John Paul Vavalle, MD
- Instructor of Medicine
- Duke University Medical Center
- Durham, North Carolina
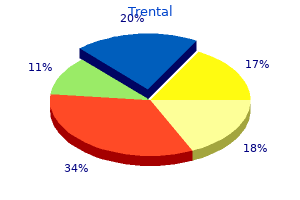
In particular arthritis reactive treatment generic trental 400 mg line, its use should be avoided in patients at higher risk of failure lupus arthritis in feet buy trental 400 mg line, including those with positive cultures at the end of the intensive treatment phase and those with evidence of cavitation on chest radiographs rheumatoid arthritis diet soda order trental 400 mg online. As a rule arthritis pain tylenol or advil cheap 400mg trental with visa, these mycobacterial species are less susceptible than M tuberculosis to antituberculous drugs arthritis medication for dogs metacam generic trental 400mg free shipping. Emergence of resistance during therapy is also a problem with these mycobacterial species, and active infection should be treated with combinations of drugs. M kansasii is susceptible to rifampin and ethambutol, partially susceptible to isoniazid, and completely resistant to pyrazinamide. A three-drug combination of isoniazid, rifampin, and ethambutol is the conventional treatment for M kansasii infection. Some authorities recommend use of a third agent, especially rifabutin, 300 mg once daily. Resistance can emerge in large populations of M leprae, eg, in lepromatous leprosy, particularly if low doses are given. Therefore, the combination of dapsone, rifampin, and clofazimine is recommended for initial therapy of lepromatous leprosy. A combination of dapsone plus rifampin is commonly used for leprosy with a lower organism burden. Because of increasing reports of dapsone resistance, treatment of leprosy with combinations of the drugs listed below is recommended. Sulfones are well absorbed from the gut and widely distributed throughout body fluids and tissues. Skin heavily infected with M leprae may contain several times more drug than normal skin. Many patients develop some hemolysis, particularly if they have glucose-6-phosphate dehydrogenase deficiency. During dapsone therapy of lepromatous leprosy, erythema nodosum leprosum often develops. It is sometimes difficult to distinguish reactions to dapsone from manifestations of the underlying illness. Absorption of clofazimine from the gut is variable, and a major portion of the drug is excreted in feces. Clofazimine is stored widely in reticuloendothelial tissues and skin, and its crystals can be seen inside phagocytic reticuloendothelial cells. It is slowly released from these deposits, so the serum half-life may be 2 months. This medication is no longer commercially available, but it can be obtained through established programs. Internationally, ministries of health can make requests directly to the World Health Organization. Curry International Tuberculosis Center and California Department of Public Health, 2016: Drug-Resistant Tuberculosis: A Survival Guide for Clinicians, Third Edition [1-305]. Hugonnet J-E et al: Meropenem-clavulanate is effective against extensively drugresistant Mycobacterium tuberculosis. Kinzig-Schippers M et al: Should we use N-acetyltransferase type 2 genotyping to personalize isoniazid doses Nahid P et al: Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: Treatment of Drug-Susceptible Tuberculosis. If dolutegravir is chosen, it must be administered twice daily due to the interaction with rifampin; alternatively, rifabutin can be used in place of rifampin, and dolutegravir can be dosed once daily. The patient is at increased risk of developing hepatotoxicity from both isoniazid and pyrazinamide given his history of alcohol use. Patient receives empiric therapy for bacterial meningitis with vancomycin and ceftriaxone, and is unimproved after 72 hours of treatment. The antifungal drugs presently available fall into the following categories: systemic drugs (oral or parenteral) for systemic infections, oral systemic drugs for mucocutaneous infections, and topical drugs for mucocutaneous infections. He was recently incarcerated near Bakersfield, California and returned to Oakland about 3 months ago. These changes have resulted in increased numbers of patients at risk for fungal infections. For many years, amphotericin B was the only efficacious antifungal drug available for systemic use. In the last several decades, pharmacotherapy of fungal disease has been revolutionized by the introduction of the relatively nontoxic azole drugs (both oral and parenteral formulations) and the echinocandins (only available for parenteral administration). The new agents in these classes offer more targeted, less toxic therapy than older agents such as amphotericin B for patients with serious systemic fungal infections. Combination therapy is being reconsidered, and new formulations of old agents are becoming available. Unfortunately, the appearance of azoleresistant and echinocandin-resistant organisms, as well as the rise in the number of patients at risk for mycotic infections, has created new challenges. Chemistry & Pharmacokinetics Amphotericin B is an amphoteric polyene macrolide (polyene = containing many double bonds; macrolide = containing a large lactone ring of 12 or more atoms). It is nearly insoluble in water and is therefore prepared as a colloidal suspension of amphotericin B and sodium deoxycholate for intravenous injection. Hepatic impairment, renal impairment, and dialysis have little impact on drug concentrations, and therefore no dose adjustment is required. Ergosterol, a cell membrane sterol, is found in the cell membrane of fungi, whereas the predominant sterol of bacteria and human cells is cholesterol. Oral amphotericin B is thus effective only on fungi within the lumen of the tract and cannot be used for treatment of systemic disease. Although it is mostly metabolized, some amphotericin B is excreted slowly Lipid Formulation of Amphotericin B Therapy with amphotericin B is often limited by toxicity, especially drug-induced renal impairment. This has led to the development of lipid drug formulations on the assumption that lipid-packaged drug binds to the mammalian membrane less readily, permitting the use of effective doses of the drug with lower toxicity. Liposomal amphotericin preparations package the active drug in lipid delivery vehicles, in contrast to the colloidal suspensions, which were previously the only available forms. Amphotericin binds to the lipids in these vehicles with an affinity between that for fungal ergosterol and that for human cholesterol. The lipid vehicle then serves as an amphotericin reservoir, reducing nonspecific binding to human cell membranes. This preferential binding allows for a reduction of toxicity without sacrificing efficacy and permits use of larger doses. Furthermore, some fungi contain lipases that may liberate free amphotericin B directly at the site of infection. Although clinical trials have demonstrated different renal and infusion-related toxicities for these preparations compared with regular amphotericin B, there are no trials comparing the different formulations with each other. Limited studies have suggested at best a moderate improvement in the clinical efficacy of the lipid formulations compared with conventional amphotericin B. Because the lipid preparations are much more expensive, their use is usually restricted to patients intolerant to , or not responding to , conventional amphotericin treatment. Except for flucytosine (and possibly griseofulvin, not shown), all currently available antifungals target the fungal cell membrane or cell wall. This amphipathic characteristic facilitates pore formation by multiple amphotericin molecules, with the lipophilic portions around the outside of the pore and the hydrophilic regions lining the inside. The pore allows the leakage of intracellular ions and macromolecules, eventually leading to cell death. Resistance to amphotericin B occurs if ergosterol binding is impaired, either by decreasing the membrane concentration of ergosterol or by modifying the sterol target molecule to reduce its affinity for the drug. Such induction therapy is especially important for immunosuppressed patients and those with severe fungal pneumonia, severe cryptococcal meningitis, or disseminated infections with one of the endemic mycoses such as histoplasmosis or coccidioidomycosis. Once a clinical response has been elicited, these patients then often continue maintenance therapy with an azole; therapy may be lifelong in patients at high risk for disease relapse. For treatment of systemic fungal disease, amphotericin B is given by slow intravenous infusion at a dosage of 0. Intrathecal therapy for fungal meningitis is poorly tolerated and fraught with difficulties related to maintaining cerebrospinal fluid access. Thus, intrathecal therapy with amphotericin B is being increasingly supplanted by other therapies but remains an option in cases of fungal central nervous system infections that have not responded to other agents. Mycotic corneal ulcers and keratitis can be cured with topical drops as well as by direct subconjunctival injection. Fungal arthritis has been treated with adjunctive local injection directly into the joint. Candiduria responds to bladder irrigation with amphotericin B, and this route has been shown to produce no significant systemic toxicity. Antifungal Activity & Clinical Uses Amphotericin B remains the antifungal agent with the broadest spectrum of action. It has activity against the clinically significant yeasts, including Candida albicans and Cryptococcus neoformans; the organisms causing endemic mycoses, including Histoplasma capsulatum, Blastomyces dermatitidis, and Coccidioides immitis; and the pathogenic molds, such as Aspergillus fumigatus and the agents of mucormycosis. Some fungal organisms such as Candida lusitaniae and Pseudallescheria boydii display intrinsic amphotericin B resistance. Owing to its broad spectrum of activity and fungicidal action, amphotericin B remains a useful agent for nearly all life-threatening mycotic infections, although newer, less toxic agents have largely replaced it for most conditions. Amphotericin B is often used as the initial induction regimen to rapidly reduce fungal burden and Adverse Effects the toxicity of amphotericin B can be divided into two broad categories: immediate reactions, related to the infusion of the drug, and those occurring more slowly. Infusion-Related Toxicity Infusion-related reactions are nearly universal and consist of fever, chills, muscle spasms, vomiting, headache, and hypotension. They can be ameliorated by slowing the infusion rate or decreasing the daily dose. Premedication with antipyretics, antihistamines, meperidine, or corticosteroids can be helpful. When starting therapy, many clinicians administer a test dose of 1 mg intravenously to gauge the severity of the reaction. This can serve as a guide to an initial dosing regimen and premedication strategy. Renal impairment occurs in nearly all patients treated with clinically significant doses of amphotericin. The degree of azotemia is variable and often stabilizes during therapy, but it can be serious enough to necessitate dialysis. A reversible component is associated with decreased renal perfusion and represents a form of prerenal renal failure. An irreversible component results from renal tubular injury and subsequent dysfunction. The irreversible form of amphotericin nephrotoxicity usually occurs in the setting of prolonged administration (>4 g cumulative dose). Renal toxicity commonly manifests as renal tubular acidosis and severe potassium and magnesium wasting. There is some evidence that the prerenal component can be attenuated with sodium loading, and it is common practice to administer normal saline infusions with the daily doses of amphotericin B. Abnormalities of liver function tests are occasionally seen, as is a varying degree of anemia due to reduced erythropoietin production by damaged renal tubular cells. After intrathecal therapy with amphotericin, seizures and a chemical arachnoiditis may develop, often with serious neurologic sequelae. Peak serum concentrations should be measured periodically in patients with renal insufficiency and maintained between 50 and 100 mcg/mL. Mechanisms of Action & Resistance Flucytosine is taken up by fungal cells via the enzyme cytosine permease. Human cells are unable to convert the parent drug to its active metabolites, resulting in selective toxicity. It may be related to enhanced penetration of the flucytosine through amphotericin-damaged fungal cell membranes. In vitro synergy with azole drugs also has been seen, although the mechanism is unclear. Resistance is thought to be mediated through altered metabolism of flucytosine, and, although uncommon in primary isolates, it develops rapidly in the course of flucytosine monotherapy. Clinical Uses & Adverse Effects the spectrum of activity of flucytosine is restricted to C neoformans, some Candida sp, and the dematiaceous molds that cause chromoblastomycosis. Flucytosine is rarely used as a single agent because of its demonstrated synergy with other agents and to avoid the development of secondary resistance. At present clinical use is confined to combination therapy with amphotericin B for cryptococcal meningitis, or with itraconazole for chromoblastomycosis. Flucytosine also has limited utility as monotherapy for fluconazole-resistant candidal urinary tract infections. The adverse effects of flucytosine result from metabolism (possibly by intestinal flora) to the toxic antineoplastic compound fluorouracil. Bone marrow toxicity with anemia, leukopenia, and thrombocytopenia are the most common adverse effects, with derangement of liver enzymes occurring less frequently. There seems to be a narrow therapeutic window, with an increased risk of toxicity at higher drug levels and resistance developing rapidly at subtherapeutic concentrations. The use of drug concentration measurements may be helpful in reducing the incidence of toxic reactions, especially when flucytosine is combined with nephrotoxic agents such as amphotericin B.
Its half-life in plasma is between 3 and 6 minutes rheumatoid arthritis news order trental with a mastercard, which is similar to that of insulin arthritis in neck from cracking purchase trental 400 mg online. The immediate pharmacological result of glucagon infusion is to raise blood glucose at the expense of stored hepatic glycogen rheumatoid arthritis va disability generic trental 400 mg overnight delivery. There is no effect on skeletal muscle glycogen rheumatoid arthritis treatment order 400 mg trental, presumably because of the lack of glucagon receptors on skeletal muscle arthritis causing numbness in feet buy trental paypal. Pharmacological amounts of glucagon cause release of insulin from normal pancreatic beta cells, catecholamines from pheochromocytoma, and calcitonin from medullary carcinoma cells. One of the precursor intermediates consists of a 69-amino-acid peptide called glicentin, which contains the glucagon sequence interposed between peptide extensions. Effect on liver: Reversal of catabolic features of insulin deficiency Inhibits glycogenolysis Inhibits conversion of fatty acids and amino acids to keto acids Inhibits conversion of amino acids to glucose Anabolic action Promotes glucose storage as glycogen (induces glucokinase and glycogen synthase, inhibits phosphorylase) Increases triglyceride synthesis and very-low-density lipoprotein formation Effect on muscle: Increased protein synthesis Increases amino acid transport Increases ribosomal protein synthesis Increased glycogen synthesis Increases glucose transport Induces glycogen synthase and inhibits phosphorylase Effect on adipose tissue: Increased triglyceride storage Lipoprotein lipase is induced and activated by insulin to hydrolyze triglycerides from lipoproteins Glucose transport into cell provides glycerol phosphate to permit esterification of fatty acids supplied by lipoprotein transport Intracellular lipase is inhibited by insulin administered as an intravenous bolus. Because insulin-treated patients develop circulating anti-insulin antibodies that interfere with radioimmunoassays of insulin, measurements of C-peptide are used to indicate beta-cell secretion. Radiology of the Bowel Glucagon has been used extensively in radiology as an aid to x-ray visualization of the bowel because of its ability to relax the intestine. Adverse Reactions Transient nausea and occasional vomiting can result from glucagon administration. These are generally mild, and glucagon is relatively free of severe adverse reactions. The disease states underlying the diagnosis of diabetes mellitus are now classified into four categories: type 1, type 2, other, and gestational diabetes mellitus. Thus, it produces an effect very similar to that of -adrenoceptor agonists without requiring functioning receptors. Effects on Smooth Muscle Large doses of glucagon produce profound relaxation of the intestine. In contrast to the above effects of the peptide, this action on the intestine may be due to mechanisms other than adenylyl cyclase activation. Type 1 Diabetes Mellitus the hallmark of type 1 diabetes is selective beta cell (B cell) destruction and severe or absolute insulin deficiency. Type 1 diabetes is further subdivided into immune-mediated (type 1a) and idiopathic causes (type 1b). Although most patients are younger than 30 years of age at the time of diagnosis, the onset can occur at any age. Type 1 diabetes is found in all ethnic groups, but the highest incidence is in people from northern Europe and from Sardinia. These antibodies facilitate the diagnosis of type 1a diabetes and can also be used to screen family members at risk for developing the disease. Most type 1 patients with acute symptomatic presentation have significant beta cell loss and insulin therapy is essential to control glucose levels and to prevent ketosis. Some patients have a more indolent autoimmune process and initially retain enough beta cell function to avoid ketosis. Severe Hypoglycemia the major clinical use of glucagon is for emergency treatment of severe hypoglycemic reactions in patients with type 1 diabetes when unconsciousness precludes oral feedings and intravenous glucose treatment is not possible. On the morning of the test, adults are then given 75 g of glucose in 300 mL of water; children are given 1. Blood samples for plasma glucose are obtained at 0 and 120 minutes after ingestion of glucose. An oral glucose tolerance test is normal if the fasting venous plasma glucose value is less than 100 mg/dL (5. A fasting value of 126 mg/dL (7 mmol/L) or higher or a 2-hour value of greater than 200 mg/dL (11. The HbA1c fraction is abnormally elevated in people with diabetes with chronic hyperglycemia. In patients who monitor their glucose levels, the HbA1c value provides a valuable check on the accuracy of their monitoring. In patients who do not monitor their glucose levels, HbA1c measurements are essential for adjusting treatment. HbA1c can be used to Type 2 Diabetes Mellitus Type 2 diabetes is a heterogenous group of conditions characterized by tissue resistance to the action of insulin combined with a relative deficiency in insulin secretion. A given individual may have more resistance or more beta-cell deficiency, and the abnormalities may be mild or severe. Although the circulating endogenous insulin is sufficient to prevent ketoacidosis, it is inadequate to prevent hyperglycemia. Patients with type 2 diabetes can initially be controlled with diet, exercise and oral glucose lowering agents or non-insulin injectables. Some patients have progressive beta cell failure and eventually may also need insulin therapy. Other Specific Types of Diabetes Mellitus the "other" designation refers to multiple other specific causes of an elevated blood glucose: pancreatectomy, pancreatitis, nonpancreatic diseases, drug therapy, etc. For a detailed list the reader is referred to the reference Expert Committee, 2003. Gestational diabetes is diagnosed in approximately 7% of all pregnancies in the United States. During pregnancy, the placenta and placental hormones create an insulin resistance that is most pronounced in the last trimester. Screening may be deferred in lower-risk women until the 24th to 28th week of gestation. Fasting plasma glucose mg/dL (mmol/L) Two hours after glucose load mg/dL (mmol/L) 1 Normal Glucose Tolerance, mg/dL (mMol/L) <100 (5. Urine or Blood Ketones Qualitative detection of ketone bodies can be accomplished by nitroprusside tests (Acetest or Ketostix). Although these tests do not detect beta-hydroxybutyric acid, which lacks a ketone group, the semiquantitative estimation of ketonuria thus obtained is nonetheless usually adequate for clinical purposes. Many laboratories now measure beta-hydroxybutyric acid, and meters are available (Precision Xtra; Nova Max Plus) for patient use that measure beta-hydroxybutyric acid levels in capillary glucose samples. Self-Monitoring of Blood Glucose Capillary blood glucose measurements performed by patients themselves, as outpatients, are extremely useful. In type 1 patients in whom "tight" metabolic control is attempted, they are indispensable. Several paper strip methods and a large number of blood glucose meters are now available for measuring glucose on capillary blood samples. Studies show that adult type 1 patients who use continuous systems have improved glucose control without an increased incidence of hypoglycemia. There is great interest in using continuous glucose monitoring systems to automatically deliver insulin by continuous subcutaneous insulin infusion pump. With this system, the continuous glucose monitor readings are used to automatically adjust the basal insulin dosing by the insulin pump. Three of the analogs are rapidly acting: insulin lispro, insulin aspart, and insulin glulisine; and three are long acting: insulin glargine, insulin detemir, and insulin degludec. Pork and beef preparations (isophane, neutral, 30/70, and lente) are still available in other parts of the world. The insulin molecules exist as dimers that assemble into hexamers in the presence of two zinc ions. The hexamers are further stabilized by phenolic compounds such as phenol and meta-Cresol. The mutations engineered into the rapidly acting insulin analogs are designed to disrupt the stabilizing intermolecular interactions of the dimers and hexamers, leading to more rapid absorption into the circulation after subcutaneous injection. For very insulin-resistant subjects who would otherwise require large volumes of insulin solution, a U500 preparation of human regular insulin is available both in a vial form and a disposable pen. If the vial form is used, it is necessary to use a U100-insulin syringe or tuberculin syringe to measure doses. Species Source Human analog Human analog Human analog Human Human Human Human analog Human analog Human analog Human Human analog Human analog Human analog Human analog Concentration U100, U200 U100 U100 U100, U500 - U100 U100, U300 U100 U100, U200 U100 U100 U100 U100 U100 All insulins are now made by recombinant technology; they should be refrigerated and brought to room temperature just before injection. The physician should then carefully note dosages in both units and volume to avoid overdosage. The disposable pen avoids this conversion issue and dispenses the regular U500 insulin in 5-unit increments. Intravenous infusions of regular insulin are particularly useful in the treatment of diabetic ketoacidosis and during the perioperative management of insulin-requiring diabetics. Rapidly acting insulin analogs-Insulin lispro (Humalog) is an insulin analog in which the proline at position B28 is reversed with the lysine at B29. Insulin aspart (Novolog) is a single substitution of proline by aspartic acid at position B28. Insulin glulisine (Apidra) differs from human insulin in that the amino acid asparagine at position B3 is replaced by lysine and the lysine in position B29 by glutamic acid. When injected subcutaneously, these three analogs quickly dissociate into monomers and are absorbed very rapidly, reaching peak serum values in as little as 1 hour. The amino acid changes in these analogs do not interfere with their binding to the insulin receptor, with the circulating half-life, or with their immunogenicity, which are all identical to those of human regular insulin. Clinical trials have demonstrated that the optimal times of preprandial subcutaneous injection of comparable doses of the rapid-acting insulin analogs and of regular human insulin are 15 minutes and 45 minutes before the meal, respectively. Although the more rapid onset of action has been welcomed as a great convenience by patients with diabetes who object to waiting as long as 45 minutes after injecting regular human insulin before they can begin their meal, patients must be taught to ingest adequate absorbable carbohydrate early in the meal to avoid hypoglycemia during the meal. Another desirable feature of rapidly acting insulin analogs is that their duration of action remains at about 4 hours for most commonly used dosages. This contrasts with regular insulin, whose duration of action is significantly prolonged when larger doses are used. In a double-blind crossover study comparing insulin lispro with regular insulin in insulin pumps, persons using insulin lispro had lower HbA1c values and improved postprandial glucose control with the same frequency of hypoglycemia. However, the concern remains that in the event of pump failure, users of the rapidly acting insulin analogs will have more rapid onset of hyperglycemia and ketosis. While insulin aspart has been approved for intravenous use (eg, in hyperglycemic emergencies), there is no advantage in using insulin aspart over regular insulin by this route. After subcutaneous injection, proteolytic tissue enzymes degrade the protamine to permit absorption of insulin. The dose regulates the action profile; specifically, small doses have lower, earlier peaks and a short duration of action with the converse true for large doses. Insulin glargine-Insulin glargine is a soluble, "peakless" (ie, having a broad plasma concentration plateau), long-acting insulin analog. The attachment of two arginine molecules to the B-chain carboxyl terminal and substitution of a glycine for asparagine at the A21 position created an analog that is soluble in an acidic solution but precipitates in the more neutral body pH after subcutaneous injection. Individual insulin molecules slowly dissolve away from the crystalline depot and provide a low, continuous level of circulating insulin. Glargine is usually given once daily, although some very insulin-sensitive or insulin-resistant individuals benefit from split (twice a day) dosing. Separate syringes must be used to minimize the risk of contamination and subsequent loss of efficacy. The absorption pattern of insulin glargine appears to be independent of the anatomic site of injection, and this drug is associated with less immunogenicity than human insulin in animal studies. Insulin detemir-In this insulin the terminal threonine is dropped from the B30 position and myristic acid (a C-14 fatty acid chain) is attached to the B29 lysine. These modifications prolong the availability of the injected analog by increasing both self-aggregation in subcutaneous tissue and reversible albumin binding. The duration of action for insulin detemir is about 17 hours at therapeutically relevant doses. It is recommended that the insulin be injected once or twice a day to achieve a stable basal coverage. Insulin Degludec-In this insulin analog, the threonine at position B30 has been removed and the lysine at position B29 is conjugated to hexadecanoic acid via a gamma-l-glutamyl spacer. In the vial, in the presence of phenol and zinc, the insulin is in the form of dihexamers but, when injected subcutaneously, it self-associates into large multihexameric chains consisting of thousands of dihexamers. The chains slowly dissolve in the subcutaneous tissue, and insulin monomers are steadily released into the systemic circulation. Insulin degludec is available in two concentrations, U100 and U200, and dispensed in pre-filled disposable pens. For convenience, these are often mixed together in the same syringe before injection. Consequently, over time, the soluble component becomes a mixture of regular and rapidly acting insulin analog at varying ratios.
The en passage vessels should be preserved to avoid postoperative ischemic neurologic deficits can arthritis in neck cause headaches cheap trental 400 mg otc. These vessels have a thin tunica media resulting in a limited presence of smooth muscle and elastic lamina arthritis in elderly dogs order 400 mg trental visa. The best strategy for disconnection of the deep parenchymal feeders involves removal of a small volume of white matter immediately surrounding the perforator to expose a more proximal segment of the vessel with relatively normal walls rheumatoid arthritis diet milk trental 400 mg without a prescription. The surgeon should attempt to incorporate the native sulci and fissures into the initial circumdissection to minimize cortical gyrus transgression rheumatoid arthritis fingers buy cheap trental 400mg on line. During the descent to reach the apex of the nidus arthritis in dogs knees order 400mg trental mastercard, the surgeon should always ensure the preservation of a wide surgical field. If hemorrhage is encountered in a suboptimally exposed surgical field during deep circumdissection, achieving hemostasis can be very challenging. Compared to the superficial cortical feeding arteries, these vessels demonstrate a smaller caliber and a less robust tunica media within the vascular wall. This histological difference results in less vasoconstriction in response to a bipolar current and subsequently these vessels can demonstrate persistent hemorrhage and retraction within the parenchyma. The left lower image illustrates the appropriate technique for coagulation of the parenchymal perforators, which first involves removal of a small volume of parenchyma adjacent to the vessel. The proximal segment of the vessel demonstrates a more native histology and therefore is more amendable to coagulation techniques, either bipolar coagulation or clip ligation. The nidus should be localized and the dissection plane should be maintained outside its margins. Any transgression of the nidus should be strictly avoided during the descent to the apex. Any coagulation of the nidus before its complete disconnection should be avoided because of the risk for hemorrhage. If a breach in the nidus wall is encountered as a result of transgressing the parenchyma too near the nidus lobules during deep circumdissection, the surgeon can place a small piece of thrombin-soaked cotton over the defect in the nidus. Aggressive coagulation of the nidus in the setting of a breach should be avoided because of the resulting alteration in luminal hemodynamics that precipitates nidus rupture and secondary cerebral edema. The draining veins that wrap around the deeper sections of the nidus should also be protected. Step 5: Protecting the Dominant Draining Vein(s) Disconnecting the main draining vein(s) should be the last step of the operation, prior to removal of the nidus. These veins should be protected until all feeding arteries are disconnected from the nidus, at which point the veins become darker. The fissures and sulci within the superficial surface of the brain should be used to minimize parenchymal transgression and facilitate dissection planes. In an attempt to avoid recurrence the excision bed should be examined for any remaining segments of the nidus and to achieve sufficient hemostasis. An en passage vessel along the right margin of the bed was preserved and can be visualized. In such a setting, a "commando" operation is necessary requiring the surgeon to remain calm, decisive, and in control. If additional exposure is necessary when searching for residual arterial feeders, the primary draining vein can be mobilized to expose underlying arterial feeders or for nidus manipulation. These veins should be angiographically distinguished preoperatively based on the caliber of the vein and velocity of flow, such that the primary vein has the greatest diameter and capacitates the largest flow. This optional step often permits enhanced mobility of the nidus, which may be necessary to access occult feeding arteries. At this stage of the operation, a timely excision is the best method to control hemorrhage. At this depth, the nidus can be disconnected from the ependymal and choroid plexus vessels. When attempting disconnection of choroidal arteries or ependymal vessels, bipolar electrocautery is generally sufficient because of a robust tunica media. However, disconnection this deep in the parenchyma can pose challenges regarding sufficient exposure of the vessel. In these settings, microclips can be applied to disconnect the vessel prior to its coagulation. The surgeon must be vigilant for retraction of the choroidal or ependymal feeding artery during attempted coagulation, because, if these vessels are not sufficiently coagulated, occult intraventricular hemorrhage and herniation syndromes can result. Therefore, unexpected brain herniation at this step of the operation should alert the operator to examine the ventricle to evacuate the blood and deal meticulously with the bleeding ependymal feeding vessels. This step is particularly important for pediatric patients, which may have ependymal or plexal contribution to the nidus and have an increased the risk for recurrence. In an attempt to preserve the integrity of the draining vein, the feeding vessel may remain unnoticed and prevent the fundamental sign of blue discoloration of the vein. In this setting, the surgeon should attempt to localize and disconnect an occult feeding artery in close proximity of the vein. Following nidus excision, complete obliteration of arteriovenous shunting within the cerebrovasculature should be verified with intraoperative angiography. Residual regions of hyperperfusion directed outwardly from the nidus excision bed can be representative of minor arteriovenous shunting. Instead, the surgeon should observe these with regular follow-up imaging, particularly in pediatric patients, who are prone to recurrence and demand surveillance follow-up. Instead, the surgeon should utilize multiple rounds of irrigation and meticulously observe for hemostasis. This can be a challenging step but patience is an essential component to achieving hemostasis along the nidus bed. This approach was devised from a culmination of techniques described by master surgeons8,9,19,20 and personal expertise. The increased incorporation of less invasive treatment modalities, such as stereotactic radiosurgery and endovascular embolization, will also impact the prevalence of microsurgically appropriate cases. The identity of the cortically visualized vessel (blue arrow) remains unknown and is therefore not disconnected. A generous osteotomy above the orbital roof facilitated an optimal operative trajectory (Row 3). The nidus was skeletonized and revealed a prominent feeding artery (red arrow) adjacent to a primary draining vein (purple arrow) (Row 4). The primary draining vein was liberated from its surrounding tissue to permit mobilization and deeper access to the nidus. The deep parenchymal feeding arteries are identified and appropriately disconnected (Row 5). Management of perisylvian arteriovenous malformations: a retrospective institutional case series and review of the literature. Multimodality treatment of brain arteriovenous malformations with microsurgery after embolization with onyx: single-center experience and technical nuances. Stereotactic radiosurgery of cranial arteriovenous malformations and dural arteriovenous fistulas. Historical perspective of treatments of cranial arteriovenous malformations and dural arteriovenous fistulas. Microsurgery for cerebral arteriovenous malformations: postoperative outcomes and predictors of complications in 264 cases. Complete obliteration of intracranial arteriovenous malformation with endovascular cyanoacrylate embolization: initial success and rate of permanent cure. Intraoperative arteriovenous malformation rupture: causes, management techniques, outcomes, and the effect of neurosurgeon experience. Endovascular and microsurgical treatment of cerebral arteriovenous malformations: Current recommendations. Surgical treatment of cranial arteriovenous malformations and dural arteriovenous fistulas. Once resection is thought to be complete, postoperative angiography is needed to make sure all early venous drainage has been eliminated. A successful outcome is also dependent on attentive care in the intensive care unit during the first few days postresection. Keywords: cerebral arteriovenous malformation, surgical technique, complication avoidance, microsurgery, endovascular embolization 14. In this chapter, we will discuss nuances of patient selection, positioning, exposure, and microsurgical technique. Management of the patients before, during, and after surgery will also be reviewed. The key to achieving this goal is in careful patient selection (in particular for the unruptured population). It can be helpful to categorize the process into three parts: (1) patient factors such as patient age, comorbidities, expectations, and concerns. It assigns the patient a score based on several factors found to be significant predictors of outcome following surgical treatment. Scores > 6 were associated with a 55% chance of an adverse surgical outcome or death. Key Points With proper patient selection and good microsurgical dissection, a significant number of lobar arteriovenous malformations can be treated with a risk much lower than their untreated natural history. Excellent preoperative evaluation including a thorough neurological examination, detailed anatomic and functional imaging, and judicious use of preoperative embolization are important in achieving the best possible outcomes. Proper patient positioning, selection of the appropriate surgical approach, and meticulous intraoperative dissection will maximize technical success. The decision about positioning is usually straightforward with the head turned in such a way that lesion is in the most superior part of the exposure. Lesions on the orbital surface generally warrant a lateral exposure if they are far from the midline, allowing for a lateral subfrontal view. Orbital surface lesions with a more medial presentation are usually best accessed from the anterior subfrontal view, making a head neutral with significant extension the position of choice. Lesions of the frontal lobe presenting to the interhemispheric fissure present several reasonable choices for positioning. One is a head neutral position with an interhemispheric approach and gentle retraction of the frontal lobe ipsilateral to the lesion from medial to lateral. This works well, particularly if the lesion is relatively superficial in the interhemispheric fissure. Another clever approach to a lesion presenting to the interhemispheric fissure is to place the patient lateral with the lesion side down. In this position, gravity naturally pulls the lesion-side brain down, giving a more natural medial-to-lateral retraction of the brain. Depending on how anterior and medially they present, they also have feeding from the anterior temporal artery and the anterior choroidal artery. Lesions that are more posterior can also recruit posterior cerebral artery feeding. It is important to keep this vasculature in mind when deciding what position to use. A true lateral position or supine with the head rotated the appropriate amount usually works well for this approach. First, it is best if the lesion is in the center of the brain exposed by the bone flap. Next, the position must facilitate access to the proximal feeding vessels and allow visualization of the draining veins. The veins, which in general cannot be sacrificed until the majority or all of the arterial input has been taken, can tether the mass of the nidus. Finally, the patient must be positioned in such a way that the surgeon is reasonably comfortable during the procedure. Long surgeries with the surgeon in some contorted position make for a long, painful day and lead to rushing and careless mistakes. Lesions with more anterior extension can be positioned supine with the head turned. For progressively more posterior lesions, it may be more comfortable to have the patient either in a semi-sitting position or prone. In the superficial frontal lobe, especially in the superior, middle, and inferior frontal gyrus, arterial supply is from anterior Dumont et al. Sitting and semi-sitting have the advantage of allowing pooled blood to run off during surgery, facilitating visualization and maximizing the effectiveness of the bipolar. The disadvantage is the added time it takes to position properly and the added risk of hypotension and air embolism. More posterior lesions are exposed via a horseshoe-shaped flap with the lesion in the center. Lesions that present to the interhemispheric fissure can be exposed via a bicoronal incision. First, care must be used in placing the cranial fixation device such as the Mayfield head holder. Either the pins can get in the way of the exposure or they can be placed too far from the equator of the head allowing the head to slip. Even if the head holder shifts subtly during the case, the resulting movement can make the skin closure difficult. Occasionally, someone may have to crawl under the blood drapes to remove the fixed head holder and switch to a horseshoe-type holder in order to complete the closure. When dissection within the interhemispheric fissure is needed, the sagittal sinus must be exposed. There are many options for this but the safest alternative is to place multiple burr holes on either side of the sinus, strip the dura of the sinus away from the bone flap, and then carefully complete the cutting of the bone immediately over the sinus. Fortunately, the dura of the sinus is very thick; unfortunately, the sinus can be arterialized and the normally easily controlled transosseous venous bleeding can be arterialized and difficult to control. Working under the bone edge, especially if there is any problem in controlling intraoperative bleeding, can lead to serious problems. The transosseous venous channels can be a source of important bleeding while turning the craniotomy as they can be arterialized.
When this occurs or when migraine has its onset during therapy with these agents arthritis pain food triggers buy trental 400mg online, treatment should be discontinued types of arthritis in feet generic 400 mg trental with amex. Withdrawal bleeding sometimes fails to occur-most often with combination preparations-and may cause confusion with regard to pregnancy arthritis definition deutsch discount 400mg trental visa. If this is disturbing to the patient arthritis glucosamine purchase trental 400 mg amex, a different preparation may be tried or other methods of contraception used rheumatoid arthritis factor normal range buy discount trental 400mg. Moderate Adverse Effects Any of the following may require discontinuance of oral contraceptives: 1. Breakthrough bleeding is the most common problem in using progestational agents alone for contraception. It is more frequently encountered in patients taking low-dose preparations than in those taking combination pills with higher levels of progestin and estrogen. Weight gain is more common with the combination agents containing androgen-like progestins. It can usually be controlled by shifting to preparations with less progestin effect or by dieting. It tends to increase with time, the incidence being about 5% at the end of the first year and about 40% after 8 years. It is often reversible upon discontinuance of medication but may disappear very slowly. Hirsutism may also be aggravated by the "19-nortestosterone" derivatives, and combinations containing nonandrogenic progestins are preferred in these patients. Clinical Uses the most important use of combined estrogens and progestins is for oral contraception. In general, they are very effective; when these agents are taken according to directions, the risk of conception is extremely small. When severe dysmenorrhea is the major symptom, the suppression of ovulation with estrogen alone may be followed by painless periods. The long-term administration of large doses of progestins or combinations of progestins and estrogens prevents the periodic breakdown of the endometrial tissue and in some cases will lead to endometrial fibrosis and prevent the reactivation of implants for prolonged periods. As is true with most hormonal preparations, many of the undesired effects are physiologic or pharmacologic actions that are objectionable only because they are not pertinent to the situation for which they are being used. Therefore, the product containing the smallest effective amounts of hormones should be selected for use. Adverse Effects the incidence of serious known toxicities associated with the use of these drugs is low-far lower than the risks associated with pregnancy. Ureteral dilation similar to that observed in pregnancy has been reported, and bacteriuria is more frequent. Vaginal infections are more common and more difficult to treat in patients who are using oral contraceptives. Following cessation of administration of oral contraceptives, 95% of patients with normal menstrual histories resume normal periods and all but a few resume normal cycles during the next few months. Patients who have had menstrual irregularities before taking oral contraceptives are particularly susceptible to prolonged amenorrhea when the agents are discontinued. Prolactin levels should be measured in these patients, since many have prolactinomas. Vascular disorders-Thromboembolism was one of the earliest of the serious unanticipated effects to be reported and has been the most thoroughly studied. Venous thromboembolic disease-Superficial or deep thromboembolic disease in women not taking oral contraceptives occurs in about 1 patient per 1000 woman years. The overall incidence of these disorders in patients taking low-dose oral contraceptives is about threefold higher. The risk for this disorder is increased during the first month of contraceptive use and remains constant for several years or more. The incidence of these disorders is too low for cost-effective screening by current methods, but prior episodes or a family history may be helpful in identifying patients with increased risk. The incidence of venous thromboembolism appears to be related to the estrogen but not the progestin content of oral contraceptives and is not related to age, parity, mild obesity, or cigarette smoking. Decreased venous blood flow, endothelial proliferation in veins and arteries, and increased coagulability of blood resulting from changes in platelet functions and fibrinolytic systems contribute to the increased incidence of thrombosis. This change occurs in the first month of treatment and lasts as long as treatment persists, reversing within a month thereafter. Myocardial infarction-The use of oral contraceptives is associated with a slightly higher risk of myocardial infarction in women who are obese, have a history of preeclampsia or hypertension, or have hyperlipoproteinemia or diabetes. In addition, facilitation of coronary arterial spasm may play a role in some of these patients. Recent studies suggest that risk of infarction is not increased in past users who have discontinued oral contraceptives. However, subarachnoid hemorrhages have been found to be increased among both current and past users and may increase with time. The risk of thrombotic or hemorrhagic stroke attributable to oral contraceptives (based on older, higher-dose preparations) has been estimated at about 37 cases per 100,000 users per year. In summary, available data indicate that oral contraceptives increase the risk of various cardiovascular disorders at all ages and among both smokers and nonsmokers. However, this risk appears to be concentrated in women 35 years of age or older who are heavy smokers. It is clear that these risk factors must be considered in each individual patient for whom oral contraceptives are being considered. Some experts have suggested that screening for coagulopathy should be performed before starting oral contraception. Gastrointestinal disorders-Many cases of cholestatic jaundice have been reported in patients taking progestin-containing drugs. The differences in incidence of these disorders from one population to another suggest that genetic factors may be involved. The jaundice caused by these agents is similar to that produced by other 17-alkyl-substituted steroids. It is most often observed in the first three cycles and is particularly common in women with a history of cholestatic jaundice during pregnancy. These agents have also been found to increase the incidence of symptomatic gallbladder disease, including cholecystitis and cholangitis. This is probably the result of the alterations responsible for jaundice and bile acid changes described above. It also appears that the incidence of hepatic adenomas is increased in women taking oral contraceptives. Ischemic bowel disease secondary to thrombosis of the celiac and superior and inferior mesenteric arteries and veins has also been reported in women using these drugs. Depression-Depression of sufficient degree to require cessation of therapy occurs in about 6% of patients treated with some preparations. Cancer-The occurrence of malignant tumors in patients taking oral contraceptives has been studied extensively. It is now clear that these compounds reduce the risk of endometrial and ovarian cancer. Some studies have shown an increased risk in younger women, and it is possible that tumors that develop in younger women become clinically apparent sooner. The relation of risk of cervical cancer to oral contraceptive use is still controversial. It should be noted that a number of recent studies associate the use of oral contraceptives by women who are infected with human papillomavirus with an increased risk of cervical cancer. Other-In addition to the above effects, a number of other adverse reactions have been reported for which a causal relation has not been established. These include alopecia, erythema multiforme, erythema nodosum, and other skin disorders. Contraindications & Cautions these drugs are contraindicated in patients with thrombophlebitis, thromboembolic phenomena, and cardiovascular and cerebrovascular disorders or a past history of these conditions. They should be avoided in patients with known or suspected tumors of the breast or other estrogen-dependent neoplasms. Since these preparations have caused aggravation of preexisting disorders, they should be avoided or used with caution in patients with liver disease, asthma, eczema, migraine, diabetes, hypertension, optic neuritis, retrobulbar neuritis, or convulsive disorders. The oral contraceptives may produce edema, and for that reason they should be used with great caution in patients in heart failure or in whom edema is otherwise undesirable or dangerous. Therefore, for women with these tumors, agents with the smallest amounts of estrogen and the most androgenic progestins should be selected. The use of progestational agents alone for contraception might be especially useful in such patients (see below). These agents are contraindicated in adolescents in whom epiphyseal closure has not yet been completed. Women using oral contraceptives must be made aware of an important interaction that occurs with antimicrobial drugs. Because the normal gastrointestinal flora increase the enterohepatic cycling (and bioavailability) of estrogens, antimicrobial drugs that interfere with these organisms may reduce the efficacy of oral contraceptives. Additionally, coadministration with potent inducers of the hepatic microsomal metabolizing enzymes, such as rifampin, may increase liver catabolism of estrogens or progestins and diminish the efficacy of oral contraceptives. Almost all users experience episodes of unpredictable spotting and bleeding, particularly during the first year of use. This preparation is not desirable for women planning a pregnancy soon after cessation of therapy because ovulation suppression can sometimes persist for as long as 18 months after the last injection. Suppression of endogenous estrogen secretion may be associated with a reversible reduction in bone density, and changes in plasma lipids are associated with an increased risk of atherosclerosis. The progestin implant method utilizes the subcutaneous implantation of capsules containing etonogestrel. The low levels of hormone have little effect on lipoprotein and carbohydrate metabolism or blood pressure. The disadvantages include the need for surgical insertion and removal of capsules and some irregular bleeding rather than predictable menses. An association of intracranial hypertension with an earlier type of implant utilizing norgestrel was observed in a small number of women. Patients experiencing headache or visual disturbances should be checked for papilledema. Contraception with progestins is useful in patients with hepatic disease, hypertension, psychosis or mental retardation, or prior thromboembolism. Postcoital Contraceptives Pregnancy can be prevented following coitus by the administration of estrogens alone, progestin alone, or in combination ("morning after" contraception). The hormones are often administered with antiemetics, since 40% of patients have nausea or vomiting. Other adverse effects include headache, dizziness, breast tenderness, and abdominal and leg cramps. Considerable controversy has accompanied the proposal to make these agents available without a prescription in the United States. They are particularly suited for use in patients for whom estrogen administration is undesirable. Beneficial Effects of Oral Contraceptives It has become apparent that reduction in the dose of the constituents of oral contraceptives has markedly reduced mild and severe adverse effects, providing a relatively safe and convenient method of contraception for many young women. Treatment with oral contraceptives has also been shown to be associated with many benefits unrelated to contraception. These include a reduced risk of ovarian cysts, ovarian and endometrial cancer, and benign breast disease. Iron deficiency and rheumatoid arthritis are less common, and premenstrual symptoms, dysmenorrhea, endometriosis, acne, and hirsutism may be ameliorated with their use. Studies of patients treated with tamoxifen as adjuvant therapy for early breast cancer have shown a 35% decrease in contralateral breast cancer. However, adjuvant therapy extended beyond 5 years in patients with breast cancer has shown no further improvement in outcome. In fact, resistant lines of tumor cells may recognize tamoxifen as an agonist rather than an antagonist, perhaps due to changes in the coregulators that interact with the estrogen receptor. Toremifene is a structurally similar compound with very similar properties, indications, and toxicities. The mechanism of its mixed agonist/antagonist relations to the estrogen receptor has been intensively studied but is still not completely understood. Tamoxifen is extensively used in the palliative treatment of breast cancer in postmenopausal women and is approved for chemoprevention of breast cancer in high-risk women (see Chapter 54). Therefore, strong inhibitors of 2D6 should be avoided in patients receiving tamoxifen.
Either radioactive iodine or thyroidectomy are reasonable and effective strategies for definitive treatment of her hyperthyroidism arthritis usa buy cheap trental 400mg online, especially before becoming pregnant to avoid an acute hyperthyroid exacerbation during pregnancy or following delivery rheumatoid arthritis definition of remission trental 400mg with amex. Her hypothyroid symptoms should have been easily corrected by the addition of levothyroxine dosed correctly at 1 does arthritis in the knee cause swelling purchase trental 400 mg with amex. Because she is young and has no cardiac disease arthritis pain in your hands trental 400 mg for sale, full replacement doses were appropriate to start arthritis relief using gelatin discount trental 400mg with mastercard. For optimal absorption, levothyroxine should be taken orally 60 minutes before meals on an empty stomach or at bedtime, and separated by 4 hours from her calcium administration. Once weekly thyroxine injections may be effective in those with ongoing nonadherence. The examining physician discovers postural hypotension and moderate vitiligo (depigmented areas of skin) and obtains routine blood tests. The natural adrenocortical hormones are steroid molecules produced and released by the adrenal cortex. Both natural and synthetic corticosteroids are used for the diagnosis and treatment of disorders of adrenal function. They are also used-more often and in much larger doses-for treatment of a variety of inflammatory and immunologic disorders. Secretion of the salt-retaining hormone aldosterone is primarily under the influence of circulating angiotensin and potassium. Corticotropin has some actions that do not depend on its effect on adrenocortical secretion. However, its pharmacologic value as an anti-inflammatory agent and its use in testing adrenal function depend on its secretory action. Inhibitors of the synthesis or antagonists of the action of the adrenocortical steroids are important in the treatment of several conditions. Some have minimal biologic activity and function primarily as precursors, and there are some for which no function has been established. The hormonal steroids may be classified as those having important effects on intermediary metabolism and immune function (glucocorticoids), those having principally salt-retaining activity (mineralocorticoids), and those having androgenic or estrogenic activity (see Chapter 40). In humans, the major glucocorticoid is cortisol and the most important mineralocorticoid is aldosterone. Adrenal androgens constitute the major endogenous precursors of estrogen in women after menopause and in younger patients in whom ovarian function is deficient or absent. Pregnenolone is the major precursor of corticosterone and aldosterone, and 17-hydroxypregnenolone is the major precursor of cortisol. The enzymes and cofactors for the reactions progressing down each column are shown on the left and across columns at the top of the figure. When a particular enzyme is deficient, hormone production is blocked at the points indicated by the shaded bars. Its synthesis and secretion are tightly regulated by the central nervous system, which is very sensitive to negative feedback by the circulating cortisol and exogenous (synthetic) glucocorticoids. The sensitivity of tissues to glucocorticoids is also circadian but inverse to that of cortisol, with low sensitivity in the late morning and high sensitivity in the evening and early night (lower panel). It is decreased by hypothyroidism, genetic defects in synthesis, and protein deficiency states. Albumin has a large capacity but low affinity for cortisol, and for practical purposes albumin-bound cortisol should be considered free. Only 1% of cortisol is excreted unchanged in the urine as free cortisol; about 20% of cortisol is converted to cortisone by 11-hydroxysteroid dehydrogenase in the kidney and other tissues with mineralocorticoid receptors (see below) before reaching the liver. Many cortisol metabolites are conjugated with glucuronic acid or sulfate at the C3 and C21 hydroxyls, respectively, in the liver; they are then excreted in the urine. Mechanism of Action Most of the known effects of the glucocorticoids are mediated by widely distributed intracellular glucocorticoid receptors. These proteins are members of the superfamily of nuclear receptors, which includes steroid, sterol (vitamin D), thyroid, retinoic acid, and many other receptors with unknown or nonexistent ligands (orphan receptors). In the absence of the hormonal ligand, glucocorticoid receptors are primarily cytoplasmic, in oligomeric complexes with chaperone heat-shock proteins (hsp). Free hormone from the plasma and interstitial fluid enters the cell and binds to the receptor, inducing conformational changes that allow it to dissociate from the heat shock proteins and dimerize. These transcription factors have broad actions on the regulation of growth factors, proinflammatory cytokines, etc, and to a great extent mediate the anti-growth, anti-inflammatory, and immunosuppressive effects of glucocorticoids. The acetonide-substituted derivatives (eg, triamcinolone acetonide) have increased surface activity and are useful in dermatology. Dexamethasone is identical to betamethasone except for the configuration of the methyl group at C16: in betamethasone it is beta (projecting up from the plane of the rings); in dexamethasone it is alpha. The glucocorticoid-binding domain is located at the carboxyl terminal of the molecule. This region folds into a "two-finger" structure stabilized by zinc ions connected to cysteines to form two tetrahedrons. The amino-terminal domain is involved in the transactivation activity of the receptor and increases its specificity. The coregulators do this by serving as bridges between the receptors and other nuclear proteins and by expressing enzymatic activities such as histone acetylase or deacetylase, which alter the conformation of nucleosomes and the transcribability of genes. Between 10% and 20% of expressed genes in a cell are regulated by glucocorticoids. Some of the effects of glucocorticoids can be attributed to their binding to mineralocorticoid receptors. A mineralocorticoid effect of the higher levels of cortisol is avoided in some tissues (eg, kidney, colon, salivary glands) by expression of 11-hydroxysteroid dehydrogenase type 2, the enzyme responsible for biotransformation to its 11-keto derivative (cortisone), which has minimal action on aldosterone receptors. When the complex binds a molecule of cortisol, an unstable complex is created and the hsp90 and associated molecules are released. A variety of regulatory factors (not shown) may participate in facilitating (coactivators) or inhibiting (corepressors) the steroid response. Among the proposed mechanisms are direct effects on cell membrane receptors for the hormone or nongenomic effects of the classic hormone-bound glucocorticoid receptor. The putative membrane receptors might be entirely different from the known intracellular receptors. Such receptors are available for direct interactions with and effects on various membrane-associated or cytoplasmic proteins without the need for entry into the nucleus and induction of transcriptional actions. Physiologic Effects the glucocorticoids have widespread effects because they influence the function of most cells in the body. The major metabolic consequences of glucocorticoid secretion or administration are due to direct actions of these hormones in the cell. However, some important effects are the result of homeostatic responses by insulin and glucagon. Although many of the effects of glucocorticoids are doserelated and become magnified when large amounts are administered for therapeutic purposes, there are also other effects-called permissive effects-without which many normal functions become deficient. For example, the response of vascular and bronchial smooth muscle to catecholamines is diminished in the absence of cortisol and restored by physiologic amounts of this glucocorticoid. Metabolic Effects the glucocorticoids have important dose-related effects on carbohydrate, protein, and fat metabolism. The same effects are responsible for some of the serious adverse effects associated with their use in therapeutic doses. Glucocorticoids stimulate and are required for gluconeogenesis and glycogen synthesis in the fasting state. Glucocorticoids increase serum glucose levels and thus stimulate insulin release but inhibit the uptake of glucose by muscle cells, while they stimulate hormone-sensitive lipase and thus lipolysis. The increased insulin secretion stimulates lipogenesis and to a lesser degree inhibits lipolysis, leading to a net increase in fat deposition combined with increased release of fatty acids and glycerol into the circulation. The net results of these actions are most apparent in the fasting state, when the supply of glucose from gluconeogenesis, the release of amino acids from muscle catabolism, the inhibition of peripheral glucose uptake, and the stimulation of lipolysis all contribute to maintenance of an adequate glucose supply to the brain. Supraphysiologic amounts of glucocorticoids lead to decreased muscle mass and weakness and thinning of the skin. This effect may be partially prevented by administration of growth hormone in high doses, but this use of growth hormone is not recommended. Anti-Inflammatory and Immunosuppressive Effects Glucocorticoids dramatically reduce the manifestations of inflammation. This is due to their profound effects on the concentration, distribution, and function of peripheral leukocytes and to their suppressive effects on inflammatory cytokines and chemokines and on other mediators of inflammation. Inflammation, regardless of its cause, is characterized by the extravasation and infiltration of leukocytes into the affected tissue. These events are mediated by a complex series of interactions of white cell adhesion molecules with those on endothelial cells and are inhibited by glucocorticoids. After a single dose of a short-acting glucocorticoid, the concentration of neutrophils in the circulation increases while the lymphocytes (T and B cells), monocytes, eosinophils, and basophils decrease. The increase in neutrophils is due both to increased influx into the blood from the bone marrow and to decreased migration from the blood vessels, leading to a reduction in the number of cells at the site of inflammation. The reduction in circulating lymphocytes, monocytes, eosinophils, and basophils is primarily the result of their movement from the vascular bed to lymphoid tissue. Glucocorticoids also inhibit the functions of tissue macrophages and other antigen-presenting cells. The effect on macrophages is particularly marked and limits their ability to phagocytose and kill microorganisms and to produce tumor necrosis factor, interleukin 1, metalloproteinases, and plasminogen activator. Both macrophages and lymphocytes produce less interleukin 12 and interferon-, important inducers of Th1 cell activity, and cellular immunity. In addition to their effects on leukocyte function, glucocorticoids influence the inflammatory response by inhibiting phospholipase A2 and thus reduce the synthesis of arachidonic acid, the precursor of prostaglandins and leukotrienes, and of platelet-activating factor. Finally, glucocorticoids reduce expression of cyclooxygenase 2, the inducible form of this enzyme, in inflammatory cells, thus reducing the amount of enzyme available to produce prostaglandins (see Chapters 18 and 36). Glucocorticoids cause vasoconstriction when applied directly to the skin, possibly by suppressing mast cell degranulation. They also decrease capillary permeability by reducing the amount of histamine released by basophils and mast cells. The anti-inflammatory and immunosuppressive effects of glucocorticoids are largely due to the actions described above. Antibody production can be reduced by large doses of steroids, although it is unaffected by moderate doses (eg, 20 mg/d of prednisone). The anti-inflammatory and immunosuppressive effects of these agents are widely useful therapeutically but are also responsible for some of their most serious adverse effects (see text that follows). Adrenal insufficiency causes marked slowing of the alpha rhythm of the electroencephalogram and is associated with depression. Increased amounts of glucocorticoids often produce behavioral disturbances in humans: initially insomnia and euphoria and subsequently depression. Large doses of glucocorticoids may increase intracranial pressure (pseudotumor cerebri). Large doses of glucocorticoids have been associated with the development of peptic ulcer, possibly by suppressing the local immune response against Helicobacter pylori. They also promote fat redistribution in the body, with increase of visceral, facial, nuchal, and supraclavicular fat, and they appear to antagonize the effect of vitamin D on calcium absorption. In addition to their effects on leukocytes, they increase the number of platelets and red blood cells. Cortisol deficiency results in impaired renal function (particularly glomerular filtration), augmented vasopressin secretion, and diminished ability to excrete a water load. Indeed, the structural and functional changes in the lungs near term, including the production of pulmonary surface-active material required for air breathing (surfactant), are stimulated by glucocorticoids. This is of particular importance in the prenatal treatment of pregnant mothers or treatment of young infants and children, when the effects of glucocorticoids may be long-term or even permanent. This has stimulated the development of many synthetic steroids with anti-inflammatory and immunosuppressive activity. In some cases, the agent given is a prodrug; for example, prednisone is rapidly converted to the active product prednisolone in the body. Pharmacodynamics the actions of the synthetic steroids are similar to those of cortisol (see above). Pharmacokinetics Pharmaceutical steroids are usually synthesized from cholic acid obtained from cattle or steroid sapogenins found in plants. The metabolism of the naturally occurring adrenal steroids has been discussed above. Although they are transported and metabolized in a fashion similar to that of the endogenous steroids, important differences exist. Although hydrocortisone has some mineralocorticoid activity, this must be supplemented by an appropriate amount of a salt-retaining hormone such as fludrocortisone. Synthetic glucocorticoids that are long-acting and devoid of salt-retaining activity should not be administered to these patients. Acute-When acute adrenocortical insufficiency is suspected, treatment must be instituted immediately. Therapy consists of large amounts of parenteral hydrocortisone in addition to correction of fluid and electrolyte abnormalities and treatment of precipitating factors. Hydrocortisone sodium succinate or phosphate in doses of 100 mg intravenously is given every 8 hours until the patient is stable. The administration of salt-retaining hormone is resumed when the total hydrocortisone dosage has been reduced to 50 mg/d.
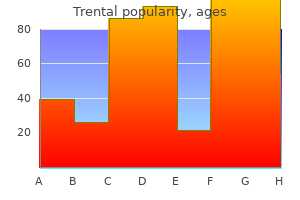
Generic trental 400 mg with mastercard. Osteoarthritis: How to get rid of arthritis in the hands and RSI.
References
- Devaney K, Goodman ZD, Ishak KG. Hepatobiliary cystadenoma and cystadenocarcinoma. A light microscopic and immunohistochemical study of 70 patients. Am J Surg Pathol. 1994;18(11):1078-1091.
- Weibel L, Turek FW, Mocaer E, Van Reeth O. A melatonin agonist facilitates circadian resynchronization in old hamsters after abrupt shifts in the light-dark cycle. Brain Res 2000;880:207-11.
- Homma S, Thompson JL, Pullicino PM, et al. Warfarin and aspirin in patients with heart failure and sinus rhythm. N Engl J Med 2012;366:1859-69.
- Coulon C, Georgiadou M, Roncal C, et al: From vessel sprouting to normalization: role of the prolyl hydroxylase domain protein/hypoxia-inducible factor oxygen-sensing machinery, Arterioscler Thromb Vasc Biol 30(12):2331-2336, 2010.
- Patel IS, Vlahos I, Wilkinson TMA, et al. Bronchiectasis, exacerbation indices, and inflammation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2004; 170: 400-407.