Thomas G. Lynch MD, FACS
- Professor of Surgery
- Chief, Vascular Surgery, University of Nebraska Medical
- Center
- Chief Surgical Service, VA Nebraska Western Iowa Health Care System,
- Omaha, Nebrasha
Rare variations have even shown the inferior vermian veins to drain into the straight sinus medications every 8 hours discount quetiapine online mastercard. This pathology is also associated with an upward tenting of the tentorium cerebelli in three of four cases reported by Rosa et al medicine bg purchase quetiapine paypal. Brain herniations into arachnoid granulations of the straight sinus, although extremely rare, have been reported in 1 out of 68 patients. Cranium bifidum with malformation of the straight sinus is rare but has been reported. The straight sinus was also positioned abnormally high and an elongated great vein of Galen. Transverse-sigmoid sinus dural arteriovenous fistula presenting with parkinsonism. Idiopathic hypertrophic cranial pachymeningitis associated with a dural arteriovenous fistula involving the straight sinus: case report. Brain herniations into arachnoid granulations: about 68 cases in 38 patients and review of the literature. A case of occult cranium bifidum combined with abnormal high position of the straight sinus. Interobserver agreement in the magnetic resonance location of cerebral vein and dural sinus thrombosis. Tentorial dural arteriovenous fistulae: operative strategies and microsurgical results for six types. Developmental deep venous system Anomaly associated with congenital malformation of the brain. Arachnoid granulations-computerized tomography and magnetic resonance imaging features: a case report. Moreover, more recent, minimally invasive intravascular procedures necessitate sampling blood from this sinus. Therefore, detailed knowledge of its anatomy and variations is important in clinical practice. It drains the cavernous sinus and receives inflow from the auditory structures and drains into the sigmoid sinus and the superior jugular bulb on each side. In the early stages of development of the cerebral venous system, the vena capitis medialis, or the medial head vein, can be seen lying medial to the emerging cranial nerve roots and otic vesicle. In adults, however, the junction occurs at the anterior surface of the jugular bulb. The deep system consists of the lateral sinus, straight sinus, and sigmoid sinus along with draining deeper cortical veins. The superficial system comprises sagittal sinuses and cortical veins, which drain superficial surfaces of both cerebral hemispheres. It rests in the lower parts of the foramen and has no relationship with the jugular foramen in about 7% of people. Benndorf and Campi16 reported two similar cases in patients undergoing endovascular management of cavernous sinus lesions. In nine sinuses, it was slightly above the jugular foramen, and in five sinuses, it was slightly below the jugular foramen. Any one of these may be more dominant, but in the majority of people, these anastomotic channels/landmarks are symmetric. Variation in Inferior Petrosal Sinus-Internal Jugular Vein Communication In 1968, Shiu et al. However, instead of draining into the superior jugular bulb, it drains into the deep cervical plexus of veins. The intensity of venous thrombosis varies with time and the state of the thrombosis within the sinuses on planar imaging. Variations of the course within the jugular foramen was also examined in 20 specimens by Rubinstein et al. The intracranial bridging veins: a comprehensive review of their history, anatomy, histology, pathology, and neurosurgical implications. The inferior petrosal sinus: a comprehensive review with emphasis on clinical implications. Anatomy of the junction of the inferior petrosal sinus and the internal jugular vein. Diagnostic tests and procedures that aid in establishing the presence of hypercortisolemia include urinary-free cortisol, late-night salivary cortisol, and the low dexamethasone suppression test. Its specificity and sensitivity were found to be 96% and 100%, respectively, according to a metaanalysis review of 21 studies. Hand injection of the contrast is then used to highlight the anatomy of the venous structures. Samples are taken before and after corticotropin-releasing hormone administration. Anatomical relationships of the cerebral and dural venous systems in the parasagittal area. The cranial venous system in man in reference to development, adult configuration and relation to the arteries. Anatomical variation of the superior petrosal vein and its management during surgery for cerebellopontine angle meningiomas. Aberrant inferior petrosal sinus: unusual transvenous approach to the cavernous sinus. The anatomy of the inferior petrosal sinus, glossopharyngeal nerve, vagus nerve, and accessory nerve in the jugular foramen. Morphologic evaluation of the caudal end of the inferior petrosal sinus using 3D rotational venography. Complications related to percutaneous transarterial embolization of intracranial dural arteriovenous fistulas in 40 patients. The Role of Bilateral Inferior Petrosal Sinus Sampling in the Diagnostic Evaluation of Cushing Disease; 2011. This author also described the connection of this sinus with the cavernous sinus as having a shape of the letter. The venous receptive function of the superior petrosal sinus is vast, consisting of the veins of the pons, upper medulla oblongata, cerebellum, and the inner ear. They also act in concert with the inferior petrosal sinus to drain the interior of the bones of the skull. This mater is impressed upon the temporal bones as they open into the cavernous sinuses and terminate in the transverse sinus. The primary venous plexus of the head divides into three strata: outer, middle, and deeper. This mesh of this venous network further divides into three strata: outer, middle, and deeper head plexuses. The deeper plexus of the head connects with the superficial plexus via intermediate channels. These intermediate channels are eventually obliterated with the development of the meninges that grow from the base of the skull and gradually extend dorsally around the neural tube to the vertex of the head. Changes in the stem of the middle dural plexus and the middle section of the primary head vein result in the superior petrosal sinus, which lies in the cavum epiptericum close to the anterior layer of the tentorium cerebelli. It later joins the cavernous sinus and then rests beneath the trigeminal ganglion and between the oculomotor and trochlear nerves. Both right and left sinuses passed under the trigeminal nerve root in three cases. The sinus divided on both sides in three cases with some portions passing under the trigeminal root and others passing over the trigeminal nerve root. Occasionally, the superior petrosal sinus may communicate with the superior ophthalmic veins through an aberrant vein termed the ophthalmopetrosal sinus in up to 9% of the cases, according to Knott. In type A, which is the most common, the superior petrosal sinus runs along the lesser sphenoid wing and connects with the anterior aspect of the cavernous sinus. In type B sinuses, the superior petrosal sinus runs along the lesser sphenoid wing and connects with the foramen ovale venous plexus or the pterygoid venous plexus, in addition to the anterior aspect of the cavernous sinus.
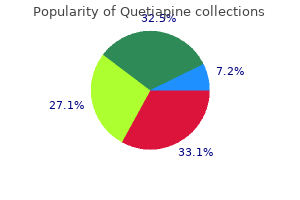
Type a (72%): the sphenoparietal sinus coursed along the lesser sphenoid wing and connected with the anterior aspect of the cavernous sinus symptoms pneumonia order quetiapine 100mg. Type b (4%): the sphenoparietal sinus coursed along the lesser sphenoid wing and connected with the foramen ovale venous plexus or the pterygoid venous plexus medications that cause constipation discount quetiapine 50mg visa. It might be found unilaterally or bilaterally and is more common on the left side. It arises from the dorsolateral portion of the transverse sinus at the junction with the sigmoid sinus and before the confluence with the transverse sinus with the superior petrosal sinus. It may also drain the posterior temporal diploic vein and the emissary veins of the cranial fossa. Stewart131 reported the there was some association between the petrosquamous and the passage of infection from the middle ear to the brain. Small veins from the middle ear may drain through the petrosquamous fissure into this sinus. In two of the five cases, a connection with the emissary veins of the foramen ovale was observed. The anterior portion of petrosquamous sinus in 1 of the cases divided into two branches: a medial and a lateral branch, which connected extracranially to the deep temporal vein. The petrosquamous sinus had an irregular contour and a tortuous course in three cases. When the sigmoid sinus is absent or underdeveloped, the petrosquamous sinus may serve as the main outflow pathway of the transverse sinus. It had an anterior-lateral and anterior-medial branch that connected it to the external jugular vein. The anterior lateral branch communicated with the deep temporal veins and the anterior-medial branch communicated with the emissary veins of the middle cranial fossa. The anterior-lateral branch left the skull through the postglenoid foramen located in the temporal squama. Of these 19 cases, 11 were found on the left side and 8 were found on the right side. In five specimens, the anterior intercavernous sinus occupied the entire anterior wall of the sella turcica. Six specimens had an inferior intercavernous sinus, which was much smaller than the other intercavernous sinuses. It was the broadest intercavernous connection in three cases and occupied the entire sella turcica in 17 cases. A posterior intercavernous sinus was the widest interconnection in one case and was also found in all specimens. This sinus passes backward from the superior orbital fissure over the greater wing of the sphenoid and petrous portion of the temporal bone and terminates in the transverse sinus. Of the 23 skulls, 16 showed it on both sides and the remainder showed it only on the left side. In 12 cases, instead of the circular sinus, Knott6 found a single intercavernous vein beneath the pituitary body. The inferior intercavernous sinus presented in three different ways on the floor of the sella turcica. Renn and Rhoton133 found that 76% had an anterior intercavernous sinus and 32% had a posterior intercavernous sinus. They also noted that the anterior intercavernous sinuses were usually larger than the posterior intercavernous sinuses; however, either one or both can be absent. Congenital duplication of the superior sagittal sinus and parietal encephalocele after vacuum extraction delivery. The superficial sylvian vein in humans: with special reference to its termination. Ueber otologisch wichtige anormalien der hirnsinus, uber accessorische sinus und bedeutendere venenverbindungen. Anatomical variants of the emissary veins: unilateral aplasia of both the sigmoid sinus and the internal jugular vein and development of the petrosquamosal sinus. Anatomic variations of the deep cerebral veins,tributaries of basal vein of Rosenthal: embryologic aspects of the regressed embryonic tentorial sinus. Anatomical variations of the straight sinus on magnetic resonance imaging in the infratentorial supracerebellar approach to pineal region tumors. The circular sinus: an anatomic study with neurosurgical and neurointerventional applications. The relationship between the superior petrosal sinus and the porus trigeminus: an anatomical study/laboratory investigation. Anatomy of the inferior petro-occipital vein and its relation to the base of the skull: application to surgical and endovascular procedures of the skull base. A note on the superior petrosal sinus and its relation to the sensory root of the trigeminal nerve. The foramina of the middle cranial fossa: a phylogenetic, anatomic and pathologic study. Venous consideration in petrosal approach: microsurgical anatomy of the temporal bridging vein. Anatomy of cranial blood sinuses with particular reference to the lateral sinuses. Cranial venous sinuses, correlation between skull markings and roentgenograms of the occipital bone. A complex dural-venous variation in the posterior cranial fossa: a triplicate falx cerebelli and an aberrant venous sinus. Persistence of multiple emissary veins of posterior fossa with unusual origin of left petrosquamosal sinus from mastoid emissary. Morphology of the temporal canal and postglenoid foramen with reference to the size of the jugular foramen in man and selected species of animals. The persistence of fetal blood sinuses and their relation to the middle ear spaces. Two cases of petrosquamosal sinus in the temporal bone presented as perioperative finding. They collect venous blood from the brain, meninges, and calvaria and deliver it to the internal jugular veins at the skull base. These sinuses converge at the torcular Herophili and drain the blood into the internal jugular veins. This system collects the blood at the cavernous sinuses and then drains either into the pterygoid plexus or via the inferior petrosal sinuses, basilar plexus into the internal jugular vein. It also allows simultaneous acquisition of low- and high-energy data in one examination and thus allows simultaneous imaging without interscan motion and with the use of only a small additional radiation dose in contrast to conventional bone subtraction technique. High-signal intensity of the inflowing fully magnetized blood contrasts against the low-signal intensity of stationary tissue. Limitations include artifactual intravascular signal loss due to insensitivity to in-plane flow or due to tortuosity and turbulent flow, high signal from background substances with short T1 values and patient motion causing vessel misregistration. Advantages include the ability to quantify flow and determine the direction of flow and greater suppression of the background tissues. The main disadvantage is low spatial resolution compared with the other contrast-enhanced sequences. Moreover, paramagnetic effects of the contrast agent shorten the intravascular T1 relaxation time resulting in increased signal intensity of the blood without saturation effects. Advantages include enhanced visualization of the vasculature, faster acquisition times, suppression of the background tissues, and avoidance of the in-plane saturation effects. Disadvantages include contrast cost, patient discomfort, and risk of allergic reactions. Lately, however, this technique is being replaced by newer less-invasive techniques. Poor positioning of the catheter tip, such as that located in the collateral vessel, can also result in false-negative interpretation of the sinus dimensions making it look stenosed.
Evaluation of measures to decrease intra-operative bacterial contamination in orthopaedic implant surgery medications hypertension 200mg quetiapine. Summary Dual-plane breast augmentation is a versatile technique that allows one to optimize long-term soft-tissue coverage in the widest variety of breast types while minimizing trade-offs to the patient and maximizing benefits symptoms to diagnosis generic 200 mg quetiapine overnight delivery. It should be noted that the majority of the high level outcomes in breast augmentation have been dual plane, and similar data with other pocket planes does not exist. If needed, further dissection between the pectoralis major and the parenchyma is accomplished to place more of the implant directly beneath the breast to have a better expansion of the parenchyma. Dual-plane breast augmentation is a partial subpectoral pocket plane for breast augmentation that was originally described in 2001. No division of the main body of the medial pectoralis major along the sternal border. The term dual-plane implies a subglandular implant inferiorly and a subpectoral implant medially and superiorly. Many surgeons who typically divide the inferior origins of the pectoralis major muscle are performing a dual-plane dissection, although they may have not recognized it as such. The reality of clinical practice is that these surgical dissection states certainly do not exist as single entities in actual procedures: they, in fact, may exist in multiple anatomic relationships along this spectrum, eg, dual plane 1. This is important because inadvertent or intentional division of the medial sternal border of the pectoralis major muscle results in uncorrectable deformities along the medial breast, including implant palpability, rippling, traction rippling, nodularity, symmastia, and soft-tissue stretch. Contraindications to the dual-plane technique include patients with extremely thin lower pole tissue, which can be identified with an inferior pole pinch of less than 5 mm (see Chapter 3: Tissue-Based Planning). In these patients, a traditional subpectoral plane is usually a better alternative, 70 7. The dual-plane 71 Dual-Plane Breast Augmentation technique is also contraindicated in body builders for whom a pocket plane above the pectoralis muscle is preferable. Once the pectoralis muscle edge moves superior to the upper areolar border, it becomes very difficult to obtain any muscle coverage at all over an implant. The placement of implant using the new inframammary incision is detailed in Chapter 8: the Inframammary Approach and the Dual-Plane Pocket. This is the preferred incision for the dual-plane technique; however, dual-plane breast augmentation may be performed via the periareolar technique or even the transaxillary technique with proper instrumentation. Nevertheless, the data generated on the dual-plane technique have been primarily via the inframammary approach. The tenets of the initial pocket dissection are detailed in Chapter 8: the Inframammary Approach and the Dual-Plane Pocket. Briefly, the pocket is dissected under direct vision with precise a 4 step traumatic technique using prospective hemostasis to eliminate bleeding within the pocket. The initial part of the dissection is the division of the inframammary pectoral origin, and this is taken to a point no further than the medial parasternal border. The main body of the pectoralis along the medial sternal border is left intact completely to maximize coverage over the implant. Despite the temptation to divide the muscle higher on the sternum to narrow the intermammary distance, this practice results in far more problems and is not recommended. Using the nondominant hand, the overlying breast parenchyma is palpated bimanually, and the degree of expansion of this parenchyma and vertical laxity is assessed. Of note, the limits of dual-plane augmentation are when the overlying skin and parenchymal laxity is greater than can be expanded with a reasonable size implant. Conventional classification of ptosis is not helpful in clinically making this decision. With the use of the nondominant hand, the overlying breast parenchyma is palpated bimanually, and the degree of expansion of this parenchyma and vertical laxity is assessed. In patients with a constricted lower pole, it is important with this maneuver to assess the expansion of the lower pole of the breast and to ensure that this is maximized. Once the surgeon has performed this maneuver, if it is deemed that an increased direct interface in the lower pole of the breast is desired then dissection is commenced between the breast parenchyma in the anterior aspect of the pectoralis major muscle. This is an incremental division of the attachments to avoid over-release, and the surgeon can continually, using 74 7. Once the dual-plane fine-tuning has been completed, the pocket is prepared with betadine triple or non-betadine triple antibiotic irrigation, and the implant is then placed into the pocket, oriented, and checked. This technique can be employed easily in virtually all breast augmentations, and the decision for the exact type of dual-plane dissection is the only intraoperative decision made during a standard primary breast augmentation. Using this technique, the scientific outcome data have been unsurpassed compared to any other pocket plane. Of note, there was also some radial scoring done of the breast parenchyma in the lower pole of the breast to further allow expansion of the lower pole. Dual plane breast augmentation: optimizing implant-soft-tissue relationships in a wide range of breast types. Summary this article details the state-of-the-art templated technique for inframammary breast augmentation. This technique is the third part of the Process of breast augmentation that is the single most transcendent concept for performing breast augmentation at the highest level. The steps are precise, systematic, performed atraumatically under direct vision with prospective hemostasis. Virtually every study that has published outcomes has used this approach and the best outcome data produced have used the inframammary incision. This article details the technical pearls for optimizing the surgical aspects of the inframammary incision. The width of the pocket is marked with a caliper with a medial and lateral dot that corresponds to the width of the selected implant. The height of the pocket is marked again using a caliper with a dot on the upper pole based on the height of the selected implant using the new inframammary position for the implant lower border. The key relationship for incision planning is the breast base width (see Chapter 3: Tissue-Based Planning) and nipple-to-fold measurement on maximal stretch. Tissue-based planning relationships, which have been previously developed, have further refined this algorithm by using the breast width, skin stretch, and the nipple-to-fold measurement to determine implant volume that optimally fills the breast. In this patient example, the breast width is 12 cm, and the nipple-to-fold measurement on stretch, as shown, is 7. The subsequent scar ended up on the lower pole of the breast placing more tension across the scar as it healed. The incision is at a minimum 4 cm long to allow precise pocket dissection under direct vision. The most medial aspect of the scar begins 1 cm medial to the papule, and the length is 4 cm or longer depending on implant size and type. Generally, the most medial extent of the incision is planned from the nipple with a vertical line dropped with the patient sitting 1 cm medial to the nipple, and the incision is planned in a curvilinear fashion from that point-the length dependent on the size of the implant. As the size of the implant increases the size of the incision and the same is true as the cohesivity of the implants becomes greater. This also helps the surgeon avoid the temptation for blunt pocket dissection, a dated technique that results in imprecise dissection, and higher rates of complications including capsular contracture and malposition not to mention negatively affecting the overall patient experience. Placing double hooks on the lower skin border or any other types of retraction on the lower aspect of the incision should be avoided.
Although rupture of an arteriovenous malformation may lead to a subarachnoid hemorrhage medications in canada purchase quetiapine line, aneurysmal rupture is a more common cause medicine vs surgery order quetiapine 200mg fast delivery. Certain tumors (particularly glioblastoma multiforme and metastatic lesions), brain abscesses, toxoplasmosis, granulomas, and active demyelinating lesions typically show ring enhancement after contrast administration. Although lymphomas can enhance in a homogeneous manner, they can also be ring enhancing. The symptoms of light-headedness and graying of vision are typically reported by patients with syncope. Other symptoms might include a heavy feeling at the base of the neck, buckling at the knees, and tinnitus. Although orthostatic hypotension is a common cause of syncope, the occurrence of syncope after micturition, rather than upon standing, suggests that this is not the cause in this case. Vasovagal syncope is another common cause of syncope but typically occurs in the setting of acute pain or with a strong emotional response. Vestibular neuronitis is characterized by vertigo, and there is no associated loss of consciousness. Treatment for viral meningitis is mainly supportive, because there are no specific treatments for most viral infections. In immune suppressed patients, it is appropriate to cover for bacterial infections as well until the preliminary cultures return. This is a neurosurgical emergency, so conservative management would only result in further neurologic decline. Because the patient has a hemorrhage, tissue plasminogen activator, which is used in acute ischemic strokes, would be contraindicated. Peripheral neuropathy, or polyneuropathy, is a more common manifestation of diabetes and often causes painful sensory symptoms distally in both legs. Patients with mononeuritis multiplex, a vasculitic neuropathy, often report the stepwise development of painful sensorimotor deficits in several individual nerve territories; nerves in watershed regions. Rupture of a cerebral aneurysm results in subarachnoid hemorrhage, not an epidural hematoma. Corticobasal ganglionic degeneration and Parkinson disease may also cause rigidity and poor postural reflexes, but are not typically associated with eye movement abnormalities. Weakness and atrophy reflect involvement of motor fibers rather than small-fiber sensory function. Anterior spinal artery syndrome usually results from infarction of the anterior spinal artery, causing ischemia to the anterior two-thirds of the spinal cord; therefore, dorsal columns are spared, but weakness and loss of pain and temperature sensation result because of involvement of the ventral horns and spinothalamic tracts. Central cord syndrome is most common in the cervical cord and typically results in loss of pain and temperature sensation in a capelike distribution. The classic features are ipsilateral weakness and loss of joint position sense with contralateral loss of pain and temperature sensation below the lesion. It is most appropriately treated with bright light therapy in the evening and melatonin to help reset her circadian rhythms. Behavioral modification is useful for many forms of insomnia, but bright light therapy is more effective for advanced sleep phase disorder. Stroke (involving either the brainstem or cerebellum) should be sudden in onset, not typically progressing over several days. Determination of the post-void residual would not help in this situation, and urodynamic studies are not indicated in the acute setting. Chronic paroxysmal headache is more common in women, whereas cluster headache is more common in men. Response to indomethacin is seen in chronic paroxysmal hemicrania, but not in cluster headache. Episodes of chronic paroxysmal hemicrania typically last for 20 minutes rather than hours. It signifies the presence of blood due to a subarachnoid hemorrhage (if blood has been present for a few hours). Increased opening pressure, increased white cell count, and pain upon needle insertion may or may not be present in either condition. Increased red cell count is seen both in a subarachnoid hemorrhage and in a traumatic tap. Examples of synucleinopathies include Parkinson disease, Lewy body dementia, and multiple system atrophy. Capillary telangiectasias, cavernous hemangiomas, and developmental venous anomalies are vascular malformations that rupture much less frequently. Possible localizations for this syndrome include the left corona radiata, left internal capsule, and the left side of the base of the pons. Infarction of the motor cortex capable of producing a right hemiplegia would also likely cause aphasia. Testing for gait abnormalities is thus a sensitive way to detect abnormalities in many different nervous system functions. A large pontine lesion will typically affect corticobulbar and corticospinal fibers bilaterally, but blinking and vertical eye movements are preserved because of intact midbrain function. It is characterized by a parkinsonian motor syndrome, visual hallucinations, and marked fluctuations in alertness, as well as an exquisite sensitivity to neuroleptic medications. The presence of Lewy bodies in the substantia nigra suggests Parkinson disease and in cortical neurons suggests dementia with Lewy bodies. Except on the rare occasion when a paroxysmal event is directly observed by the physician, the best way to distinguish a seizure from other episodes of neurologic dysfunction such as syncope, migraine, or transient ischemic attack is by detailed characteristics obtained from the history. The other listed choices may contribute to the diagnostic workup, but none is as important as the history in making the diagnosis. Fungal and tuberculous meningitides can share a common profile with bacterial meningitis except that the leukocytosis predominantly involves lymphocytes rather than neutrophils (except initially). Lesions in the left optic radiation produce a right homonymous hemianopia, and lesions of the right occipital lobe a left homonymous hemianopia. Lower trunk brachial plexopathy or C8 or T1 radiculopathies would involve the fourth and fifth digits and intrinsic muscles of the hand (including those innervated by the median nerve). Leg strength, pinprick appreciation, and cold sensation should be impaired, whereas joint position sense should be preserved (a dissociated sensory loss). A sensory level should be present over the torso, reflecting a spinal cord injury. Other tests need to be considered to confirm the diagnosis, but it is important to know the current respiratory status before any other test, particularly because neck weakness may be accompanied by diaphragm weakness. Typically, episodes of vertigo are brief, lasting 10 to 30 seconds, with no symptoms in between attacks. A cerebellar stroke would not produce recurrent positional symptoms and would likely be associated with other neurologic deficits. Migraine is very unlikely; it would be a mistake to assume that a new headache in a 77-year-old woman represents recurrence of an old problem. The preservation of repetition and comprehension points to a transcortical motor aphasia. Vitamin B12 deficiency may cause subacute combined degeneration of the spinal cord and dementia. Computed tomography of the head before lumbar puncture in adults with suspected meningitis. Neuronal atlas of the dorsal horn defines its architecture and links sensory input to transcriptional cell types.
Purchase quetiapine 200 mg with visa. UPDATE Subtle Signs of Autism in a 9 Year Old.
References
- Alifrangis C, Agarwal R, Short D, et al. EMA/CO for high-risk gestational trophoblastic neoplasia: good outcomes with induction low-dose etoposide- cisplatin and genetic analysis. J Clin Oncol 2013;31(2):280-286.
- Holm HA, Kalvenes S, Abidgaard U: Changes in plasma antithrombin (heparin cofactor activity) during intravenous heparin therapy: Observations in 198 patients with deep venous thrombosis, Scand J Haematol 35:564, 1985.
- Hollowell JG, Greenfield SP: Screening siblings for vesicoureteral reflux, J Urol 168(5):2138-2141, 2002.
- Vanhoefer U, Rougier P, Wilke H, et al. Final results of a randomized phase III trial of sequential high-dose methotrexate, fluorouracil, and doxorubicin versus etoposide, leucovorin, and fluorouracil versus infusional fluorouracil and cisplatin in advanced gastric cancer: a trial of the European Organization for Research and Treatment of Cancer Gastrointestinal Tract Cancer Cooperative Group. J Clin Oncol 2000;18(14):2648-2657.
- Mahle WT, Visconti KJ, Freier MC, et al: Relationship of surgical approach to neurodevelopmental outcomes in hypoplastic left heart syndrome. Pediatrics 2006; 17(1): e90-eConnor JA, Arons RR, Figueroa M, et al: Clinical outcomes and secondary diagnoses for infants born with hypoplastic left heart syndrome. Pediatrics 2004; 114:e160-eChrisant MR, Naftel DC, Drummond-Webb J, et al: Fate of infants with hypoplastic left heart syndrome listed for cardiac transplantation: A multicenter study. J Heart Lung Transplant 2005; 24:576-582.