Jonathan R. Hiatt MD, FACS
- Robert and Kelly Day Professor of General Surgery
- Chief, Division of General
- Surgery
- Vice Chairman for Education, Department of Surgery, David Geffen School
- of Medicine at University of California Los Angeles, Los Angeles, California
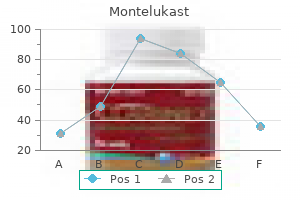
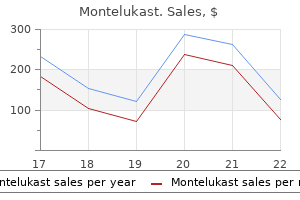
Therapeutic data from large randomized controlled trails relating to neurocardiogenic syncope are very limited [48] asthma treatment algorithm cheap 5 mg montelukast. A large randomized controlled trial Differential Diagnosis of Epilepsy 31 with fludrocortisone showed a trend toward benefit asthma treatment 4 syphilis purchase genuine montelukast online, perhaps more so in younger patients [55] asthma treatment oral discount 4mg montelukast visa. Elastic stockings asthma symptoms 32 order 5 mg montelukast amex, with or without fludrocortisone asthma symptoms getting worse best buy for montelukast, are used widely but, like disopyramide, have not been shown to be effective. Cardiac pacing had been shown effective in two randomized controlled trials [56] for the treatment of refractory neurocardiogenic syncope, but is now felt perhaps to represent the non-blinded nature of these studies and a reflection of expectation rather than real benefit [57]. Post-concussive events [58], in which tonic posturing, clonic movements or confusion stares are seen shortly after a concussive injury, are felt by some to represent a syncopal event, although there is some evidence to suggest such injuries have an epileptic basis. Either way, the prognosis is excellent and recognition of this distinctive syndrome important, particularly in the emergency department setting. Non-epileptic seizures Non-epileptic seizures has become a preferred term to describe the events referred to often as pseudoseizures, psychogenic seizures or hysterical seizures, as it lacks the pejorative implications of the older names. Definition of these episodes is difficult; convulsive activity is witnessed but has no electrical correlate and is felt to reflect psychological stresses of some sort, although these are rarely specifically identified [59]. These episodes may be extremely difficult to distinguish from epileptic events, even by experienced observers (Tables 2. Often, they receive health benefits of some sort, are unemployed and require high levels of care at home [59]. There is no consensus on the mechanism of these events from a psychiatric point of view, and often no specific psychiatric diagnosis can be made; the disorder itself seems to be the sole clinical manifestation of the problem [61]. Some consider the condition as a manifestation of a personality disorder [62], or a somatization disorder [63]. Munchausen syndrome by proxy, in which the description of seizures in the child is fabricated by the caretaker, is a form of child abuse and is a different condition [64]. Although the seizures are often precipitated by emotional stress or specific circumstances, this is not always the case. There is sometimes a family history of epilepsy, of epilepsy earlier in life or of personal encounters with epileptics, perhaps in a paramedical situation or as a carer. Events are usually very disruptive and dramatic, typically leading to multiple hospital admissions, and have a propensity to occur in public where they may be readily observed. First are attacks in which there is loss of contact, flaccid collapse and immobility. The second form are attacks of florid motor activity, often with sideto-side head shaking, pelvic thrusting and back arching. Variability from one event to another is common, making the lack of stereotypy a valuable clinical feature. The prolonged duration of many of the episodes is the most obvious clue to their non-organic nature. It is not uncommon for episodes to wax and wane from 30 minutes to hours in duration. Crying and screaming may be striking features of the episodes, and complex organized activity may be seen. Cyanosis is infrequent, but can be seen in some patients who may have what appears to be an adult version of breath-holding attacks. Tongue Dissociative seizures (convulsive type) In come cases emotion or stress Rare (if at all) Variable Can be prolonged and variable May be speech Asynchronous flailing of limbs, irregular, wax and wane, pelvic thrusting, opisthotonos May bite tongue (usually tip), carpet burns, injury rare. Directed violence not uncommon Variable responsiveness, often possible to communicate Often reactive Sometimes Few minutes, may be prolonged Synchronous and rhythmic, initially small amplitude fast evolve to slow large amplitude jerks Lateral tongue biting, accidental injury, posterior dislocation of shoulder, crush vertebral fracture Complete loss None Common Few minutes Source: Shorvon 2009 [118]. Interestingly, almost exclusively, this group of patients reports fecal incontinence. After the event recovery is usually rapid and often accompanied by emotional distress. However, not all events resolve rapidly, and prolonged unresponsiveness with normal vital signs may follow. The lack of tachycardia during this phase is a helpful feature diagnostically but may be complicated by the sometimes frenetic motor activity of the episode. This may cause elevated creatinine kinase levels on testing, helping to reinforce the organic basis of the episode to emergency department staff and intensivists, who frequently deal acutely with such patients. Injuries, often said to exclude a psychogenic cause, are recognized surprisingly frequently [65]. Furthermore, some patients have been treated urgently with parenteral benzodiazepines or even paralysis and intubation in a critical care setting. Some non-epileptic events are embellished organic syndromes, such as syncope or hyperventilation. The clinical scenario occurs in a hysterical or anxious person who experiences syncopal symptoms, hyperventilates and then evolves into a very complex and clearly non-organic behaviour that attracts attention while the prodrome becomes lost in the drama. Confirming the diagnosis is usually easy, particularly if a video can be taken by an onlooker. Patients who refuse monitoring, or those who have no events while being monitored, present a very difficult diagnostic problem, but most will have typical events in hospital. Seizures originating in the frontal lobe can be bizarre, frequent and associated with preserved awareness, and they are often refractory to medication. The stereotypic nature of the events, many of which occur from sleep, and some response to acute parenteral therapy provide clues. In these situations the finding of a relevant structural abnormality on imaging studies supports the diagnosis of seizures, but negative imaging studies do not exclude it. Engaging the patient in a therapeutic relationship is the most valuable component, followed by an explanation of the non-electrical basis of the events and recognizing that the condition causes disability. Confirming this belief with the patient takes much of the tension out of the situation. Confronting patients with a diagnosis of functional illness does little for their long-term care and often leads to re-presentation to other hospitals, with the consequent risk of inappropriate therapy. A face-saving compromise is often required, with an agreement by the patient to reduce or withdraw anticonvulsant therapy, avoid hospitalization and, where appropriate, to seek help from a psychiatrist to address underlying issues, such as depression. Accepting the care of one neurologist, or at least of one centre, is a major component of the clinical management plan [62]. However, controversy exists as to whether these patients should be managed by neurologists at all (in my view psychiatrists have little to offer these patients) and the temptation to treat with anticonvulsants is too great in the primary care setting. Engaging the patient in a positive therapeutic relationship minimizes risk, enables the anticonvulsant medications to be managed appropriately and can lead to a good long-term outcome. They are episodes of fear or discomfort often accompanied by somatic symptoms such as palpitations, dizziness, light-headedness and epigastric sensation, which may have a rising element [68,69]. Fearful patients want to escape and feel that the episodes indicate a life-threatening disorder. The attacks can be situational but most often occur spontaneously without a clear precipitant. As with seizures, attacks can be nocturnal and can cluster, occurring many times daily after long breaks between episodes. Overlap with the symptomatology of both complex partial seizures and syncope is marked, and seizures are not infrequently initially misdiagnosed as panic attacks, rather than the reverse [70]. The presence of other psychiatric features, such as comorbid depression, can assist in making a diagnosis of panic attack. Lifetime prevalence has been estimated at around 2%, with a higher risk for women. Although the condition is usually diagnosed in young adults, it has been described in children and the elderly. Highly variable in severity, these episodes are often disruptive and overlap considerably with other psychiatric syndromes, particularly agoraphobia and depression. At least 50% of patients with panic disorder develop a significant depressive illness during their life; the majority are depressed when they present for treatment [71]. Management consists of a reassurance directed at specific unfounded concerns regarding underlying illnesses and psychiatric therapy of the phobic and depressive elements [71]. Migraine Migraine is surprisingly often mistaken for epilepsy, particularly when the headache is mild or absent [72]. Migrainous aura may have visual, sensory or motor features that are suggestive of seizure activity and alertness is sometimes impaired. Postictal headache is common in epilepsy and often has a vascular quality, which may further complicate the diagnosis. Some unusual types of seizures, particularly those that originate in the occipital lobe, can be difficult to distinguish from migraines because features such as visual disturbance occur in both disorders [74,75]. Because there is no diagnostic test for migraine, the diagnosis is made on clinical grounds. Migraines are more common among those who develop syncope and there is often some overlap with the symptoms. Although visual disturbances are the Differential Diagnosis of Epilepsy 33 most common neurological feature of migraine, sensory or motor change, speech disturbance, amnesia or confusion and even loss of consciousness may occur. Migraine may have specific triggers, such as foods, medication, emotional stress or visual stimuli. Sensory or visual symptoms generally build up slowly and typically spread over minutes, progressing stepwise from one affected cortical region to the next, with resolution of the symptoms occurring as each new region becomes involved. The duration of the build up of visual symptoms is an important feature in differentiating these attacks from occipital lobe seizures which usually reach their height within a few seconds. The visual phenomenology of migraine also, unlike that of seizures, tends to resolve gradually. Response to anticonvulsant therapy is an unreliable basis for making the diagnosis. As epilepsy and migraine are both common, one might anticipate encountering them occasionally in the same patient. There seems to be no excess of epilepsy among patients with migraine overall [77]. They also noted that there seemed to be a particular link between catamenial epilepsy and migraine with aura. The increased cerebral blood flow that is induced by seizure activity is felt to be responsible for this headache. Often, these types of headaches occur in patients who suffer migraines at other times. However, the patient who presents with new-onset headache and seizure obviously requires the exclusion of an acute neurological problem, such as intracranial haemorrhage or infection. Seizures of occipital origin have many features of migraine, with visual hallucinations or amaurosis often complicated by headache. Benign partial epilepsy with occipital paroxysms is a syndrome of childhood to teenage years [81]. Hallucinations are typically simple in nature but can be complex and followed by complex partial or generalized convulsions [82], after which come the headache with nausea and vomiting. Occipital seizures resulting from structural pathologies, such as coeliac disease and mitochondrial encephalomyelopathies, may share these features [83]. Finding interictal spikes in patients with migraine suggests an alternative diagnosis, such as benign occipital epilepsy in children or the possibility of a structural lesion in adults. Sleep disorders A review of the many abnormalities that arise from sleep is outside the scope of this brief chapter. On the other hand, some epilepsies arise exclusively from sleep and there is a propensity for partial seizures to occur in sleep or shortly after waking [86]. Benign rolandic epilepsy is an example of a seizure syndrome that is associated with sleep. Although the classic tetrad of narcolepsy involves excessive daytime sleepiness, cataplexy, hypnogogic or hypnopompic hallucinations and sleep paralysis, not every component occurs in a given individual. Cataplexy, sudden episodes of sleep and hallucinations are sometimes misidentified as seizures [90]. Paroxysmal nocturnal dystonia is an often dramatic movement disorder arising in sleep. Many patients originally diagnosed with this condition have since been recognized to have frontal lobe epilepsies [85]. The history of daytime seizures is also helpful in confirming a diagnosis of epilepsy. Children wake from sleep screaming and crying inconsolably for many minutes, after which they go back to sleep and are amnesic of the episode. Events usually occur from slow wave sleep, typically 30 minutes to 4 hours after going to sleep. Sleepwalking is a related problem, and the features are well known to the general population [93]. The automatic activity of wandering is sometimes less florid, featuring motor activity that may imitate the automatisms of complex partial seizures, with repetitive hand movements. Hypnogogic myoclonus, although a normal event most have had experience of, sometimes brings patients to the epilepsy clinic, often through the observations of an anxious partner and sometimes in the setting of recognized epilepsy. Pathological fragmentary myoclonus, in which fragments of myoclonus of early stage sleep persist into stages 3 and 4, may be seen with any cause of disrupted sleep. Periodic movements of sleep are so distinctive that it is rare for them to be confused with seizures [94,95]. They are characterized by repetitive flexion and extension, sometimes quite vigorously, of hip, knee, ankle and toe for a period of 30 s or so. The episodes frequently recur throughout the night, and can persist into wakefulness, troubling the bed partner but not the patient. Sometimes dramatic and prolonged, the 34 Chapter 2 activity can be complex, violent or aggressive and accompanied by agitation and vocalizations. Although most parasomnias can be distinguished from epileptic disorders by their distinctive clinical features, polysomnography allows definitive diagnosis in most instances [96]. Hyperekplexia is a rare disorder of infancy, where an exaggerated startle response occurs in response to unexpected stimuli, particularly auditory events.
This is an important consideration asthma symptoms runny nose order 5mg montelukast free shipping, as asthma 7 news discount montelukast 4mg, for instance asthma treatment in qatar generic 5mg montelukast with visa, the legal requirements for driving are not necessarily the same as the clinical requirements in terms of treatment asthma symptoms vs heart attack generic montelukast 5 mg amex. In the nineteenth century asthma definition 666 buy 4mg montelukast with amex, all seizures were considered to have both predisposing and also exciting components, and the production of seizures was considered invariably the result of both influences acting together (Jackson repeated the commonly used analogy of gunpowder and the spark). In a recent survey, it was found that 97% of patients with epilepsy believe that there is at least one precipitant for some of their seizures, and 28% believe that there is a precipitant for all of their seizures [44]. The line between the two is not easy to define, and to do so is to apply largely arbitrary criteria. Gastaut [45] defined reflex epilepsies as those in which all seizures, or a large part of them, are reliably provoked by naturally occurring or artificial stimulation of a certain receptor or group of receptors, and a similar formulation was given by the 2001 glossary. Photosensitive epilepsy is by far the most common type and has been extensively studied. The frequency and type of visual stimulation can be highly specific in individuals, and there is also a genetic predisposition in some cases. Examples include musicogenic epilepsy, in which sometimes a highly specific piece of music triggers the seizures, or seizures induced by thinking, reading, eating or sometimes highly specific cognitive tasks. Internal triggers, such as the effects of menstruation of fatigue, are not usually included in the category, nor are more indirect external triggers such as alcohol intake. The first major conference devoted solely to the topic of status epilepticus was the Xth Marseille Colloquium, held in 1962 led by Henri Gastaut [48]. Although no duration was specified in the definition, Gastaut later specified a duration of 60 minutes to define status epilepticus. Status was thus subdivided then into three types: generalized status epilepticus, partial status epilepticus and unilateral status epilepticus. Definition and classification were the subject of detailed consideration in the monograph on status epilepticus published in 1994, Table 1. The emphasis on timing of treatment led Lowenstein to propose that any convulsive seizure continuing for more than 5 minutes in duration should be considered a case of status epilepticus. Definition (Terminology) and Classification in Epilepsy 21 was formulated so that there was no delay in initiating emergency therapy in patients with prolonged seizures [50]. Finally, Axis 4 divides age groups into neonatal, infancy, childhood, adolescent and adulthood, and elderly (Table 1. Without impairment of consciousness (aura continua, with autonomic, sensory, visual, olfactory, gustatory, emotional/psychic/experiential, or auditory symptoms) ii. Location: generalized (including bilateral synchronous patterns), lateralized, bilateral independent, multifocal 4. Time-related features: prevalence, frequency, duration, daily pattern duration and index, onset (sudden or gradual) and dynamics (evolving, fluctuating or static) 5. Elderly (>60 years) 22 Chapter 1 work in progress and it will be interesting to see to what extent this new scheme is helpful in practice. Afterthought In this chapter, I have tried to sketch out the evolution over time of definition and classification of epilepsy since the work of Jackson (whose oeuvre marks the dawn of modern epilepsy), to provide a summary of current classifications and provide a brief critique. A number of general observations concerning classification and terminology in epilepsy become apparent when an historical approach is taken, and I end this chapter with a brief consideration of these. What is abundantly clear from the historical perspective is that the state of knowledge in the field of epilepsy is such that our current and past classifications schemes have been by necessity utilitarian and not scientific. Although much effort has been expended, and with boring regularity unsubstantiated claims to the contrary have been made, we are as far as ever from being able to devise a suitably scientific schema. First, there is a danger that, through a desire to be too all-inclusive, the schemes become too complex and unwieldy, thereby losing their utilitarian value. Given that they are gardening in character and thus derive their worth entirely from their utility in common practice, complexity is an enemy. The failure of uptake of the 1989 Classification of the Epilepsies and Epileptic Syndromes into widespread usage, for instance, was not due to its poor quality (indeed, on the contrary, it is of excellent quality) but due to its complexity. As knowledge advances, the field becomes more complex, but the difficult trick for classificationists is to maintain a balance between the Scylla of superficiality and the Charybdis of intricacy. This was what Engel postulated in 2001 and what the current Commission is also pursuing. Even with such databases, there is a need for a single simple scheme, and the main categories of the 1989 classification are difficult to beat in this regard. Another essential feature, often overlooked, is the extraordinary care needed when devising terminology. It has also, simply through its linguistic implications, directed scientific research. Modern sloppiness in the use of terminology, which is currently a widespread problem, has the absolutely opposite effect. Furthermore, the current fashion for continual change, often spuriously justified as being needed by advances in science, should be deprecated. All that is achieved by continuous tinkering of definition and classification is chaos and confusion, and this erodes the authority of any scheme. To do so is damaging as well as unnecessary, and there are disadvantages not only for epileptologists, but also for those engaged in more general medical practice and in legal, regulatory and societal arenas. This is perhaps because at one level it is the work of gardeners not botanists, and thus has been usually a matter of opinion (assertion) and not of fact. Everyone can have an opinion, and it seems that everyone does, often from a limited viewpoint (the current author is guilty of this), and it is sad to see the intrusion of politics and personal opinions and vanities into a field that should be dry and academic. One lesson is that the schemes, being largely of an opinionated nature, must win the approval of the community at large and cannot be forced through on to unwilling recipients. One way of garnering wide support is for committees or panels to devise the systems and for the drafts to be sent out for wide consultation. However, this only works if the results of the consultation are heeded, as Gastaut found to his cost in 1969/1970. The best classification schemes have also depended on an acceptance of the authority of their authors, and the widespread respect that Jackson, Gastaut and Dreifuss commanded was instrumental in the success of their schema. Reprinted from Transactions of the St Andrews Medical Graduates Association, 1869. Terminology and organization of seizures and epilepsies: radical changes not justified by new evidence. Classification concepts and terminology: is clinical description assertive and laboratory testing objective Modern technology calls for a modern approach to classification of epileptic seizures and the epilepsies. The concept of symptomatic epilepsy and the complexities of assigning cause in epilepsy. Seizure semiology: its value and limitations in localizing the epileptogenic zone. Synopsis and conclusions of the International colloquium on reflex seizures and epilepsies, Geneva 1988. Status Epilepticus: Mechanisms of Brain Damage and Treatment Advances in Neurology, Vol 34. Although the diagnosis of an epileptic disorder can be straightforward, it is often not so, and this is especially the case if the event is unwitnessed, or if the history is incomplete. There are a wide variety of neurological and non-neurological conditions that are mistaken for epilepsy, and the most frequent and challenging distinction is between epileptic events and syncope or presyncope. A number of studies have shown that syncope is commonly misdiagnosed as epilepsy, largely through ignorance of the complex prodrome that may occur, and the sometimes dramatic nature of a clinical event that shares many features with epileptic convulsions [1]. Less common disorders that are confused with epilepsy include cerebral ischaemia or paroxysmal symptoms of demyelinating disease, raised intracranial pressure, Tourette syndrome and other movement disorders. Patients presenting with behavioural symptoms most often have a primary psychiatric diagnosis but are often thought to be suffering a seizure disorder. The surprising abundance of misdiagnosed epilepsy has been confirmed in a number of studies, and is cause for much concern [2,3]. The incorrect diagnosis is often catastrophic for the patient, resulting in significant restriction to social activity and employability, as well as administration of unnecessary medication. Loss of driving privileges is often the most immediate and traumatic component for patients whose livelihood depends on a valid driving licence. From all perspectives, the diagnosis of epilepsy requires clinical skill and judgement, and it is incumbent on the clinician to attach a definite diagnosis only if certain. General approach to the diagnosis of episodic disturbances As an enormous variety of conditions can cause episodes of transiently disturbed consciousness or function, the major component of clinical management consists of separating out the various causes, usually on clinical grounds. Determining the nature of events can be challenging, particularly when the event has been unwitnessed or when the patient is an inadequate historian. Obtaining a clear account of the nature of the attack is the most important single component of the assessment. Ascertain precisely the circumstances of the event, any warning that occurred, the duration of the attack, exactly what occurred during the event, the nature and speed of recovery and as well as whether there were any focal or lateralizing signs after the event. There is no substitute for a detailed history of the attack from both the patient and any eyewitnesses, and obtaining a detailed account of the circumstances of the event as well. Whereas the patient may recall a simple fall or brief loss of consciousness, an eyewitness may provide a detailed account of generalized convulsion with postictal confusion, tongue biting and so on, for which the patient is often amnesic. Clinical examination can provide useful information, particularly if undertaken in the hours after the event, but is most often non-contributory. Events that occur in particular circumstances should always raise the suspicion of syncope. There are obvious causes, such as sudden pain, venesection, emotion, standing for long periods or watching unpleasant movies. However, mechanical causes, such as cough, urination or defecation, may also provoke syncope; the differences between syncope and epilepsy are detailed later in the chapter. Episodes of loss of consciousness occurring with postural change are more likely to be syncopal. Other physical precipitants, such as change in head position, rolling in bed, looking up at a high the Treatment of Epilepsy. Events that occur from sleep, even if only some of the time, are almost always epileptiform. Seizures are sometimes linked to particular phases of the menstrual cycle, and while once thought to indicate a functional element, this is very common in women with epilepsy. Episodes that occur when under emotional stress, if in difficult circumstances, particularly in the cognitively impaired, might be behavioural in origin rather than due to seizure activity; however, the distinction is sometimes difficult, and this can be further complicated when it is suggested that the behavioural alterations are a feature of a postictal state. The symptoms in the immediate moments prior to the event are diagnostically critical. True vertigo is rarely a feature of epileptic attacks but it is not always easy to distinguish vertigo from brief seizures. If a typical account of shimmering scotomatous deficit evolving over some minutes with or without a headache following, and possibly associated with other neurological symptoms, is described then migraine becomes a strong possibility. The duration of attacks is probably the best single guide when considering the nature of the episodes. With epileptic events, there is often some warning and build-up to maximal deficit (although usually over a matter of a few seconds in contrast to migraine which builds up over minutes), whereas, with ischaemic vascular episodes, the onset is abrupt and typically maximal deficit at the outset with gradual resolution. Since consciousness is usually unimpaired in focal cerebrovascular events involving the hemispheres, altered consciousness during attacks of this type is more suggestive of an epileptic aetiology. Although status epilepticus, both convulsive and non-convulsive, can certainly be prolonged it is a relatively uncommon event among people with chronic seizures. After an event, rapid recovery, perhaps with sweatiness or nausea and vomiting, is more typical of syncope than of epilepsy. Occasionally there is marked alteration in mood and behaviour postictally; less often a true psychosis occurs postictally which, although typically self-limiting, sometimes dominates the presentation. Motor activity, or the lack of it, during the event often helps clarify the nature of the attack. If absences are typical with abrupt cessation of activity and prompt resumption of activity at the end of the few-second-long episode then the diagnosis is usually clear. There may be minor tone changes or flickering of the eyelids but marked motor activity is not a feature. Classic complex partial seizures are easy to diagnose if they comprise a warning followed by loss of contact, oral and manual automatisms and postictal confusion, sometimes with lateralizing signs noted during or after the event. Generalized convulsive activity can be more difficult to distinguish from syncope. The total absence of confusion after a generalized convulsive event should immediately raise the suspicion that the event was not epileptic. During a seizure, well-organized motor activity is uncommon, although automatisms can sometimes be perseverative and simple activities are continued, although in an incomplete and sometimes clumsy manner.
This statement can be viewed as the culmination of a series of previous studies of animal electricity started by Luigi Galvani [2] and von Humboldt [3] acute asthmatic bronchitis icd 9 code effective 5 mg montelukast, and subsequently pursued using cortical stimulation experiments by Fritsch and Hitzig [4] and the clinical observations of Todd [5] asthma symptoms mild moderate severe discount montelukast online master card. Since then severe asthma definition gina 4 mg montelukast sale, increasingly refined investigatory techniques have provided a great deal of information about how epileptic discharges are generated and propagated within the central nervous system asthma film purchase montelukast 5 mg fast delivery, and the many different ways in which they manifest themselves that we have learned to recognize from clinical observation asthma symptoms only when sick order genuine montelukast. Subsequently, owing to the emphasis given to the progressive course of some of these mechanisms, the term epileptogenesis has often been employed to define the process whereby an initial event leads to the constitution of a persistent epileptic condition. As in the case of many other pathological conditions, experimental models have made a major contribution to our understanding of epileptogenesis. This is not just a question of semantics, because the relevance of experimental results to the advances made in our understanding of epilepsy depends on how suitably the experiment has been designed for this purpose. Operationally, it is enough to say that an experimental preparation should be referred to as a model (of epilepsy, seizures or epileptogenic mechanisms) only if it faithfully reproduces the clinical and electroencephalographic characteristics of human epilepsies or seizures, or the biological changes that are known to be associated with them. Over the last few years, animal experiments have been effectively supplemented by human tissue studies of brain specimens surgically removed for the treatment of drug-refractory epilepsies. Experimental studies have shown that a number of different agents that affect excitatory or inhibitory neurotransmission, intrinsic cell excitation mechanisms or the ionic microenvironment can induce seizures. Lower trace: field recording of the discharge synchronously involving a large neuronal population. This chapter deals with the epileptogenic mechanisms that putatively account for naturally occurring animal and human epilepsies and that are known or promising targets for strategies aimed at treating epilepsies and preventing epileptogenesis. Membrane ion channels the excitability of nerve cells depends on the movement of ions through specific voltage-dependent or receptor-activated membrane channels. The kinetics of transmembrane ion currents has been extensively investigated by means of various types of voltage-clamp recordings, whereas the effects of ion currents on cell membrane potential can be detected by means of current clamp recordings. The N-terminal region is particularly important in beginning the process of subunit association that leads to channel assembly, a process that is facilitated by the presence of accessory subunits and significantly influenced by a large number of different environmental influences. It leads to the formation of channels with different degrees of permeability to the various ions and different opening and inactivating kinetics, depending on the type of subunits assembled, their stoichiometric characteristics and the relative position of each subunit within the hetero-oligomeric complex. The identification of the molecular structure of the various subunits and their corresponding coding genes has revealed a surprising multiplicity of distinct subunits, of which the pattern of assembly can lead to a considerable number of channel subtypes with different properties [9,10]. The expression pattern of putative epileptogenic dysfunctions therefore needs to be carefully investigated, not only at the level of brain topography, but also at cellular and subcellular levels. Voltage-gated channels these form a category of ion channels that undergo voltage-dependent conformational changes leading to transitions from the closed to open state or vice versa. Each domain contains six transmembrane segments, the fourth one being the voltage sensor, and the loop between the fifth and sixth forming the ion-selective pore. Owing to the effect of ion pumps in resting conditions, membrane potential is kept around -70 mV. The lines below the tracings depict the time course of ion currents with different kinetics. Grey lines indicate currents that tend to depolarize the membrane and black lines indicate currents that polarize it. In the uppermost part is a schematic representation of the protein structure of, 1 and 2 subunits. Note the tetrameric structure of -subunit with four transmembrane domains each composed by six transmembrane segments, the fourth is the voltage sensor whereas the loop between the fifth and six segments forms the ion selective pore. Many of these effects were consistent with a gain of function of Na+ channels, and thus with a pathologically increased membrane excitability [16,21]. This interesting topic shows the complex scenario of channel pathology and highlights the need for further investigation aimed at understanding the effect of sodium channel mutations at circuitry level rather than in individual neurons. Moreover, it has been found that molecular interactions with modulatory proteins or drugs can partially rescue the function of Na+ channels with mutations that normally lead to a complete loss of function [26]. This evidence further shows that more research is needed to clarify the functional effects of channel mutations in vivo and the variability of the phenotypes resulting from Na+ channel mutations. Mechanisms of Epileptogenesis 41 Unlike Na2+ and Ca2+ channels, which are large monomeric proteins that include four homologous repeats, K+ channels are made by the assembly of four proteins each of which contain six transmembrane domains and is therefore similar to one Na+ or Ca2+ repeat, thus the resulting structure is similar to that of Na+ and Ca2+ channels, but the number of possible subtypes is much higher because of the large number of possible combinations. Although it is assumed that there are subtle functional differences between the different subtypes, the currents flowing through the K+ channels are grouped in a relatively limited number of physiological categories. Disrupted K+ channel function is involved in the epileptogenesis in some spontaneously occurring human epilepsies. However, this is difficult to prove experimentally for three reasons: (i) given its paramount importance for protein synthesis and metabolism, a considerable amount of Ca2+ is stored in the cytoplasmic reticulum and any artificial change in its concentration in an experimental preparation can mobilize it from the storage compartment to the ionized free fraction, thus leading to complex effects on cell excitability that are further complicated by metabolic effects, which are often difficult to resolve; (ii) the role of Ca2+ in promoting vesicle fusion at nerve terminals adds a presynaptic effect that has to be taken into account when evaluating membrane excitability as a function of Ca2+ concentration; and (iii) a number of the Ca2+-dependent K+ currents contributing to cell excitability may be impaired when Ca2+ concentration is artificially lowered, thus leading to indirect and somehow unpredictable consequences that may obscure the direct effect of Ca2+ movement across the membrane. The characterized Due to the fact that neuronal membrane needs a perfect balance of ionic currents to regulate intrinsic the physiological excitability, malfunctioning of other voltage sensitive channels can be critical to 42 Chapter 3 generate pathological oscillations and paroxysmal events. Ligand-gated channels Ligand-gated channels, or receptors, are molecular complexes that include a pore region or ionophore, which becomes permeable to some ions when the relevant ligand binds to a specific binding site. Ligand-gated channels are classified according to a scheme based on the ligand (neurotransmitter or neuromodulator), with a number of functionally distinct subtypes being differentiated in each category based on pharmacological (affinity for artificial ligands) or physiological criteria (selective ion permeability). Pharmacological agents acting on receptors can affect not only the primary epileptogenic process, but also its effects in regions beyond the epileptogenic area. The amino acids glutamate and aspartate are the two main excitatory neurotransmitters in the cerebral cortex and act through various receptor subtypes, the subunit composition of which determines the selective ionic permeability and kinetics of the respective ionic currents [47]. Five subunits from seven subunit subfamilies (, and) assemble to form a heteropentameric Cl-permeable channel. Furthermore, the hyperexcitable dentate gyrus removed from patients with temporal lobe epilepsy retains bicuculline-sensitive synaptic inhibition [53]. Membrane ion channels as targets for antibodies in acquired autoimmune disorders Antibodies to neuronal surface proteins have been found in patients with seizures presenting as symptom of paraneoplastic or autoimmune encephalopathies [66,67]. The precise mechanisms of seizures resulting from the synthesis of antibodies against channel or receptors remain incompletely understood [68]. In fact, the possibility of a direct action of the antibody on the channel and/or receptor has been hypothesized for Rasmussen encephalitis [69] but not ultimately demonstrated. Channel and receptor trafficking and plasticity the efficient delivery of cellular constituents to their proper location is of fundamental importance for all cells and has a pivotal role in normal neuronal functions. Protein trafficking is essential in developmental processes and plasticity and includes neurotransmitters release by exocitosis, recycling of synaptic vesicle proteins and regulation of receptor signalling. Neuronal function can be significantly modified by alterations in the levels of receptors, ion channels and transporters at both pre- and postsynaptic level and defective protein trafficking can be a significant mechanism in sustaining excitability changes and epileptogenesis. A main topic relating to trafficking defect in epilepsies arise from observation made on genetically determined channelopathies, which can be assumed as a general model of excitability changes resulting from disturbed protein function and interaction which can also occur as a consequence of epileptogenic events supporting epileptogenic progression. Its pore region has a pentameric structure consisting of various hetero- or homologous combinations of eight -subunits and three -subunits. As the 4-subunit is widely distributed in the mammalian brain, it is puzzling how the mutation can cause a focal hyperexcitability syndrome. Some mutations in Na+ channel function directly lead to hyperexcitability thus accounting for the occurrence of seizures; however, other mutations lead to loss-offunction that often results from folding and/or trafficking defects capable of reducing channel expression. Some of these mutations appear to act through decreasing binding of calmoduline which impairs the exit of Kv7. The possibility that the genetic background or modifying genes have a role in influencing trafficking dependent defects may account for different phenotypic expression of the same gene mutation, which effect can be attenuated or increased by modulatory proteins. This can open novel therapeutic possibilities acting by rescuing trafficking-defective mechanisms using appropriate drugs or interacting proteins. These therapeutic strategies may be targeted to amend specific genetic defects but can also model future treatments for acquired epilepsies. In fact, beside inherited channelopathies, evidence obtained in models of acquired epilepsies also point toward excitability dysfunction resulting from defective trafficking of ionic channels. For instance, decreased availability of A-type potassium ion channels found in models of temporal lobe epilepsy has been attributed to result from transcriptional (loss of channels) and post-translational (increased channel phosphorylation by extracellular signal-regulated kinase) mechanisms [76]. The knowledge of protein trafficking defects and adaptive mechanisms taking place during epileptogenic processes might open new strategies in the therapeutic interventions. K+ channels the synchronization of large populations of synaptically connected neurons. The physiology of this multisynaptic system and its relevance to epilepsy have been a focus of intense research. In this section the role of local circuits regional networks and system are considered. Such networks can be discretely localized or more widely distributed within one hemisphere [83]. The concept of an epileptogenic network as seizure generator typically applies to limbic epilepsies. Their physiological and pathophysiological properties relevant to epileptogenesis are further commented upon here. Some information concerning the significance of integrative hippocampal activities has come from studies of the correlations between cell activities and behaviour. Above all, these have demonstrated a fundamental relationship between the discharging properties of hippocampal cells and arousal, the most important finding being the modifications created during the acquisition of conditioned responses. Thanks to these properties, the limbic (and particularly hippocampal) circuits are capable of recording and storing traces of information originating from the various sensory systems by constructing a cognitive map that is continuously updated on the basis of experience [86]. The relevance of hippocampal plasticity in the pathophysiology of temporal lobe epilepsies was first demonstrated by Graham Goddard [87]. The role of such an epileptogenic plasticity in determining the progressive course of some types of epilepsies is discussed further in the next section. The arrows in parts (a) and (b) indicate efferent and afferent connections, respectively. Sensory information reaches the amygdala through the lateral nucleus and is then distributed in parallel to the various other nuclei by means of a system of highly organized intra-amygdaloid circuits. Amygdala discharges are often associated with oral feeding automatisms (chewing movements) that are sometimes accompanied by salivation [89], less frequently with unmotivated fear and even more rarely with the emotional expressions of anger and aggressiveness described in classic animal studies [90]. Cingulate gyrus the cingulate region appears to be involved in conditioned responses presumably connected with the acquisition of avoidance reactions. The symptomatology of epileptic seizures originating from the anterior cingular region includes terror, screams, aggressive verbal expressions, complex gestural automatisms, vegetative disturbances and visual hallucinations associated with only partial alterations in consciousness [91]. The anatomical basis underlying the motor expression of the responses are the connections between this region and the caudate nucleus, the ventral pontine nuclei, the ventral part of the periaqueductal grey matter and the deep strata of the superior colliculus. The posterior or retrosplenial cingulate region seems to be particularly involved in the processes of spatial discrimination associated with visual information. Among the limbic structures many networks can be identified that account for the clinical manifestations of limbic seizures and for the spread of the generating discharges inside and outside the limbic area possibly resulting in secondary generalization. What makes the system prone to seizure generation is matter for hypothesis-driven investigations, putative mechanisms include genetic and developmental factors and their interaction, but also environmental factors that electively affect the excitable properties of the relevant system. In this sense the SystE hypothesis provides a conceptual alternative to the current views based on the double dichotomy: focal versus generalized/idiopathic versus symptomatic epilepsies. One condition that exemplifies well the concept of SystE is absence epilepsy and its relationship with thalamo-cortical system. Recent evidence indicates that a non-inactivating Na+ current component may act synergistically with the T-type Ca2+ current [101]. Both the thalamic the organization of the fibre connections within the brain is so rich that the number of circuits that one can identify is virtually unlimited. Yet the claims of a given circuit as the basis for a given type of seizures should be accepted only when sound proof of its responsibility is provided. Among the corticocortical fibre bundles, specific mention should be made of the frontal callosal projections that have a role of in the interhemispheric synchronization of epileptic discharges. They obtained different types of pseudogeneralized discharges depending on the location of the bilateral frontal loci, a finding that correlates well with the marked tendency towards the bilateral expression of seizures with a frontal origin in humans. Systems Recently, the hypothesis that some types of epilepsies are caused by the specific susceptibility of functionally specialized brain systems as a whole has been proposed [93]. The involved neural system is defined as a set of synaptically interconnected areas, the coordinated activities of which lead to functional results that cannot be obtained by the activity of the elements alone. The definition reproduces in neurobiological terms the one used in engineering, mathematics, and information technology. Moreover, mice lacking (1G) T-type Ca2+ channels show a lack of the burst firing of thalamocortical relay neurons and resistance to absence seizures [42]. For the system epilepsy hypothesis, however, this debate is relatively unimportant. Indeed, what really matters is that the electroclinical expression of absence seizures requires the involvement of the full thalamo-cortical loop whose functional specialization is the control of vigilance [93]. Similar considerations can be made for juvenile myoclonic epilepsies, benign childhood epilepsy with centrotemporal spikes and West syndrome, which are discussed in Avanzini et al. The biological mechanisms responsible for this progressive course of the epileptogenic process have been extensively investigated as potential targets of strategies to prevent the development of epilepsy. An important question is whether the seizures themselves can activate mechanisms capable of facilitating epileptogenesis. Plastic changes in channels and receptors Changes in Na+ channel subunit expression have been reported in the hippocampal tissue from experimental animals [105,106] and from patients with temporal lobe epilepsy [107]. These molecular changes result in the enhancement of Na+ current, which can contribute to epileptogenesis [106]. Moreover, complex changes in neurotransmitter and neuromodulator systems have been reported (for review see [112]), which can participate in epileptogenic mechanisms.
Buy generic montelukast 10mg on line. Asthma|अस्थमा |English #healthmaantra.
Syndromes
- You have MAT and your symptoms get worse, do not improve with treatment, or you develop new symptoms
- Vision loss (rare)
- Rheumatoid factor test
- Abdominal ultrasound
- Any disorder that causes damage to the nervous system or causes muscle weakness
- Arterial blood gases
- Family history of hardening of the arteries
- Are there facial tics?
- The scrape contains dirt and other debris deep inside.
- Urinalysis
If the anemia is microcytic asthma symptoms phlegm discount montelukast 10mg on line, one would consider iron deficiency or chronic blood loss asthma 6 steps buy 10mg montelukast amex. If it is macrocytic asthma definition volume purchase 5mg montelukast with amex, consideration should be given to pernicious anemia or folate deficiency asthma triggers definition generic montelukast 5mg fast delivery. A hematologist will perform a bone marrow examination for a more definitive diagnosis asthma movie cheap montelukast generic. The patient usually will also complain of weakness and may be found to have weakness when the muscles are tested. Finally, with bilateral ankle clonus there will often be hyperactive reflexes throughout the lower extremities and sometimes in the upper extremities. If it is unilateral, then it is a sign of either hemiparesis or monoplegia; and if it is hemiplegia or hemiparesis, one should consider the possibility of a cerebral disorder. If there is headache and papilledema, that disorder is most likely a space-occupying lesion of the brain such as a brain tumor, abscess, or hematoma. If there is hemiparesis and it is acute in onset, there is most likely an occlusion of one of the cerebral arteries, whereas if the hemiparesis is gradual in onset, one should consider multiple sclerosis and, once again, a brain tumor. Ankle clonus associated with monoplegia is more likely related to a spinal cord tumor, but a parasagittal tumor could also be present. Bilateral ankle clonus is more likely caused by a disorder of the spinal cord such as a spinal cord tumor, amyotrophic lateral sclerosis, or multiple sclerosis. However, if there are cranial nerve signs, one must consider a brain stem tumor as well as other degenerative diseases of the brain and brain stem. If there are no findings on the examination to indicate a level, then, of course, the entire spine would have to be covered. The spinal tap with analysis of the 74 fluid for myelin basic protein and gamma globulin levels should be done if multiple sclerosis is suspected. Finally, the most cost-effective approach to a patient with ankle clonus is to refer the patient to a neurologic specialist. There is no cough or night sweats to suggest tuberculosis, carcinoma, or other pulmonary conditions. Acute anorexia would most likely be caused by an acute febrile disease or acute psychiatric disturbance. The most likely abdominal mass to produce anorexia as the only symptom would be an early pancreatic neoplasm. Other neoplasms may be felt and/or metastasize to the liver and cause hepatomegaly. If there is a chronic cough, one should consider tuberculosis or carcinoma of the lung. Hepatomegaly without any other masses present in the abdomen would certainly bring to mind cirrhosis. Also, the hepatomegaly may be related to a collagen disease or metastatic carcinoma. A complete endocrinologic workup by an endocrinologist may be indicated if all the above studies are negative. Patients with a normal physical examination and normal diagnostic studies should be referred to a psychiatrist. If the anosmia or unusual odor is intermittent, then one should consider psychomotor epilepsy. A skull fracture, particularly if it involves the cribriform plate, may interrupt the olfactory nerves and cause anosmia. If there is unilateral anosmia, one should consider an olfactory groove meningioma. Multifocal neurologic signs should suggest multiple sclerosis, and additional neurologic signs such as memory loss should suggest an olfactory groove meningioma or parietal lobe tumor. Many systemic diseases may cause anosmia, including hypothyroidism, diabetes, renal failure, hepatic failure, and pernicious anemia. This symptom is often delusional, so a psychiatrist may need to be consulted at the outset. Sulfonamides are notorious for causing renal failure, but one must also consider amphotericin B, gold compounds that might be administered in arthritis, and lead and other drugs or heavy metals. If there is hypertension and anuria, one should consider acute or chronic glomerulonephritis, polycystic kidneys, and acute tubular necrosis. If there is a low blood pressure, one should consider prerenal causes of anuria such as dehydration, blood loss, the acute abdomen, and other causes of shock. If there is chest pain, one should consider myocardial infarction or pulmonary infarction. If there is chest or abdominal pain with hypertension, then one should consider dissecting aneurysm. Enlargement of both kidneys should suggest bilateral hydronephrosis or polycystic kidneys. Enlarged bladder would make one think of bladder neck obstructions due to prostatic hypertrophy or carcinoma or a urethral stricture. Occasionally, what is thought to be an enlarged bladder is actually a pelvic mass that is obstructing the ureters. Hematuria would suggest glomerulonephritis, acute tubular necrosis, intravascular hemolysis, and nephrolithiasis. A Foley catheter should be passed and attached to drainage to determine the urine output. If there is obstructive uropathy due to bladder neck obstruction, this will obviously determine the diagnosis, as there will be a large volume of urine and it should be taken off gradually. Then studies of obstructive uropathy can be done, including cystoscopy and 80 retrograde pyelography. If the obstructive uropathy is caused by obstruction of the ureter, renal ultrasonography can be reliable in detecting the dilated calyces or dilated ureter. If the patient presents with anuria and hypotension, the most important thing is to reestablish the blood pressure with a bolus of normal saline or dopamine drip. If the anuria does not cease at this point, high-dose furosemide or a mannitol infusion can be started. The clinician should examine the urinary sediment himself, and this will identify cases of acute glomerulonephritis, lupus erythematosus, and acute tubular necrosis with considerable accuracy. If intravascular hemolysis is suspected, serum haptoglobins and serum hemoglobin tests should be done. Renal angiography and aortography should be done in cases of suspected dissecting aneurysm or bilateral renal artery stenosis. Abdominal ultrasound will also be helpful in diagnosing polycystic kidneys and pelvic masses that may be obstructing the ureter. In difficult cases, a renal biopsy may be necessary to diagnose the various collagen diseases and the various forms of glomerulonephritis. Intermittent anxiety suggests the possibility of psychomotor epilepsy, a pheochromocytoma, or insulinoma. It is also possible that the patient is suffering from an intermittent cardiac arrhythmia such as paroxysmal supraventricular tachycardia or atrial fibrillation. The young or middle-aged patient is more likely to be suffering from a psychiatric disorder, whereas the older patient may be suffering from cerebral arteriosclerosis or some other type of dementia. Tachycardia that is sustained during sleep would suggest hyperthyroidism, caffeine effects, or other drug effects. Sustained tachycardia with weight loss makes hyperthyroidism a very likely possibility. If routine laboratory studies and physical examination are normal, a trial of selective serotonin reuptake inhibitors may be warranted before launching on an expensive diagnostic workup. A 24-hour urine collection for catecholamines should also be done to rule out a pheochromocytoma. Twenty-four-hour Holter monitoring may be necessary to rule out a paroxysmal cardiac arrhythmia. If these are not revealing, perhaps 24-hour Holter monitoring may be of some value. It may be even wiser to consult a psychiatrist before undertaking an expensive workup. Episodic aphasia, apraxia, or agnosia would suggest epilepsy, transient ischemic attacks, migraine, or hypertensive encephalopathy. Acute onset of aphasia, apraxia, or agnosia would suggest a cerebral vascular accident, or if there is fever, the onset of a cerebral abscess. The gradual onset of aphasia, apraxia, and agnosia would suggest a tumor or other type of space-occupying lesion. Headaches with aphasia, apraxia, and agnosia might suggest migraine, but one should not forget a brain tumor. Fourvessel angiography may need to be considered, but a neurologist should be consulted before this is done. If there is associated dyspnea, one should look for congestive heart failure, pulmonary emphysema, and other cardiopulmonary conditions. Edema in the lower extremities along with significant proteinuria certainly suggests a nephrotic syndrome, whether it is caused by glomerulonephritis, diabetes, or a collagen disease. If there is no significant proteinuria, then a primary peritoneal condition such as tuberculous peritonitis or peritoneal carcinomatosis must be considered. A peritoneal tap with analysis of the fluid to determine whether it is a transudate or exudate, and cell block studies as well as amylase, culture and sensitivity should be done; an elevated amylase indicates pancreatic disease. Laparoscopy is useful in differentiating peritoneal carcinomatosis from tuberculous peritonitis. As the diagnostic tests become more expensive, the clinician should consider a referral to a gastroenterologist, nephrologist, or hepatologist before proceeding. Consultation with a cardiologist or hepatologist would be prudent before ordering expensive diagnostic tests. Neurologic examination discloses no nystagmus or papilledema, but there is definite loss of vibratory and position sense in the lower extremities and a smooth tongue. If there are long tract signs such as hyperactive reflexes and loss of vibratory or position sense, one should consider multiple sclerosis, pernicious anemia, or basilar artery insufficiency. If there are glove and stocking hypoesthesia and hypoactive reflexes, one should consider peripheral neuropathy or tabes dorsalis. Hysterical patients and patients who are malingering will often show a completely normal neurologic examination, but be unable to walk or stand without staggering. The author has been particularly impressed with patients applying for longterm disability who stagger a great deal without support, but as soon as support in the form of a cane is given, their ataxia completely clears up. If there 91 is vertigo, tinnitus, or deafness, then an audiogram and caloric testing should be done. If vascular disease is suspected, magnetic resonance angiography will allow assessment of the vertebral-basilar arteries. Patients with hypoactive reflexes and glove and stocking hypesthesia and hypalgesia will need a neuropathy workup (see page 378). When there is ataxia in the presence of a normal neurologic examination, referral to a psychologist for psychometric testing should be done. Unilateral masses are usually an abscess or enlarged lymph nodes due to some infectious process in the extremity served by the axillary nodes or the breast served by the axillary nodes. When the masses are bilateral, one should consider a systemic infection, leukemia, or advanced lymphoma. Rheumatoid arthritis and tuberculosis may be associated with bilateral axillary nodes. A painful axillary mass is usually an acute abscess or an acute inflammation of the lymph node caused by infection on the extremity or breast supplied by the lymph node or hidradenitis suppurativa. Fever with a bilateral axillary mass would suggest an acute systemic infection or infectious mononucleosis. Fever with a unilateral axillary mass would suggest that there is mastitis, a breast abscess, or lymphangitis of the extremity supplied by the axillary lymph nodes. If the mass is unilateral, are there signs of an infection on the extremity or breast supplied by the axillary nodes In tularemia, there will be a bubo on the extremity supplied by the axillary nodes, and in lymphadenitis, there should be an infectious lesion on the extremity involved. If the lymphadenitis is caused by mastitis, there should be a breast discharge or extreme tenderness and enlargement of the breast. Mammography should be done in cases of unilateral axillary masses that suggest lymphadenopathy. In the final analysis, a biopsy of the mass may need to be done to make the diagnosis. If there is fever, one should consider an infectious process, most likely a cerebral abscess. It may also be because of a spinal cord tumor or other space-occupying lesion of the spinal cord. If there is associated central facial palsy on the ipsilateral side, one should consider an infarct or a space-occupying lesion of the opposite cerebral hemisphere. If there are cranial nerve signs aside from a facial palsy, one should consider a brain stem lesion, especially if they are contralateral. Unilateral hyperactive reflexes of the upper and lower extremity with cranial nerve signs should bring to mind middle cerebral artery thrombosis or hemorrhage, carotid stenosis, and a space-occupying lesion of the brain. Hyperactive reflexes of the upper and lower extremities with no cranial nerve signs should suggest a high spinal cord tumor or a herniated cervical disk, especially if it is unilateral. Unilateral hyperactive reflexes of the lower extremity only would suggest an anterior cerebral artery thrombosis or parasagittal meningioma.
References
- Barbour PJ, Castaldo JE, Rae-Grant AD, et al. Internal carotid artery redundancy is signficantly associated with dissection. Stroke 1994;25:1201.
- Katz MD, Kligman I, Cai L-Q, et al: Paternity by intrauterine insemination with sperm from a man with 5-reductase-2 deficiency, N Engl J Med 336:994n997, 1997.
- Amin MB. Selected other problematic testicular and paratesticular lesions: rete testis neoplasms and pseudotumors, mesothelial lesions and secondary tumors. Mod Pathol 2005;18 Suppl 2:S131-45.
- Uthman I, Taher A, Abbas O, et al. Successful treatment of refractory skin manifestations of systemic lupus erythematosus with rituximab: report of a case. Dermatology 2008;216:257-9.
- Faddy MJ, Gosden RG, Gougeon A, et al. Accelerated disappearance of ovarian follicles in mid-life: implications for forecasting menopause. Hum Reprod 1992; 7:1342-1346.
- Akyol A, Akyildiz UO, Tataroglu C. Vascular Parkinsonism: a case of lacunar infarction localized to mesencephalic substantia nigra. Parkinsonism Relat Disord 2006;12(7):459-61.
- Beam E, Dioverti V, Razonable RR. Emerging cytomegalovirus management strategies after solid organ transplantation: challenges and opportunities. Curr Infect Dis Rep. 2014;16(9):419.
- Zorgniotti AW, Toth A, Macleod J: Infrared thermometry for testicular temperature determinations, Fertil Steril 32(3):347n348, 1979.