Leonard Kaban, DMD, MD, FACS
- Walter C Guralnick Professor and Chairman
- Department of Oral and Maxillofacial Surgery
- Harvard School of Dental Medicine
- Chief, Department of Oral and Maxillofacial Surgery
- Massachusetts General Hospital
- Boston, Massachusetts
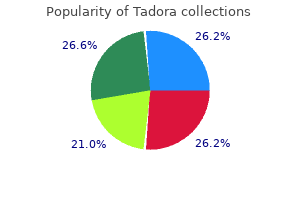
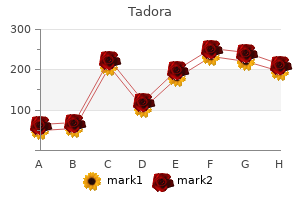
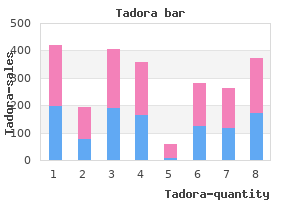
Food and Drug Administration requires that Nutrition Facts labels portray the trans fat content of packaged food erectile dysfunction toys buy cheap tadora 20 mg line. Some municipalities erectile dysfunction treatment electrical generic tadora 20 mg free shipping, such as New York City, have banned the use of trans fats in restaurants. However, because of the potential dangers of alcohol abuse, health professionals are reluctant to recommend increased alcohol consumption to their patients. Red wine may provide cardioprotective benefits in addition to those resulting from its alcohol content (for example, red wine contains phenolic compounds that inhibit lipoprotein oxidation; see p. Although caloric intake in the United States has shown a modest increase since 1971, the incidence of obesity has dramatically increased (see p. During this same period, carbohydrate consumption has significantly increased (as fat consumption decreased), leading some observers to link obesity with carbohydrate consumption. However, obesity has also been related to increasingly inactive lifestyles and to calorie-dense foods served in expanded portion size. Classification of carbohydrates Dietary carbohydrates are classified as simple sugars (monosaccharides and disaccharides), complex sugars (polysaccharides), and fiber. Monosaccharides: Glucose and fructose are the principal monosaccharides found in food. Free fructose is found together with free glucose and sucrose in honey and fruits (for example, apples). Disaccharides: the most abundant disaccharides are sucrose (glucose + fructose), lactose (glucose + galactose), and maltose (glucose + glucose). Polysaccharides: Complex carbohydrates are polysaccharides (most often polymers of glucose) that do not have a sweet taste. Starch is an example of a complex carbohydrate that is found in abundance in plants. Common sources include wheat and other grains, potatoes, dried peas and beans, and vegetables. Fiber: Dietary fiber is defined as the nondigestible, nonstarch carbohydrates and lignin (a noncarbohydrate polymer of aromatic alcohols) present intact in plants. Soluble fiber is the edible parts of plants that is resistant to digestion and absorption in the human small intestine but is completely or partially fermented by bacteria to short-chain fatty acids in the large intestine. Fiber can absorb 10 15 times its own weight in water, drawing fluid into the lumen of the intestine and increasing bowel motility and promoting normal laxation. This delayed emptying also results in reduced peaks of blood glucose following a meal. Also, fiber-rich diets decrease the risk for constipation, hemorrhoids, and diverticulosis. Dietary carbohydrate and blood glucose Some carbohydrate-containing foods produce a rapid rise followed by a steep fall in blood glucose concentration, whereas others result in a gradual rise followed by a slow decline. Requirements for carbohydrate Carbohydrates are not essential nutrients, because the carbon skeletons of most amino acids can be converted into glucose (see p. However, the absence of dietary carbohydrate leads to ketone body production (see p. It is recommended that added sugar represent no more than 25% of total energy because of concerns that sugar may displace nutrient-rich foods from the diet, potentially leading to deficiencies of certain micronutrients. Simple sugars and disease There is no direct evidence that the consumption of simple sugars is harmful. Contrary to folklore, diets high in sucrose do not lead to diabetes or hypoglycemia. However, there is an association between sucrose consumption and dental caries, particularly in the absence of fluoride treatment. Nine of the 20 amino acids needed for the synthesis of body proteins are essential (that is, they cannot be synthesized in humans). Quality of proteins the quality of a dietary protein is a measure of its ability to provide the essential amino acids required for tissue maintenance. This amino acid score provides a method to balance intakes of poorer-quality proteins with high-quality dietary proteins. It has a low biologic value as a result of deficiencies in several essential amino acids. Proteins from plant sources: Proteins from plant sources have a lower quality than do animal proteins. However, proteins from different plant sources may be combined in such a way that the result is equivalent in nutritional value to animal protein. For example, wheat (lysine deficient but methionine rich) may be combined with kidney beans (methionine poor but lysine rich) to produce an improved biologic value. Positive nitrogen balance: this occurs when nitrogen intake exceeds nitrogen excretion. It is observed during situations in which tissue growth occurs, for example, in childhood, pregnancy, or during recovery from an emaciating illness. Negative nitrogen balance: this occurs when nitrogen loss is greater than nitrogen intake. It is associated with inadequate dietary protein; lack of an essential amino acid; or during physiologic stresses, such as trauma, burns, illness, or surgery. Requirement for protein in humans the amount of dietary protein required in the diet varies with its biologic value. The greater the proportion of animal protein included in the diet, the less protein is required. People who exercise strenuously on a regular basis may benefit from extra protein to maintain muscle mass, and a daily intake of about 1 g/kg has been recommended for athletes. Women who are pregnant or lactating require up to 30 g/day in addition to their basal requirements. When excess protein is eliminated from the body as urinary nitrogen, it is often accompanied by increased urinary calcium, thereby increasing the risk of nephrolithiasis and osteoporosis. The protein-sparing effect of carbohydrate: the dietary protein requirement is influenced by the carbohydrate content of the diet. When the intake of carbohydrates is low, amino acids are deaminated to provide carbon skeletons for the synthesis of glucose that is needed as a fuel by the central nervous system. If carbohydrate intake is less than 130 g/day, substantial amounts of protein are metabolized to provide precursors for gluconeogenesis. Therefore, carbohydrate is considered to be "protein-sparing," because it allows amino acids to be used for repair and maintenance of tissue protein rather than for gluconeogenesis. Affected individuals show a variety of symptoms, including a depressed immune system with a reduced ability to resist infection. Kwashiorkor: Kwashiorkor occurs when protein deprivation is relatively greater than the reduction in total calories. Protein deprivation is associated with severely decreased synthesis of visceral protein. Kwashiorkor is commonly seen in developing countries in children after weaning at about age 1 year, when their diet consists predominantly of carbohydrates. Typical symptoms include stunted growth, skin lesions, depigmented hair, anorexia, enlarged fatty liver, edema, and decreased serum albumin concentration. Edema results from the lack of adequate blood proteins, primarily albumin, to maintain the distribution of water between blood and tissues. It is associated with decreased treatment tolerance and response and decreased survival time. Marasmus: Marasmus occurs when calorie deprivation is relatively greater than the reduction in protein. It usually occurs in developing countries in children younger than age 1 year when breast milk is supplemented with watery gruels of native cereals that are usually deficient in both protein and calories. The energy generated by the metabolism of the macronutrients is used for three energy-requiring processes that occur in the body: resting metabolic rate, physical activity, and thermic effect of food. Dietary w-3 polyunsaturated fats suppress cardiac arrhythmias and reduce serum triacylglycerols, decrease the tendency for thrombosis, and substantially reduce the risk of cardiovascular mortality. When they are consumed as part of a diet in which caloric intake is equal to energy expenditure, they do not promote obesity. The quality of a protein is a measure of its ability to provide the essential amino acids required for tissue maintenance.
Syndromes
- Contractures of heels and legs
- Puncture to the lung if the neck or chest veins are used, causing lung collapse (pneumothorax)
- Overstimulation
- Tumors
- Feeding problems
- Tell your doctor about any allergies or health conditions you have, what medicines you are taking, and what anesthesia or sedation you have had before.
Heterozygotes erectile dysfunction medicine name in india purchase tadora 20mg visa, representing 1 in 12 African Americans online erectile dysfunction drugs reviews buy tadora us, have one normal and one sickle cell gene. They usually do not show clinical symptoms (but may under conditions of extreme physical exertion with dehydration) and can have a normal life span. This altered mobility of HbS is a result of the absence of the negatively charged glutamate residues in the two chains, thereby rendering HbS less negative than HbA. This interruption in the supply of oxygen leads to localized anoxia (oxygen deprivation) in the tissue, causing pain and eventually death (infarction) of cells in the vicinity of the blockage. Variables that increase sickling: the extent of sickling and, therefore, the severity of disease is enhanced by any variable that increases the proportion of HbS in the deoxy state (that is, reduces the affinity of HbS for O2). Treatment: Therapy involves adequate hydration, analgesics, aggressive antibiotic therapy if infection is present, and transfusions in patients at high risk for fatal occlusion of blood vessels. Possible selective advantage of the heterozygous state: the high frequency of the bS mutation among black Africans, despite its damaging effects in the homozygous state, suggests that a selective advantage exists for heterozygous individuals. For example, heterozygotes for the sickle cell gene are less susceptible to the severe malaria caused by the parasite Plasmodium falciparum. One theory is that because these cells in individuals heterozygous for HbS, like those in homozygotes, have a shorter life span than normal, the parasite cannot complete the intracellular stage of its development. This fact may provide a selective advantage to heterozygotes living in regions where malaria is a major cause of death. In HbC, however, a lysine is substituted for the glutamate (as compared with a valine substitution in HbS). These patients do not suffer from infarctive crises, and no specific therapy is required. In this disease, some -globin chains have the sickle cell mutation, whereas other -globin chains carry the mutation found in HbC disease. They are called compound heterozygotes because both of their -globin genes are abnormal, although different from each other. Methemoglobinemias Oxidation of the heme iron in hemoglobin to the ferric (Fe 3+) state forms methemoglobin, which cannot bind O2. This oxidation may be caused by the action of certain drugs, such as nitrates, or endogenous products such as reactive oxygen species (see p. The oxidation may also result from inherited defects, for example, certain mutations in the - or -globin chain promote the formation of methemoglobin (HbM). They are, therefore, particularly susceptible to the effects of HbM-producing compounds. Symptoms are related to the degree of tissue hypoxia and include anxiety, headache, and dyspnea. Distribution of sickle cell in Africa expressed as a percentage of the population with disease. Thalassemias the thalassemias are hereditary hemolytic diseases in which an imbalance occurs in the synthesis of globin chains. Normally, synthesis of the - and -globin chains is coordinated, so that each -globin chain has a -globin chain partner. In the thalassemias, the synthesis of either the - or the -globin chain is defective. There are only two copies of the -globin gene in each cell (one on each chromosome 11). Because the -globin gene is not expressed until late in fetal gestation, the physical manifestations of -thalassemias appear only several months after birth. Those individuals with -thalassemia minor make some chains, and usually do not require specific treatment. However, those infants born with thalassemia major are seemingly healthy at birth but become severely anemic, usually during the first or second year of life due to ineffective erythropoiesis. If one of the four genes is defective, the individual is termed a silent carrier of -thalassemia, because no physical manifestations of the disease occur. If two -globin genes are defective, the individual is designated as having -thalassemia trait. If three -globin genes are defective, the individual has hemoglobin H (4) disease, a hemolytic anemia of variable severity. If all four -globin genes are defective, hemoglobin Bart (4) disease with hydrops fetalis and fetal death results, because -globin chains are required for the synthesis of HbF. The subunits occupy different relative positions in deoxyhemoglobin compared with oxyhemoglobin. It has a constrained structure that limits the movement of the polypeptide chains. The binding of O2 to Hb causes rupture of some of the ionic and hydrogen bonds, and movement of the dimers. The oxygen-dissociation curve for Hb is sigmoidal in shape (in contrast to that of myoglobin, which is hyperbolic), indicating that the subunits cooperate in binding O2. Cooperative binding of O2 by the four subunits of Hb means that the binding of an O2 molecule at one heme group increases the oxygen affinity of the remaining heme groups in the same Hb molecule. Fetal blood has a lower affinity for oxygen than does adult blood because HbF has an increased affinity for 2,3-bisphosphoglycerate. HbA 1c differs from HbA by a single, genetically determined amino acid substitution. HbA2 is a minor component of normal adult hemoglobin, first appearing shortly before birth and rising to adult levels (about 2% of the total hemoglobin) by age 6 months. Acidosis favors the conversion of hemoglobin from the taut to the relaxed conformation. HbS is significantly less soluble in the deoxygenated form, compared with oxyhemoglobin S. A decrease in pH (acidosis) causes the oxygen-dissociation curve to shift to the right, indicating a decreased affinity for oxygen. This favors the formation of the deoxy, or taut, form of hemoglobin, and can precipitate a sickle cell crisis. The binding of 2,3-bisphosphoglycerate is increased, because it binds only to the deoxy form of hemoglobins. Carbon dioxide increases the oxygen affinity of hemoglobin by binding to the Cterminal groups of the polypeptide chains. The oxygen affinity of hemoglobin increases as the percentage saturation increases. The binding of oxygen at one heme group increases the oxygen affinity of the remaining heme groups in the same molecule. Carbon dioxide decreases oxygen affinity because it lowers the pH; moreover, binding of carbon dioxide to the N-termini stabilizes the taut, deoxy form. Deoxyhemoglobin has a greater affinity for protons and, therefore, is a weaker acid. It should have increased O2 affinity and, consequently, decreased delivery of O 2 to tissues. Increased O2 affinity (decreased delivery) results in a left shift in the O2-dissociation curve. In HbC, the polar glutamate is replaced by polar lysine rather than by nonpolar valine as in HbS. Oxidation of the heme component of hemoglobin to the ferric (Fe 3+) state forms methemoglobin. The methemoglobinemias are characterized by chocolate cyanosis (a brownish blue coloration of the skin and mucous membranes and chocolate-colored blood) as a result of the dark-colored methemoglobin. Symptoms are related to tissue hypoxia and include anxiety, headache, and dyspnea. For example, collagen and elastin are found as components of skin, connective tissue, blood vessel walls, and the sclera and cornea of the eye. Each fibrous protein exhibits special mechanical properties, resulting from its unique structure, which are obtained by combining specific amino acids into regular, secondary structural elements. This is in contrast to globular proteins, whose shapes are the result of complex interactions between secondary, tertiary, and, sometimes, quaternary structural elements. Although these molecules are found throughout the body, their types and organization are dictated by the structural role collagen plays in a particular organ. In some tissues, collagen may be dispersed as a gel that gives support to the structure, as in the extracellular matrix or the vitreous humor of the eye. In other tissues, collagen may be bundled in tight, parallel fibers that provide great strength, as in tendons.
This is an evolving avenue of research that overall indicates that the hepatocyte has adaptive responses in place to handle cholestasis erectile dysfunction pills at walmart purchase tadora pills in toronto, and that these pathways may be amenable to pharmacological therapies [3 erectile dysfunction after stopping zoloft buy discount tadora 20mg,21,52,53]. Future expectations Although we have seen new identifications of genes associated with genetic forms of cholestasis. On a diagnostic front, it is anticipated that we will be able to explore diagnostics as well as genotypeΰhenotype correlations as more and more of these disease-causing genes become available for commercial testing (see. Nutritional and therapeutic means of enhancing the response of the liver to cholestasis [3,24], as well as knowledge about the roles of immaturity, inflammation, and diet-derived substances that may, in fact, exacerbate ongoing cholestasis, are expected to be revealed. Liver disease associated with canalicular transport defects: current and future therapies. The transporter "variome": the missing link between gene variants and bile salt transporter function. Nuclear receptor regulation of the adaptive response of bile acid transporters in cholestasis. Preliminary observations of pool size and synthesis rate following prenatal administration of dexamethasone and phenobarbital. Physiologic cholestasis: elevation of the primary serum bile acid concentrations in normal infants. A nuclear-receptor-dependent phosphatidylcholine pathway with antidiabetic effects. Molecular regulation of hepatobiliary transport systems: clinical implications for understanding and treating cholestasis. Heat stress enhances recovery of hepatocyte bile acid and organic anion transporters in endotoxemic rats by multiple mechanisms. Genetic variations of bile salt transporters as predisposing factors for drug-induced cholestasis, intrahepatic cholestasis of pregnancy and therapeutic response of viral hepatitis. Immaturity of the biliary excretory system predisposes neonates to intrahepatic cholestasis. Mechanisms of disease: update on the molecular etiology and fundamentals of parenteral nutrition associated cholestasis. Intestinal failureassociated liver disease: management and treatment strategies past, present, and future. Use of cholecystokinin to prevent the development of parenteral nutritionassociated cholestasis. Nuclear receptor ligands: rational and effective therapy for chronic cholestatic liver disease? Management requires a multidisciplinary team involving the hepatologist, critical care specialist, and liver transplant surgeon. The absence of adequately powered studies to inform diagnostic algorithms, to assess markers of disease severity and trajectory, and to guide liver transplant decisions transfers a significant burden to the clinician. Constructing a diagnostic approach and individualized management strategy that may include the decision to pursue liver transplantation is challenging. What is the risk of deterioration or improvement on each day the child is alive with his/her native liver? The "onset of jaundice" is a time point that is difficult to define as it is dependent on clinical observation by individuals with disparate expertise in assessing jaundice. Entry criteria for the longitudinal cohort study by the Pediatric Acute Liver Failure Study Group were developed by a consensus of experts who served as the site principal investigators [1]. Those entry criteria are (1) children with no known evidence of chronic liver disease, (2) biochemical evidence of acute liver injury, and (3) coagulopathy not corrected by vitamin K. A previously healthy patient typically experiences a non-specific prodrome of variable duration with features that might include abdominal discomfort and malaise with or without fever. Symptoms may persist or wax and wane for days or weeks before the child is brought to medical attention. In the absence of jaundice or other clinically evident sign of liver dysfunction, the child may receive empiric Liver Disease in Children, Fourth Edition, ed. Improved assessment and estimate of the clinical trajectory will enhance transplant decisions in the future. The uncertainty regarding where the patient resides along the "natural course" of the disease at the time of initial presentation or at any point thereafter requires considerable clinical judgment. Given the insufficient number of organs to satisfy patient needs, the field would be well served if there were a more precise method to identify those patients who will survive without a liver transplant, as well as those who will die despite liver transplant. Patient outcome is reflected, in part, by the interaction among etiology, disease severity, supportive management, and treatment. Yet, outcomes vary among children with seemingly similar etiology, disease severity, and treatment; therefore, additional factors are likely involved to explain these variations. Modifying factors likely include the inflammatory milieu, end-organ damage, immune activation, potential for liver regeneration, and management interventions. Medical Etiology Specific etiologies can be broadly categorized as infectious, immunologic, metabolic, and toxin/drug related. It is available without prescription and is commercially available as a single formulation or can be compounded with decongestants or narcotics. Acetaminophen is safe and well tolerated when dosing instructions are strictly followed. However, it has a low therapeutic index, and in certain individuals or clinical scenarios, chronic administration of therapeutic dosages of acetaminophen can result in significant hepatotoxic effects [5,6]. The most common scenario follows an intentional single ingestion of a hepatotoxic dose that is >100 mg/kg. Plasma acetaminophen at 4 and 24 hours after a single ingestion will assist in determining the relative toxicity of the ingestion [7]. Females over 10 years of age represent the most common demographic associated with intentional overdose in children, but it should be considered in all age groups outside the newborn period [1]. Immediately following ingestion, patients may experience non-specific symptoms of nausea and vomiting. While a liver biopsy is not generally indicated in the setting of known acetaminophen overdose, centrilobular hepatic necrosis is the hallmark finding and should raise the consideration of acetaminophen toxicity even without a clear history of exposure. N-Acetylcysteine given enterally or intravenously can successfully reverse the toxic injury if given as soon after the ingestion as possible, ideally within 24 hours. If treatment is delayed beyond 24 hours following ingestion, the patient is at increased risk of having irreversible liver injury. Regardless of the interval between ingestion and presentation, N-acetylcysteine should be administered where a toxic ingestion occurred. If treatment is not initiated, jaundice develops within 48 to 72 hours, with death occurring in the most severe cases by 5 to 7 days following the ingestion. Therapeutic misadventures or unintentional exposure to a single hepatotoxic dose of acetaminophen or chronic exposure at daily doses of <100 mg/kg can also result in hepatotoxicity. Risk factors for developing severe hepatotoxicity include concomitant use of other medicines that alter hepatic metabolism, delayed medical care, younger age, and prolonged periods of fasting [5,8]. The presence of acetaminophen adducts in the serum may indicate unsuspected acetaminophen hepatotoxicity [9]. Similar to children with a single intentional overdose, alanine aminotransferase levels can reach into the many thousands with a relatively low total bilirubin level. The therapeutic benefit of N-acetylcysteine in patients with chronic acetaminophen exposure is untested and uncertain. The list of xenobiotics associated with liver failure is extensive and expanding, a partial list is found in Table 4. Hepatotoxic agents, such as industrial solvents and mushroom toxin, are dose dependent and will predictably result in liver injury or failure. The diagnosis of hepatotoxic liver injury is based upon the interval between drug ingestion and the onset of symptoms, the known hepatotoxicity of the offending agent, serum drug levels (if available), and liver biopsy findings [11]. The diagnosis of idiosyncratic drug-related liver failure is based upon largely circumstantial evidence, so a degree of skepticism should be maintained regarding the role of drug exposure in causing the hepatic injury [6,12]. In teenagers, a history should include evidence of depression, recreational drug use. Any exposure to hepatotoxic drugs, chemicals, or herbals should be considered possibly related to the liver injury.
The toxic metabolite can damage the cell itself or initiate various amplifying processes within the cell or external to the cell erectile dysfunction causes premature ejaculation cheapest generic tadora uk, such as immune response impotence yoga poses purchase 20mg tadora free shipping. Direct toxins typically injure the liver without metabolism, but in principle amplification pathways could also be involved. Reactive metabolites may alter other hepatocellular proteins to produce neoantigens. When toxic metabolites or reactive oxygen species or cytokines stimulate Kupffer cells, specific mechanisms of cell damage are set into motion involving tumor necrosis factor- or nitric oxide produced by Kupffer cells. Nitric oxide elaborated by Kupffer cells and hepatocytes plays a role in acetaminophen hepatotoxicity. Kupffer cells can activate natural killer cells and natural killer T-cells in the liver. Kupffer cells also elaborate various factors that are cytoprotective to hepatocytes [23]. For example, genetic polymorphisms affecting the extent of cytokine production may be relevant to diclofenac hepatotoxicity [24]. Some components of the innate immune system, such as interleukin-10 and certain prostaglandins, are hepatoprotective. Therefore, in addition to pharmacogenetics, immunogenetics must be considered to explain drug hepatotoxicity. Classification of chemicals that cause liver injury has to account for inevitable toxicity or for idiosyncrasy, whether from biochemical toxicity or an immune process, or some combination of the two (Table 22. Hepatotoxic agents can be categorized as follows: intrinsic, contingent, and as eliciting an immunoallergic response. The contingent hepatotoxin causes hepatotoxicity only when hepatic biotransformation is abnormal so that toxic metabolites are more likely to be generated or detoxification pathways are deficient. Hepatic biotransformation may be abnormal on an acquired or pharmacogenetic basis. This category encompasses the category denoted as "metabolic idiosyncrasy" by others. A hepatotoxin eliciting an immunoallergic response is identified when hepatotoxicity is accompanied by fever, eosinophilia, and atypical lymphocytosis or is characterized histologically by hepatic granulomatosis. If the biochemical mechanism of hepatic biotransformation is established for a given chemical, then it is possible to predict circumstances in which that chemical would function as a contingent hepatotoxin. Currently, it is often impossible to identify abnormal hepatic biotransformation owing to a pharmacogenetic defect until after drug-induced hepatotoxicity has occurred. For the affected individual, the hepatotoxicity appears to be a chance aberration. The clinical presentations and liver pathology of drug hepatotoxicity are extremely diverse. Selected drugs and environmental toxins illustrate this broad range of drug hepatotoxicity affecting adults or children (Table 22. Drugs selected for detailed commentary here include some already encountered in clinical practice and some which may prove important in the pediatric age bracket in the future. These symptoms subside and then there is an asymptomatic interval before liver injury becomes clinically apparent. At that point, jaundice, abnormal serum aminotransferases, and coagulopathy develop. Serum aminotransferases may be extremely high in this condition, and the degree of abnormality is not necessarily predictive of outcome. In a large retrospective series of children (mainly girls) with acetaminophen overdose, prothrombin time >100 seconds (international normalized ratio, >7), hypoglycemia (<2. Treatment of acute acetaminophen hepatotoxicity involves the use of what is effectively an antidote, N-acetylcysteine. N-Acetylcysteine is most effective if given within 10 hours of acetaminophen ingestion, and it may be of little benefit more than 24 hours after ingestion of the acetaminophen. Late administration of Nacetylcysteine has been associated with greater survival in adults with acute acetaminophen intoxication; no adverse side effects of the N-acetylcysteine were observed [29,30]. The dose of Nacetylcysteine must be appropriate for body weight because an inappropriately high dose may be toxic, causing respiratory compromise or hypotension. Other measures, such as charcoal, may be effective very early, that is, within 1 hour of ingestion; acetaminophen ingestion itself typically causes vomiting. Hemodialysis may be used early when plasma concentrations of acetaminophen are high: otherwise it is not effective. As the metabolism of acetaminophen in adolescents is similar to that of the adult, treatment should be aggressive; younger children also require N-acetylcysteine and supportive treatment, even when the timing and total amount of acetaminophen taken are uncertain. Liver transplantation may be required for those children in liver failure who show no improvement despite full supportive treatment. Recent experience suggests that the prognosis is good in a child if after 48 hours of treatment with N-acetylcysteine the prothrombin time and serum aminotransferases are all normal. In addition to this acute type of hepatotoxicity, which is encountered in toddlers invading the medicine cabinet or in suicidal teenagers, acetaminophen hepatotoxicity in children can present more subtly, as therapeutic misadventure. This occurs through various sorts of unintentional error: actual dosing error through misunderstanding the dose or using the wrong measuring device, substitution of one formulation for another, failure to appreciate how often acetaminophen turns up in various over-the-counter medications, and the general belief that acetaminophen is "safe" for children. In typical cases, rather large doses of acetaminophen (approximately 30ͷ0 mg/kg, less in small infants) are administered at regular intervals (usually every 2ʹ hours) for 2 to 3 days, or longer, before hepatotoxicity becomes evident. This is sometimes described as "chronic" overdose, but the actual time frame is comparatively short. The liver disease presents as acute liver failure, and the systemic signs of toxicity and the asymptomatic period do not occur. Diagnosis is difficult unless a very meticulous drug history is taken to determine exactly what preparation of acetaminophen was used and how often. Getting the actual drug containers, even if they were discarded, may be critically important. The acute liver failure is frequently attributed to another etiology, usually acute viral hepatitis. Since its first description in this chapter, numerous cases of this type of acetaminophen hepatotoxicity have been documented [32ͳ4]. The estimate of the lethal dose per kilogram body weight (140 mg/kg) is based on observations in adults and is probably not accurate for children in this scenario. A suggested threshold on the order of 90ͱ20 mg/kg daily with more than 1 day of drug administration is highly controversial because it impinges on the dose schedule of 15 mg/kg daily administered every 4 hours around the clock. Indeed some caution about this routine dose is appropriate: taking the "safe" dose of acetaminophen daily can cause asymptomatic elevations of alanine aminotransferase in adults [35] and for children a maximum total dose of 75 mg/kg daily is advised. The Rumack nomogram for treatment with N-acetylcysteine does not apply in the situation of an infant or young child with highdose chronic dosing. Importantly, finding a measurable serum concentration of acetaminophen 24 hours or more after the last dose should suggest the possibility of acetaminophen hepatotoxicity. The elimination half-life can be estimated from two drug levels obtained at a reasonable interval apart: if it is greater than 4 hours, it suggests hepatotoxicity. In general, it seems reasonable to treat these patients with N-acetylcysteine as soon as possible. Anorexia and food avoidance, which may have accompanied the underlying illness for which acetaminophen was used, may exacerbate the hepatotoxicity by causing acute depletion of glutathione stores. These children tend to present for medical assessment late in the disease course, and this may be an important reason for the poor prognosis. The primary mechanism for acetaminophen hepatotoxicity involves the formation of a toxic metabolite. The important role of drug metabolism in this hepatotoxicity is reflected in the predominance of hepatocellular injury in Rappaport zone 3. It is conjugated by glutathione, provided that sufficient glutathione is available, to form mercapturic acid, which is excreted in the urine. Intracellular processes amplifying cellular damage contribute to the liver injury, which may seem to be disproportionate to the amount of toxic metabolite produced. Apart from glutathione, other cytoprotective metabolic pathways dependent on diet may be important [40]. As part of an extracellular enhancement mechanism, various cytokines can increase or decrease the liver injury.
Order 20 mg tadora with mastercard. Erectile Dysfunction (नपुंसकता) Treatment In HIndi | Ayurvedic Viral.
References
- Sulaiman, M.N., Buchholz, N.P., Clark, P.B. The role of ureteral stent placement in the prevention of Steinstrasse. J Endourol 1999;13:151-155.
- McAdams S, Kim N, Dajusta D, et al: Preoperative stone attenuation value predicts success after shock wave lithotripsy in children, J Urol 184:1804, 2010.
- Mariano F, et al. Production of platelet-activating factor in patients with sepsis-associated acute renal failure. Nephrol Dial Transplant. 1999;14:1150-1157.
- Nahab F, Kass-Hout T, Shaltoni HM. Periprocedural antithrombotic strategies in acute ischemic stroke interventional therapy. Neurology 2012;79:S174-81.