Kenneth B. Roberts, MD
- Associate Professor
- Department of Therapeutic Radiology
- Yale University School of Medicine
- Attending Physician
- Department of Radiation Oncology
- Yale-New Haven Hospital
- New Haven, Connecticut
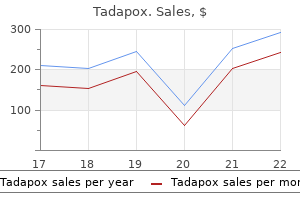
Endoleaks can appear during the first 30 days after implantation erectile dysfunction 31 years old purchase genuine tadapox online, in which case they are termed primary erectile dysfunction specialist doctor tadapox 80mg without prescription. The reappearance of an endoleak after its spontaneous resolution or after it was treated is termed a recurrent endoleak erectile dysfunction drugs patents generic tadapox 80mg. These leaks are usually corrected by further securing the attachment sites with angioplasty balloons can erectile dysfunction cause low sperm count order tadapox no prescription, stents impotence 20 years old cheap tadapox 80 mg on-line, or stent graft extensions. They can be minimized by careful patient selection and accurate preprocedural measurements. The greater the number of patent side branches, the greater the likelihood of leak formation. Preprocedural embolization of patent lumbar or inferior mesenteric arteries is not performed routinely. Metallic coils are then used to embolize the vessel near its communication with the aneurysm. A percutaneous translumbar approach has also been described; this involves direct puncture of the aneurysm sac at the level of the endoleak using a 19-gauge, 20-cm needle. Liquid embolic agents such as n-butyl cyanoacrylate have also been successfully used. When such an endoleak occurs, there is direct communication between systemic arterial blood and the aneurysm sac, which must be repaired immediately on diagnosis. Such endoleaks can usually be corrected by bridging the defect with a stent graft extension. These leaks are believed to be the most dangerous because of rapid repressurization of the aneurysm sac. At present, the management and treatment of endoleaks remain a work in progress, despite advances in stent graft technology. More and continued investigations are needed to determine when and how patients with endoleaks are managed after endovascular aneurysm repair. In summary, a successful stent graft procedure should result in successful implantation of the device, thereby preventing aneurysm rupture by permanently excluding the aneurysm from the arterial circulation while retaining long-term device patency. Early results are promising, but the future role of this treatment modality is not certain. Imaging will continue to have a pivotal role in the preprocedural evaluation of patients with abdominal aortic aneurysms and surveillance of their repairs. Patients with stent grafts should have lifelong follow-up, both clinically and radiologically. Various complications may occur after endovascular implantation of a stent graft, and many of these can be treated by interventionalists. Some complications are potentially fatal and interpreting physicians need to be familiar with their appearance. Awareness and understanding of potential complications should help ensure a safe and successful procedure. Endovascular repair of abdominal aortic aneurysms: current status and future directions. A meta-analysis of 21,178 patients undergoing open or endovascular repair of abdominal aortic aneurysm. Surgical repair of ruptured abdominal aortic aneurysms in the state of Maryland: factors influencing outcome among 527 recent cases. Selection and preparation of high-risk patients for repair of abdominal aortic aneurysms. Abdominal aortic and iliac artery aneurysms: clinical presentation, natural history, and indications for intervention. Solitary aneurysm of the iliac artery system: an estimate of their frequency of occurrence. Early results of endovascular aortic aneurysm surgery with aortouniiliac graft, contralateral iliac occlusion, and femorofemoral bypass. Abdominal aortic aneurysms: preliminary technical and clinical results with transfemoral placement of endovascular self-expanding stent grafts. Endoleak as a predictor of outcome after endovascular aneurysm repair: AneuRx multicenter clinical trial. Clinical outcome of internal iliac artery occlusions during endovascular treatment of aorto-iliac aneurysmal diseases J Vasc Interv Radiol 2000; 11:567-571. However, it is also a major operation, with the potential for significant blood loss, stress on the cardiopulmonary system, and a prolonged hospital stay. In particular, patients who have significant comorbidities have a significantly increased mortality risk associated with the procedure. A limitation of endovascular repair, however, is that patients with certain types of vascular anatomy are not candidates for the procedure. For example, some length of nonaneurysmal infrarenal aorta (depending on the device used) must be present for placement of the proximal attachment of the endovascular graft. Aortic neck angles more than 45 degrees are often problematic for proper endograft implantation and may result in excessive stress on the device. Trapezoidal, conical, or thrombus-filled aortic necks may cause device instability. In a healthy patient with any of these limitations of anatomy, open surgical repair may be the preferred option. In one study, there was no significant difference in mortality rates between the two procedures, and although retroperitoneal repair was associated with less frequent respiratory failure, it was also associated with more frequent wound complications. Attention should also be given to possible aneurysms of the hypogastric and external iliac arteries. The common and external iliac arteries may be severely affected by atherosclerotic disease, and may require arterial bypass grafting. These aneurysms require greater exposure than infrarenal aneurysms, and are technically more demanding. Repair of juxtarenal, pararenal, or suprarenal aneurysms require suprarenal clamping, which are associated with increased risk for renal damage because of ischemia. The incidence of renal failure peaks within the initial 3 days following surgery and between 1 and 4 weeks postoperatively. Cardiac-related complications, including arrhythmia, infarction, and congestive heart failure, occur in about 10% to 15% of patients after elective aneurysm repair. Perioperative renal dysfunction predicts a poorer prognosis and correlates with poor preoperative renal function. Insufficient management of pulmonary disease is also associated with a poorer prognosis. Peripheral ischemia develops in less than 1% of patients postoperatively, but may occur because of damage to diseased arteries during cross clamping, iliac dissection, or peripheral embolization from aortic plaque. Spinal cord ischemia, which may result in paralysis, can occur secondary to a variety of differing factors. The artery of Adamkiewicz may arise below L3 in a minority of patients and ligation of a lumbar artery in the aneurysm sac in such a patient may lead to spinal cord ischemia. An additional cause is suprarenal or supraceliac cross clamping that compromises the spinal cord circulation. Colonic ischemia most commonly develops because of ligation of the inferior mesenteric artery. The ureter may have a variant course in patients with renal anomalies such as horseshoe kidney, further raising the likelihood for its injury. Options for repair of ureteral injury include placement of a stent and reimplantation of the injured ureter into the bladder. The suprarenal aorta is of particular concern in fenestrated and branched stent grafts. Postoperative Mortality and Survival the postoperative mortality rate for elective open repair is approximately 5%; it is lower in younger healthier patients and higher in older at-risk patients. Additional factors include the experience of the operating surgeon, need for urgent (rather than elective) repair, and hospital volume (hospitals with higher surgical volumes generally have a lower mortality rate than those with lower volumes). Surgical Conversion from Endovascular Repair Conversion from endovascular to open repair may be required for a number of reasons (Table 104-1). In one study, the mortality rate of patients who underwent emergency conversion operations was 40%. Erectile dysfunction may occur because of poor flow through the internal pudendal artery as a result of narrowing or occlusion, ligation of the internal iliac artery, an embolus or emboli in the distal pudendal arteries, or injury to the sympathetic nerves in the fascia surrounding the aorta. Other late complications include pseudoaneurysm formation, graft thrombosis, infection, aortoenteric fistula, aneurysm rupture, colonic ischemia, and peripheral embolism. Flank ecchymosis (the Grey-Turner sign) may be apparent, and reflects retroperitoneal hemorrhage. It does not contain all the layers normally present in an arterial wall and are at risk for rupture. Anastomotic pseudoaneurysms most commonly result from arterial degeneration or infection. Pseudoaneurysms may also manifest with symptoms caused by compression of adjacent structures or acute limb ischemia, or as an asymptomatic pulsatile mass. Some patients present with a herald bleed followed by temporary stoppage and then severe hemorrhage. These patients may present with a herald upper gastrointestinal bleed followed by severe hemorrhage. Ultrasound is an operator-dependent modality and is often suboptimal in patients who are obese or of large body habitus and in patients with excessive overlying bowel gas may obscure proper visualization of the abdominal aorta. Associated septicemia, wound infection, and graft dysfunction from thrombosis or hemorrhage from the anastomotic site may occur. Infections that occur more than 4 months postoperatively may present with more subtle signs and symptoms, and a fever may be absent. Such patients have a higher likelihood of presenting with signs of complications from their aortic graft infection, such as pseudoaneurysm, aortoenteric fistula, hydronephrosis, or osteomyelitis. Patients with an aortocaval fistula most commonly present with abdominal pain, back pain, and dyspnea. On physical examination, a machinery-type abdominal bruit may be auscultated, and an abdominal thrill may be palpated. Occasionally, color and Duplex scanning are useful, such as in the identification of an aortocaval fistula. Oral water-soluble contrast, however, is helpful for the evaluation of a suspected aortoenteric fistula in a patient who is not actively bleeding. A delayed-phase acquisition (90 to 120 seconds postcontrast, 2- to 3 mmreconstructions) is also carried out to evaluate the abdomen and pelvis. Angiography may also be performed prior to planned endovascular repair to evaluate tortuous proximal aneurysm necks and tortuous iliac arteries. In cases of end-to-side proximal anastomosis, the enhancing graft may be seen running ventral and parallel to the nonenhancing diseased or aneurysmal aorta, which is now collapsed. The graft bifurcation is at a higher level compared with the now occluded native bifurcation in cases of aortic-bi-iliac or aortobifemoral grafts. In cases of more complicated grafts such as combined unilateral aortoiliac with or without femoral to femoral bypass, knowledge of surgical history helps the interpreting physician to follow the graft as an enhancing tubular structure from the site of the proximal to distal anastomosis. Most (90%) of these occur between the aortic bifurcation and iliac veins or distal vena cava. Duplex ultrasound demonstrates high-velocity flow in the inferior vena cava or the left renal vein. Aortic Graft Infection Aortic graft infection occurs in 1% to 5% of reconstructions. However, abnormal perigraft soft tissue density may also represent hematoma, fibrosis, and/or postoperative changes. Although the normal graft has surrounding fat attenuation in the early postoperative period, there should be less than 5 mm of soft tissue attenuation between the aneurysm wall and underlying graft. Persistent fluid or soft tissue attenuation around the graft may persist for up to 3 months after surgery. Similarly, pockets of gas around the graft may be present for up to 10 days after surgery, but persistence after about 4 weeks postsurgery suggests infection. B, Delayed-phase acquisition demonstrates a left renal nephrogram and infarction of the right kidney with lack of enhancement sparing the lower pole. Aortoenteric Fistula Secondary aortoenteric fistula is a rare but severe complication after abdominal aortic surgery, with mortality rates approaching 100%. They often result from infection near the proximal anastomosis between the aorta and prosthesis. It is estimated that 80% of secondary aortoenteric fistulas involve the duodenum; typically, its third and fourth parts are affected. These fistulae may occur at any time between 2 weeks and many years after surgery. Conventional x-ray catheter angiography may be combined with embolization and/or stent placement for therapy. B, this fluid collection extended inferiorly into the iliac fossa as well as medially and was incorporated with the ventral margin of the psoas major muscle (short arrow) and with the wall of the left lateral aortic aneurysm wall (long arrow). The aortic graft is wrapped by the native aortic wall and moderate intervening abnormal fluid is present, indicating graft infection. An axial T2-weighted image in a patient with graft anastomosis to the femoral artery shows low signal intensity (arrow) around the vessels, consistent with postoperative fibrosis. Fluid, on the other hand, demonstrates high signal intensity on T2-weighted sequences, as noted within the right inguinal canal (red arrow). Ultrasound may demonstrate a focal area of increased echogenicity associated with an absent or tardus parvus Doppler waveform. Renal scintigraphy may show a focal photopenic area corresponding to the area of infarction.
Diseases
- Hypoplastic left heart syndrome
- Egg hypersensitivity
- Aortic window
- Acute myeloblastic leukemia without maturation
- Alport syndrome macrothrombocytopenia
- Desbuquois syndrome
- Essential thrombocytosis
- 5-Nucleotidase syndrome, rare (NIH)
The major limitation of this technique is dependence on accurate designation of the course of the renal artery erectile dysfunction pills sold at gnc order 80 mg tadapox free shipping. In addition erectile dysfunction icd 9 code 2013 purchase generic tadapox pills, because the images are only a single voxel in thickness erectile dysfunction cleveland clinic cheap tadapox 80 mg overnight delivery, small or thin structures may not be included in the tomogram image causes of erectile dysfunction include quizlet tadapox 80mg amex. Then erectile dysfunction medicine reviews generic tadapox 80mg visa, the value of each voxel is determined by the maximum value along an array directed perpendicular to the imaging plane and through the volumetric data set. By subtracting the precontrast data set from the postcontrast data set, the resulting postprocessed data set will contain only information regarding the distribution of contrast material. Various filters may be applied to the source data to create different colors or degrees of opacity corresponding to each voxel value. In this manner, certain voxel values may be emphasized or minimized to evaluate specific structures. Accessory renal arteries and unexpected anatomic variants may be easier to appreciate with these images. The limitation of this technique is the potential to create or overlook pathology because many of the attributes of the image are arbitrarily determined. For instance, the colors and degrees of transparency are user-defined variables and may be vulnerable to error. For renal artery stenosis, the segment of vessel involved, length of stenosis, and grading of degree of stenosis should be reported. Finally, other nonvascular findings such as renal size, renal parenchymal assessment, and other incidental findings should be included. The aorta should be described in regard to its course, caliber, and presence of pathology (atherosclerotic disease, aortic aneurysm, aortic dissection, etc. Metformin hydrochloride all right before, but not after, contrast medium administration. The effects of time varying intravascular signal intensity and k-space acquisition order on three-dimensional mr angiography image quality. Three-dimensional phase-contrast magnetic resonance angiography: a useful clinical adjunct to gadolinium-enhanced three-dimensional renal magnetic resonance angiography. In patients with a hemodynamically significant reduction in renal artery caliber, there is a reduction in renal perfusion pressure distal to the stenosis. This results in the activation of the renin-angiotensin-aldosterone system, whereby renin is released from the juxtaglomerular apparatus, and a cascade of events occurs that ultimately leads to peripheral vasoconstriction, blood volume increase, and an elevation in blood pressure. There is also an increase in the creatinine level, which is the most common reason for pursuing a diagnosis of renal vascular disease. Ideally, continuous blood pressure monitoring should be performed and personnel trained in basic cardiopulmonary resuscitation should be immediately available in case of hypotension. An intravenous line can be placed for hydration, and should be used for those patients who are at high risk of cardiac disease and those receiving intravenous enalaprilat. Patients should not be discharged home unless their blood pressure is at least 70% of their baseline blood pressure. Calcium channel blockers have been reported to cause false-positive results and cessation prior to the study should also be considered. Oral captopril or intravenous enalaprilat may be used, although captopril is used more commonly. The oral captopril dose is 25 to 50 mg in adults, and 1 mg/kg in children, with a maximum dose of 50 mg. The captopril tablet is generally crushed and dissolved in water to ensure better gastric absorption. Peak systemic concentrations of captopril occur around 60 minutes after administration and then begin to decrease; therefore, the radiopharmaceutical is injected 60 minutes following captopril administration. Patients receiving oral captopril should avoid solid foods for at least 4 hours prior to administration to aid gastric absorption, although normal hydration should be continued. The radiopharmaceutical may be given 15 minutes following enalaprilat administration and the intravenous line should be maintained, because enalaprilat administration may be associated with more significant hypotension. The use of enalaprilat avoids the problem of uneven or incomplete gastric absorption, which could be an issue with captopril. In addition, the shorter waiting period prior to injection may also lead to a shorter study duration than when using oral captopril. Captopril is generally more widely used and therefore will be discussed in this chapter. Patients should be appropriately hydrated, because dehydration can affect renal perfusion curves. Hydration will also help decrease radiation dose to the bladder wall5 and to the surrounding reproductive organs by diluting the radioactivity in the bladder. Patients can receive oral or intravenous hydration, although intravenous hydration is generally preferred with enalaprilat. A baseline blood pressure reading should be taken and recorded prior to administration of the medication. At the culmination of the study, a final blood pressure reading should be taken prior to discharge home. Patients receiving enalaprilat should have blood pressure measured every 5 minutes during the examination. The patient should void when the waiting period comes to an end, prior to imaging, because a full bladder may affect emptying of the upper tract6 and could also lead to premature termination of the study if the patient needs to void during imaging. The patient is then brought into the scan room and positioned supine on the imaging table with the camera located posteriorly to ensure that the kidneys are lying at the same depth, which could be affected with the patient semirecumbent or sitting. The study should be dynamic, with the first series generally consisting of 1 sec/ frame for 1 minute to assess early perfusion, the second series consisting of 5 sec/frame for 24 frames, and the final functional sequence, 30 sec/frame for 60 frames, for a total imaging time of approximately 30 minutes. The patient should void at the end of the study to reduce radiation dose to the kidneys, bladder, and pelvic organs. A postvoid bladder residual can also be calculated with a postvoid image consisting of a single 60-sec/frame image. Correction for infiltration can be done by imaging the injection site and qualitatively or quantitatively assessing the injection dose. A quantitative evaluation is performed by determining the ratio of infiltrated counts to the original counts in the injected dose; with this method, syringe counts should be calculated prior to injection. Assessment of a region of interest over the abdominal aorta during the immediate postinjection perfusion phase can also provide information about the quality of the injection bolus. The 1-day protocol requires the patient to visit the imaging department only once, but the length of time spent may be longer than with the 2-day protocol. It is helpful to obtain a single static postvoid image of the kidneys and bladder prior to the second injection of the radiopharmaceutical to assess how much, if any, residual activity remains, because residual activity could interfere with interpretation of the second imaging sequence. Following radiotracer injection, the loop diuretic furosemide may also be administered intravenously to clear radiotracer activity from the collecting system, reducing retention which could otherwise confound quantitative assessment. These patients generally are found to have ischemic nephropathy, often with a small shrunken kidney. Bilateral cortical retention is more often caused by dehydration or a hypotension artifact rather than bilateral renal artery stenosis. An increase in the 20/peak (ratio of cortical activity at 20 minutes to the amount of peak activity) or 20/3 ratio (count activity at 20 minutes divided by the activity at 3 minutes). Grades 1 through 3 reflect progressive worsening from baseline, with increasing grade indicating more corresponding profound changes. An increase in time to maximum parenchymal uptake (Tmax) of at least 2 to 3 minutes. Chronic administration of certain antihypertensives can reduce specificity of the examination and these medications may need to be held prior to the study. Computer quantification can aid in interpretation and has been found to be useful in reducing false-positive results in patients with mildly abnormal perfusion at baseline. A, the captopril study was performed first and revealed asymmetric renal function and bilateral cortical retention. B, A baseline scan shows continued renal asymmetry but with normalization of right renal function and a small change in the left. A change of 10% or more in differential function, the amount each kidney contributes to overall function. The curves can be summarized as follows: grade 0, normal curve; grade 1, peak mildly delayed (longer than 5 minutes) and with delayed excretion; grade 2, very delayed uptake but some washout; grade 3, extremely delayed uptake with no washout; grade 4, complete renal failure, in which the blood pool moves through the kidney in the vascular phase, with no extraction phase. Society of Nuclear Medicine Procedure Guideline for Diagnosis of Renovascular Hypertension, version 3. Calcium channel blockers: a potential cause of false-positive captopril renography. The effect of hydration on the dose to the urinary bladder wall during technetium-99m diethylene triamine penta-acetic acid renography. Dogra Sonography of renal vessels in modern practice combines the use of gray-scale, color Doppler, power Doppler, and contrast-enhanced ultrasound imaging. Duplex sonography of renal vessels is a common screening modality for the evaluation of hypertensive patients worldwide because it is the most inexpensive and noninvasive imaging method. Duplex sonography has proven to be a good modality for the assessment of flow in renal and intrarenal vessels and enables measurement of flow parameters that are significant in many kidney diseases. Renal artery stenosis is the most common curable cause of hypertension and of end-stage renal disease as well. Sonography plays a vital role in the detection of renal artery stenosis and occlusion, and in the follow-up of renal stents and renal allografts. In addition, sonography of renal vessels is used to evaluate numerous other conditions, such as renal vein thrombosis and renal tumors. Renal Doppler ultrasound also provides valuable information regarding urinary tract obstruction and various other renal parenchymal diseases. Clinically, renal arterial indications are more common, notably for the evaluation of possible renal artery stenosis. Renal Artery Stenosis the detection of renal artery stenosis in hypertensive patients. However, because it is one of the few treatable causes of hypertension, second only to the secondary hypertension caused by the use of oral contraceptives in women,5 it remains a common indication for renal artery imaging. Renovascular hypertension is also responsible for the development of endstage renal disease in 20% of patients. Additionally, ultrasound contrast agents can aid in the sonographic evaluation of renal vessels. The highest transducer frequency that will provide the best resolution should be selected, depending on the depth of penetration required. About one third of patients with medial fibroplasia show progression of the disease, but complications such as dissection and thrombosis are rarely seen. Takayasu Arteritis Takayasu arteritis, or nonspecific arteritis, is associated with stenosis (and occlusion) of the aorta and renal arteries. The disease predominantly involves the media of the vessel and then progresses to cause fibrosis of intima and the adventitia. Most of the patients present during adulthood, very frequently during the third decade of life. Renal Artery Thrombosis A renal artery can be occluded by atherosclerotic embolism, thromboembolism, thrombus in situ, aortic dissection, or vasculitis. Renal artery embolism is a common cause of renal insufficiency in older patients, especially those with atherosclerosis. Renal artery thromboembolism can occur in association with a variety of conditions, such Text continued on p. A, Longitudinal gray-scale image in right lateral decubitus position reveals the longitudinal dimension of the right kidney to be 8. C, Pulse wave Doppler imaging at the origin of the right renal artery reveals a peak systolic velocity of 4. D, Pulse wave Doppler of the middle segmental artery reveals an acceleration time of 0. A, Color Doppler image depicting left renal artery stenosis as an area of color aliasing (arrow). D, Spectral waveform of middle segmental artery reveals a tardus parvus waveform supporting the diagnosis of a hemodynamically significant renal artery stenosis. Gray-scale longitudinal images of right (A) and left (B) kidneys reveal considerable differences in the longitudinal dimensions of both kidneys. D, Spectral waveform of right upper segmental artery reveals pulsus tardus parvus waveform. A, Color aliasing (short arrow) is seen in the proximal segment (arrowhead) of the right renal artery. B, Pulse wave Doppler image of the proximal segment of main renal artery reveals a peak systolic velocity of 452 cm/sec. C, Accessory renal artery (long arrow) is seen arising from the aorta (short arrow). D, Pulse wave Doppler ultrasound image of the accessory renal artery reveals a normal peak systolic velocity of 145. Renal angiography reveals stenosis of the middle segment of the renal artery supplying the allograft (arrow). Color aliasing (arrow) is seen at the site of stenosis of the left (A) and right (B) renal arteries. B, Color Doppler image shows stenosis at the origin of right renal artery (arrow). A, Color Doppler image of aorta in longitudinal plane shows smooth long segment of narrowing of the aorta, with areas of moderate (arrowheads) to severe stenosis (arrows).
Cheap tadapox online amex. Top 8 Erectile Dysfunction Remedies - by Dr Sam Robbins.
A validation study on the intraobserver and interobserver reproducibility of renal artery duplex ultrasound erectile dysfunction drugs and nitroglycerin order tadapox. Contrast-enhanced breath-hold three-dimensional magnetic resonance angiography in the evaluation of renal arteries: optimization of technique and pitfalls erectile dysfunction treatment adelaide cheap tadapox 80mg mastercard. A dual-chamber power injector and a dedicated 3D workstation are also recommended erectile dysfunction labs generic 80 mg tadapox amex. Often erectile dysfunction treatment delhi cheap tadapox 80 mg otc, there is generalized or diffuse atherosclerotic plaque formation with concomitant involvement of the aorta and the ostium or proximal segment of the main renal artery erectile dysfunction recreational drugs effective tadapox 80mg. Renal Donor Evaluation Many renal transplantations are performed with living renal donors because of the insufficient availability of cadaveric kidneys. The renal and vascular anatomy, etiology of obstruction, functional significance of obstruction and concomitant conditions will determine the treatment approach. The vascular features of the tumor may assist staging of the tumor and presurgical planning. Also, the detection of accessory renal arteries or possibly extracapsular feeding arteries of a renal malignancy are important preoperative determinations because knowledge of their presence will minimize intraoperative bleeding complications, especially for laparoscopic nephrectomies, which are becoming increasingly popular surgeries. Patients may develop skin thickening to such an extent that it results in decreased joint mobility. Fibrosis may also occur in other parts of the body including the diaphragm, musculature of the lower abdomen and extremities, and the pulmonary vasculature. Consequently, extreme caution is advised in administering gadolinium-based contrast material in those patients with advanced renal failure. Multidetector row array technology and slip-ring gantry design allow volumetric coverage from the upper abdominal aorta through the common iliac arteries within one breath-hold. The data set may be reconstructed at different slice thicknesses to review the images. The development of acute renal impairment secondary to contrastinduced nephropathy may prohibit proper clearance of metformin, which is eliminated through the kidneys, and result in lactic acidosis. However, the drawback of using less contrast material is the shortened duration of the contrast bolus, which increases the challenge for proper coordination of imaging with opacification of the arteries. That is to say, if scanning is too fast, imaging may occur prior to complete opacification of the target vasculature, resulting in suboptimal arterial contrast enhancement and poor arterial visualization. Alternatively, if scanning is slow or performed too late, images would illustrate the venous phase of the bolus with suboptimal arterial enhancement, Consequently, it is important to accurately determine circulation time to achieve an optimal scan. In this technique, a small test dose of contrast material, 10 to 15 mL, is infused at a rate of 3 to 4 mL/sec followed by repetitive scans obtained at the level of the upper abdominal aorta at 2-second intervals. The main drawbacks with this technique include the higher volume of contrast administered and the additional ionizing radiation dose associated with the timing bolus. In this technique, a region of interest is selected in the upper abdominal aorta at approximately the level of the celiac artery. Although this technique results in a lesser amount of contrast administered than the timing bolus technique, the additional nondiagnostic ionizing radiation dose is comparable to that required for a timing test bolus scan. The drawback with this technique is the time lag between contrast opacification exceeding the threshold and actual initiation of the scan. For instance, selecting too low a threshold may initiate the scan before peak opacification is achieved. Alternatively, selecting too high a threshold may miss the peak enhancement phase or not trigger the scan at all. The patient is placed in the supine position and intravenous access is obtained in the upper extremity. The phased-array coil permits implementation of parallel imaging techniques, which can shorten acquisition times and increase image resolution. The arms are propped up anterior to the level of the coil to avoid wrap-around artifact. For instance, this techniques enables the detection of microscopic or intravoxel fat within adrenal adenomas. The acquisition times are generally less than 1 second permitting essentially motion-free T2-weighted images. This technique is useful in uncooperative patients or patients who cannot adequately breath-hold. The complete volume of the adrenal glands and kidneys may be imaged within a single breath-hold to minimize respiratory and other motion artifacts and allow advanced 3D image postprocessing. Contrast infusion time is the duration of the contrast infusion (10 sec for 20 mL of contrast infused at 2 mL/sec). If a centric phase ordering is used, the central lines of k-space are acquired at the beginning of data acquisition and scan delay is typically timed by simply adding 2 seconds to the circulatory time. The addition of 2 seconds minimizes the risk for ringing artifacts that can occur if central k-space views are sampled during the rapid rise in gadolinium concentration. With alternate acquisition of the tagged and nontagged images and subtracting these two data sets, a bright blood image, without background signal, can be obtained. It is less effective in regions of slow flow, such as within the peripheral arteries, where blood in the imaging volume is not being adequately replaced by tagged blood. Third, extensive computational time is required to integrate the independent data from multiple channels. Finally, the signal-to-noise ratio will be decreased inversely with the acceleration factor because of the under-sampling of k-space. In any case, the source data should be routinely evaluated to corroborate specific findings. This technique uses the difference in signal detected by receiver coils positioned over different parts of the body. By incorporating the differences in sensitivity of multiple coils to detect signal from the same source, information regarding spatial localization may be obtained and may reduce the number of phase-encoding steps required to produce an image. First, special coils must be designed with independent coil elements having their own receiver channels. Because the renal artery may be tortuous in course, segments of the artery may course in and out of the visualization plane resulting in the appearance of pseudostenoses. This modified technique allows complete visualization of the renal artery in one plane of section. B, Spectral waveform of right middle segmental artery shows tardus parvus waveform pattern (arrows). A, Longitudinal gray-scale image shows a slightly hypoechoic area (arrows) in the lower pole of the kidney. Renal Vein Thrombosis Renal vein occlusion can occur because of thrombus formation, intraluminal tumor, or external compression of the renal vein. Anatomic Considerations Renal Arteries Both renal arteries arise from the abdominal aorta approximately 1 to 1. Sonographically, it is identified as the largest vessel seen posterior to the inferior vena cava. Gray-scale longitudinal images of the left (A) and right kidney (B) show significant differences between the longitudinal dimensions of both kidneys. Color Doppler images of the left kidney (C) and right kidney (D) reveal only residual flow in the midpole of the left kidney but normal flow in the right kidney. E, F, Color Doppler and spectral waveform images of left main renal artery (E) and left middle segmental artery (F). The right renal vein (long arrow) lies anterior to the right renal artery (short arrow). Bannister and associates17 have reported accessory renal arteries in approximately 25% to 30% of individuals; however, most imaging studies have reported these in from 12% to 22% of patients. The rate of successful imaging of the accessory renal artery varies between 0% and 24%. In the presence of a normal main renal artery, a concerted attempt should be made to search for these vessels because stenosis of an accessory renal artery can similarly result in renovascular hypertension. The left renal artery (long arrow) enters the renal hilum and divides into segmental arteries (short arrow), and the segmental artery gives rise to interlobar arteries (arrowheads). Arcuate arteries give rise to the cortical and medullary branches, which supply the cortex and medulla, respectively. Most of the blood flow (90%) to the kidney goes to the cortex, with only 10% flowing into the medulla. Intrarenal Arteries: Segmental, Interlobar, and Arcuate Arteries After entering the hilum, the main renal arteries split into anterior and posterior divisions. The arteries in these divisions give rise to segmental arteries, usually four, that supply each of the four vascular regions of the kidney- apical, anterior, posterior, and inferior. The segmental arteries give rise to lobar and interlobar arteries that travel between the medullary pyramids. On sonography, the left renal vein appears larger than the right in a supine position. The left adrenal vein, left gonadal vein, and lumbar veins are tributaries of the left renal vein. The left renal vein runs a horizontal course and is placed anterior to the aorta and posterior to the superior mesenteric artery. B, Left main renal artery (long arrow) and accessory renal artery (short arrow) are seen arising from aorta. Blood flow in the renal and adrenals veins is blue because the direction of blood flow is away from the transducer. Segmental arteries (long arrows) give rise to the interlobar arteries (short arrows), which further give rise to the arcuate arteries (arrowheads). To see the presence of atherosclerotic plaque in the abdominal aorta, the aorta should be scanned in its entirety-that is, from the origin of the celiac artery to the bifurcation of the aorta into the common iliac arteries. The ostium of the superior mesenteric artery and the celiac artery should also be assessed. In addition to atherosclerotic plaque, the aorta is also evaluated for any aneurysm, stenosis, coarctation, or features of aortic arteritis. If bowel gas interferes with the visualization of the aorta, the transducer can be placed in paramedian longitudinal planes, and medial sweeps of the transducer can then be made to facilitate visualization of the aorta. For proper color flow assessment, the parameters of the machine have to be calibrated for every patient. To do this, an area of laminar flow in the aorta is identified and this window is used to adjust color gain, pulse repetition frequency, and wall filter. After taking these measurements, the ostium of the renal arteries is identified just inferior and caudal to the origin of the superior mesenteric artery. The transducer is placed at the midpoint between the xiphoid process and umbilicus. If overlying bowel gas interferes with the examination, the transducer is swept in a cranial or caudal direction to look for the vessel. If this fails, then the liver can be used as an acoustic window to scan the proximal and middle segments of both renal arteries. The distal segment of both renal arteries is scanned, along with the intrarenal vessels, by the respective lateral and flank approaches by using the ipsilateral kidneys as acoustic windows. In children, sometimes the longitudinal span from a lateral and flank approach can help visualize both renal arteries. Main Renal Arteries Both renal arteries are assessed by gray-scale sonography for any area of narrowing of the lumen, calcification, or atherosclerotic plaque. The diameter of the main renal artery is also assessed in its proximal segment (proximal 2 cm). Color flow Doppler is then used to visualize any areas of turbulence and color aliasing. Both renal veins are also assessed for patency, along with the examination of renal arteries. As far as color Doppler and spectral wave imaging of the renal arteries is concerned, the ideal transducer position is one in which the direction of blood flow in the vessel is parallel to the ultrasound beam and the Doppler angle of insonation is almost 0 degrees. Practically, this is only possible in very thin and cooperative patients who can hold their breath reliably. A normal spectral waveform in the renal artery is that of low resistance with continuous forward diastolic flow. This results in a Doppler angle of nearly 0 degrees and blood flow is seen as red because its direction is toward the transducer. If the anterior transverse approach is not successful, the patient is rotated 45 degrees to the right anterior oblique position. A, Color Doppler image of the aorta shows the sampling gate (long arrow) placed at an area of laminar flow in the aorta, which is usually at the level of origin of the renal arteries (short arrows). B, Color and pulse wave Doppler image shows the sampling gate (arrow) in the proximal segment of renal artery (also see. The transducer is placed slightly to the left of midline and rotated toward the right so that blood flow of the middle segment of the right renal artery is parallel to the ultrasound beam. If this anterior approach is unsuccessful, a lateral approach through the liver is used. Sometimes, pediatric patients are placed in the right lateral decubitus position; a longitudinal scan through the left kidney provides a good view for adequate visualization of both renal arteries. In situations in which other approaches to assess the proximal and middle segments of renal arteries fail because of bowel gas, morbid obesity, or inability to hold the breath, the lateral approaches in decubitus positions are used to assess the proximal two thirds of both renal arteries. An additional approach that yields a banana or banana peel view is also popular with renal sonographers. A, Spectral waveform pattern in main renal artery is of low impedance with continuous forward diastolic flow and a characteristic early systolic peak (arrow) at the end of the systolic rise.
Psyllium afra (Black Psyllium). Tadapox.
- Constipation.
- Improving high cholesterol.
- Are there any interactions with medications?
- What other names is Black Psyllium known by?
- What is Black Psyllium?
- Cancer, diarrhea, irritable bowel syndrome (IBS), and other conditions.
- Are there safety concerns?
- How does Black Psyllium work?
- Dosing considerations for Black Psyllium.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96139
References
- Williams HE, Smith LH Jr: L-glyceric aciduria. A new genetic variant of primary hyperoxaluria, N Engl J Med 278(5):233n238, 1968.
- Tabernero J, Yoshino T, Cohn AL, et al. Ramucirumab versus placebo in combination with second-line FOLFIRI in patients with metastatic colorectal carcinoma that progressed during or after first-line therapy with bevacizumab, oxaliplatin, and a fluoropyrimidine (RAISE): a randomised, double-blind, multicentre, phase 3 study. Lancet Oncol 2015;16(5):499-508.
- Casillas S, Delaney CP, Senagore AJ, et al. Does conversion of a laparoscopic colectomy adversely affect patient outcome? Dis Colon Rectum 2004;47:1680-85.
- Berrouschot J, Sterker M, Bettin S, et al. Mortality of spaceoccupying ('malignant') middle cerebral artery infarction under conservative intensive care. Intensive Care Med 1998;24:620-3.
- Heriot AG, Tekkis PP, Constantinides V, et al. Meta-analysis of colonic reservoirs versus straight coloanal anastomosis after anterior resection. Br J Surg 2006;93(1):19-32.
- Wright AS, Douglas RC, Thomas LN: Androgen-induced regrowth in the castrated rat ventral prostate: role of 5alpha-reductase, Endocrinology 140(10):4509n4515, 1999.
- Lindau A. Zur frage der angiomatosis retinae und ihrer hirncomplikation. Acta Ophthal 1927;4:193-226.