per day, reduces it to about 150 mL of feces by absorbing water and salts, and eliminates the feces by defecation. The cecum26 is a blind pouch in the lower right abdominal quadrant inferior to the ileocecal valve. The appendix is densely populated with lymphocytes and is a significant source of immune cells. The colon is that part of the large intestine between the ileocecal junction and rectum (not including the cecum, rectum, or anal canal). The ascending colon begins at the ileocecal valve and passes up the right side of the abdominal cavity. Anal sinuses (b) Anal canal Which anal sphincter is controlled by the autonomic nervous system Here it becomes the descending colon, which passes down the left side of the abdominal cavity. Ascending, transverse, and descending colons thus form a squarish, three-sided frame around the small intestine. The pelvic cavity is narrower than the abdominal cavity, so at the hip bone, the colon turns medially and travels along the iliac fossa before turning downward at the pelvic inlet into the pelvic cavity. Despite its name, the rectum is not quite straight but has three lateral curves as well as an anteroposterior curve. It has three infoldings called transverse rectal folds (rectal valves), which enable it to retain feces while passing gas. Here, the mucosa forms longitudinal ridges called anal columns with depressions between them called anal sinuses. As feces pass through the canal, they press the sinuses and cause them to exude extra mucus and lubricate the canal during defecation. Prominent hemorrhoidal veins form superficial plexuses in the anal columns and around the orifice. Unlike veins in the limbs, they lack valves and are particularly subject to distension and venous pooling. Hemorrhoids are permanently distended veins that protrude into the anal canal or form bulges external to the anus. They can result from the impaired venous return that occurs in obesity and pregnancy. Although it completely encircles the colon just as it does the small intestine, its longitudinal fibers are especially concentrated in three thickened, ribbonlike strips. Haustra are conspicuous in colonic X-rays of living patients; they are not evident in a cadaver, however, because they disappear when muscle tone is lost at death. In the rectum and anal canal, the longitudinal muscle forms a continuous sheet and haustra are absent. The anus is regulated by two sphincters: an internal anal sphincter composed of smooth muscle of the muscularis externa and an external anal sphincter composed of skeletal muscle of the pelvic diaphragm. The ascending and descending colon are retroperitoneal and have a serosa only on the anterior surface, whereas the transverse and sigmoid colon are entirely enclosed in serosa and anchored to the posterior abdominal wall by the mesocolon. The serosa of the transverse through sigmoid colon often has omental appendages, clublike fatty pouches of peritoneum of unknown function. Microscopic Anatomy the mucosa of the large intestine has a simple columnar epithelium in all regions except the lower half of the anal canal, where it has a nonkeratinized stratified squamous epithelium. The latter provides more resistance to the abrasion caused by the passage of feces. There are no circular folds or villi in the large intestine, but there are intestinal crypts. They are deeper than in the small intestine and have a greater density of goblet cells; mucus is their only significant secretion. The lamina propria and submucosa have an abundance of lymphatic tissue, providing protection from the bacteria that densely populate the large intestine. Intestinal Microbes and Gas the large intestine harbors about 800 species of bacteria collectively called the gut microbiome. We provide them with room and board while they provide us with nutrients from our food that we are not equipped to extract on our own. For example, they digest cellulose, pectin, and other plant polysaccharides for which we have no digestive enzymes, and we absorb the resulting sugars. Thus, we get more nutrition from our food because of these bacteria than we would get without them. Indeed, one person may get more calories than another from the same amount of food because of differences in their bacterial populations. Some bacteria also synthesize B vitamins and vitamin K, which are absorbed by the colon. This vitamin K is especially important because the diet alone usually does not provide enough to ensure adequate blood clotting. One of the less desirable and sometimes embarrassing products of these bacteria is intestinal gas. The large intestine contains about 7 to 10 L of gas, expelling about 500 mL/day as flatus and reabsorbing the rest. Much of this is swallowed air that has worked its way through the digestive tract, but the gut microbes add to it. Painful cramping can result when undigested nutrients pass into the colon and furnish an abnormal substrate for bacterial action, so the bacteria produce excess gas-for example, in lactose intolerance. Indole, skatole, and H2S produce most of the odor of flatus and feces, whereas the others are odorless. The hydrogen gas is combustible and has been known to explode during the use of electrical cauterization in surgery. Absorption and Motility the large intestine takes 36 to 48 hours to reduce the residue of a meal to feces, with the residue spending the greatest time (about 24 h) in the transverse colon. This churns and mixes the residue, promotes water and salt absorption, and passes the residue distally to another haustrum. They are often triggered by the gastrocolic and duodenocolic reflexes, in which filling of the stomach and duodenum stimulates motility of the colon. Mass movements occur especially in the transverse to sigmoid colon, often within an hour after breakfast, moving the feces that accumulated and stretched the colon overnight. Defecation Stretching of the rectum stimulates the defecation reflexes, which account for the urge to defecate that is often felt soon after a meal. You may find it enlightening to compare the following discussion of the defecation reflexes with the similar mechanisms controlling urination (see fig. The predictability of the defecation reflexes is useful in house training pets and toilet training children. Stretch signals travel through the plexus to the muscularis of the descending and sigmoid colon and the rectum. This activates a peristaltic wave that drives feces downward, and it relaxes the internal anal sphincter. This reflex is relatively weak, however, and usually requires the cooperative action of the following reflex. These reflexes are involuntary and are the sole means of controlling defecation in infants and some people with transecting spinal cord injuries. However, the external anal sphincter, like the external urethral sphincter controlling urination, is under voluntary control, enabling one to limit defecation to appropriate circumstances. Voluntary retention of feces is also aided by the puborectalis muscle, which loops around the rectum like a sling and creates a sharp anorectal angle that blocks the passage of feces. Defecation normally occurs only when the external anal sphincter and puborectalis muscle are voluntarily relaxed. The kink in the rectum then straightens out and the sphincter opens to allow the feces to fall away. Defecation is also aided by the voluntary Valsalva maneuver, in which a breath hold and contraction of the abdominal muscles increase abdominal pressure, compress the rectum, and squeeze the feces from it. This maneuver can also initiate the defecation reflex by forcing feces from the descending colon into the rectum. The external anal sphincter and external urethral sphincter are controlled together by inhibitory signals from the brainstem, Sigmoid colon 2 Stretch receptors Rectum Anal canal Internal anal sphincter 3 4 External anal sphincter 1 Feces stretch the rectum and stimulate stretch receptors, which transmit signals to the spinal cord. Impulses from the brain prevent untimely defecation by keeping the external anal sphincter contracted. The solids are about 30% bacteria, 30% undigested dietary fiber, 10% to 20% fat, and smaller amounts of protein, sloughed epithelial cells, salts, mucus, and other digestive secretions. Some spinal cord injuries and diseases abolish the voluntary control of the external anal sphincter. The resulting inability to voluntarily retain the feces is called fecal incontinence. If the defecation urge is suppressed, contractions cease in a few minutes and the rectum relaxes. The defecation reflexes reoccur a few hours later or when another mass movement propels more feces into the rectum. How does the mucosa of the large intestine differ from that of the small intestine Name and briefly describe two types of contractions that occur in the colon and nowhere else in the alimentary canal. Inflammation of the appendix, with swelling, pain, and sometimes gangrene, perforation, and peritonitis. Malignant tumors especially of the esophagus, stomach, colon, liver, and pancreas, with colon and pancreatic cancer being among the leading causes of cancer death in the United States. Produces granular lesions and fibrosis of intestine, diarrhea, and lower abdominal pain. Presence of inflamed herniations (outpocketings, diverticula) of the colon, associated especially with low-fiber diets. Can result from esophageal obstructions (tumors, constrictions) or impaired peristalsis (due to neuromuscular disorders). Atrophy of intestinal villi triggered in genetically susceptible individuals by gluten, the protein component of cereal grains. Results in severe malabsorption of most nutrients, causing watery or fatty diarrhea, abdominal pain, diminished growth, and multiple problems tied to nutritional deficiencies. Protrusion of part of the stomach into the thoracic cavity, where the negative thoracic pressure may cause it to balloon. Often causes gastroesophageal reflux (especially when a person is supine) and esophagitis (inflammation of the esophagus). Chronic inflammation resulting in ulceration of the large intestine, especially the sigmoid colon and rectum. Hiatal hernia Ulcerative colitis You can find other digestive system disorders described in the following places: Portal hypertension and ascites in Deeper Insight 20. A frontier Army doctor stationed at Fort Mackinac, William Beaumont, was summoned to examine St.
What is wrong with this thinking hair loss in men ministry buy discount finasteride 5 mg line, and what accounts for the loss of consciousness Consider a man in good health with a 650 mL tidal volume and a respiratory rate of 11 breaths per minute hair loss in men 1950 finasteride 5 mg online. Assuming his anatomical dead space is 185 mL hair loss 6 months after giving birth buy finasteride 1 mg on line, calculate his alveolar ventilation rate in liters per minute hair loss stress order finasteride 1 mg on line. An 83-year-old woman is admitted to the hospital hair loss cure september 2013 finasteride 5mg without prescription, where a critical care nurse attempts to insert a nasoenteric tube ("stomach tube") for feeding. The patient begins to exhibit dyspnea, and a chest X-ray reveals air in the right pleural cavity and a collapsed right lung. You must be familiar with the forces of capillary fluid exchange to understand glomerular filtration, the first step in urine production (see "Filtration and Reabsorption" in section 20. The concepts of osmosis, tonicity, and osmolarity are central to understanding the stages of urine production and the role of the kidneys in regulating fluid balance and urine concentration (see "Osmosis" and "Osmolarity and Tonicity," both in section 3. The urinary system consists of six principal organs: two kidneys, two ureters, the urinary bladder, and the urethra. The urinary tract has important spatial relationships with the vagina and uterus in females and the prostate gland in males. We rid the body of some of these wastes through the respiratory and digestive tracts and the sweat glands, but the urinary system is the principal means of waste excretion. The rest of the urinary system serves only for the transport, storage, and elimination of urine. As we will see, the kidneys also play indispensable roles in regulating blood volume, pressure, and composition. In performing these tasks, they have a very close physiological relationship with the endocrine, circulatory, and respiratory systems, covered in recent chapters. Anatomically, the urinary system is closely associated with the reproductive system. In many animals, the eggs and sperm are emitted through the urinary tract, and the two systems have a shared embryonic development and adult anatomical relationship. This is reflected in humans, where the systems develop together in the embryo and, in the male, the urethra continues to serve as a passage for both urine and sperm. We examine the anatomical relationship between the urinary and reproductive systems in chapter 27, but the physiological link to the circulatory and respiratory systems is more important to consider at this time. Although the primary role of the kidneys is excretion, they play more roles than are commonly realized: They filter the blood and excrete the toxic metabolic wastes. They secrete the hormone erythropoietin, which stimulates the production of red blood cells and thus supports the oxygen-carrying capacity of the blood. They help to regulate calcium homeostasis and bone metabolism by participating in the synthesis of calcitriol. In conditions of extreme starvation, they help to support the blood glucose level by synthesizing glucose from amino acids. In view of such diverse roles, it is easy to see why renal failure can lead to the collapse of many other physiological functions as well. Among the most toxic of our metabolic wastes are small nitrogen-containing compounds called nitrogenous wastes (fig. Although less toxic than ammonia and less abundant than urea, these too are potentially harmful. Excretion Excretion is the process of separating wastes from the body fluids and eliminating them from the body. The respiratory system excretes carbon dioxide, small amounts of other gases, and water. The integumentary system excretes water, inorganic salts, lactate, and urea in the sweat. The digestive system not only eliminates food residue (which is not a process of excretion) but also actively excretes water, salts, carbon dioxide, lipids, bile pigments, cholesterol, and other metabolic wastes. The urinary system excretes a broad variety of metabolic wastes, toxins, drugs, hormones, salts, hydrogen ions, and water. Position and Associated Structures the kidneys lie against the posterior abdominal wall at the level of vertebrae T12 to L3. The right kidney is slightly lower than the left because of the space occupied by the large right lobe of the liver above it. The kidneys are retroperitoneal, along with the ureters, urinary bladder, renal artery and vein, and the adrenal glands (fig. Gross Anatomy Each kidney weighs about 150 g and measures about 11 cm long, 6 cm wide, and 3 cm thick-about the size of a bar of bath soap. The lateral surface is convex, and the medial surface is concave and has a slit, the hilum, that admits the renal nerves, blood vessels, lymphatics, and ureter. If the kidney were not retroperitoneal, where on this figure would you have to relocate it The kidneys are suspended by collagen fibers that extend from the fibrous capsule, through the fat, to the renal fascia. The renal fascia is fused with the peritoneum anteriorly and with the fascia of the lumbar muscles posteriorly. In spite of all this, the kidneys drop about 3 cm when one goes from lying down to standing, as when getting out of bed in the morning. Under some circumstances, they become detached and drift even lower, with pathological results (see nephroptosis, or "floating kidney," in table 23. The renal parenchyma-the glandular tissue that forms the urine-appears C-shaped in frontal section (fig. It encircles a medial cavity, the renal sinus, occupied by blood and lymphatic vessels, nerves, and urine-collecting structures. Adipose tissue fills the remaining space in the sinus and holds these structures in place. The parenchyma is divided into two zones: an outer renal cortex about 1 cm thick and an inner renal medulla facing the sinus. Extensions of the cortex called renal columns project toward the sinus and divide the medulla into 6 to 10 renal pyramids. Each pyramid is conical, with a broad base facing the cortex and a blunt point called the renal papilla facing the sinus. This is a hint of how important the kidneys are in regulating blood volume and composition. Just before or after entering the hilum, the renal artery divides into a few segmental arteries, and each of these further divides into a few interlobar arteries. An interlobar artery penetrates each renal column and travels between the pyramids toward the corticomedullary junction, the boundary between the cortex and medulla. Each arcuate artery gives rise to several cortical radiate arteries, which pass upward into the cortex. The pathway through the vasa recta (instead of peritubular capillaries) applies only to the juxtamedullary nephrons. Pink indicates the arterial supply to the nephrons; violet indicates the portal system of connected capillary beds; and blue indicates venous drainage of the kidney. The efferent arteriole usually leads to a plexus of peritubular capillaries, named for the fact that they form a network around another part of the nephron, the renal tubule. The renal tubule reabsorbs most of the water and solutes that filtered out of the blood at the glomerulus and returns these to the bloodstream by way of these peritubular capillaries. The peritubular capillaries carry it away to the cortical radiate veins, arcuate veins, interlobar veins, and the renal vein, in that order. Here, the efferent arterioles descend immediately into the medulla and give rise to the vasa recta instead of peritubular capillaries. Capillaries of the vasa recta lead into venules that ascend and empty into the arcuate and cortical radiate veins. Capillaries of the vasa recta are wedged into the tight spaces between the medullary parts of the renal tubule, and carry away water and solutes reabsorbed by those sections of the tubule. For clarity, vasa recta are shown only on the left and peritubular capillaries only on the right. In the juxtamedullary nephron (left), the efferent arteriole gives rise to the vasa recta of the medulla. Each nephron is composed of two principal parts: a renal corpuscle, which filters the blood plasma, and a long coiled renal tubule, which converts the filtrate to urine. The parietal (outer) layer is a simple squamous epithelium, and the visceral (inner) layer consists of elaborate cells called podocytes7 wrapped around the capillaries of the glomerulus. The two layers 7 podo = foot; cyte = cell are separated by a filtrate-collecting capsular space. In tissue sections, this space appears as an empty circular or C-shaped space around the glomerulus. At the vascular pole, the afferent arteriole enters the capsule, bringing blood to the glomerulus, and the efferent arteriole leaves the capsule and carries blood away. Thus, the glomerulus has a large inlet and a small outlet-a point whose functional significance will become apparent later. At the urinary pole, the parietal wall of the capsule turns away from the corpuscle and gives rise to the renal tubule. The simple squamous epithelium of the capsule becomes simple cuboidal in the tubule. It is about 3 cm long and divided into four regions: the proximal convoluted tubule, nephron loop, distal convoluted tubule, and collecting duct (fig. The first three of these are parts of one nephron; the collecting duct receives fluid from many nephrons. Each region has unique physiological properties and roles in the production of urine. It is the longest and most coiled of the four regions and therefore dominates histological sections of renal cortex. It has a simple cuboidal epithelium with prominent microvilli (a brush border), which attests to the great deal of absorption that occurs here. The nephron loop is a long U-shaped portion of the renal tubule found mostly in the medulla. They form the initial part of the descending limb and part or all of the ascending limb. The cells here are heavily engaged in active transport of salts, so they have very high metabolic activity and are loaded with mitochondria, accounting for their thickness. It forms most of the descending limb, and in some nephrons, it rounds the bend and continues partway up the ascending limb. The cells here have low metabolic activity, but the thin segment of the descending limb is very permeable to water. It is shorter and less coiled than the proximal convoluted tubule, so fewer sections of it are seen in histological sections. It has a cuboidal epithelium with smooth-surfaced cells nearly devoid of microvilli. Numerous collecting ducts converge toward the tip of a medullary pyramid, and near the papilla, they merge to form a larger papillary duct. The flow of fluid from the point where the glomerular filtrate is formed to the point where urine leaves the body is: glomerular capsule proximal convoluted tubule nephron loop distal convoluted tubule collecting duct papillary duct minor calyx major calyx renal pelvis ureter urinary bladder urethra. Their proximal and distal convoluted tubules are commingled in a single tangled mass in each nephron. They have very long nephron loops that extend as far as the apex of the renal pyramid. They have relatively short nephron loops that dip only slightly into the outer medulla before turning back (see fig. As you will see later, nephron loops are responsible for maintaining an osmotic gradient in the medulla that helps the body conserve water. Although only 15% of the nephrons are juxtamedullary, they are almost solely responsible for maintaining this gradient. Explain the forces that promote and oppose filtration, and calculate the filtration pressure if given the magnitude of these forces; and c. Renal Innervation Wrapped around each renal artery is a renal plexus of nerves and ganglia (see fig. The plexus follows branches of the renal artery into the parenchyma of the kidney, issuing nerve fibers to the blood vessels and convoluted tubules of the nephrons. The renal plexus carries sympathetic innervation from the abdominal aortic plexus (especially its superior mesenteric and celiac ganglia) as well as afferent pain fibers from the kidneys en route to the spinal cord. Stimulation by the sympathetic fibers of the renal plexus tends to reduce glomerular blood flow and therefore the rate of urine production, although these rates are influenced by other factors as well. Another role of the sympathetic fibers is to respond to falling blood pressure by stimulating the kidneys to secrete renin, an enzyme that activates hormonal mechanisms for restoring blood pressure. The kidneys also receive parasympathetic innervation from branches of the vagus nerve, but the function of this is unknown. Arrange the following in order from the most numerous to the least numerous structures in a kidney: glomeruli, major calyces, minor calyces, cortical radiate arteries, interlobar arteries. Trace the path taken by one red blood cell from the renal artery to the renal vein.
Hydrogen ions are also a potent stimulus to the peripheral chemoreceptors hair loss in men zone discount finasteride 5mg visa, which mediate about 25% of the respiratory response to pH changes hair loss cream purchase finasteride with mastercard. When pH alone changes hair loss in men quilters buy finasteride on line, there is a strong effect on respiration; when Pco2 alone changes hair loss ulta purchase finasteride 5 mg without a prescription, the effect is weaker hair loss in men will trichomoniasis 1mg finasteride with amex. Therefore, even though these two variables usually change together, we can see that the chemoreceptors react primarily to the H+. A Pco2 less than 37 mm Hg is called hypocapnia,30 and is the most common cause of alkalosis. Thus, the H+ on the right is consumed, and as H+ concentration declines, the pH rises and ideally returns the blood from the acidotic range to normal. In diabetes mellitus, for example, rapid fat oxidation releases acidic ketone bodies, causing an abnormally low pH called ketoacidosis. Ketoacidosis tends to induce a form of dyspnea called Kussmaul respiration (see table 22. Even in eupnea, the hemoglobin is 97% saturated with O2, so little can be added by increasing pulmonary ventilation. At low elevations, such a low Po2 seldom occurs even in prolonged holding of the breath. A moderate drop in Po2 does stimulate the peripheral chemoreceptors, but another effect overrides this: As the level of HbO2 falls, hemoglobin binds more H+ (see fig. This raises the blood pH, which inhibits respiration and counteracts the effect of low Po2. At about 10,800 feet (3,300 m), arterial Po2 falls to 60 mm Hg and the stimulatory effect of hypoxemia on the carotid bodies overrides the inhibitory effect of the pH increase. However, this is not true; all these values remain essentially the same in exercise as they do at rest. It appears that the increased respiration has other causes: (1) When the brain sends motor commands to the muscles (via the lower motor neurons of the spinal cord), it also sends this information to the respiratory centers, so they increase pulmonary ventilation in anticipation of the needs of the exercising muscles. In contrast to homeostasis by negative feedback, this is considered a feed-forward mechanism, in which signals are transmitted to the effectors (brainstem respiratory centers) to produce a change in anticipation of need. Thus, the respiratory centers increase breathing because they are informed that the muscles have been told to move or are actually moving. Therefore, the Pco2 of the arterial blood is an important driving force in respiration, even though its action on the chemoreceptors is indirect. This automatically ensures that the blood is at least 97% saturated with O2 as well. When it drops below 60 mm Hg, however, it excites the peripheral chemoreceptors and stimulates an increase in ventilation. The increase in respiration during exercise results from the expected or actual activity of the muscles, not from any change in blood gas pressures or pH. Oxygen Imbalances Hypoxia is a deficiency of oxygen in a tissue or the inability to use oxygen. It is not a respiratory disease in itself but is often a consequence of respiratory diseases. Hypoxia is classified according to cause: Hypoxemic hypoxia, a state of low arterial Po2, is usually due to inadequate pulmonary gas exchange. Some of its root causes include atmospheric deficiency of oxygen at high elevations; impaired ventilation, as in drowning or aspiration of foreign matter; respiratory arrest; and the degenerative lung diseases discussed shortly. It also occurs in carbon monoxide poisoning, which prevents hemoglobin from transporting oxygen. Ischemic hypoxia results from inadequate circulation of the blood, as in congestive heart failure. Anemic hypoxia is due to anemia and the resulting inability of the blood to carry adequate oxygen. Histotoxic hypoxia occurs when a metabolic poison such as cyanide prevents the tissues from using the oxygen delivered to them. This is especially critical in organs with the highest metabolic demands, such as the brain, heart, and kidneys. It is safe to breathe 100% oxygen at 1 atm for a few hours, but oxygen toxicity rapidly develops when pure oxygen is breathed at 2. Excess oxygen generates hydrogen peroxide and free radicals that destroy enzymes and damage nervous tissue; thus, it can lead to seizures, coma, and death. This is why scuba divers breathe a mixture of oxygen and nitrogen rather than pure compressed oxygen (see Deeper Insight 22. Hyperbaric oxygen was formerly used to treat premature infants for respiratory distress syndrome, but it caused retinal deterioration and blinded many infants before the practice was discontinued. How is most oxygen transported in the blood, and why does carbon monoxide interfere with this Give two reasons why highly active tissues can extract more oxygen from the blood than less active tissues do. Name the pH imbalances that result from these conditions and explain the relationship between Pco2 and pH. What is the most potent chemical stimulus to respiration, and where are the most effective chemoreceptors for it located They are almost always caused by cigarette smoking, but occasionally result from air pollution, occupational exposure to airborne irritants, or a hereditary defect. Chronic bronchitis is severe, persistent inflammation of the lower respiratory tract. Goblet cells of the bronchial mucosa enlarge and secrete excess mucus, while at the same time, the cilia are immobilized and unable to discharge it. Thick, stagnant mucus accumulates in the lungs and furnishes a growth medium for bacteria. Several already have been mentioned in this chapter and some others are briefly described in table 22. In severe cases, the lungs are flabby and cavitated with spaces as big as grapes or even ping-pong balls. The severity of the disease may not be fully appreciated by looking only at histological specimens since such large spaces are not seen on microscope slides. The air passages open adequately during inspiration, but they tend to collapse and obstruct the outflow of air. Air becomes trapped in the lungs, and over a period of time a person becomes barrel-chested. The overly stretched thoracic muscles contract weakly, which further contributes to the difficulty of expiration. People with emphysema can become exhausted and emaciated because they expend three to four times the normal amount of energy just to breathe. Even slight physical exertion, such as walking across a room, can cause severe shortness of breath. Hypoxemia stimulates the kidneys to secrete erythropoietin, which leads to accelerated erythrocyte production and polycythemia (see fig. Transmitted especially by contact of contaminated hands with mucous membranes; not transmitted orally. Acute lung inflammation and alveolar injury stemming from trauma, infection, burns, aspiration of vomit, inhalation of noxious gases, drug overdoses, and other causes. Alveolar injury is accompanied by severe pulmonary edema and hemorrhaging, followed by fibrosis that progressively destroys lung tissue. A lower respiratory infection caused by any of several viruses, fungi, or protozoans, but most often the bacterium Streptococcus pneumoniae. Causes filling of alveoli with fluid and dead leukocytes and thickening of the respiratory membrane, which interferes with gas exchange and causes hypoxemia. Cessation of breathing for 10 seconds or longer during sleep; sometimes occurs hundreds of times per night, often accompanied by restlessness and alternating with snoring. Over time, may lead to daytime drowsiness, hypoxemia, polycythemia, pulmonary hypertension, congestive heart failure, and cardiac arrhythmia. Pulmonary infection with the bacterium Mycobacterium tuberculosis, which invades the lungs by way of air, blood, or lymph. Progressive fibrosis compromises the elastic recoil and ventilation of the lungs and causes pulmonary hemorrhaging as it invades blood vessels. The most important cause of lung cancer is cigarette smoking, distantly followed by air pollution. There are three forms of lung cancer, the most common of which is squamous-cell carcinoma. In its early stage, basal cells of the bronchial epithelium multiply and the ciliated pseudostratified epithelium transforms into the stratified squamous type. As the dividing epithelial cells invade the underlying tissues of the bronchial wall, the bronchus develops bleeding lesions. Dense swirled masses of keratin appear in the lung parenchyma and replace functional respiratory tissue. A second form of lung cancer, nearly as common, is adenocarcinoma,32 which originates in the mucous glands of the lamina propria. This originates in the main bronchi but invades the mediastinum and metastasizes quickly to other organs. As a tumor invades the bronchial wall and grows around it, it compresses the airway and may cause atelectasis (collapse) of more distal parts of the lung. Growth of the tumor produces a cough, but coughing is such an everyday occurrence among smokers it seldom causes much alarm. Lung cancer metastasizes so rapidly that it has usually spread to other organs by the time it is diagnosed. Common sites of metastasis are the pericardium, heart, bones, liver, lymph nodes, and brain. The chance of recovery is poor relative to other cancers, with only 18% of patients surviving for 5 years after diagnosis. As early as the fifth century bce, Aristotle described divers using snorkels and taking containers of air underwater in order to stay down longer. Some Renaissance artists depicted divers many meters deep breathing from tubes to the water surface. The short snorkels used today are about the maximum length that will work for surface breathing. Another reason snorkels cannot be used at greater depths is that water pressure increases by 1 atm for every 10 m of depth, and even at 1 m the pressure is so great that a diver cannot expand the chest muscles without help. The tanks create a positive intrapulmonary pressure and enable the diver to inhale with only slight assistance from the thoracic muscles. On land, nitrogen presents no physiological problems; it dissolves poorly in blood and it is physiologically inert. But under hyperbaric conditions, larger amounts of nitrogen dissolve in the blood. Strong currents, equipment failure, and other hazards sometimes make scuba divers panic, hold their breath, and quickly swim to the surface (a breath-hold ascent). Ambient (surrounding) pressure falls rapidly as a diver ascends, and the air in the lungs expands just as rapidly. Then, when the diver takes a breath of air at the surface, alveolar air goes directly into the bloodstream and causes air embolism. After passing through the heart, the emboli enter the cerebral circulation because the diver is head-up and air bubbles rise in liquid. The resulting cerebral embolism can cause motor and sensory dysfunction, seizures, unconsciousness, and drowning. In one case, children trapped air in a bucket 1 m underwater and then swam under the bucket to breathe from the air space. One child filled his lungs under the bucket, did a "mere" 1 m breath-hold ascent, and his alveoli ruptured. He died in the hospital, partly because the case was mistaken for drowning and not treated for what it really was. This would not have happened to a person who inhaled at the surface, did a breath-hold dive, and then resurfaced-nor is barotrauma a problem for those who do breath-hold dives to several meters. Decompression tables prescribe safe rates of ascent based on the depth and the length of time a diver has been down. If a diver ascends too rapidly, nitrogen "boils" from the tissues-especially in the 3 m just below the surface, where the relative pressure change is greatest. Nitrogen bubbles in the pulmonary capillaries cause chokes-substernal pain, coughing, and dyspnea. These symptoms usually occur within an hour of surfacing, but they are sometimes delayed for up to 36 hours. Caisson disease was first reported in the late 1800s among workmen building the foundations of the Brooklyn Bridge. Any respiratory disorder that causes hypoxemia stimulates accelerated erythropoiesis in the red bone marrow. The distinction between the respiratory and conducting divisions of this system, and constituents of each division 4. The distinction between the upper and lower respiratory tract and the dividing line between them 5. The extent of the nasal cavity, names of its anterior and posterior openings, and names of the two chambers separated by the nasal septum, and histology of its mucosa 6.
Order generic finasteride online. Hair Transplant |Hair Implant | FUE Hair Transplant । DHI Hair Transplant ।DHT Hair Transplant.
Local anesthetics such as procaine (Novocaine) and tetracaine selectively deaden specific nerves hair loss in men kegel purchase 5 mg finasteride overnight delivery. They decrease the permeability of membranes to Na+ hair loss 6 months after stress generic finasteride 5mg line, thereby reducing their ability to produce action potentials hair loss cure earache finasteride 5mg amex. A sound knowledge of anatomy hair loss cure 309 buy finasteride 1mg online, control of infection and pain hair loss 5 months after baby order finasteride in india, and development of better tools converged to allow surgeons time to operate more carefully. It attracted a more educated class of practitioner, which put it on the road to becoming the remarkable lifesaving approach that it is today. The special route and effect of pain signals that involve the reticular formation; how responses to these signals differ from other responses to pain 12. Names of some analgesic neuropeptides and how they affect the sensation of pain 5. Structure of the tympanic membrane and tympanic cavity; the names, structures, and anatomical arrangement of the auditory ossicles; the two middle-ear muscles; and anatomy of the auditory tube, its contribution to hearing, and its relevance to middleear infections 7. The bony and membranous labyrinths of the inner ear; the names and distribution of the two inner-ear fluids in relation to the labyrinths 8. Structure of the spiral organ, especially the hair cells and tectorial membrane; differences between inner and outer hair cells 11. How vibrations of the tympanic membrane lead to stimulation of the cochlear nerve 13. How the outer hair cells tune the cochlea to improve its sensitivity to differences in pitch 15. The pathway from cochlear nerve to auditory centers of the brain; the feedback pathway from the pons back to the cochlea, and its purpose 16. Differences between static and dynamic equilibrium and between linear and angular acceleration 17. Structure of the saccule and utricle and the relevance of the spatial orientation of the macula in each one 18. How linear acceleration stimulates the hair cells of the saccule and utricle during linear acceleration; how the body senses the difference between vertical and horizontal acceleration 19. Structure of the semicircular ducts, especially the crista ampullaris and cupula 20. How acceleration stimulates hair cells of the crista ampullaris, and why the combined input of the six semicircular ducts enables 16. The definition of sensory transduction and the relationship of neural action potentials to that concept 3. Five primary taste sensations, and sensations other than taste that play a part in flavor 4. Mechanisms by which sugars, salts, alkaloids, acids, and glutamate excite taste cells 5. Which nerves carry taste signals, what routes they take to the brain, and what brain centers receive gustatory input 6. Which cranial nerve carries olfactory signals to the brain, and the route and point of termination of its nerve fibers 9. Sensory routes from the olfactory bulbs to the temporal lobes, insula, orbitofrontal cortex, hippocampus, amygdala, and hypothalamus 10. Three types of unencapsulated sensory nerve endings, and what it means to say a nerve ending is unencapsulated 2. Six types of encapsulated nerve endings and how these differ from unencapsulated endings 3. The main routes for somatosensory signals from the head, and from the lower body, to the brainstem; the final destination of proprioceptive signals in the brain; and the final destination of most other sensory signals 4. Differences between somatic and visceral pain, and between superficial and deep somatic pain 7. The general three-neuron pathway typically taken by pain signals to the cerebral cortex 9. Pain pathways from receptors in the head to the cerebral cortex, including the cranial nerves that carry pain signals 10. Pain pathways from the lower body to the cerebral cortex, including the spinal cord tracts that carry pain signals 16. How sound is generated; what physical properties of a sound wave are measured in hertz and decibels; and what sensory qualities of sound correspond to those two physical properties 2. The total range of human hearing, in hertz, and the narrower range in which humans hear best 3. The decibel level of ordinary conversation and the thresholds of hearing and pain 4. Why it cannot be said that the vestibular system senses motion of the head, but only changes in the rate of motion 22. The path taken by signals in the vestibular nerve to the cerebrum, cerebellum, reticular formation, spinal cord, and nuclei of the three cranial nerves for eye movements 23. General structure of the retina; its two points of attachment to the wall of the eye; and the locations, structure, and functional significance of the optic disc, optic nerve, macula lutea, and fovea centralis 9. Structure and action of the pupillary constrictor and dilator; anatomy of their autonomic innervation; and the photopupillary reflex 11. Principles of refraction; points at which refraction occurs as light enters the eye; relative contributions of the cornea and lens to image formation, and the reason for the difference 12. The difference between emmetropia and the near response, and three mechanisms of the near response 13. Histological layers and cell types of the retina; three types of photoreceptor cells and their respective functions; functions of the retinal bipolar, ganglion, horizontal, and amacrine cells 14. The structures of rods and cones; where visual pigments are contained in these cells; the general structure of rhodopsin and photopsin; and how these two pigments differ 15. Why a single retinal receptor system cannot achieve both low-threshold night vision and high-resolution day vision; why rod vision works in very low light but sacrifices resolution to do so; and why cone vision gives high resolution but sacrifices light sensitivity 19. Difference between S, M, and L cones; how neural coding and three cone types produce sensitivity to innumerable colors; and what causes color blindness 20. Projection pathways from the eyes to the occipital lobe and to the superior colliculi and pretectal nuclei of the midbrain 22. Hemidecussation, where it occurs, and how it determines what areas of the visual field are seen by the right and left occipital lobes 16. The definition of vision and the range of electromagnetic wavelengths over which human vision occurs 2. Six extrinsic eye muscles, their anatomy, the eye motions they produce, and the cranial nerves that control them 3. Components of the lacrimal apparatus and the route taken by tears as they wash over the eye and drain into the nasal cavity 4. Norepinephrine is a neuromodulator that blocks the conduction of pain signals by second-order spinal neurons. The most finely detailed vision occurs when an image falls on a pit in the retina called the. Three rows of in the cochlea have V-shaped arrays of stereocilia and tune the frequency sensitivity of the cochlea. The is a tiny bone that vibrates in the oval window and thereby transfers sound vibrations to the inner ear. The of the midbrain receives auditory input and triggers the head-turning auditory reflex. Olfactory neurons synapse with mitral cells and tufted cells in the, which lies inferior to the frontal lobe. In the phenomenon of, pain from the viscera is perceived as coming from an area of the skin. Building Your Medical Vocabulary State a meaning of each word element, and give a medical term that uses it or a slight variation of it. Things we see with the left eye are perceived only in the right cerebral hemisphere. Rods and cones release their neurotransmitter when stimulated by light, but not in total darkness. The principle of neural convergence is explained under "Neural Pools and Circuits" in section 12. What type of cutaneous receptor enables you to feel an insect crawling through your hair Contraction of a muscle usually puts more tension on a structure, but contraction of the ciliary muscle puts less tension on the lens. Janet has terminal ovarian cancer and is in severe pelvic pain that has not yielded to any other treatment. A neurosurgeon performs an anterolateral cordotomy, cutting across the anterolateral region of her lumbar spinal cord. In discussing the synthesis of this class of hormones, it will be assumed that you are familiar with protein structure (see "Proteins" in section 2. Many hormones exert their effects by binding to proteins of the plasma membranes of their target cells. A review of the transport maximum (Tm) of membrane proteins (see "Carrier-Mediated Transport" in section 3. Gap junctions join single-unit smooth muscle, cardiac muscle, epithelial, and other cells to each other. They enable cells to pass nutrients, electrolytes, and signaling molecules directly from the cytoplasm of one cell to the cytoplasm of the next through pores in their plasma membranes (see fig. Neurotransmitters are released by neurons, diffuse across a narrow synaptic cleft, and bind to receptors on the surface of the next cell. Paracrines1 are secreted by one cell, diffuse to nearby cells in the same tissue, and stimulate their physiology. Hormones,2 in the strict sense, are chemical messengers that are transported by the bloodstream and stimulate physiological responses in cells of another tissue or organ, often a considerable distance away. Certain hormones produced by the pituitary gland in the head, for example, act on organs as far away as the pelvic cavity. This chapter is concerned mainly with hormones and, to some extent, paracrine secretions. The glands, tissues, and cells that secrete hormones constitute the endocrine3 system; the study of this system and the diagnosis and treatment of its disorders is called endocrinology. The most familiar hormone sources are the organs traditionally recognized as endocrine glands, such as the pituitary, thyroid, and adrenal glands, among others (fig. Growing knowledge of endocrinology has revealed, however, that hormones are also secreted by numerous organs and tissues not usually thought of as glands, such as the brain, heart, small intestine, bones, and adipose tissue. I f the body is to function as an integrated whole, its organs must communicate with each other and coordinate their activities. Even simple organisms composed of only a few cells have mechanisms for intercellular communication, suggesting that such mechanisms evolved very early in the history of life. In humans, two such systems are especially prominent-the nervous and endocrine systems, which communicate with neurotransmitters and hormones, respectively. Nearly everyone has heard of at least some hormones- growth hormone, thyroid hormone, estrogen, and insulin, for example. At least passingly familiar, too, are some of the glands that secrete them (such as the pituitary and thyroid glands) and some disorders that result from hormone deficiency, excess, or dysfunction (such as diabetes, goiter, and dwarfism). We will start with the relatively familiar and large-scale aspects of this system-a survey of the endocrine glands, their hormones, and the principal effects of those hormones. We will then work our way down to the finer and less familiar details-the chemical identity of hormones, how they are made and transported, and how they produce their effects on their target cells. Shorter sections at the end of the chapter discuss the role of the endocrine system in adapting to stress, some hormonelike paracrine secretions, and the pathologies that result from endocrine dysfunction. The classical distinction between exocrine and endocrine glands has been the presence or absence of ducts. Most exocrine glands secrete their products by way of a duct onto an epithelial surface such as the skin or the mucosa of the digestive tract. Endocrine glands, by contrast, are ductless and release their secretions into the bloodstream (see fig. After reading this chapter, name at least three hormone-secreting organs that are not shown in this illustration. As we see in the photo that opens this chapter, endocrine glands have an unusually high density of blood capillaries; these serve to pick up and carry away their hormones. These vessels are an especially permeable type called fenestrated capillaries, which have patches of large pores in their walls allowing for the easy uptake of matter from the gland tissue (see fig. Some glands and secretory cells defy simple classification as endocrine or exocrine. Liver cells, for example, behave as exocrine cells in the traditional sense by secreting bile into ducts that lead ultimately to the small intestine. However, they also secrete hormones into the blood, and in this respect they act as endocrine cells. One important difference is the speed with which they start and stop responding to a stimulus. The nervous system typically responds within a few milliseconds, whereas it takes from several seconds to days for a hormone to act. When a stimulus ceases, the nervous system stops responding almost immediately, whereas hormonal effects can last for days or even longer. On the other hand, under long-term stimulation, most neurons quickly adapt and their response declines. Another difference is that an efferent nerve fiber innervates only one organ and a limited number of cells within that organ, so its effects are usually precisely targeted and relatively specific.
References
- Schessl J, Zou Y, McGrath MJ, et al. Proteomic identification of FHL1 as the protein mutated in human reducing body myopathy. J Clin Invest. 2008;118:904-912.
- Ross MN, Haase GM, Poole MA, et al. Comparison of totally implanted reservoirs with external catheters as venous access devices in pediatric oncology patients. Surg Gynecol Obstet 1988;167(2):141-144.
- Kim YH, Czer LS, Soukiasian HJ, et al. Ischemic mitral regurgitation: revascularization alone versus revascularization and mitral valve repair. Ann Thorac Surg 2005;79(6): 1895-1901.
- Parker LH, Schmidt M, Jin SW, et al: The endothelial-cell-derived secreted factor Egfl7 regulates vascular tube formation, Nature 428(6984):754-758, 2004.
- Meston CM, Frohlich PF: Update on female sexual function, Curr Opin Urol 11:603n609, 2001.
- Ditto PH, Jacobson JA, Smucker WD, Danks JH, Fagerlin A. Context changes choices: a prospective study of the effects of hospitalization on life-sustaining treatment preferences. Med Decis Making. 2006;26(4):313-322.
- Copin MC, Devisme L, Buisine MP, et al. From normal respiratory mucosa to epidermoid carcinoma: expression of human mucin genes. Int J Cancer 2000;86:162-8.