Alison C. Abreu, MD
- Assistant Professor of Family Medicine and Psychiatry
- Roy J. and Lucille A. Carver College of Medicine
- University of Iowa
- Iowa City, Iowa
Although fluids of this type are adequate for most pediatric patients prostate cancer 80 year old discount rogaine 2 line, individual patient characteristics must prostate 90 foundation purchase rogaine 2 with visa, as always prostate cancer 9 gleason purchase rogaine 2 60 ml free shipping, be considered when choosing the type of fluid to use man health hu purchase rogaine 2 60ml on line. It is treated first with volume resuscitation when needed followed by repletion of the free water deficit man health malaysia order rogaine 2 60 ml line, and by addressing the underlying cause. In anesthesia practice, hyperkalemic cardiac toxicity is associated with the administration of succinylcholine to patients with upper motor neuron lesions or severe burns. Carbohydrate-inducedhypophosphatemia(refeedingsyndrome), mediated by insulin-induced cellular phosphate uptake, is the most commonly encountered type in hospitalized patients. Effects of hypernatraemia in the central nervous system and its therapy in rats and rabbits. A study in animals showing the effect of untreated hypernatremia that results in brain lesions, myelinolysis, and cellular necrosis. The refeeding syndrome should be characterized as a syndrome of generalized fluid and electrolyte imbalance. Recommended electrolyte supplementation and laboratory monitoring can help prevent the disorder in susceptible patients. In recent years, new potential targets involved in the pathogenesis of heart failure have been identified. A summary of new findings regarding alterations of magnesium and phosphorus metaboilism are reviewed for the clinician. Brain cell volume regulation in hyponatremia: role of sex, age, vasopressin, and hypoxia. The use of ethanol as a marker to detect and quantify the absorption of irrigation fluid during transurethral resection of the prostate. Upregulation of aquaporin-2 water channel expression in chronic heart failure rat. Secretion of brain natriuretic peptide in patients with aneurysmal subarachnoid haemorrhage. Severe hyponatraemia after plastic surgery in a girl with cleft palate, medial facial hypoplasia and growth retardation. Postoperative hyponatraemic encephalopathy following elective surgery in children. Postoperative hyponatremia despite near-isotonic saline infusion: a phenomenon of desalination. Development of severe hyponatraemia in hospitalized patients: treatment-related risk factors and inadequate management. Novel agents for the treatment of hyponatremia: a review of conivaptan and tolvaptan. Dual impact of tolvaptan on intracellular and extracellular water in chronic kidney disease patients with fluid retention. Preoperative serum potassium levels and perioperative outcomes in cardiac surgery patients. Separation of myocardial versus peripheral effects of calcium administration in normocalcemic and hypocalcemic states using pressure volume (conductance) relationships. Efficacy of pamidronate in reducing skeletal events in patients with advanced multiple myeloma. Comparison of risedronate to alendronate and calcitonin for early reduction of nonvertebral fracture risk: results from a managed care administrative claims database. The refeeding syndrome: an approach to understanding its complications and preventing its occurrence. Intravenous phosphate repletion regimen for critically ill patients with moderate hypophosphatemia. Effect of acute magnesium administration on the frequency of ventricular arrhythmia in patients with heart failure. Effects of intravenous magnesium in suspected acute myocardial infarction: overview of randomised trials. Correction of ionized plasma magnesium during cardiopulmonary bypass reduces the risk of postoperative cardiac arrhythmia. Developed with the special contribution of the Heart Failure Association and the European Heart Rhythm Association. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Developed in Collaboration With the International Society for Heart and Lung Transplantation. Micropuncture study of hypertonic mannitol diuresis in the proximal and distal tubule of the dog kidney. Loop diuretics for chronic renal insufficiency: a continuous infusion is more efficacious than bolus therapy. The relative significance of blood urea nitrogen and serum creatinine concentrations in azotemia. Unexpected effects of treating hypertension in men with electrocardiographic abnormalities: a critical analysis. Diuretics, serum potassium and ventricular arrhythmias in the Multiple Risk Factor Intervention Trial. Effects of exogenous intravenous glucose on plasma glucose and lipid homeostasis in anesthetized infants. A novel isotonic-balanced electrolyte solution with 1% glucose for intraoperative fluid therapy 108. Hypotonic versus isotonic maintenance fluids after surgery for children: a randomized controlled trial. Furthermore, massive bleeding can produce an acquired hemostatic defect called massive transfusion coagulopathy that is characterized by tissue injury, dilutional hemostatic changes, hypothermia, acidosis, and multiorgan dysfunction. Tissue injury and the stress response activate fibrinolysis that can further contribute to coagulopathy and bleeding. The vascular endothelium plays a major role in preventing clotting; it presents an important anticoagulation interface with circulating blood. Multiple substances are released to prevent activation of both cellular and humoral components of hemostasis. Understanding hemostasis, perioperative bleeding, and treatment of coagulopathy in the current era requires knowledge of the multiple interactions that occur between molecular and cellular components of the coagulation cascade. Hemostasis, which means the "halting of blood," protects the individual from massive bleeding secondary to minor trauma. In pathologic states, however, thrombosis can occlude the microvasculature, leading to organ ischemia. Hemostasis is therefore highly regulated by a number of factors, including (1) vascular extracellular matrix and alterations in endothelial reactivity, (2) platelets, (3) coagulation proteins, (4) inhibitors of coagulation, and (5) fibrinolysis. Exposure of subendothelial vascular basement membrane activates platelets, and expression of tissue factor also activates thrombin generation and signals other inflammatory pathways. Platelet activation is an important mechanism for initiation of the coagulation cascade. Receptors on platelets bind to the damaged 837 emostasis is a critical homeostatic mechanism of survival that involves vascular, cellular, and plasma components that interact to stop bleeding. Surgery produces complex alterations and defects in hemostatic mechanisms, particularly in trauma, cardiac surgery with or without cardiopulmonary bypass, major orthopedic surgery, and neurosurgery. Vascular effects include vasoconstriction, expression of procoagulant factors such as tissue factor, and loss of normal anticoagulant functions of the endothelium. Coagulation and clot formation occur by cellular and humoral factors that interact together with local and systemic factors. In many patients, multiple quantitative and qualitative hemostatic abnormalities develop as part of surgery, tissue injury, and complex underlying medical conditions. Additionally, the increasing use of multiple anticoagulation agents to treat cardiovascular disease contributes to preexisting perioperative hemostatic defects and increases the potential for bleeding. Thrombin activates a positive feedback loop by producing more of itself, cleaves fibrinogen to insoluble fibrin, and activates platelets that release more procoagulant and inflammatory factors. Most patients with inherited risk factors for hypercoagulability are at risk to develop venous thromboembolic events early in life. Fibrinogen is an increasingly important target for therapeutic interventions in bleeding and coagulopathy. Similarly, patients with the highest plasma fibrinogen concentration have an approximately twofold increased risk for arterial thrombosis, and stroke patients with fibrinogen levels of 450 mg/dL or greater have poorer functional outcomes. Once platelets adhere, they undergo surface receptor changes that cause platelets to aggregate. Once platelets aggregate, they expose factors on their surface that provides a substrate for activation of the coagulation cascade and formation of the early hemostatic plug. Any abnormality in platelet number or function poses a significant risk for perioperative coagulopathy. Hypercoagulability Normal hemostasis is a balance between procoagulant and anticoagulant mechanisms. The coagulation system ensures that bleeding does not continue indefinitely after vascular injury. This is balanced by thromboresistant forces involving anticoagulant proteins to control clot formation and fibrinolytic proteins to remove clot once vascular injury has been repaired. A proper balance between these systems must be maintained to ensure the fluid nature of blood, yet be readily activated when pathologic activation occurs. Hypercoagulability, also known as thrombophilia or a prothrombotic state, is a condition in which blood clots more readily than normal. It results from a shift of the normal equilibrium of procoagulant and anticoagulant forces in favor of coagulation. Procoagulant forces (red) and natural anticoagulant/fibrinolytic forces (blue) are shown. Inherited risk factors are presented in diamond shapes with lettering and arrows indicating the mechanism for the hypercoagulable effect. This most commonly manifests as microthrombi within cutaneous vessels, a condition known as "warfarin skin necrosis. Heparin and related glycosaminoglycans are normally present on endothelial surfaces or administered therapeutically. Heterozygous antithrombin deficiency is associated with approximately 50% of normal levels, whereas homozygous antithrombin deficiency is likely always fatal in the newborn or in utero, and is exceedingly rare. Fibrinolysis Modulation Fibrinolysis regulates the extent of clot formation and vascular patency as part of hemostatic regulation. After tissue and vascular injury, multiple hemostatic mechanisms are initiated to modulate fibrinolysis. However, most acquired risk factors are multifactorial and have mechanisms that remain to be fully characterized. Procoagulant forces (red) and natural anticoagulant/fibrinolytic forces (blue) are diagrammed. Acquired risk factors are presented in diamond shapes with lettering and arrows indicating the mechanism for the hypercoagulable effect. Note that some acquired risk factors have multiple effects; see text for full details. Severe hepatic dysfunction and cirrhosis lead to decreased synthetic capabilities and decreased levels of anticoagulant factors, including antithrombin, protein C, protein S, and plasminogen. This, in turn, increases platelet activation and is an important cause of hypercoagulability. Although a low-flow state is a component of the Virchow triad, it alone does not create thrombosis. The importance of the other two Virchow factors- vessel wall abnormalities and dysfunctional blood constituents-is now becoming clear at the molecular level. Antibody-mediated endothelial injury and tissue factor production further increase the prothrombotic state. Although counterintuitive, bleeding is rare even in the presence of severe thrombocytopenia. This can be observed intraoperatively and can present as anaphylaxis, usually accompanied by acute thrombocytopenia. The mainstay agents include intravenous administration of a direct thrombin inhibitor, either argatroban or bivalirudin. Previously used agents that were derivatives of the leech protein hirudin are no longer available (desirudin, lepirudin). If heparin use is unavoidable or planned, the heparin exposure should be limited to the surgery itself, with alternative anticoagulation used preoperatively and postoperatively. If cardiac surgery is required, prospective studies have evaluated bivalirudin as the most investigated and useful alternative, although plasmapheresis has also been reported. Risk Factors for Bleeding Perioperative bleeding with increased transfusion requirements is caused by patient-related, procedure-related, and process-related factors. Surgery-induced tissue injury with both large vessel bleeding and microvascular bleeding can occur. Patients often have acquired defects that can be complicated by the surgical insult, or coagulation abnormalities that occur owing to antiplatelet or anticoagulant drug use or massive blood loss. Major coagulation abnormalities occur perioperatively and are influenced by multiple factors, including type of surgery, cardiopulmonary bypass, and preexisting abnormalities. Coagulopathic states and risk factors predisposing to surgical bleeding are listed in Tables 43. Patients with atherosclerotic cardiovascular disease often receive anticoagulation and/or antiplatelet therapies that interfere with hemostasis (see Chapter 45). Surgical patients have acquired changes in hemostasis that contribute to postoperative bleeding, including activation of coagulation, fibrinolytic, and inflammatory pathways. Congenital or acquired qualitative platelet defects increase bleeding risk (see earlier text).
After conventional measures to support the bleeding patient have failed prostate ultrasound 60ml rogaine 2 with amex, consideration of nonspecific bleeding reduction strategies may be warranted prostate cancer treatment options purchase rogaine 2 online now. Anti-fibrinolytic agents such as -amino caproic acid or tranexamic acid prostate cancer jokes purchase rogaine 2 60 ml without prescription, while not specific antidotes or procoagulant agents per se prostate what does it do purchase 60 ml rogaine 2 visa, can stabilize residual clot formation that may occur in the presence of antithrombotic therapy androgen hormone memes order line rogaine 2. Arterial Thrombosis Prophylaxis: Patients with a prior history or risk of arterial thrombosis, the major example being coronary artery disease and myocardial infarction, are often treated with drugs that target platelet receptors and enzymes. TxA2 binds to its cognate receptor and stimulates Ca2+ influx to result in platelet aggregation. However in cases of hemorrhage that require immediate treatment, a platelet transfusion may help by introducing functional platelets into circulation. Prasugrel however does not exhibit such variable response because it bypasses the activation step which makes it a more uniformly effective platelet function inhibitor. Platelet transfusion can be used in emergency cases of hemorrhage with variable efficacy. Lab-Guided Platelet Transfusion: With the availability of rapid platelet functional assays, an assessment of platelet inhibition level coupled with a platelet count could be performed to calculate the estimated number of functional circulating platelets. The patient can thus be transfused in a lab-guided fashion to achieve recommended functional platelet counts the procedure needs. No rigorous clinical data exists for the transfusion of platelets to patients treated with antiplatelet therapy so the above is only a proposal that has not been validated but it offers a rational, possibly reproducible method to treat. Of note, while the above tests have been used to predict anti-platelet therapy resistance, they cannot at this time predict bleeding tendency. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). However challenges to the provision of an adequate supply of safe blood are enormous in these resource-limited countries. Responses indicated that a national blood transfusion service existed in 38 countries and 32 had a blood transfusion policy, although only in 11 cases was this supported by legislation. The long-term sustainability of national systems should external aid decrease is a major concern for most of these countries, and this concern has contributed to a debate over the appropriate mixture of national or centralized systems versus more localized or regional centers. Whichever approaches are used, major challenges for the provision of safe blood in the developing world include the shortages of knowledgeable, skilled healthcare workers and the difficulty and cost of implementing quality systems in workplaces where these concepts are completely unknown. Blood Supply: the number of whole blood donations per 1000 population is an indicator of the general availability of blood in a country. A recent study evaluated the effect of blood shortages in the setting of obstetrical hemorrhage. The reason for the young donor ages is multifactorial, including the general age distribution of the populations of each country, but also reflect the fact that in many developing countries a large percentage of blood donations come from blood drives at high schools (where students are generally a few years older than their counterparts in high-income countries). In addition, in 47% of low-income countries testing is not performed in a quality assured manner. Finally a steady, reliable supply of test reagents remains a problem in several countries. More studies need to be done in these low-income countries, which often also have high donor seroprevalence rates and suboptimal quality assurance, in order to truly know what the residual risks are in any given region. Nevertheless, current data indicate that residual risks are, unfortunately, still, clearly orders of magnitude higher in much the developing world than in high-income countries. However, some access to components is beginning to be important even in low-income countries as they gradually introduce more sophisticated medical and surgical treatments. Large numbers of transfusions are used for the treatment of severe anemia in infants and young children. Accordingly, one important processing consideration is the availability of partial whole blood or red cell units. Measures that are routinely used in high-income countries to reduce transfusion complications are neither available nor affordable in low-income countries. These include pre-storage leukoreduction, bacterial testing, gamma-irradiation and avoidance of plasma-containing components from male donors. However, it is likely (though unfortunately not documented) that this relatively neglected component of the blood transfusion process represents an important weak link in the provision of safe transfusions. As well as the need for increased financial resources, there is a great need for the education of physicians, nurses and technologists in all aspects of transfusion medicine including their role in assuring transfusion safety. For example, in Denmark, 76% of all transfusions are given to patients over 65 years old, while in Benin (a low-income country in West Africa), 65% of all transfusions are given to children under 5 and 17% to females aged 14 to 45 years. Acute severe anemia in childhood requiring transfusion is frequently associated with malaria or sickle cell disease. However the development of severe anemia and the resultant need for transfusion (in children or adults) may also be related to an underlying state of chronic anemia. Given the limited access to laboratory testing and the late stage of illness at which patients typically present, it is likely that these causes of anemia are frequently treated with transfusions rather than with timely and optimal therapy of the basic underlying condition. As an example, the guidelines for transfusion of children with anemia are reproduced in Table 53. Other Blood Components: There is no precise information available on the use of other blood components in low-income countries. Their use is likely restricted to university-affiliated hospitals who offer some degree of specialized care such as cancer treatment and cardiovascular surgery, and who have access to at least limited laboratory support such as automated complete blood counts and basic coagulation testing. However even in these settings, basic equipment such as freezers and platelet agitators may not always be available. As they become more available, it will be essential to ensure such education if inappropriate use is to be avoided. It is therefore likely that blood that would be considered incompatible and therefore inappropriate for transfusion in the developed world is frequently being transfused in low-income countries. Hemoglobin concentration of 4g/dl or less (or hematocrit 12%), whatever the clinical condition of the patient. Hospital identification bands are rarely used and supplies of any sort for any step of the process, either on the hospital ward or in the blood bank may run out. Very few studies reporting acute transfusion reactions in resource-limited settings have been published. In the absence of patient monitoring during transfusion, it is likely that many acute transfusion reactions go unrecognized. Additionally, given the lack of systematic documentation of all steps in the transfusion process, traceability of blood units from donor to recipient is currently almost impossible in most low-income countries. Conclusion: As a specialty, transfusion medicine is in its infancy in the developing world. The importance of assuring transfusion safety within hospitals is still severely neglected. Hopefully attention to this equally vital component of transfusion safety will increase in low-income settings as it has recently in high-income countries. Maternal mortality in subSaharan Africa: the contribution of ineffective blood transfusion services. Blood transfusion safety in Africa: a literature review of infectious disease and organizational challenges. Estimate of the residual risk of transfusion-transmitted human immunodeficiency virus infection in sub-Saharan Africa: a multinational collaborative study. Resources are available in the hospital through legal and ethics consultation, and for many surgeries and diseases, the patient who refuses blood can have a similar outcome to transfusable patients when the correct systems are put in place. The use of blood derivatives, however, is not specifically prohibited, and the Watch Tower encourages members to personally decide whether accepting these component fractions violates the doctrine on blood. Examples of such potentially approved blood product derivatives include cryoprecipitate, albumin, immunoglobulin (including RhIg), clotting factor concentrates prepared from blood, and interleukins. While standard transfusions are unacceptable, there are some related procedures that are not specifically prohibited, including plasma exchange, dialysis, intraoperative blood salvage, hemodilution, blood donation strictly for the purpose of further fractionation of components, and transfusion of autologous blood as long as the continuous circuit with the patient remains. Transfusion of preoperatively donated autologous blood is, however, prohibited, due to the belief that blood should not be taken out of the body and stored (Table 54. The right of a competent adult to refuse consent for medical treatment is accepted, and documentation of refusal for transfusion should be placed in the medical record. Worst-case scenario discussions should be held, and documentation to this effect should also be included in the medical record. Most institutes have policies and documents specific to the consent (or refusal) to receive blood products. Some clinicians opt to have patients sign the notes stating these discussions were held. Some Specific Circumstances Require Additional Consideration: Trauma: Situations of trauma are difficult, in that Medical Directive cards may not be immediately available. Pregnant Women and Children: the treatment of pregnant women and children deserves special attention. Given that minor children are not considered capable of informed consent, it is recommended that the clinician seek legal intervention in cases where the fetus or child is placed at risk by parental refusal for transfusion. Blood Management: Conversations with the patient regarding treatment options should be held in private, to ensure confidentiality. Such options include blood conservation, optimizing coagulation as well as the use of non-blood adjunctive therapies. Blood conservation can be achieved by reducing blood loss through decreased phlebotomy and meticulous surgical care, intraoperative blood salvage, and/or acute normovolemic hemodilution. The potential complications of each of these treatments must be weighed carefully against their potential beneficial effects. The Hospital Information Services department of the Watch Tower Society has established Hospital Liaison Committees. These committees consist of ministers that are available to support physicians, patients, and social workers, and can be reached at 718-560-4300, hid. There are both non-immune and immune causes for platelet refractoriness (Table 55. The hospital transfusion service physician or his or her designee should communicate the evaluation steps for platelet refractory patients to the ordering physician, including: 1. Medications most commonly implicated in platelet refractoriness include amphotericin, heparin and vancomycin; other drugs implicated include antithymocyte globulin, granulocyte-macrophage colony-stimulating factor, granulocyte colony-stimulating factor, and interferons. Splenomegaly reduces both the post-transfusion platelet count increment and the time to next transfusion in comparison to individuals with normal spleens. In addition, platelets stored longer than 48 hours may have decreased viability following transfusion. In this assay, the serum from the alloimmunized patient is incubated with the apheresis platelet sample in specially treated wells, and the presence of alloantibodies 364 Suspect alloimmune refractoriness Jeanne E. Note, however, that a large number of products may need to be crossmatched to locate compatible products for broadly alloimmunized patients. Bleeding, Platelet Refractory Patient: Transfusion of large numbers of platelets is often attempted in bleeding, platelet-refractory patients, but may not result in a detectable increase in platelet count. Platelet transfusion for patients with cancer: clinical practice guidelines of the American Society of Clinical Oncology. Factors affecting posttransfusion platelet increments, platelet refractoriness, and platelet transfusion intervals in thrombocytopenic patients. Massive transfusion can occur in a variety of clinical settings, including cardiovascular, spinal and liver surgery; trauma; gastrointestinal bleeds; and obstetrics. Clinical Significance: the physiologic response to blood loss is to preferentially maintain tissue oxygenation to the brain and heart by shunting blood from other organs, shifting fluid from intracellular to extracellular space and from interstitial to intravascular space, and conserving water and electrolytes. Loss of up to 10% of blood volume results in few symptoms; loss of up to 20% does not usually cause signs or symptoms when the patient is at rest, but will result in tachycardia with exercise; and loss of up to 30% results in hypotension and tachycardia, especially with exercise. Once blood loss exceeds 30%, serious signs and symptoms of cardiovascular compromise occur, including tachycardia with weak pulse, hyperpnea, hypotension, decreased central venous pressure and cardiac output, and cold clammy skin. In the severely injured trauma patient, uncontrolled hemorrhage is one of the most common causes of mortality. Over the past three decades, hemorrhage has remained the ultimate cause of mortality in approximately 30% of trauma fatalities, second only to traumatic brain injury. Pregnancy is the leading cause of death among women of childbearing age worldwide. One potential difference in the management is the need for higher fibrinogen levels: women with fibrinogen levels >400 mg/dl did not develop postpartum hemorrhage. Thus incorporating fibrinogen level measurements and higher use of cryoprecipitate or fibrinogen concentrate in the care of these patients may be beneficial. Except in trauma and some obstetrical circumstances, massive transfusion for cardiac and liver transplantation (and other circumstances mentioned above) follows the general considerations below; however, few clinical trials exist to guide therapy in these and other massive transfusion situations. These other clinical situations may have different Transfusion Medicine and Hemostasis. Yet timely and appropriate access to blood products, as well as clear communication and multidisciplinary planning are paramount in the management of all massively bleeding patients. Crystalloid versus Colloid Replacement: Crystalloids distribute quickly into total body water and can cause peripheral and pulmonary edema, but are less expensive than colloid solutions. Colloid solutions primarily remain (at least initially) intravascular, but are more expensive and can cause allergic reactions. In addition, the current goal of volume resuscitation is euvolemia, and sometimes hypotensive resuscitation, and to avoid supra-normal resuscitation. Euvolemia entails moderate volume resuscitation with the possible use of vasopressor agents to support hemodynamics.
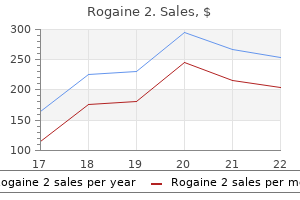
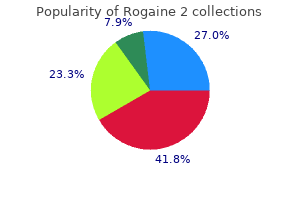
Colloid replacement therapy might still be indicated in early volume resuscitation after acute blood loss prostate oncology williston purchase cheap rogaine 2. Extravascular (subendothelial) collagen and tissue factor are exposed to the flowing blood prostate tuna generic 60 ml rogaine 2 visa. The intact vascular wall (blue) mens health zimbabwe order rogaine 2 pills in toronto, platelets (white ovals) prostate cancer young men order rogaine 2 60 ml without a prescription, erythrocytes (red circles) mens health 6 pack challenge 2013 cheap rogaine 2 60 ml visa, and fibrin (green) are depicted. Platelet transfusion and measures to increase von Willebrand factor can augment this process. These factors can be replaced using plasma transfusion or specific factor concentrates (see text for details). In order to decrease multiple donor exposures, single-donor platelet apheresis is increasingly used. During the apheresis procedure, donor blood is placed in the extracorporeal circuit and centrifuged to separate platelets. Clinical Uses Platelet transfusion is used to prevent or treat bleeding due to platelet dysfunction or thrombocytopenia. Platelet transfusion can be required even with a normal platelet count if platelet dysfunction is clinically suspected or identified by platelet function testing. The lack of virus reduction procedures for platelet concentrates has been a major concern, and transmissions of Zika virus via platelet transfusion were recently reported. Further clinical validations are needed as to its indications and efficacies against emerging pathogens. Problems due to platelet alloimmunization include refractoriness to platelet transfusion and post-transfusion purpura. This typically occurs after group O platelet transfusion in non-group O recipients. However, other plasma products have been increasingly used to make up the shortfall in plasma supply in the United States. The recovery of coagulation factors after each plasma unit is about 2% to 3% in the adult but can vary with donors, clinical hemorrhage, and/ or ongoing consumption. Leukoreduced plasma undergoes pathogen reduction steps, including amotosalen and ultraviolet light (Intercept Blood System). The plasma is subsequently aliquoted in an individual flask and freeze-dried over 4 days. Each bottle of powdered plasma is reconstituted with 200 mL of sterile water before transfusion. For congenital factor deficiency, plasma transfusion should be considered only if recombinant or plasma-derived factor concentrate is not available (Table 44. Plasma products are sometimes transfused prophylactically before invasive procedures when risk of bleeding is high, but there is limited evidence and no cut-off level for any coagulation test that clearly indicates the need for plasma. Plasma can be used as a replacement fluid (plasma exchange) in patients undergoing therapeutic plasma exchange (apheresis). The risk of fluid overload owing to a large volume of plasma transfusion should be considered in patients with limited cardiovascular reserve. Hypocalcemia can result from citrate accumulation after plasma transfusion, and is treated with calcium chloride or gluconate. Risk of viral transmission has been reduced significantly since the 1990s by implementing nucleic acid testing for human immunodeficiency virus and hepatitis C virus. The minimal level of plasma fibrinogen to minimize perioperative bleeding has not been established. Each unit contains 150 to 250 mg of fibrinogen; 5 to 10 units are thawed and pooled before infusion (Table 44. Each unit of cryoprecipitate increases plasma fibrinogen by approximately 100 mg/dL per 5 kg body weight. The volume of cryoprecipitate required to Side Effects Exposure to multiple donors from pooled cryoprecipitate units is a major concern since no viral inactivation procedure is clinically available. Fibrinogen Concentrate Fibrinogen concentrate is a lyophilized product prepared from plasma. It can be rapidly reconstituted and administered intravenously because no thawing or blood type matching is required. The incidence of thromboembolic complications appears to be nearly 7-fold higher in those without congenital factor deficiency. Several small retrospective clinical studies have demonstrated hemostatic effects of fibrinogen replacement after complex cardiac surgical cases,104,105 but the results of recent prospective randomized trials for fibrinogen replacement in cardiac surgery are mixed (Table 44. Four-factor prothrombin complex concentrate versus plasma for rapid vitamin K antagonist reversal in patients needing urgent surgical or invasive interventions: a phase 3b, open-label, non-inferiority, randomised trial. Elevated systemic thrombin activity thus increases protein C activation as observed in thrombophilia,138 sepsis,139 and traumatic injury. Local and systemic regulation of coagulation and fibrinolysis at a site of vascular injury are shown. Lessons from the aprotinin saga: current perspective on antifibrinolytic therapy in cardiac surgery. The infectious risk of plasma-derived protein C is low owing to viral inactivation steps, including polysorbate-80, vapor-heat, and ion exchange chromatography. Precautions for use include bleeding, sodium overload, rare allergic reactions and heparin-induced thrombocytopenia due to trace amounts of heparin. Clinical use of aprotinin has been resumed but is limited to coronary bypass grafting surgery in Canada and Europe after its suspension from 2007 to 2012 owing to safety concerns. Antifibrinolytic therapy appears to be useful in bleeding associated with menorrhagia 149 and chronic thrombocytopenia. With renal or ureteral bleeding, lysine analogs can increase the risk of ureteral obstruction due to clot formation. In mild to moderate von Willebrand disease and hemophilia A, intravenous desmopressin (0. Desmopressin is often administered to patients with preexisting platelet dysfunction related to antiplatelet drugs and uremia. Disadvantages include inactivation of natural clotting enzymes, such as thrombin, and potential for inflammation and delayed wound healing. Microfibrillar collagen (Avitene, Bard) increases local platelet adhesion and activation, leading to hemostasis within 5 minutes. The collagen particles do not cause much swelling and are reabsorbed within 8 weeks. They are supplied with separate vials of fibrinogen, thrombin, and calcium chloride that are mixed at the wound by a dual-syringe applicator. A patch sponge (TachoSil, Baxter) impregnated with lyophilized human fibrinogen and thrombin is also available for treatment of raw surface bleeding. To prevent viral transmission from the human plasma, fibrinogen and thrombin are treated with solvent-detergent, nanofiltration or vapor-heat. Gelatin forms (Gelfoam, Pfizer; Gelfilm, Pfizer; Surgiform, Surgiform Technology, Ltd. Another gelatin-based sealant (FloSeal, Baxter) is a mixture of human thrombin and bovine-derived gelatin-based matrix. Thrombin generates fibrin from blood fibrinogen and the gelatin particles expand to tamponade bleeding. These topical agents are generally safe and useful adjuncts for hemostasis when used for appropriate indications and anatomic sites. The extent of coagulopathy varies with the type and stage of liver and biliary tract disease. The policy on blood transfusion was changed recently-acceptance of fractionated products of "primary components" was left to the individual believer (Table 44. Improved pathogen detection in donors and pathogen reduction treatments should allow increasingly safer supplies of allogeneic blood products. Expedited surgical control of bleeding is crucial in improving morbidity and mortality, and there does not appear to be any specific ratio of blood products that can be recommended. The use of thromboelastography/thromboelastometry can be helpful in the selection of hemostatic product(s). Use of factor concentrates in acquired factor deficiency is generally considered to be off-label, but there are some supportive data available for certain indications. The proper indication(s) and site(s) should be considered to reduce untoward complications. Notably, fluid overload or similar cardiac events were more frequent in the plasma group (3% vs. Improved hemostasis was more frequently observed in the 1:1:1 group than in the 1:1:2 group (86. The increased donor exposure was evident in the 1:1:1 group (median 19 U plasma plus platelets vs. This study failed to point to the optimal ratio (or volume) of plasma and platelet transfusion. Fibrinogen or fibrin polymerization was not continuously monitored and cryoprecipitate was seldom used in either group of patients (median, 0 unit). In addition, the incidences of major hemorrhage or cardiac tamponade leading to reoperation were reduced by 50% (P = 0. Thromboelastometry-guided intraoperative haemostatic management reduces bleeding and red cell transfusion after paediatric cardiac surgery. Platelets and plasma were the only 2 products available for hemostatic therapy during the study. Hyperfibrinolysis was evident on thromboelastometry in only 5% of patients, while plasma fibrinolysis markers were elevated in 57% of patients in proportion to the base deficit and hypotension on admission. The 28-day mortality of patients with hyperfibrinolysis on thromboelastometry was 40%, whereas it was 12% in those with elevated plasma fibrinolysis markers. These data suggest that hyperfibrinolysis on thromboelastometry represents a marker of worse prognosis and that antifibrinolytic therapy should be considered according to the injury severity regardless of the thromboelastometry findings. Patient blood management the pragmatic solution for the problems with blood transfusions. Effect of a patient blood management programme on preoperative anaemia, transfusion rate, and outcome after primary hip or knee arthroplasty: a quality improvement cycle. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology. Practice guidelines for perioperative blood transfusion and adjuvant therapies: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies. Cross-sectional guidelines for therapy with blood components and plasma derivatives. Storage, and Transportation, Blood Banking and Transfusion Medicine: Basic Principles and Practice, 2nd Ed. Restrictive versus liberal transfusion strategy in the perioperative and acute care settings: a context-specific 24. Randomised trial of blood transfusion versus a restrictive transfusion policy after hip fracture surgery. Efficacy and safety of erythropoietin and intravenous iron in perioperative blood management: a systematic review. A single dose of erythropoietin reduces perioperative transfusions in cardiac surgery: results of a prospective single-blind randomized controlled trial. The role of albumin as a resuscitation fluid for patients with sepsis: a systematic review and meta-analysis. Fibrinogen estimates are influenced by methods of measurement and hemodilution with colloid plasma expanders. Blood platelets are concentrated near the wall and red blood cells, in the center in flowing blood. Multiple electrode whole-blood aggregometry and bleeding in cardiac surgery patients receiving thienopyridines. Prophylactic platelet transfusion for prevention of bleeding in patients with haematological disorders after chemotherapy and stem cell transplantation. Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup: surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Thresholds for perioperative administration of hemostatic blood components and coagulation factor concentrates: an unmet medical need. Goal-directed hemostatic resuscitation of trauma-induced coagulopathy: a pragmatic randomized clinical trial comparing a viscoelastic assay to conventional coagulation assays.
Palpation of a direct inguinal hernia is performed by placing the palmar surface of the index and/or middle finger over the inguinal triangle and asking the person to cough or bear down (strain) prostate zero order rogaine 2 with a visa. The finger can also be placed in the superficial inguinal ring; if a direct hernia is present prostate information best buy rogaine 2, a sudden impulse is felt medial to the finger when the person coughs or bears down prostate health and sex rogaine 2 60 ml for sale. Cysts and Hernias of Canal of Nuck Indirect inguinal hernias can occur in women; however prostate miracle buy 60ml rogaine 2 mastercard, they are approximately 20 times more common in men man health daily relationships category purchase rogaine 2 60ml fast delivery. If the processus vaginalis persists in females, it forms a small peritoneal pouch, the canal of Nuck, in the inguinal canal that may extend to the labium majus. The size of the hydrocele depends on how much of the processus vaginalis persists. Detection of a hydrocele requires transillumination, a procedure during which a bright light is applied to the side of the scrotal enlargement in a darkened room. Blood does not transilluminate; therefore, transillumination can differentiate a hematocele or hematoma from a hydrocele. Characteristic Predisposing factors Direct (Acquired) Weakness of anterior abdominal wall in inguinal triangle. The appendices of the epididymis are remnants of the cranial end of the mesonephric (wolffian) duct, the embryonic genital duct that in the male forms part of the ductus deferens. Varicocele the vine-like pampiniform plexus of veins may become dilated (varicose) and tortuous, producing a varicocele, which is usually visible only when the man is standing or straining. The enlargement usually disappears when the person lies down, particularly if the scrotum is ele- vated while supine, allowing gravity to empty the veins. Varicoceles may result from defective valves in the testicular vein, but kidney or renal vein problems can also result in distension of the pampiniform veins. Cancer of Testis and Scrotum Lymphogenous metastasis is common to all testicular tumors, so a knowledge of lymphatic drainage is helpful in treatment (Kumar et al. Metastasis of testicular cancer may also occur by hematogenous spread of cancer cells (via the blood) to the lungs, liver, brain, and bone. The fatty layer of subcutaneous tissue of the abdominal wall is replaced in the scrotum by the smooth dartos muscle, whereas the membranous layer is continued as the dartos fascia and scrotal septum. Testes: the testes are the male gonads, shaped and sized like large olives or small plums, that produce sperms and male hormones. The epididymis clings to the more protected superior and posterior aspects of the testis. The peritoneum consists of two continuous layers: the parietal peritoneum, which lines the internal surface of the abdominopelvic wall, and the visceral peritoneum, which invests viscera such as the stomach and intestines. Like the overlying skin, the peritoneum lining the interior of the body wall is sensitive to pressure, pain, heat and cold, and laceration. The pain produced is poorly localized, being referred to the dermatomes of the spinal ganglia providing the sensory fibers, particularly to midline portions of these dermatomes. Intraperitoneal in this case does not mean inside the peritoneal cavity (although the term is used clinically for substances injected into this cavity). Intraperitoneal organs have conceptually, if not literally, invaginated into the closed sac, like pressing your fist into an inflated balloon (see the discussion of potential spaces in the Introduction). Similarly, the subperitoneal urinary bladder has parietal peritoneum only on its superior surface. The dark arrow passes from the greater sac of the peritoneal cavity (P) through the omental (epiploic) foramen and across the full extent of the omental bursa (lesser sac). As the organs develop, they invaginate (protrude) to varying degrees into the peritoneal sac, acquiring a peritoneal covering, the visceral peritoneum. Other viscera, such as the stomach and spleen, protrude completely into the peritoneal sac and are almost completely invested by visceral peritoneum-that is, they are intraperitoneal. Intraperitoneal viscera with a mesentery, such as most of the small intestine, are mobile, the degree of which varies with the length of the mesentery. Although the liver and spleen do not change shape as a result of intrinsic activity (although they may slowly change in size when engorged with blood), their need for a covering of visceral peritoneum is dictated by the need to accommodate passive changes in position imposed by the adjacent, highly active diaphragm. Peritoneal fluid lubricates the peritoneal surfaces, enabling the viscera to move over each other without friction, and allowing the movements of digestion. In addition to lubricating the surfaces of the viscera, the peritoneal fluid contains leukocytes and antibodies that resist infection. However, there is a communication pathway in females to the exterior of the body through the uterine tubes, uterine cavity, and vagina. This communication constitutes a potential pathway of infection from the exterior. It undergoes exuberant growth, however, to provide the large absorptive surface required by nutrition. By the end of the 10th week of development, the gut is much longer than the body that contains it. For this increase in length to occur, the gut must gain freedom of movement relative to the body wall at an early stage, while still maintaining the connection with it necessary for innervation and blood supply. The rate of growth of the gut initially outpaces the development of adequate space within the trunk (body), and for a time the rapidly lengthening gut extends outside the developing anterior body wall (see "Brief Review of the Embryological Rotation of the Midgut," on p. Starting from the primordial position, suspended from the midline of the posterior abdominal wall (A), the mesocolon shifts to the left (B) and gradually fuses with the left posterior parietal peritoneum (C). The arrow indicates the left paracolic gutter, the site where an incision is made during mobilization of the colon during surgery. Sometimes the descending colon retains a short mesentery, similar to the stage shown in C, especially where the colon is in the iliac fossa. The mesentery is held there until the layer of peritoneum that formed the left side of the mesentery and the part of the visceral peritoneum of the colon lying against the body wall fuse with the parietal peritoneum of the body wall. The descending colon (as well as the ascending colon on the right side) has thus become secondarily retroperitoneal, having once been intraperitoneal (Moore et al. The layers of peritoneum that fused now form a fusion fascia, a connective tissue plane in which the nerves and vessels of the descending colon continue to lie. However, the roots of the short mesenteries do not remain attached to the midline but shift to the left or right by a fusion process like that described for the descending colon. A mesentery is a double layer of peritoneum that occurs as a result of the invagination of the peritoneum by an organ and constitutes a continuity of the visceral and parietal peritoneum. A mesentery connects an intraperitoneal organ to the body wall-usually the posterior abdominal wall. The mesentery of the jejunum and ileum (small intestine) and sigmoid mesocolon have been cut close to their parietal attachments. This median section of the abdominopelvic cavity of a male shows the relationships of the peritoneal attachments. The greater omentum is shown in its "normal" position, covering most of the abdominal viscera. The greater omentum has been removed from the greater curvature of the stomach and transverse colon to reveal the intestines. The greater omentum has been reflected superiorly, and the small intestine has been retracted to the right side to reveal the mesentery of the small intestine and the transverse mesocolon. All these structures have a continuous attachment along the greater curvature of the stomach, and are all part of the greater omentum, separated only for descriptive purposes. Such areas are called bare areas, formed in relation to the attachments of the peritoneal formations to the organs, including mesenteries, omenta, and ligaments that convey the neurovascular structures. A peritoneal fold is a reflection of peritoneum that is raised from the body wall by underlying blood vessels, ducts, and ligaments formed by obliterated fetal vessels. The central part of the greater omentum has been cut out to show its relation to the transverse colon and mesocolon. The hepatoduodenal ligament (free edge of lesser omentum) conveys the portal triad: hepatic artery, bile duct, and portal vein. This median section of the abdominopelvic cavity shows the subdivisions of the peritoneal cavity. This section shows that the omental bursa is an isolated part of the peritoneal cavity, lying dorsal to the stomach and extending superiorly to the liver and diaphragm (superior recess) and inferiorly between the layers of the greater omentum (inferior recess). The red arrows pass from the greater sac through the omental foramen into the omental bursa. The index finger is passing from the greater sac through the omental foramen into the omental bursa (lesser sac). A primary mechanism in preventing such infection is a mucous plug that effectively blocks the external os (opening) of the uterus to most pathogens, but not to sperms. The patency of the uterine tubes can be tested clinically by means of a technique in which air or radiopaque dye is injected into the uterine cavity, from which it normally flows through the uterine tubes into the peritoneal cavity (hysterosalpingography; see Chapter 3 for more details). It is more difficult to achieve watertight anastomoses of extraperitoneal structures that have an outer adventitial layer, such as the thoracic esophagus. The Peritoneum and Surgical Procedures Because the peritoneum is well innervated, patients undergoing abdominal surgery experience more pain with large, invasive, open incisions of the peritoneum Peritonitis and Ascites When bacterial contamination occurs during laparotomy, or when the gut is traumatically penetrated or ruptured as the result of infection and inflammation. Occasionally, more localized accumulations of fluid may have to be removed for analysis. The needle is inserted superior to the empty urinary bladder, in a location that avoids the inferior epigastric artery. Exudation of serum, fibrin, cells, and pus into the peritoneal cavity occurs, accompanied by pain in the overlying skin and an increase in the tone of the anterolateral abdominal muscles. Given the extent of the peritoneal surfaces and the rapid absorption of material, including bacterial toxins, from the peritoneal cavity, when a peritonitis becomes generalized (widespread in the peritoneal cavity), the condition is dangerous and perhaps lethal. General peritonitis also occurs when an ulcer perforates the wall of the stomach or duodenum, spilling acid content into the peritoneal cavity. Ascites may also occur as a result of mechanical injury (which may also produce internal bleeding) or other pathological conditions, such as portal hypertension (venous congestion), widespread metastasis of cancer cells to the abdominal viscera, and starvation (when plasma proteins fail to be produced, altering concentration gradients and producing a paradoxically protuberant abdomen). In all these cases, the peritoneal cavity may be distended with several liters of abnormal fluid, interfering with movements of the viscera. If the abdomen is drawn in as the chest expands (paradoxical abdominothoracic rhythm) and muscle rigidity is present, either peritonitis or pneumonitis (inflammation of the lungs) may be present. Because the intense pain worsens with movement, people with peritonitis commonly lie with their knees flexed to relax their anterolateral abdominal muscles. Intraperitoneal Injection and Peritoneal Dialysis the peritoneum is a semipermeable membrane with an extensive surface area, much of which (subdiaphragmatic portions in particular) overlies blood and lymphatic capillary beds. For this reason, anesthetic agents, such as solutions of barbiturate compounds, may be injected into the peritoneal cavity by intraperitoneal (I. In renal failure, waste products such as urea accumulate in the blood and tissues and ultimately reach fatal levels. Peritoneal dialysis may be performed in which soluble substances and excess water are removed from the system by transfer across the peritoneum, using a dilute sterile solution that is introduced into the peritoneal cavity on one side and then drained from the other side. For the long term, it is preferable to use direct blood flow through a renal dialysis machine. Peritoneal Adhesions and Adhesiotomy If the peritoneum is damaged, by a stab wound for example, or infected, the peritoneal surfaces become inflamed, making them sticky with fibrin. This tethering may cause chronic pain or emergency complications such as intestinal obstruction when the intestine becomes twisted around an adhesion (volvulus). Functions of Greater Omentum the greater omentum, large and fat laden, prevents the visceral peritoneum from adhering to the parietal peritoneum. It often forms adhesions adjacent to an inflamed organ, such as the appendix, sometimes walling it off and thereby protecting other viscera from it. The abscess may be walled inferiorly by adhesions (see the blue box "Subphrenic Abscesses," p. Fluid in Omental Bursa Perforation of the posterior wall of the stomach results in the passage of its fluid contents into the omental bursa. The recesses determine the extent and direction of the spread of fluids that may enter the peritoneal cavity when an organ is diseased or injured. As none of the boundaries of the foramen can be incised because each contains blood vessels, the swollen intestine must be decompressed using a needle so it can be returned to the greater sac of the peritoneal cavity through the omental foramen. Purulent material (consisting of or containing pus) in the abdomen can be transported along the paracolic gutters into the pelvis, especially when the person is upright. Conversely, infections in the pelvis may extend superiorly to a subphrenic recess situated under the diaphragm (see the blue box "Subphrenic Abscesses," p. Similarly, the paracolic gutters provide pathways for the spread of cancer cells that have sloughed Severance of Cystic Artery the cystic artery must be ligated or clamped and then severed during cholecystectomy, removal of the gallbladder. Alternate compression and release of pressure on the hepatic artery allows the surgeon to identify the bleeding artery and clamp it.
Purchase rogaine 2 60 ml overnight delivery. How To Plan Vegan Bodybuilding Meals | High Protein.
References
- Kuestner LM, Reilly LM, Jicha DL, et al: Secondary aortoenteric fistula: Contemporary outcome with use of extraanatomic bypass and infected graft excision. J Vasc Surg 21:184, 1995.
- Genrich GL, Guarner J, Paddock CD, et al. Fatal malaria infection in travelers: novel immunohistochemical assays for the detection of Plasmodium falciparum in tissues and implications for pathogenesis. Am J Trop Med Hyg 2007;76(2):251-9.
- Brown DD, Juhl RP, Warner SL. Decreased bioavailability of digoxin due to hypocholesterolemic interventions. Circulation. 1978;58:164-172.
- Tobacman LS: Thin filament-mediated regulation of cardiac contraction, Annu Rev Physiol 58:447-481, 1996.
- Moriai T: Clinical course of acute gastric mucosal lesions caused by acute infection with Helicobacter pylori. N Engl J Med 341:456, 1999.
- Ocaranza MP, et al. Protective role of the ACE2/Ang-(1-9) axis in cardiovascular remodeling. Int J Hypertens 2012;2012:594 361.